Abstract
Background
The elbow is more susceptible to loss of motion after trauma than any other joint. Open arthrolysis often is performed for posttraumatic elbow stiffness if the stiffness does not improve with nonsurgical treatment, but the midterm results of this procedure and factors that may limit recovery have not been widely studied.
Questions/purposes
We reviewed patients who had undergone open arthrolysis with hinged external fixator for severe posttraumatic elbow stiffness (ROM ≤ 60°) with a minimum of 5 years followup to (1) analyze ROM gains; (2) assess functional improvement with the Mayo Elbow Performance Index (MEPI) and DASH, quality of life with the SF-36, pain with VAS, and ulnar nerve function with the Amadio rating scale and Dellon classification; and (3) identify complications and risk factors that might hinder mid-term elbow motion recovery after this procedure.
Methods
Between March 2011 and December 2012, we generally offered patients with elbow stiffness an open arthrolysis procedure when function did not improve with 6 months of nonoperative therapy, and no contraindications such as immature heterotopic ossification or complete destruction of articular cartilage were present. During that time, 161 patients underwent open arthrolysis for posttraumatic elbow stiffness at our institution; 49 of them satisfied the study inclusion criteria (adults with elbow ROM ≤ 60° as a result of trauma) and exclusion criteria (stiffness caused by burns or central nervous system injuries, causative trauma associated with nonunion or malunion of the elbow, severe articular damage that would have necessitated joint arthroplasty, or prior elbow release). In general, a combined medial-lateral approach to the elbow was performed to address the soft tissue tethers and any blocks to elbow motion, and a hinged external fixator was applied for 6 weeks to maintain elbow stability and improve the efficacy of postoperative rehabilitation. These patients were evaluated retrospectively at a mean followup period of 69 months (range, 62–83 months), and demographics, disease characteristics, arthrolysis details, pre- and postoutcome measures as noted, and complications were recorded via an electronic database. Multivariate regression analysis was performed to identify factors associated with ROM recovery.
Results
At final followup, total ROM increased from a preoperative mean of 27 ± 20° to a postoperative mean of 131 ± 11° (mean difference, 104°; 95% CI, 98°–111°; p < 0.001), and 98% (48 of 49) of patients achieved a functional ROM of 30° to 130°. Improvements were also found in functional scores (MEPI: 54 ± 12 to 95 ± 7, mean difference, 41 points; DASH: 48 ± 17 to 8 ± 8, mean difference, 40 points; both p < 0.001), life quality (physical SF-36: 46 ± 11 to 81 ± 12, mean difference, 35 points; mental SF-36: 43 ± 14 to 80 ± 9, mean difference, 37 points; both p < .001), pain (VAS: 2.5 ± 2.4 to 0.4 ± 0.8; mean difference, 2.0 points; p < 0.001), and ulnar nerve function (Amadio score: 7.8 ± 1.9 to 8.4 ± 0.8; mean difference, 0.6 points; p = 0.004). A total of 18% (nine of 49 patients) developed complications, including new-onset or exacerbated nerve symptoms (four patients), recurrent heterotopic ossification (two patients), and pin-related infections (three patients). No patients underwent subsequent surgery for any of the above complications. Lastly, the medium-term ROM was divided into ROM ≤ 120° (n = 9) and ROM > 120° (n = 40). After controlling for potential confounding variables such as duration of stiffness and tobacco use, we found that tobacco use was the only independent risk factor examined (odds ratio, 9; 95% CI, 2–47; p = 0.009) associated with recovery of ROM.
Conclusions
Satisfactory medium-term results were found for open arthrolysis with hinged external fixation with our protocol in patients who had severe posttraumatic elbow stiffness. Appropriate and sufficient releases of tethered soft tissues and correction of any blocks that affect elbow motion intraoperatively, a dedicated team approach, and an aggressive and systematic postoperative rehabilitation program are the core steps for this procedure. Additionally, the importance of preoperative discontinuation of tobacco use should be emphasized.
Level of Evidence
Level IV, therapeutic study.
Introduction
The elbow is a complex trochleo-ginglymoid joint, consisting of articulations between the humerus, ulna, and radius, which allows the hand to move freely within a sphere, created by shoulder movement, with a radius formed by the combined length of the arm and forearm. The full range of normal elbow motion is not needed for most activities, as an extension-flexion arc of 100° (between 30° and 130°) and a forearm rotational arc of 100° equally divided between pronation and supination are enough to lead a relatively normal life [23]. However, a loss of 50° in the arc of motion has been reported to cause an 80% loss of function [23]; moreover, increased usage of devices such as computers and mobile phones may require more upper-extremity mobility than previously described; for example, one more recent study found an extension-flexion arc of about 120° from 23° to 142° and a pronation-supination arc of nearly 140° from 65° to 77° was needed for more contemporary demands on the elbow [30].
