History
Patellar dislocation has a prevalence of approximately 5.8 per 100,000 patients. The prevalence rises substantially to 29 per 100,000 in the 10- to 17-year-old population [14]. Multiple studies have reported that trochlear dysplasia may be present in patients with patellar instability (Fig. 1) [13, 14, 18]. Trochlear dysplasia is defined as a flattened femoral groove that provides inadequate bony stability for lateral patella translation. This lack of inherent osseous stability leads to repetitive overload of the medial patellofemoral ligament, further contributing to patellar instability [6].
Fig. 1.

Clinical photographs of a patient with patellar dislocation on exam.
Malghem and Maldague [18] were radiologists who initially identified trochlear dysplasia by measuring the depth of the trochlear sulcus on lateral radiographs. In his seminal work on trochlear dysplasia, Henri Dejour et al. [12] identified the crossing sign on lateral radiographs as a radiographic marker of trochlear dysplasia. The crossing sign is the radiographic representation of the deepest point of the trochlear sulcus crossing the anterior border of the femoral condyles. The authors classified trochlear dysplasia into Types I to III based on the level at which the crossing sign was observed on lateral radiographs, with a more distal crossing sign representing a shorter length of the trochlear grove and therefore a more severe dysplasia. Later, Henri Dejour et al. [13] used radiographs and CT scans to modify his initial classification by removing the trochlear length from the classification and adding the presence of a supratrochlear spur. In 1998 David DeJour et al. [11] further modified the classification into a four-type system (Types A to D) that combined the true lateral knee radiograph with an axial CT scan. Although initially described on a CT scan, in current practice, it is classified based on either CT or MRI scan. [1, 10, 11]. The current four-type Dejour classification is based on the presence of supratrochlear spurs, double contours, and the crossing sign on lateral radiographs (Fig. 2A-B) combined with different trochlear morphologies as seen on axial images (Fig. 3A-C).
Fig. 2 A-B.
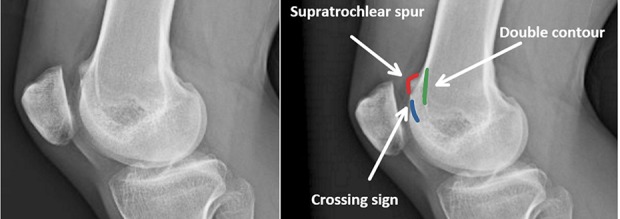
(A) Lateral knee radiograph with radiographic signs of trochlear dysplasia without labels. (B) Lateral knee radiograph with radiographic signs of trochlear dysplasia with labels: the blue line is the “Crossing sign,” representing the deepest point of the trochlear sulcus crossing the anterior border of the femoral condyles, the red line is a “Supratrochlear spur”, the prominence of the trochlea on the anterior aspect of the femoral cortex, and the green line is the “Double contour” line, the hypoplastic medial facet posterior to the lateral facet.
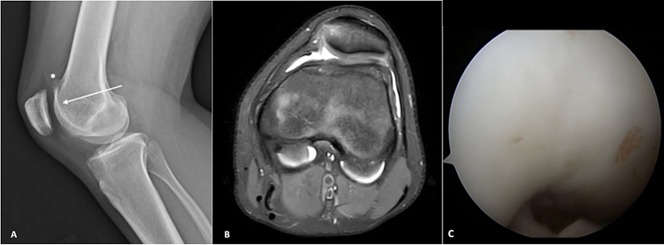
Fig. 3 A-C.
These images demonstrate trochlear dysplasia consistent with Dejour B trochlear dysplasia. (A) In this lateral knee radiograph, the asterisk (*) identifies the “Supratrochlear spur” and the arrow points to she “Crossing sign.” (B) This axial MRI shows a flattened trochlear groove. (C) This is an arthroscopic view of a flattened trochlea.
Other objective measurements have also been used to describe trochlear dysplasia including the tibial trochlear-trochlear groove distance, trochlear depth index, trochlear sulcus volume, trochlear length, medial condylar trochlear offset, lateral trochlear inclination, lateral condyle index, and patellotrochlear index [3-5, 9, 21, 23, 26]. There are other approaches for assessing patellar instability, but with respect to classifications of trochlear dysplasia, the Dejour classification may be the most widely used system. However, from the best evidence currently available, we believe this classification lacks utility in clinical practice and in the research setting due to unsatisfactory grading of the degree of dysplasia, lack of reproducibility and reliability, and its inability to guide treatment [17, 22, 24, 25].
