Abstract
Background
Patient-reported outcomes (PROs) are increasingly relevant when evaluating the treatment of orthopaedic injuries. Little is known about how PROs may vary in the setting of polytrauma or secondary to high-energy injury mechanisms, even for common injuries such as distal radius fractures.
Questions/purposes
(1) Are polytrauma and high-energy injury mechanisms associated with poorer long-term PROs (EuroQol Five Dimension Three Levels [EQ-5D-3L] and QuickDASH scores) after distal radius fractures? (2) What are the median EQ-5D-3L, EQ-VAS [EuroQol VAS], and QuickDASH scores for distal radius fractures in patients with polytrauma, high-energy monotrauma and low-energy monotrauma
Methods
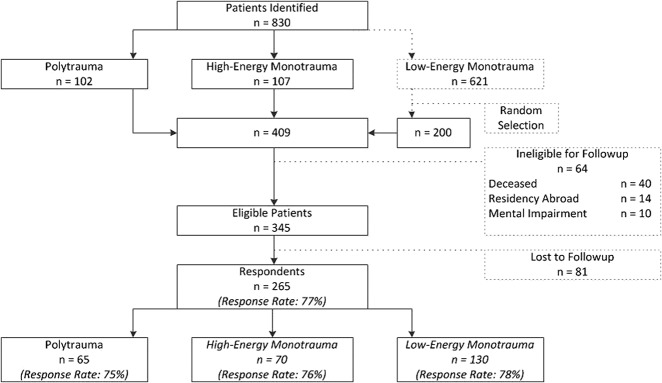
This was a retrospective study with followup by questionnaire. Patients treated both surgically and conservatively for distal radius fractures at a single Level 1 trauma center between 2008 and 2015 were approached to complete questionnaires on health-related quality of life (HRQoL) (the EQ-5D-3L and the EQ-VAS) and wrist function (the QuickDASH). Patients were grouped according to those with polytrauma (Injury Severity Score [ISS] ≥ 16), high-energy trauma (ISS < 16), and low-energy trauma based on the ISS score and injury mechanism. Initially, 409 patients were identified, of whom 345 met the inclusion criteria for followup. Two hundred sixty-five patients responded (response rate, 77% for all patients; 75% for polytrauma patients; 76% for high-energy monotrauma; 78% for low-energy monotrauma (p = 0.799 for difference between the groups). There were no major differences in baseline characteristics between respondents and nonrespondents. The association between polytrauma and high-energy injury mechanisms and PROs was assessed using forward stepwise regression modeling after performing simple bivariate linear regression analyses to identify associations between individual factors and PROs. Median outcome scores were calculated and presented.
Results
Polytrauma (intraarticular: β -0.11; 95% confidence interval [CI], -0.21 to -0.02]; p = 0.015) was associated with lower HRQoL and poorer wrist function (extraarticular: β 11.9; 95% CI, 0.4–23.4; p = 0.043; intraarticular: β 8.2; 95% CI, 2.1–14.3; p = 0.009). High-energy was associated with worse QuickDASH scores as well (extraarticular: β 9.5; 95% CI, 0.8–18.3; p = 0.033; intraarticular: β 11.8; 95% CI, 5.7–17.8; p < 0.001). For polytrauma, high-energy trauma, and low-energy trauma, the respective median EQ-5D-3L outcome scores were 0.84 (range, -0.33 to 1.00), 0.85 (range, 0.17–1.00), and 1.00 (range, 0.174–1.00). The VAS scores were 79 (range, 30–100), 80 (range, 50–100), and 80 (range, 40–100), and the QuickDASH scores were 7 (range, 0– 82), 11 (range, 0–73), and 5 (range, 0–66), respectively.
Conclusions
High-energy injury mechanisms and worse HRQoL scores were independently associated with slightly inferior wrist function after wrist fractures. Along with relatively well-known demographic and injury characteristics (gender and articular involvement), factors related to injury context (polytrauma, high-energy trauma) may account for differences in patient-reported wrist function after distal radius fractures. This information may be used to counsel patients who suffer a wrist fracture from polytrauma or high-energy trauma and to put their outcomes in context. Future research should prospectively explore whether our findings can be used to help providers to set better expectations on expected recovery.
Level of Evidence
Level III, therapeutic study.