Elbow stiffness can be disabling, in that it impairs important daily activities; the elbow is more susceptible to motion loss than any other joint after trauma [9]. Bony and soft-tissue factors are important causes of elbow arthrofibrosis [12, 25], which can be anatomically classified as intrinsic, extrinsic, or mixed [22]. Mansat and Morrey [21] classified the severity of stiffness by ROM: > 90°, mild; 60–90°, moderate; 30–60°, severe; < 30°, extremely severe. Restoring a functional ROM and achieving a pain-free, stable elbow are the primary goals when treating elbow stiffness. Early physical therapy, and/or dynamic or static progressive splinting, may restore functional motion in some patients with extrinsic elbow contracture [38]. Generally, surgery is indicated if the lost function does not improve with nonoperative therapy. Open arthrolysis is the most commonly reported treatment method and has been proven effective: a mean ROM of 103° (varying from 85° to 129°), a mean gain of 51° (varying from 38° to 60°), and a complication rate of 23% (between 0% and 59%) at followup were reported in a systematic review including 637 patients in 21 studies [13].
Numerous articles over recent decades have reported the short-term (< 5 years) benefits of open arthrolysis [3, 7, 10, 13, 14, 29, 39-41, 43, 46]. However, to our knowledge no study has reported the medium-term (≥ 5 years) clinical outcomes for severe posttraumatic elbow stiffness (ROM ≤ 60°) treated by open arthrolysis and external fixation and risk factors that might influence elbow motion recovery in this time frame.
We therefore reviewed our experience with a large group of patients who underwent open arthrolysis for elbow stiffness with subsequent treatment involving hinged external fixator placement and a systematic postoperative rehabilitation program to (1) analyze ROM gains; (2) assess functional improvement with the Mayo Elbow Performance Index (MEPI) and the DASH, quality of life quality with the SF-36, pain with the VAS, and ulnar nerve function with the Amadio rating scale and Dellon classification; and (3) identify complications and risk factors that might hinder midterm elbow motion recovery after this procedure.
Patients and Methods
Study Design and Participants
This retrospective study considered patients who presented to our institution with elbow stiffness between March 2011 and December 2012. The ethics committee of our hospital concluded that no approval was necessary because of the retrospective study design. All patients signed informed consent to collect, file, and use the data.
Our indications for open arthrolysis were (1) no benefit from a 6-month trial of nonoperative therapy; (2) lack of extension > 30° or flexion < 130°. Contraindications were (1) immature heterotopic ossification (HO) , (2) local history of soft-tissue infection, (3) complete destruction of the articular cartilage, (4) inability to perform postoperative rehabilitation, and (5) severe systemic disorders prohibiting surgery.
For those undergoing open arthrolysis, inclusion criteria for this study were severe elbow stiffness as a result of trauma (ROM ≤ 60°) in adult patients at the time of arthrolysis. Our exclusion criteria were: (1) trauma associated with burns or central nervous system injuries, (2) trauma associated with non- or malunion of the elbow, (3) severe articular damage such that arthroplasty would be indicated, and (4) prior elbow release.
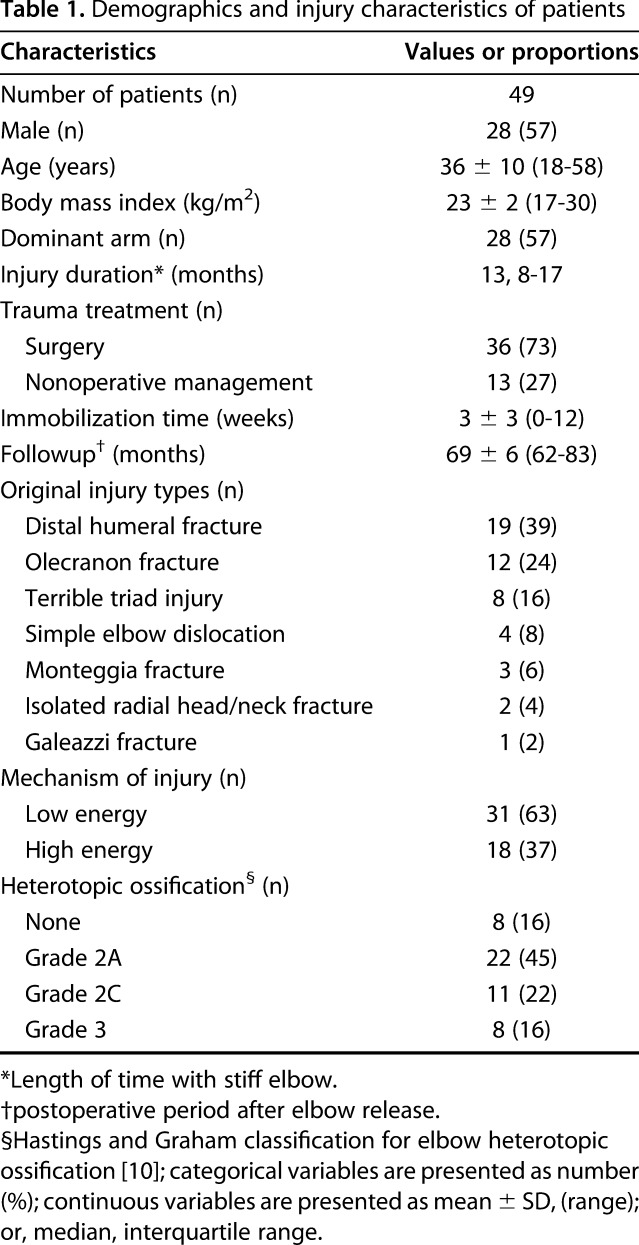
During the period of this study, 161 patients underwent open arthrolysis at our institution. After we applied the aforementioned inclusion and exclusion criteria for the present study, 49 patients remained in the analysis (Fig. 1). The 49 patients included 28 men and 21 women; 28 patients had stiffness in their dominant arm. Twenty-seven patients had extremely severe motion loss (< 30°) and 22 had severe motion loss (30°–60°); the mean age was 36 ± 10 years (range, 18–58 years) at time of release. Forty-one patients demonstrated some degree of mature HO, including 22 Hastings Grade 2A, 11 Grade 2C and eight Grade 3 [11]. The mean followup period was 69 ± 6 months (range, 62–83 months). The most common mechanism of initial elbow injury was a low-energy injury (31 of 49, 63%), and the most common initial injury type was distal humerus fracture (19 of 49, 39%) (Table 1).