Purpose
Classification systems are most valuable when they are reproducible and helpful in guiding clinical management. Patellar instability can be caused by multiple different anatomic factors, including trochlear dysplasia, patella alta, patellar tilt, rotational deformities, and increased tibial trochlear-trochlear groove distances [6, 13]. Dejour et al. [13] found that among patients with a history of patellofemoral dislocation, 85% had radiographically observed trochlear dysplasia. The crossing sign was identified in 96% of patients with trochlear dysplasia compared with 3% of controls. The four-type Dejour classification system was originally devised to help identify and categorize trochlear dysplasia and potentially determine treatment options; however, we believe it does not accurately or consistently grade the severity of trochlear dysplasia [13]. Moreover, by itself, the Dejour classification may not be helpful in preoperative planning and counseling.
There is some inconsistency in the literature regarding which Dejour types should be considered severe dysplasia. Some authors have simplified the four-type Dejour classification into two grades (low and high grade) for evaluation of trochlear dysplasia. Some authors believe that medial patellofemoral ligament reconstruction alone may improve clinical and functional outcomes in moderate dysplasia while reserving a combined medial patellofemoral ligament with trochleoplasty for severe dysplasia [27]. Others have reported that as an isolated procedure, trochleoplasty should be all that is necessary in the presence of any grade of trochlear dysplasia [7]. Still others have reported that trochleoplasty, as a stand-alone procedure, is effective in knees with substantial features of high-grade trochlear dysplasia [8]. Fucentese et al. [15], using a modified classification combining patients with Dejour B and D as high-grade and A and C as low-grade trochlear dysplasia, evaluated the clinical outcomes at a mean follow-up of 4 years for 44 knees in 38 patients who underwent trochleoplasty for patellar instability. The authors found that patients with Dejour Types B and D dysplasia, in which a supratrochlear spur is present, had better outcomes with lower subjective knee pain and pain during sporting activities than patients with Dejour Type A or C dysplasia, in which a supratrochlear spur is not present.
Description
The Dejour classification of trochlear dysplasia is assessed using lateral knee radiographs as well as axial CT or MRI imaging to evaluate abnormal trochlear morphology. The classification is based on the presence of the crossing sign, a supratrochlear spur, and double contour sign on lateral radiographs [11, 13]. A crossing sign, believed to be pathognomonic for trochlear dysplasia, is described as the radiographic representation of the deepest point on the trochlear sulcus that crosses the anterior border of the femoral condyles. This reflects a deficient proximal trochlea with a reduced relative height of the lateral trochlear wall [12]. A supratrochlear spur is a prominence of the trochlea above the anterior femoral cortex and is measured by the distance between a line tangential to the anterior femoral cortex and a line parallel to it through the trochlear groove. A spur larger than > 3 mm is believed to exemplify high-grade dysplasia. This indicates an elevation of the trochlear floor with loss of relative lateral trochlear height and increased susceptibility to patellar instability [2]. A double contour is present when the medial facet is hypoplastic and can be visualized posterior to the lateral facet. The classification further differentiates dysplasia based on axial CT or MRI imaging. On axial images, the trochlea may be seen as shallow but concave and flattened, having lateral facet convexity and medial facet hypoplasia, and a “cliff” (clearly asymmetric facets with a vertical inclination between the facets) in Dejour Types A to D, respectively (Fig. 4). A sulcus angle can also be measured from the highest point on the condyles to the lowest point of the intercondylar groove, with an average measurement of 137° ± 8° in healthy individuals [13]. Although not a part of the Dejour classification, a sulcus angle measuring more than 145° in a Merchant view knee radiograph with the knee in 45° knee flexion and the beam at 30° inclination caudal down the patellar femoral joint is characteristic of trochlear dysplasia (Fig. 5) [13, 19].