Introduction
Patient-reported outcomes (PROs) are becoming increasingly important when evaluating the treatment of orthopaedic injuries [14]. Part of the challenge in implementing PROs is that outcomes are often context- and patient-dependent [25]. When measuring PROs within highly heterogeneous patient populations, such as a population of trauma patients, the statistical variance in measured PROs is often also correspondingly large, making an accurate comparison of treatment outcome and cost challenging [26]. To avoid this problem, many existing studies on PROs after musculoskeletal injury have focused on specific conditions or treatments using well-defined, homogenous patient populations. In this setting, patients with greater complications, such as those who sustain polytrauma or multiple (extremity) injuries, are often excluded [4, 28, 33, 35].
There is a gap in our understanding of PROs in patients who have sustained polytrauma with orthopaedic injuries and those with orthopaedic injuries sustained in the context of high-energy injury mechanisms [11]. For example, while it is well known that PROs after isolated distal radius fractures vary by age, gender, or articular stepoff, the variation in PROs is less understood in patients with multiple or high-energy injuries, even though wrist fractures occur in nearly 3.5% of patients with polytrauma [3, 10, 15, 19, 23]. Therefore, while articular stepoff and demographic characteristics may still be relevant factors, we do not know if the magnitude of their association is dwarfed by other factors related to a larger burden of injury.
Therefore, we asked: (1) Are polytrauma and high-energy injury mechanisms associated with poorer long-term PROs (EuroQol Five Dimension Three Levels [EQ-5D-3L] and QuickDASH scores) after distal radius fractures? (2) What are the median EQ-5D-3L, EQ-VAS [EuroQol VAS], and QuickDASH scores for distal radius fractures in patients with polytrauma, high-energy monotrauma, and low-energy monotrauma?
Patients and Methods
Study Design and Setting
Using followup questionnaires, we obtained additional data regarding a patient cohort on which we have previously reported. In the previous study, we used the same cohort of patients to assess the incidence rate and fracture morphology of distal radius fractures in polytrauma patients compared with monotrauma patients. [10]. In the present study, we included patients whose injury occurred between January 2008 and December 2015, and followup examinations were performed in April and May 2018.
Participants
After obtaining an institutional review board waiver, using ICD-9 codes, we identified all patients who presented with a traumatic distal radius fracture for evaluation at our Level 1 trauma center during the inclusion period in this retrospective study. We reviewed the medical records (notes and available imaging) of all patients older than 16 years at the time of trauma and older than 18 years at the time of followup to determine eligibility. Patients who underwent their initial treatment at an outside facility and patients with no followup beyond the primary presentation were deemed ineligible. Eligible patients were divided into three groups: polytrauma, high-energy monotrauma, and low-energy monotrauma. Polytrauma was defined as an Injury Severity Score (ISS) of at least 16. The ISS calculates injury severity based on the most severe injuries sustained per body region [29]. As a result, all patients with an ISS less than 16 were considered to have monotrauma. The energy of injury mechanism was defined according to the Advanced Trauma Life Support guidelines [32]. Patients who did not meet the criteria for high-energy trauma were considered to have low-energy trauma. Patients who had died, were mentally impaired, had an insufficient command of the Dutch language, and resided outside the Netherlands were excluded for followup.
All patients with polytrauma and high-energy monotrauma and a random sample of 200 patients with low-energy monotrauma who sustained a wrist fracture were included. The 200 patients in the low-energy monotrauma sample were drawn from the total cohort of 621 low-energy monotrauma patients who were treated for a wrist fracture at our institution during the study period using a random number generator. We approached the selected patients to complete two questionnaires. To all patients eligible for followup, we sent a recruitment letter explaining the study, the two questionnaires, an informed consent form, and a stamped return envelope. If there was no response within 4 weeks of mailing the letter, we contacted patients by telephone to obtain verbal informed consent and administer the questionnaires. We varied the time of the calls to maximize the response rate [28].
Questionnaires were completed after a median of 6 years since injury (IQR, 4–8 years; range, 2–10 years).