Fig. 1.
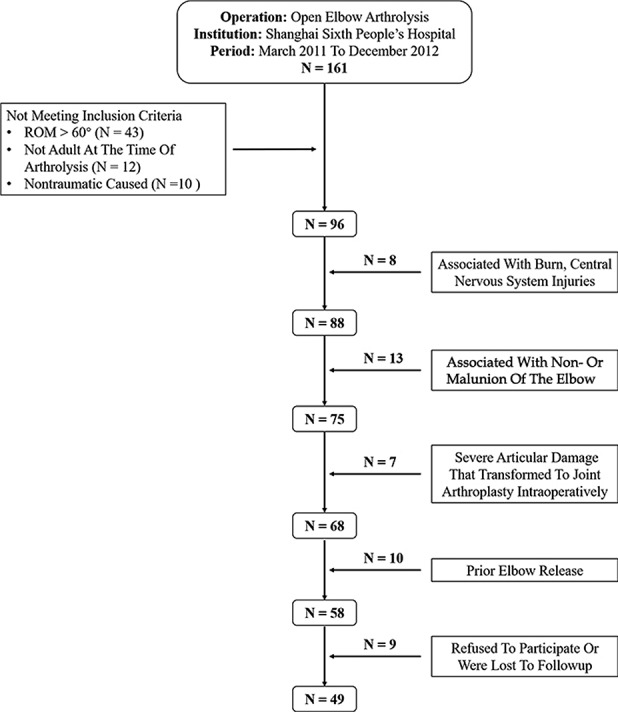
This flowchart shows the patient inclusion and exclusion criteria.
Table 1.
Demographics and injury characteristics of patients
Surgical Technique
All procedures were performed with the patient in the supine position under general anesthesia by the senior surgeon (CF) with a sterile air tourniquet applied. The incision was chosen based on prior surgical incisions and the anatomy involved. In general, a combination of lateral (along the lateral column) and medial-posterior (posterior to the medial epicondyle) incisions were preferred, unless the patient had undergone previous surgery via a posterior incision. In our experience, we divided the factors affecting elbow motion into tethering constraints and blocks to motion. Either anterior tethering (such as a thickened anterior capsule, contracture or HO of the anterior band of the medial collateral ligament and/or flexor muscle-tendon units, or scarred skin); or posterior block, (for example, a scar or loose bodies in the olecranon fossa, or olecranon osteophytes) can cause extension dysfunction. Similarly, either posterior tethering or anterior blocks may lead to loss of elbow flexion. The strategies of arthrolysis were generally similar for stiffness caused by trauma such as distal humerus fracture, olecranon fracture, or elbow dislocation. After the skin incision, the deeper exposure for arthrolysis was similar regardless of the incision. In general, we primarily used a combined medial-lateral approach, with the medial approach addressing posterior tethering and block factors, and the lateral approach managing anterior tethering and block factors [20, 40].
In the medial approach, the ulnar nerve was identified at the medial border of the triceps and was routinely released from the ligament of Struthers or the medial intermuscular septum proximally to its entry under the flexor carpi ulnaris distally. Careful attention was paid to the preservation of vascular pedicles of the ulnar nerve. Then the triceps tendon margin was split and reflected off the distal humerus, and the posterior and transverse bundles of the medial collateral ligament were incised to expose the posterior aspect of the joint. The posterior capsule was incised or resected if a contracture had formed as a posterior tethering factor. Posterior block factors such as scar tissue, loose body or osteophyte in the olecranon fossa were removed under direct visualization. Olecranon fossa osteoplasty or olecranon tip osteotomy was performed if osteophytes had formed around the olecranon, to achieve more improvement in extension. Occasionally a pie-crusting technique for triceps tendon release (another type of posterior tethering factor) was performed as needed to improve flexion contracture, in which the triceps tendon was gradually lengthened by making multiple stab incisions into the tendon with a No. 11 surgical blade [41].