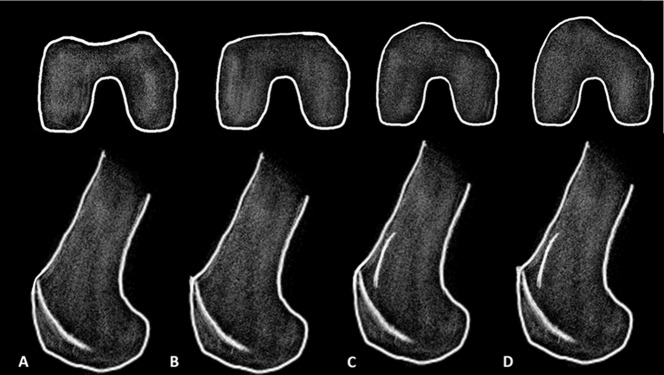
Fig. 4 A-D.
Illustrations of the Dejour classification on axial and lateral projection depicted as: (A) Dejour A, (B) Dejour B, (C) Dejour C, and (D) Dejour D.
Fig. 5 A-B.
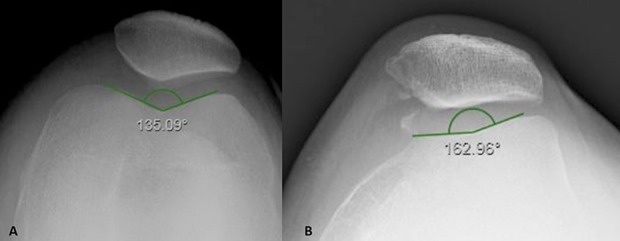
A sulcus angle is drawn on a Merchant view of the knee from the highest points of the medial and lateral condyle to the lowest point of the intercondylar notch. (A) This figure shows normal trochlear sulcus measurement (138° ± 6°). (B) In this image, a sulcus angle > 145° is indicative of trochlear dysplasia.
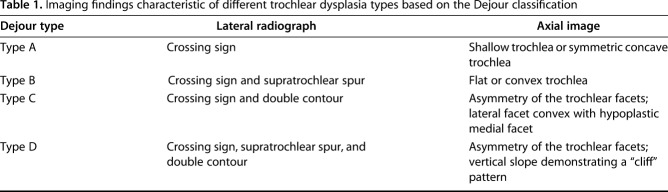
The Dejour classification system is divided into Types A, B, C, and D dysplasia using specific radiographic parameters (Table 1). In type A dysplasia (Fig. 4A), there is a crossing sign on the lateral radiographs and the trochlear groove is symmetric but shallower than normal, with a sulcus angle greater than 145° on axial images. In type B (Fig. 4B), there is a crossing sign as well as a supratrochlear spur on lateral radiographs, with a flat trochlea on axial images. In Type C (Fig. 4C), there is a crossing sign and double contour on lateral radiographs, with lateral facet convexity and medial facet hypoplasia on axial images. In Type D (Fig. 4D), there is a crossing sign, supratrochlear spur, and double contour on lateral radiographs, and a “cliff” on axial images because of asymmetry of the lateral and medial femoral trochlear facets.
Table 1.