Demographics
The median age at the time of injury was 50 years (interquartile range [IQR], 31–63 years), with a median ISS of 9 (IQR, 9–14; range, 4–50). Among the group of patients with polytrauma and high-energy monotrauma, most were men (69% and 60%, respectively), while most patients with low-energy monotrauma were women (81%) (Table 1). Among all patients with wrist fractures, 145 (52%) were treated operatively (79% of fractures in patients with polytrauma, 80% of fractures in patients with high-energy monotrauma, and 36% of fractures in patients with low-energy monotrauma trauma). Most patients who were surgically treated underwent open reduction internal fixation (120 of 145; 83%). The only difference between respondents and nonrespondents was the presence of more severe fractures in polytrauma respondents than in polytrauma nonrespondents (p = 0.026) (see Table, Supplemental Digital Content 1, http://links.lww.com/CORR/A177).
Table 1.
Demographic and injury characteristics
Variables, Outcome Measures, Data Sources, and Bias
We reviewed medical records and imaging to obtain data on the following characteristics: age at the time of trauma, gender, ISS, injury mechanism, AIS codes, bilateral fracture, concomitant ipsilateral upper extremity injury, Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification, open fracture, and surgical treatment. Two investigators (SF, QV) reviewed and classified distal radius fractures according to the AO/OTA classification [22]. When there was uncertainty, two attending trauma surgeons (RM, FH) were consulted and group discussions led to consensus. To decrease interobserver variability during the analysis, all fractures were then grouped as extraarticular (23.A) or intraarticular (partial articular [23.B] and complete articular [23.C]) (thereby not accounting for radial styloid fractures). Concomitant injuries of the involved upper extremity were recorded and grouped based on anatomic location. Treatment choice was according to the treating surgeon’s preference and based on the amount of displacement, rotation, and stability.
PROs at greater than 2 years of followup were assessed using measures of general health-related quality of life (HRQoL) and wrist function. We assessed HRQoL with the EQ-5D-3L and the EQ-VAS. The EQ-5D-3L is a standardized instrument to measure general health status based on the level of experienced problems (no problems, some problems, extreme problems) in five dimensions (mobility, self-care, usual activities, pain or discomfort, and anxiety or depression) [34]. Scores were calculated using a scoring algorithm appropriate for a population of Dutch patients [27], with a possible range from -0.33 to 1.00. The EQ-VAS was developed to record an individual’s current self-rated health on a scale from 0 to 100. For both the EQ-5D and the EQ-VAS, higher scores represent higher HRQoL [34]. We evaluated patient-reported wrist function using the QuickDASH questionnaire, which consists of 11 items to measure physical function and symptoms in patients with any or multiple musculoskeletal disorders of the upper limb. Scores range from 0 to 100, with higher scores indicating worse function [2]. The DASH has been shown to be reliable, valid, and responsive in a population of patients with hand and wrist trauma, and the QuickDASH is as precise as the DASH questionnaire in patients with upper extremity disorders [7, 16]. More specifically, the DASH questionnaire has been described as a valid and reliable PRO measure to assess function and disability in Dutch patients with displaced wrist fractures [18]. Changes of approximately 14 points in the QuickDASH score represent minimal clinically important changes [12, 31].
Accounting for all Patients
A total of 830 patients were identified initially. After randomly selecting 200 patients with low-energy monotrauma trauma and applying the exclusion criteria for followup, we approached 345 patients for followup by questionnaire. Questionnaires were completed by 265 patients with 277 fractures (12 patients sustained bilateral distal radius fractures), leading to a response rate of 77% for the total cohort; 75% for polytrauma patients; 76% for high-energy monotrauma; 78% for low-energy monotrauma (p = 0.799 for difference between the groups). (Fig. 1).
Fig. 1.
This flowchart shows the inclusion process and response to the questionnaires.
Statistical Analysis and Study Size
We calculated baseline characteristics as medians and IQRs for continuous variables and absolute numbers with percentages for categorical variables. We compared the baseline characteristics of respondents and nonrespondents in the four groups of interest using chi-square and Mann-Whitney U tests, and we compared response rates between the groups using ANOVA. Differences in PROs between the groups were calculated using Kruskal-Wallis tests. The strength of correlations among the three different outcome measures was assessed using Pearson’s correlation coefficient. We first determined associations between individual factors and the PROs of interest with a simple bivariate linear regression analysis (see Table, Supplemental Digital Content 2, http://links.lww.com/CORR/A178). The final models were selected with forward stepwise regression modeling to avoid overfitting. In this approach, factors associated with the outcome in the bivariate analysis were included in the multivariable regression model. Factors no longer associated with the outcome were omitted only if doing so did not increase the deviance of the model. Factors excluded from the bivariate analysis were reincorporated only if doing so reduced the overall deviance of the model [30]. Interaction terms were applied to the analyses. All statistical analyses were performed using STATA® 13.1 (StataCorp LP, College Station, TX, USA). A p value of < 0.05 was considered statistically significant.