From the lateral approach, the extensor origins of the brachioradialis and extensor carpi radialis longus tendons were elevated away from the lateral epicondyle, and the brachialis and the radial nerve were then mobilized away from the distal humerus to the medial-anterior region using an elevator to expose the anterior elbow. The lateral collateral ligament was partially released, and the hypertrophic anterior capsule (an anterior tethering factor) excision was performed while protecting the median nerve and the brachial artery. Anterior block factors like scar tissue, loose bodies or osteophyte in the radial fossa or coronoid fossa were also removed under direct visualization. Coronoid fossa osteoplasty was performed if osteophytes had formed around the coronoid, to achieve more improvement in flexion. Exploration and release of the radial nerve was performed (four patients in this study) if the patient had a very long disease duration or childhood injury, especially in cases of severe extension deformity, extensive anterolateral heterotopic bone, or preoperative radial nerve symptoms.
Forearm rotation dysfunction combined with stiffness was managed in the same operation as extension-flexion dysfunction in our study, but only when caused by an abnormal proximal radioulnar joint (PRUJ), an incongruent radial head after trauma, or adhesions between the annular ligament and radial head; otherwise, we recommend treating these issues separately. Scar and adhesions around the radial head and PRUJ primarily lead to rotation dysfunction, and contracture release was performed in these circumstances. Reconstruction was performed for radial-head malunion or nonunion limiting forearm rotation after elbow trauma. Simple radial head osteoplasty, head resection, and prosthetic replacement are the three choices in this setting. Special attention was paid to the posterior interosseous nerve, which runs from the radial nerve at the radiohumeral joint line proximally to its entry under the supinator distally.
We routinely remove metal implants that were inserted during previous procedures if the preoperative radiographs show solid fracture union and the time interval between the previous fixation and the index procedure is long enough to allow for fracture union. In the event of iatrogenic fractures, surgeons should follow the principle of “release first, removal next,” meaning that the metal implants are removed after complete release.
Passive mobility of 0° to 130° at surgery was considered to be a sufficient release. Stress and pivot-shift tests were performed intraoperatively to assess elbow stability. The collateral ligaments and the flexor and extensor origins were repaired or reattached for all patients, either by direct suture or suture anchor depending on stability after arthrolysis [39]. In all patients, after satisfactory ROM was achieved, a hinged external fixator (Orthofix, Verona, Italy) was applied to the elbow along its rotational axis as identified by C-arm radiography, as described in our previous studies [20, 39, 43, 46]. This provides additional stability and enables early, controlled joint mobilization. The ulnar nerve was transposed subcutaneously and stabilized with fascial slings [6]. Two drainage tubes were left in place to prevent hematoma, and the wound was closed in layers after local application of vancomycin powder [42]. The elbow ROM was documented in all patients to guide individual rehabilitation.
The mean operative time was 149 ± 50 minutes (range, 75-300 minutes). Overall, 17 patients were approached via the posterior midline (after a prior incision), four medially only, and 28 via combined medial and lateral incisions. In addition to soft-tissue release performed in all 49 patients; 41 patients underwent HO excision. As for collateral ligament repair, direct suture was performed in 14 patients; suture anchor was performed only laterally in eight, only medially in 22, and both laterally and medially in the remaining five. No intraoperative complications were observed.
Postoperative Treatment
Postoperative rehabilitation consisted of three stages: (1) from the first day to 6 weeks, celecoxib (Pfizer Pharmaceuticals LLC, Vega Baja, Puerto Rico; 200 mg orally, twice daily) was prescribed as a precaution against HO [36]. Patients were instructed to lift the upper limb and perform active muscle contraction. Early rehabilitation with cryotherapy was administered under close supervision by the same physical therapist (WW): active-assisted-passive cycles of flexion and extension (30 on the first day, increased by 30 per day until 300 were achieved) and forearm rotation exercises with temporary removal of the external fixator (at least twice daily). (2) The hinged external fixator was removed at 6 weeks in the outpatient operating room. This began the second stage, which lasted until the end of the third month. During this stage, in addition to flexion and extension exercises (300 circles daily equally distributed in the morning, afternoon and evening), a systematic forearm-rotation rehabilitation program was initiated (twice in the morning, afternoon and evening, respectively) at home with the help of family members, who were taught the rehabilitation protocol during the first stage. In our experience, it is not difficult for patients and family members to understand and complete the rehabilitation. If they had any questions, they were asked to visit the outpatient clinic or contact us by telephone at any time. (3) Continued exercises (at least 30 minutes in the morning, afternoon and evening, respectively, which could be separated into several parts) were prescribed in the third stage, lasting for at least 1 year, and weightbearing exercises were encouraged, starting with 1 kg, under supervision. Patients’ rehabilitation progress was followed up at 6 weeks, 3 months, and 1 year postoperatively in the outpatient clinic.