Imaging findings characteristic of different trochlear dysplasia types based on the Dejour classification
Validation
Three studies have evaluated the reliability of the Dejour classification. Current evidence suggests that the four-type Dejour classification has substantial intra- and interobserver variability, and therefore offers little value in day-to-day clinical assessment of grading and classifying trochlear dysplasia and for communication in research. The classification by itself does not reliably grade trochlear dysplasia unless it is simplified to a two-grade classification, that is, low-grade versus high-grade, and therefore does not provide any guidelines for treatment. Moreover, there is no agreement as to which Dejour types should be classified as low- and high-grade dysplasia. Remy et al. [22] reported on the validity of the original Dejour classification, with seven observers evaluating 68 lateral knee radiographs. They found poor intraobserver and interobserver reliability, with kappa correlation coefficients of 0.3 and 0.17, respectively. That study did find that the crossing sign was a good indicator of trochlear dysplasia, with only 3.1% of dysplastic trochleas being rated as normal. Various authors have found that the reliability of the Dejour classification may be potentially improved if the trochlear morphology is grouped into low-grade (Dejour Type A) or high-grade dysplasia (Dejour Types B, C, and D). In a study of 50 knees, Lippacher et al. [17] reported on the intra- and interobserver reliability of the Dejour classification, with four surgeons first evaluating lateral radiographs and then independently evaluating axial MRIs at two time points 4 weeks apart. For the lateral radiographs, the four classification types had intraobserver reliabilities ranging from 30% to 78% and on axial MRI ranging between 32% and 74%. The interobserver reliability on lateral radiographs ranged from 24% to 58% and on axial MRI ranged from 28% to 60%. When using a two-grade simplified grouping with Type A as low-grade and Types B, C, and D as high-grade dysplasia, the authors demonstrated improved the intra- and interobserver reliability. With this grouping, the intra- and interobserver reliability on lateral radiographs ranged from 56% to 88% and 60% to 76% respectively. On axial MRI, the intra- and interobserver reliability ranged from 70% to 90% and 62% to 96%, respectively. However, it must be noted that this grouping was not described for the grading of trochlear dysplasia in the original Dejour classification and potentially gives up some utility by pooling dissimilar entities. Nevertheless, the reliability of this simplified classification is still moderate to low in this study. More recently, Tscholl et al. [25] evaluated the agreement between lateral radiographs and axial MRI in analyzing Dejour’s classification of trochlear dysplasia in 228 knees with recurrent patellar dislocations. The authors demonstrated that the overall agreement of the four-type Dejour classification scheme was just 45% when trochlear dysplasia was measured at the mid-patellar height approximately 3.8 ± 0.6 cm above the joint line, but increased to 82% when patients were grouped into low-grade (Dejour Types A and C) and high-grade dysplasia (Dejour Types B and D) [25].
In a study of 38 skeletally immature patients undergoing surgery for patellar instability, Stepanovich et al. [24], compared the Dejour classification and the medial condylar trochlear offset, trochlear depth index, and lateral trochlear inclination to assess their reliability and correlation with patellar instability. The authors found that the four Dejour types as seen on MRI had low interobserver (kappa = 0.687) and intraobserver reliability (kappa = 0.596). Other measurements used in this study [24], including the medial condylar trochlear offset (kappa = 0.86 and 0.95), trochlear depth index (kappa = 0.93 and 0.98), and lateral trochlear inclination (kappa = 0.94 and 0.93), showed higher inter and intraobserver reliability, respectively. Although the Dejour classification is widely known, these alternative measurements of trochlear morphometry may be more reliable and reproducible than the Dejour types in describing trochlear dysplasia. Data from the studies currently available suggest that the Dejour classification is unreliable and should not be used routinely in clinical practice, as better alternatives are available. Nevertheless, further validation studies are needed to better evaluate the best alternative measurements to use to grade trochlear dysplasia.
The Dejour classification is a well-known classification system of trochlear dysplasia evaluating the risk of patellar instability. However, many other methods have been described for evaluating trochlear dysplasia and patellar instability [4, 6, 9, 20, 21]. MRI can be used to evaluate several different anatomic structures, including the medial patellofemoral ligament, and measurements can be made for evaluating trochlear morphology. Carrillon et al. [9] describe the lateral trochlear inclination, measured by drawing a line parallel to the posterior femoral condyle and another line parallel to the articular surface of the lateral trochlear facet; the angle thus formed was found to be 93% sensitive and 87% specific for identifying patellar instability using a cutoff of 11°. However, currently there are no studies evaluating the intra- and interobserver reliability for these trochlear morphometric measurements. The trochlear depth index is measured using a modification of the technique previously described by Pfirrmann et al. [21]. A line is initially drawn parallel to the posterior condyle that intersects at the lowest point of the trochlea. Using this line, the maximum perpendicular height of the medial and lateral trochlear facets is measured. The trochlear depth index is finally calculated as the average of the medial and lateral trochlear facet heights. One radiographic study found that a trochlear depth cut off of less than 3 mm was 100% sensitive and 96% specific in adults and 81% sensitive and 89% specific in a pediatric population for the diagnosis of trochlear dysplasia [21]. Biedert et al. [3, 4] described two additional measurements of trochlear morphology, the lateral condyle index and patellotrochlear index, which are measured on a lateral cut of a sagittal MRI with the knee in 0° flexion. Alternative methods for evaluating trochlear morphology for dysplasia have thus been described, but have not undergone substantial validation studies.