Results
Polytrauma (intraarticular: β -0.11; 95% confidence interval [CI], -0.21 to -0.02; p = 0.015) was associated with somewhat lower HRQoL and modest poorer wrist function (extraarticular: β 11.9; 95% CI, 0.4–23.4; p = 0.043; intraarticular β 8.2; 95% CI, 2.1–14.3; p = 0.009). High-energy was associated with slightly worse QuickDASH scores as well (extraarticular: β 9.5; 95% CI, 0.8–18.3; p = 0.033; intraarticular β: 11.8; 95% CI, 5.7–17.8; p < 0.001). Older age was also slightly associated with lower HRQoL (values per year). For the QuickDASH, male gender was associated with somewhat better outcomes when accounting for HRQoL using EQ-5D-3L outcome scores (Table 2). Male gender was also associated with somewhat better QuickDASH scores when considering EQ-VAS scores as HRQoL measure (see Table, Supplemental Digital Content 3, http://links.lww.com/CORR/A179).
Table 2.
Multivariable regression analyses
For polytrauma, high-energy trauma, and low-energy trauma, the respective median EQ-5D-3L outcome scores were 0.84 (range -0.33 to 1.00), 0.85 (range, 0.17–1.00), and 1.00 (range, 0.174–1.00). The VAS scores were 79 (range, 30–100), 80 (range, 50–100), and 80 (range, 40–100), and the QuickDASH scores were 7 (range, 0–82), 11 (range, 0–73), and 5 (range, 0–66), respectively (Fig. 2A-C). Taking into account the minimal clinically important difference (MCID) of 14, the reported differences are minor [12, 31].
Fig. 2.

(A) This graph shows EQ-5D-3L scores for patients with polytrauma, high-energy monotrauma, and low-energy monotrauma. Higher scores represent better HRQoL. (B) EQ-VAS scores for patients with polytrauma, high-energy monotrauma, and low-energy monotrauma are shown. Higher scores represent better HRQoL. (C) QuickDASH scores for patients with polytrauma, high-energy monotrauma, and low-energy monotrauma are shown. Higher scores represent worse wrist function.
All three outcome metrics were correlated: EQ-5D and EQ-VAS (correlation coefficient = 0.60, p < 0.001), QuickDASH and EQ-5D (correlation coefficient = -0.45, p < 0.001), and QuickDASH and EQ-VAS (correlation coefficient = -0.40, p < 0.001). In general, worse HRQoL scores (EQ-5D-3L and EQ-VAS) are correlated with worse wrist function (QuickDASH scores).
Discussion
Patient-reported outcomes are increasingly important for patients, physicians, and health care policymakers. These PROs may be context specific. However, there is limited information on how PROs for extremity fractures vary in patients with polytrauma and those with fractures resulting from high-energy injury mechanisms. We observed that older age and polytrauma were associated with worse general HRQoL. Polytrauma, high-energy mechanisms, intraarticular involvement, and lower HRQoL were associated with worse QuickDASH wrist function scores.
First, this study was subject to response bias; however, we did have a relatively high response rate of 77% for this type of study [28], with comparable response rates between the three groups. In addition, we identified no important differences in demographic characteristics between respondents and nonrespondents. Second, questionnaires were completed at various lengths of followup. Outcome scores change over time but have also been described as plateauing after 1 year (especially HRQoL after trauma) [1, 13], and no questionnaires in the present study were completed before this point. Furthermore, the followup duration was added to the regression analyses, but it was omitted from the final multivariable regression analysis because of a lack of association, as described in our statistical methods. Third, because this was a retrospective study, not all potential factors could be assessed. For example, function before the injury and patient psychological factors such as depression or self-esteem may have influenced the outcome measures [17], but these measures could not be examined retrospectively. Therefore, factors identified as associated with HRQoL and wrist function in the present study should not be seen as the only influential factors. Fourth, since this study was conducted in a tertiary referral center, many patients did not receive routine followup at our institution. Therefore, long-term postoperative imaging studies assessing factors such as posttraumatic arthritis were not available for most patients and limited our ability to incorporate these clinical factors into the analyses. Fifth, because patients included in the present study were treated over a relatively large time span, technique-related and surgeon-related changes may have influenced the outcome measures. However, the followup duration, indicative of the period of treatment, was not associated with PROs.