Data Collection
Patient medical records were reviewed from by the authors (ZS, HC, JR, JL) via an electronic database. Data included patient demographics, history of injury and treatment, operative details, outcomes, and complications were collected for all 49 patients included, which were all evaluated by the Elbow Dysfunction Clinical Team in our hospital led by one of the investigators (CF). Motion was measured with a handheld goniometer, and forearm rotation was assessed using a handheld pencil with the elbow at 90° of flexion. We used the following: MEPI and DASH to evaluate elbow function, SF-36 for quality of life, and patient-rated VAS questionnaire from 0 to 10 for pain, Amadio rating scale [1] and Dellon classification [8] for ulnar nerve function. Among these, the MEPI is the most widely used elbow functional assessment, whose results are classified into four categories: excellent, 90–100; good, 75–89; fair, 60–74; and poor, 0–59. The DASH is a valid and responsive scoring system that assesses the disability of the upper extremity, with higher scores represent greater severity. The SF-36 is a measure of health status with higher scores represent better quality. The Dellon classification differentiates changes of the ulnar nerve, including sensory (paresthesia, vibratory perception, and 2-point discrimination) and motor symptoms (muscle weakness and atrophy). The Amadio score also demonstrates ulnar nerve function by assessing the status of pain, weakness, and numbness on a scale from 0 to 9 points, with higher scores representing better function. Hastings and Graham [11] proposed a radiographic and clinical classification, distinguishing three classes of elbow HO: Grade 1, no functional limitation; Grade 2A, limited flexoextension; Grade 2B, limited pronosupination; Grade 2C, 2A combined with 2B; Grade 3, ankylosis. Complications such as new-onset or exacerbated nerve symptoms, recurrent HO, elbow instability, wound infection, and pin-related complications were also recorded. To identify risk factors that might influence medium-term elbow motion recovery, such as disease duration, tobacco use, and initial fracture pattern, we divided the medium-term ROM into two groups: ROM ≤ 120° (n = 9) and ROM > 120° (n = 40), based on the modern functional ROM (flexion of 140° - extension of 20° = 120°) reported by Sardelli et al. [30].
Statistical Analysis
Continuous data are presented as mean ± SD (range) when they were normally distributed; otherwise, the median and interquartile range are reported. Categoric data are presented as number and percentages. Independent- or paired-samples T-test, or Wilcoxon signed rank or Mann-Whitney tests were used to assess continuous data such as ROM and followup time. We used the Kruskal-Wallis, Fisher’s exact, or Pearson χ2 test to compare qualitative data, such as the Dellon classification and sex. Univariate analysis was used to assess the association between different factors such as disease duration and tobacco use and medium-term ROM recovery. Multivariate ordinal regression was then performed to control for confounding effects. Associated p values < 0.05 were considered indicative of a statistically significant between-group difference. Statistical analysis was performed with IBM SPSS 22.0 software (IBM Corp, Armonk, NY, USA).
Results
Mean elbow ROM before arthrolysis was 27° ± 20°, and this increased to an average of 131° ± 11° (mean difference, 104°; 95% CI, 98°–111°; p < 0.001) at the final followup after release. The proportion of patients with functional ROM before surgery improved from 0% (0 of 49) to 98% (48 of 49) after surgery (odds ratio 49; 95% CI, 7–341; p < 0.001). The total forearm rotational arc increased from a preoperative mean of 115° ± 59° to a postoperative mean of 145° ± 36° (mean difference, 30°; 95% CI, 17°–43°; p < 0.001).
The mean MEPI increased from 54 ± 12 preoperatively to 95 ± 7 postoperatively (mean difference, 41 points; 95% CI, 37–45 points; p < 0.001). The results were graded as excellent in 36 patients and good in 13, with none fair or poor (Fig. 2). The mean DASH (scored inversely) improved from 48 ± 17 to 8 ± 8 points (mean difference, 40 points; 95% CI, 34–45 points; p < 0.001). The physical and mental SF-36 improved from 46 ± 11 and 43 ± 14 preoperatively to 81 ± 12 and 80 ± 9 points at final followup (mean difference, 35 and 37 points; 95% CI, 30–40 and 32–42 points; both p < 0.001), respectively. The mean preoperative and postoperative VAS pain score was 2.5 ± 2.4 and 0.4 ± 0.8 points (mean difference, 2.1 points; 95% CI, 1.5–2.7 points; p < 0.001). At the last followup, 11 patients complained of mild pain that did not hamper daily activities, and one patient complained of constant but mild pain in labor-intensive work. Preoperative ulnar-nerve symptoms occurred in 14 patients: Dellon [8] Grade 1 (mild, n = 9), Grade 2 (moderate, n = 2), and Grade 3 (severe, n = 3); and also in 14 at the last followup: three in Grade 2 and eleven in Grade 1(Fig. 3) The mean Amadio score [1] for these 49 patients increased from 7.8 ± 1.9 to 8.4 ± 0.8 points (mean difference, 0.6 points; 95% CI, 0.2–1.1 points; p = 0.004), with an effect size of 0.43 and a standardized response mean of 0.44 by distribution-based approaches for this difference of 0.6 points [16, 26].
Fig. 2.