Limitations
The Dejour classification has several limitations. The most important limitation of this classification is that the reliability and reproducibility is too low for routine use in research and clinical practice. The classification system is based on true lateral radiographs with knees in 30° of flexion with superimposition of the femoral condyles and an axial CT or MRI. As a result, the findings are sensitive to the quality of lateral radiographs. Even 5° of rotation of the distal femur can cause a false-positive or false-negative result in identifying the crossing sign, which is an indication of trochlear dysplasia [16]. The classification also does not provide any measurements of trochlear length or depth of the trochlear groove, diminishing its utility in describing all types of trochleas. It also does not provide any cumulative grading of trochlea dysplasia, and thus does not offer firm guidelines regarding surgical management. As in adults, the Dejour classification has also been reported to have limited reliability in children with trochlear dysplasia [24].
In a recent study, Nelitz et al. [20] found that the four-type Dejour classification could not be accurately defined using quantitative measurements of trochlear geometry. They found that various quantitative measurements of trochlear dysplasia such as medial, central, and lateral trochlear height, patellar lateralization, and condylar asymmetry were variably distributed among Dejour Types A to D. When the authors grouped patients with Dejour Types B, C, and D as having high-grade dysplasia and Dejour Type A patients as low-grade dysplasia, they demonstrated that sensitivity ranged from 75% to 86% and specificity from 76% to 84% for lateral trochlear inclination, trochlear facet asymmetry and depth of trochlear groove in defining low- and high-grade dysplasia. All remaining measurements had poor sensitivity varying from 49% to 67% and poor specificity ranging from 40% to 72%. The authors found that the intra- and interobserver reliability for all measured parameters were fair to moderate for high-grade dysplasia (intraclass correlation coefficient [ICC] values varied between 0.34 and 0.58) and good to excellent for low-grade dysplasia [ICC values varied between 0.71 and 0.88]), which further exemplified that the Dejour classification scheme is unreliable for objective assessment of trochlear dysplasia.
Conclusion
The Dejour classification describes trochlear morphology based on lateral radiographs and axial CT or MRI images. However, its poor reliability, reproducibility, and lack of objective grading regarding the severity of trochlear dysplasia as a treatment guide implies that it has limited value. Furthermore, it could potentially be misleading if used in the clinical and research setting. The usefulness of the Dejour classification may be enhanced with the use of advanced imaging modalities such as MRI, both for quantitative grading and improving its clinical relevance. There is a need for studies evaluating various indices describing trochlear morphometry to define the severity of trochlear dysplasia and aid in treatment decisions.
Acknowledgments
We would like to thank Daniel Phelan MD for helping us select the clinical images that have been included in the manuscript.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution waived approval for the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Albany Medical Center, Albany, NY, USA.
References
- 1.Arendt EA, Dejour D. Patella instability: building bridges across the ocean a historic review. Knee Surg Sports Traumatol Arthrosc. 2013;21:279-293. [DOI] [PubMed] [Google Scholar]
- 2.Beaufils P, Thaunat M, Pujol N, Scheffler S, Rossi R, Carmont M. Trochleoplasty in major trochlear dysplasia: current concepts. Sports Med Arthrosc Rehabil Ther Technol. 2012;4:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Biedert RM, Albrecht S. The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc. 2006;14:707-712. [DOI] [PubMed] [Google Scholar]
- 4.Biedert RM, Netzer P, Gal I, Sigg A, Tscholl PM. The lateral condyle index: a new index for assessing the length of the lateral articular trochlea as predisposing factor for patellar instability. Int Orthop. 2011;35:1327-1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307-310. [PubMed] [Google Scholar]
- 6.Bollier M, Fulkerson JP. The role of trochlear dysplasia in patellofemoral instability. J A, Acad Orthop Surg. 2011;19:8-16. [DOI] [PubMed] [Google Scholar]