Polytrauma was associated with slightly poorer HRQoL. Longer-term wrist function was associated with injury mechanisms, intraarticular involvement, and gender. Data on the influence of energy transfer on injury during trauma are relatively sparse. Our finding that higher-energy injuries were associated with worse QuickDASH scores, even in the absence of polytrauma, may reflect soft tissue damage associated with fractures resulting from high-energy trauma. During traumatic injury, although bony injury is evident in the resulting fracture, the damaging effects of energy dissipation into the surrounding soft tissues is less obvious [21]. Similar findings have been reported for calcaneal fractures [37]. Other studies have demonstrated differences between patients with polytrauma and those with monotrauma, and our findings are aligned with the findings of these studies [15, 36, 37]. Patients with polytrauma often have persistent pain and general disabilities that impact their long-term HRQoL, and because the scope of injuries for patients with monotrauma is smaller than that for patients with polytrauma, the difference is not surprising [9, 10, 23]. In addition, it is likely that we did not see an effect of intraarticular involvement and the injury mechanism because their contribution to general HRQoL is proportionally much smaller than that of polytrauma. The importance of articular surface involvement has been known since Knirk and Jupiter’s classic paper [19], but the effect of gender on PROs is less clear [5, 20, 24, 38]. We found that gender (women) was associated with worse wrist function. Differences between men and women in the levels of functioning, coping attempts, and pain behavior may play a role, but a future study is needed to investigate these differences [8, 20].
Patients who sustained distal radius fractures in the context of polytrauma or high-energy trauma reported slightly worse EQ-5D-3L scores. These patients also reported somewhat impaired wrist functioning compared with patients who sustained low-energy distal radius fractures as their only injury. Future, prospective studies should explore the clinical importance of the differences measured, as minimal clinically important differences for the QuickDASH have been reported to be higher than the differences reported in this study [12, 31]. It is possible that these differences may have been influenced by other factors for which we could not account. We also found that the EQ-5D and EQ-VAS scores were strongly correlated with patient-reported wrist function using the QuickDASH, similar to a previous study that suggested that general health function may influence region-specific PROs [36]. The finding that EQ-VAS scores were correlated with wrist function implies that even a single question on self-reported health status can improve outcome measurement. Our results highlight the importance of obtaining general and region-specific measures of HRQoL when evaluating PROs after injury. Without adjusting for general health measures, nearly all patients who sustain wrist fractures in a polytrauma setting would be judged to have worse wrist function than a control group of patients with isolated distal radius fractures. Determining the consequence of context on injuries will only increase in importance as health systems transition to value-based payment models based on the quality of delivered care, especially since musculoskeletal injuries are the fastest growing and largest cause for US Medicare spending [6, 11, 39].
In conclusion, we found that polytrauma, high-energy injury mechanisms and worse HRQoL scores were independently associated with slightly inferior wrist function after distal radius fractures. In addition to relatively well-known demographic and injury characteristics (gender and articular involvement), factors related to injury context (polytrauma and high-energy trauma) may account for differences in patient-reported wrist function after wrist fracture.
This information may be used to counsel patients with distal radius fractures sustained in the context of polytrauma or high-energy trauma. Awareness of variation of PROs based on injury context may help physicians to better understand reported outcomes. Future research should explore whether this concept may be used to set better expectations on recovery and to target treatment options. It may also be investigated whether polytrauma and high-energy trauma affect outcomes after different types of orthopaedic injuries.
Acknowledgments
None.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Investigation performed at University Medical Center Utrecht, The Netherlands.