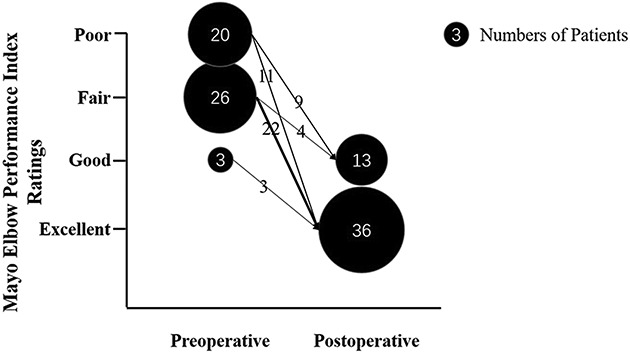
The improvement of preoperative to postoperative Mayo Elbow Performance Index Ratings for elbow function is shown here.
Fig. 3.
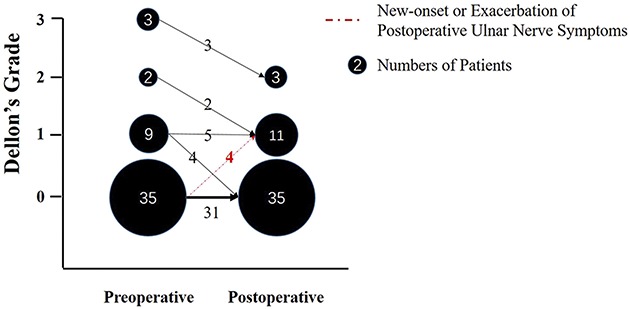
The improvement of preoperative to postoperative Dellon’s Grade for ulnar nerve symptoms is shown here.
A total of 18% (nine of 49 patients) developed complications, including new-onset or exacerbated nerve symptoms (four patients), recurrent heterotopic ossification (two patients), and pin-related infections (three patients). No patients underwent additional surgery for any of these complications. In detail, apart from the four patients who developed ulnar nerve complications, no patient was found to have new-onset or exacerbated radial or median nerve symptoms postoperatively, and all complained of only mild-to-moderate numbness on an infrequent basis that did not affect daily life. There were two cases of recurrent HO classified as Hastings [11] Grade 1 (did not affect elbow movement) and Grade 2A (affected extension of 35°, and was acceptable to the patient). Three patients developed pin-related infections, which all resolved with careful pin care and oral/intravenous antibiotics alone. No other complications were reported.
Examining the two groups divided by the medium-term ROM (≤ 120°, n = 9; > 120°, n = 40) and after controlling for potential confounding variables such as disease duration and tobacco use, we found tobacco use was the only factor independently associated with poorer mid-term ROM recovery (odds ratio, 9; 95% CI, 2-47; p = 0.009). Disease duration was found not to be an independent factor (p = 0.979) and no other demographic, disease, or surgical characteristics were predictive factors.
Discussion
The elbow is more susceptible to loss of motion after trauma than any other joint due to both soft tissue and bony factors [9, 12, 25]. Open arthrolysis often is performed for posttraumatic elbow stiffness if the lost function does not improve with nonoperative therapy. Numerous articles over recent decades have reported the short-term (< 5 years) benefits of this procedure [3, 7, 10, 13, 14, 29, 39-41, 43, 46]; however, the midterm results of this procedure and factors that may limit recovery have not been widely studied. In this study, we evaluated retrospectively a total of 49 patients with severe elbow stiffness (ROM ≤ 60°) at a mean followup period of 69 months (range, 62–83 months). Satisfactory medium-term results were found for open arthrolysis with hinged external fixator in patients who had severe posttraumatic elbow stiffness. We believe that appropriate management of the tethering and block factors that affect elbow motion while maintaining a strict and systematic postoperative rehabilitation program are the core steps. Additionally, the importance of preoperative discontinuation of tobacco use is emphasized.
Limitations
There are a number of limitations to our study. The study is retrospective, so there may have been selection bias, but we followed consistent indications for surgery during the study period, and carefully defined our inclusion and exclusion criteria so the reader can tell to which patients our findings best apply. Also, there is a low overall prevalence of elbow stiffness. The relative heterogeneity of the case series and the relatively low number of patients analyzed are therefore limitations of this study; we did not include patients with nonunions or malunions, and these diagnoses may certainly result in elbow stiffness. Still, our series represents a large group of patients who have undergone the procedure and been followed for 5 years or longer. The low number of patients may also affect the results of multivariate analysis, as some of the no-difference findings may indeed prove to be associated with ROM recovery in larger studies. Third, the use of a hinged external fixator for all patients in our series may also be considered a limitation. Though the techniques of applying the fixator and its effectiveness were described in our previous studies [20, 39, 43, 46], a matched cohort study may better determine its value in the future. Another limitation was our inability, due to partial loss of short-term followup medical records in the electronic database, to identify if there were any declines in clinical outcomes between the short-term (< 5 years) and the medium-term (≥ 5 years). If the improvement in short-term outcomes is maintained, long-term (≥ 10 years) benefits could more reasonably be predicted in the future. Fifth, the measurement of pre- and postoperative ROM for each patient was performed by a doctor from the Elbow Dysfunction Clinical Team each time, and inter- and intraobserver reliability were not tested, which might favor detection bias. Finally, nearly 20% of the patients (49) were excluded for loss to followup or because the patient declined to participate (nine patients), which could have led to transfer bias if those that were lost had poorer ROM or additional complications.