- 7.Camathias C, Speth BM, Rutz E, Schlemmer T, Papp K, Vavken P, Studer K. Solitary trochleoplasty for treatment of recurrent patellar dislocation. JBJS Essent Surg Tech. 2018;8:e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Camathias C, Studer K, Kiapour A, Rutz E, Vavken P. Trochleoplasty as a solitary treatment for recurrent patellar dislocation results in good clinical outcome in adolescents. Am J Sports Med. 2016;44:2855-2863. [DOI] [PubMed] [Google Scholar]
- 9.Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh VA. Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology. 2000;216:582-585. [DOI] [PubMed] [Google Scholar]
- 10.Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc Rev. 2007;15:39-46. [DOI] [PubMed] [Google Scholar]
- 11.Dejour D, Reynaud P, Lecoultre B. Pain and patellar instability classification. [in French]. Med Hyg. 1998;56:1466-1471. [Google Scholar]
- 12.Dejour H, Walch G, Neyret P, Adeleine P. Dysplasia of the femoral trochlea. [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1990;76:45-54. [PubMed] [Google Scholar]
- 13.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19-26. [DOI] [PubMed] [Google Scholar]
- 14.Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, White LM. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114-1121. [DOI] [PubMed] [Google Scholar]
- 15.Fucentese SF, Zingg PO, Schmitt J, Pfirrmann CW, Meyer DC, Koch PP. Classification of trochlear dysplasia as predictor of clinical outcome after trochleoplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19:1655-1661. [DOI] [PubMed] [Google Scholar]
- 16.Koeter S, Bongers EM, de Rooij J, van Kampen A. Minimal rotation aberrations cause radiographic misdiagnosis of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2006;14:713-717. [DOI] [PubMed] [Google Scholar]
- 17.Lippacher S, Dejour D, Elsharkawi M, Dornacher D, Ring C, Dreyhaupt J, Reichel H, Nelitz M. Observer agreement on the Dejour trochlear dysplasia classification: a comparison of true lateral radiographs and axial magnetic resonance images. Am J Sports Med. 2012;40:837-843. [DOI] [PubMed] [Google Scholar]
- 18.Malghem J, Maldague B. Depth insufficiency of the proximal trochlear groove on lateral radiographs of the knee: relation to patellar dislocation. Radiology. 1989;170:507-510. [DOI] [PubMed] [Google Scholar]
- 19.Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391-1396. [PubMed] [Google Scholar]
- 20.Nelitz M, Lippacher S, Reichel H, Dornacher D. Evaluation of trochlear dysplasia using MRI: correlation between the classification system of Dejour and objective parameters of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2014;22:120-127. [DOI] [PubMed] [Google Scholar]
- 21.Pfirrmann CW, Zanetti M, Romero J, Hodler J. Femoral trochlear dysplasia: MR findings. Radiology. 2000;216:858-864. [DOI] [PubMed] [Google Scholar]
- 22.Remy F, Chantelot C, Fontaine C, Demondion X, Migaud H, Gougeon F. Inter- and intraobserver reproducibility in radiographic diagnosis and classification of femoral trochlear dysplasia. Surg Radiol Anat. 1998;20:285-289. [DOI] [PubMed] [Google Scholar]
- 23.Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J. The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee. 2006;13:26-31. [DOI] [PubMed] [Google Scholar]
- 24.Stepanovich M, Bomar JD, Pennock AT. Are the current classifications and radiographic measurements for trochlear dysplasia appropriate in the skeletally immature patient? Orthop J Sports Med. 2016;4:2325967116669490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tscholl PM, Wanivenhaus F, Fucentese SF. Conventional radiographs and magnetic resonance imaging for the analysis of trochlear dysplasia: The influence of selected levels on magnetic resonance imaging. Am J Sports Med. 2017;45:1059-1065. [DOI] [PubMed] [Google Scholar]
- 26.Voss A, Shin SR, Murakami AM, Cote MP, Achtnich A, Herbst E, Schepsis AA, Edgar C. Objective quantification of trochlear dysplasia: Assessment of the difference in morphology between control and chronic patellofemoral instability patients. Knee. 2017;24:1247-1255. [DOI] [PubMed] [Google Scholar]
- 27.Zaffagnini S, Previtali D, Tamborini S, Pagliazzi G, Filardo G, Candrian C. Recurrent patellar dislocations: trochleoplasty improves the results of medial patellofemoral ligament surgery only in severe trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. [Published online ahead of print March 22, 2019]. DOI: 10.1007/s00167-019-05469-4. [DOI] [PubMed]