References
- 1.Baldry Currens JA, Coats TJ. The timing of disability measurements following injury. Injury. 2000;31:93–98. [DOI] [PubMed] [Google Scholar]
- 2.Beaton DE, Wright JG, Katz JN, Amadio P, Bombardier C, Cole D, Davis A, Hudak P, Marx R, Hawker G, Makela M, Punnett L. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am . 2005;87:1038–1046. [DOI] [PubMed] [Google Scholar]
- 3.Chung KC, Kotsis SV, Kim HM. Predictors of Functional Outcomes After Surgical Treatment of Distal Radius Fractures. J Hand Surg. Am. 2007;32:76–83. [DOI] [PubMed] [Google Scholar]
- 4.Coetzee JC, Ly TV. Treatment of primarily ligamentous Lisfranc joint injuries: primary arthrodesis compared with open reduction and internal fixation. Surgical technique. J Bone Joint Surg Am . 2007;89:122–127. [DOI] [PubMed] [Google Scholar]
- 5.Cowie J, Anakwe R, McQueen M. Factors associated with one-year outcome after distal radial fracture treatment. J Orthop Surg (Hong Kong). 2015;23:24–28. [DOI] [PubMed] [Google Scholar]
- 6.Cutler DM, Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med . 2012;366:1075–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dacombe PJ, Amirfeyz R, Davis T. Patient-reported outcome measures for hand and wrist trauma: Is there sufficient evidence of reliability, validity, and responsiveness? Hand. 2016;11:11–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Shormilisy N, Strong JMP. Associations among gender, coping patterns and functioning for individuals with chronic pain: A systematic review. Pain Res Manag . 2015;20:48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferree S, van der Vliet QMJ, van Heijl M, Houwert RM, Leenen LPH, Hietbrink F. Fractures and dislocations of the hand in polytrauma patients: Incidence, injury pattern and functional outcome. Injury. 2017;48:930–935. [DOI] [PubMed] [Google Scholar]
- 10.Ferree S, van der Vliet QMJ, Nawijn F, Bhashyam AR, Houwert RM, Leenen LPH, Hietbrink F. Epidemiology of distal radius fractures in polytrauma patients and the influence of high traumatic energy transfer. Injury. 2018;49:630-635. [DOI] [PubMed] [Google Scholar]
- 11.Flanagan CD, Rascoe AS, Wang DM, Vallier H. Revenue for initial orthopaedic trauma care. J Orthop Trauma. 2018;32:433-438. [DOI] [PubMed] [Google Scholar]
- 12.Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G. Minimal clinically important difference of the Disabilities of the Arm, Shoulder and Hand Outcome Measure (DASH) and its shortened version (QuickDASH). J Orthop Sport Phys Ther . 2014;44:30–39. [DOI] [PubMed] [Google Scholar]
- 13.Gabbe BJ, Simpson PM, Sutherland AM, Wolfe R, Lyons RA, Cameron PA. Evaluating time points for measuring recovery after major trauma in adults. Ann Surg . 2013;257:166–172. [DOI] [PubMed] [Google Scholar]
- 14.Gagnier JJ. Patient reported outcomes in orthopaedics. J Orthop Res . 2017;35:2098–2108. [DOI] [PubMed] [Google Scholar]
- 15.Gallay S, Hupel T, Beaton D, Schemitsch E, McKee M. Functional outcome of acromioclavicular joint injury in polytrauma patients. J.Orthop Trauma. 1998;12:159–163. [DOI] [PubMed] [Google Scholar]
- 16.Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): Validity and reliability based on responses within the full-length DASH. BMC Musculoskelet. Disord. 2006;7:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jayakumar P, Overbeek CL, Lamb S. What factors are associated with disability after upper extremity injuries? A systematic review. Clin Orthop Relat Res. 2018;476:2190-2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kleinlugtenbelt YV, Krol RG, Bhandari M, Goslings JC, Poolman RW, Scholtes VAB. Are the patient-rated wrist evaluation (PRWE) and the disabilities of the arm, shoulder and hand (DASH) questionnaire used in distal radial fractures truly valid and reliable? Bone Joint Res . 2018;7:36–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Join. Surg Am. 1986;68:647–59. [PubMed] [Google Scholar]
- 20.MacIntyre NJ, Dewan N. Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther. 2016;29:136–145. [DOI] [PubMed] [Google Scholar]