Improvements in ROM
In this study, 49 patients followed for a minimum of 5 years had improvements in their elbow motion, with a mean elbow ROM improvement from 27° preoperatively to 131° postoperatively and forearm rotational arc increasing from 115° preoperatively to 145° postoperatively. A large number of articles over recent decades have reported the benefits of open arthrolysis for posttraumatic elbow stiffness [3, 7, 10, 13, 14, 29, 39-41, 43, 46], however, almost all of them reported short-term (< 5 years) outcomes. The only article reporting medium-term (> 5 years) results retrospectively described 25 patients with a mean followup time of 7.8 years (range, 5–10.8 years) [32]. They found a ROM improvement from 55° to 105° at 1-year followup, which increased slightly at the final followup to 110° (p = 0.12). Whether hinged external fixation improves ROM after contracture release remains controversial. Some authors avoid routine application due to pin-related complications such as infections, loosening and breakage; while others advocate its use for severe contractures and note satisfactory improvement at followup [5, 13, 15, 28, 46]. Besides the advantages of maintaining elbow stability and improving the efficacy of daily rehabilitation, many clinical rationales justify its use: resisting rotatory, shearing, and varus-valgus force; and relieving the pressure on ulnohumeral and radiohumeral joints. An average ROM gain of 88° was reported with the use of external fixation in other centers [15, 28], which was higher than the mean of 51° noted with open arthrolysis alone [13], though with a higher complication rate. In another systematic review [5] involving 810 patients in 28 studies, the authors found that the difference in the total complication rate between the patients treated with and without hinged external fixation was not significant (p = 0.177). Actually, these risks could be controlled under careful manipulation by surgeons. In our previous study, an improvement was noted in flexion-extension arc (from 27° to 126°) after applying a distal radius-positioned hinged external fixator for 38 severe stiff elbows with a mean followup of 31 months. Pin-related infection occurred in two patients and no other fixation-related complications were reported [46]. We chose the radial facet of the distal radius instead of the middle ulna for the distal part of fixator for several reasons: First, the distal radius is much thicker and stronger than the middle ulna for pin placement, while the ulna is more susceptible to fractures during passive manipulation during rehabilitation. Second, it is less affected by elbow movement during rehabilitation, as radius pin sites are distal to the released elbow. Third, less muscle-mass injury occurs with less likelihood of adhesions, as distal radius pin sites avoid forearm muscles. Last, it is more convenient for surgeons to place the pin here.
Outcomes Scores
Patients in this study universally improved on all of the outcomes scores measuring elbow function, life quality, pain, and ulnar nerve function. Although life quality assessments have been carried out after various orthopaedic treatments [4, 31], few studies have focused on the assessment of elbow arthrolysis. An improvement in health status (physical SF-36, from 39 to 49 points; mental SF-36, from 49 to 54 points) was also reported in a 22-patient study [19]. Moreover, the authors of that study found these improvements did not correlate (physical SF-36, p = 0.52; mental SF-36, p = 0.42) with improvement in elbow motion. Our results on these measures also compare favorably with other reports. In the only other article reporting medium-term results, the mean MEPI increased from a preoperative level of 65 to 85 points at the last followup, and the pain level decreased from a mean of 4.5 on the VAS to 2.5 [32]. A range from 89 to 96 points of improvement in the MEPI at followup was also reported in other studies with hinged external fixation for severe stiffness [15, 28, 46]. The ulnar nerve function calculated by Amadio scores [1] improved only a mean of 0.6 points at followup in our series, and both effect size (0.43) and standardized response mean (0.44) were less than 0.5 (low responsiveness), which likely means this difference of 0.6 points is not clinically important [16, 26].
Complications and Factors Associated with Poor ROM
The prevalence of complications in this study was 18% (nine of 49). Among these, four of 49 patients (8%) reported new-onset nerve symptoms with mild-to-moderate numbness that did not affect daily life. This is similar to the mean level of 8.6% reported in a systematic review [5]. Iatrogenic injury during surgery, increased nerve length, and intraneural pressure associated with improved ROM all contribute to nerve complications, especially delayed-onset ulnar neuropathy [34]. Though a decompression length of > 7 cm and subcutaneous anterior transposition of the nerve are routinely performed, ulnar neuritis may still prove unavoidable [2]. Our previous study retrospectively included 260 patients who underwent routine ulnar nerve transposition during open elbow arthrolysis. A final incidence of ulnar neuritis of 9.2% was reported [6]. Other complications included two of 49 patients (4%) who were discovered to have recurrent HO (Grade 1, did not affect elbow movement; Grade 2A, had an impact on extension of 35° and was acceptable for patient) but neither incurred recurrent stiffness, which is less than the prior systematic review reported mean of 5.6% [5]. Selective COX-2 receptor inhibitors [36] and radiotherapy [24] play important roles in preventing HO formation, and in our study all patients were prescribed celecoxib postoperatively for about 4 to 6 weeks. Our previous study compared 152 patients with and without celecoxib use, and found that celecoxib use was the protective factor (odds ratio, 0.152; p < .001) for HO recurrence and could be an effective and safe option [36]. Finally, only three of 49 patients (6%) reported pin-related complications without any deep wound infection, which was lower than the mean reported 1.6% and 17.4% for wound and pin-related complications respectively in a systematic review [5]. Although contracture severity degree preoperatively, longer operative time, and diabetes were reported to be potential risk factors in that review [5], careful pin and wound care remains paramount, with regional antibiotic prophylaxis showing some promise [42].