- 21.Marsh JL, Saltzmann CL. Axial-loading injuries: Tibial plafond fractures. In: Rockwood CA, Bucholz RW, Court-Brown CM, Heckman JD, eds. Rockwood and Green’s fractures in adults . 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:2203–2234. [Google Scholar]
- 22.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster T a, Prokuski L, Sirkin MS, Ziran B, Henley B, Audigé L. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21:1–133. [DOI] [PubMed] [Google Scholar]
- 23.Mkandawire NC, Boot DA, Braithwaite IJ, Patterson M. Musculoskeletal recovery 5 years after severe injury: Long term problems are common. Injury. 2002;33:111–115. [DOI] [PubMed] [Google Scholar]
- 24.Moore CM, Leonardi-Bee J. The prevalence of pain and disability one year post fracture of the distal radius in a UK population: A cross sectional survey. BMC Musculoskelet Disord . 2008;9:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Porter ME, Larsson S, Lee TH. Standardizing Patient Outcomes Measurement. N Engl J Med. 2016:10–12. [DOI] [PubMed] [Google Scholar]
- 26.Porter ME, Lee TH. Why strategy matters now. N Engl J Med . 2015;372:1681–1684. [DOI] [PubMed] [Google Scholar]
- 27.Ramos-Goni JM, Rivero-Arias O. Eq5d: A command to calculate index values for the EQ-5D quality-of-life instrument. Stata J . 2011;11:120–125. [Google Scholar]
- 28.Rios-Diaz AJ, Herrera-Escobar JP, Lilley EJ, Appelson JR, Gabbe B, Brasel K, deRoon-Cassini T, Schneider EB, Kasotakis G, Kaafarani H, Velmahos G, Salim A, Haider AH. Routine inclusion of long-term functional and patient reported outcomes (PROs) into trauma registries. J Trauma Acute Care Surg . 2017;83:97-104. [DOI] [PubMed] [Google Scholar]
- 29.Scaling CoI. The Abbreviated Injury Scale, 1998 revision (AIS-98). Des Plaines (IL): Association for the Advancement of Automotive Medicine (AAAM); 1998. [Google Scholar]
- 30.Shankaran V, Jolly S, Blough D, Ramsey SD. Risk factors for financial hardship in patients receiving adjuvant chemotherapy for colon cancer: a population-based exploratory analysis. J Clin Oncol . 2012;30:1608–1614. [DOI] [PubMed] [Google Scholar]
- 31.Sorensen AA, Howard D, Tan WH, Ketchersid J, Calfee RP. Minimal clinically important differences of 3 patient-rated outcomes instruments. J Hand Surg Am . 2013;38:641–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Subcommittee ATLS, American College of Surgeons’ Committee on Trauma, International ATLS working group. Advanced trauma life support (ATLS®). J Trauma Acute Care Surg . 2013;74:1363–1366. [DOI] [PubMed] [Google Scholar]
- 33.Sutherland AG, Alexander DA, Hutchison JD. Recovery after musculoskeletal trauma in men and women. J Trauma. 2005;59:213–216. [DOI] [PubMed] [Google Scholar]
- 34.Szende A, Janssen MB, Cabasés JM, Ramos Goñi JM. Self-Reported Population Health: An International Perspective based on EQ-5D. Dordrecht, The Netherlands: Springer; 2014. [PubMed] [Google Scholar]
- 35.Tejwani NC, Takemoto RC, Nayak G, Pahk B, Egol KA. Who is lost to followup?: A study of patients with distal radius fractures. Clin Orthop Relat Res . 2010;468:599–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Turchin DC, Schemitsch EH, McKee MD, Waddell JP. Do foot injuries significantly affect the functional outcome of multiply injured patients? J Orthop Trauma. 1999;13:1–4. [DOI] [PubMed] [Google Scholar]
- 37.van der Vliet QMJ, Hietbrink F, Casari F, Leenen LPH, Heng M. Factors influencing functional outcomes of subtalar fusion for posttraumatic arthritis after calcaneal fracture. Foot Ankle Int . 2018;39:1062-1069. [DOI] [PubMed] [Google Scholar]
- 38.Wilson K, von der Heyde R, Sparks M, Hammerschmidt K, Pleimann D, Ranz E, Rector J, Sniezak D. The impact of demographic factors and comorbidities on distal radius fracture outcomes. Hand. 2014;9:80–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Young WW, Young JC, Smith JS, Rhodes M. Defining the major trauma patient and trauma severity. J Trauma . 1991;31:1125–1141. [PubMed] [Google Scholar]