After controlling for potential confounding variables such as disease duration and tobacco use, we found that the only factor negatively associated with patients’ recovery of ROM was tobacco use. A lot of attention has been paid recently to the relationship between tobacco use and orthopaedic surgery outcomes, mostly showing negative effects [35]. In experimental studies, fibrosis and adhesions have been reported to have close relationships with smoking through extracellular regulated protein kinases and transforming growth factor-β signaling pathways [17, 33], which have been presumed to play an important role in the development of joint contractures and tendon adhesions [18]. However, the relatively small sample size (only nine patients with ROM ≤ 120°) and the exclusion criteria in our study may affect the results of multivariate analysis, as some of the no-difference findings may indeed be associated with ROM recovery, including obesity [29, 44], glucose metabolism status [37], hypertension, absence of intraoperative anterior ulnar nerve transposition [29], initial injury type, articular-surface damage, and coma [7], as has been reported by other authors. Among these factors, some authors assumed that soft tissue contracture involving the capsule and surrounding musculature resulting from prolonged duration of stiffness might contribute to poor results and to the formation of heterotopic bone itself [10, 14, 45]; other authors did not observe this [3]. Persistent postoperative ulnar nerve neuropathy was also reported to be a strong predictor of poor outcome after elbow contracture release [10, 27].
Conclusion
Satisfactory medium-term results were found for open arthrolysis with hinged external fixation in patients who had severe posttraumatic elbow stiffness, with increased elbow ROM, improved function, quality of life, and pain relief. We believe that appropriately managing the tethering and block factors that affect elbow motion intraoperatively, while stressing an aggressive and systematic postoperative rehabilitation program are the core steps to this procedure. Preoperative discontinuation of tobacco use should also be stressed. Further research with a larger population from multiple clinical centers in a prospective fashion will help to determine the importance of additional risk factors and the value of and refined indications for hinged external fixation.
Acknowledgments
We thank the personnel from the Elbow Dysfunction Clinical Team, led by Prof. Cunyi Fan, for participating in the patient and data collection. This study was supported by the Department of Orthopaedics from Shanghai Sixth People’s Hospital East Affiliated to Shanghai University of Medicine & Health Sciences.
Footnotes
The institution of one or more of the authors (CF) has received, during the study period, funding from Project of Key Discipline Group of Shanghai Pudong New Area Health and Family Planning Commission (PWZxq2017-03), Three-year Action Plan of Clinical Skills and Innovation of Shanghai Hospital Development Center (16CR3029A), and Project of Medical Guidance of Foundation of Shanghai Committee of Science and Technology (17411966900).
Each author certifies that neither he or she, nor any member of his or her immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution waived approval for the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Amadio PC. Anatomical basis for a technique of ulnar nerve transposition. Surg Radiol Anat . 1986;8:155-161. [DOI] [PubMed] [Google Scholar]
- 2.Blonna D, Wolf JM, Fitzsimmons JS, O'Driscoll SW. Prevention of nerve injury during arthroscopic capsulectomy of the elbow utilizing a safety-driven strategy. J Bone Joint Surg Am . 2013;95:1373-1381. [DOI] [PubMed] [Google Scholar]
- 3.Breborowicz M, Lubiatowski P, Dlugosz J, Ogrodowicz P, Wojtaszek M, Lisiewicz E, Zygmunt A, Romanowski L. The outcome of open elbow arthrolysis: comparison of four different approaches based on one hundred cases. Int Orthop . 2014;38:561-567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Briani RV, Ferreira AS, Pazzinatto MF, Pappas E, De Oliveira Silva D, Azevedo FM. What interventions can improve quality of life or psychosocial factors of individuals with knee osteoarthritis? A systematic review with meta-analysis of primary outcomes from randomised controlled trials. Br J Sports Med . 2018;52:1031-1038. [DOI] [PubMed] [Google Scholar]
- 5.Cai J, Wang W, Yan H, Sun Y, Chen W, Chen S, Fan C. Complications of open elbow arthrolysis in post-traumatic elbow stiffness: a systematic review. PLoS One . 2015;10:e0138547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cai J, Zhou Y, Chen S, Sun Y, Yuanming O, Ruan H, Fan C. Ulnar neuritis after open elbow arthrolysis combined with ulnar nerve subcutaneous transposition for post-traumatic elbow stiffness: outcome and risk factors. J Shoulder Elbow Surg . 2016;25:1027-1033. [DOI] [PubMed] [Google Scholar]
- 7.Chen S, Liu J, Cai J, Zheng W, Li Z, Chen W, Fan C. Results and outcome predictors after open release of complete ankylosis of the elbow caused by heterotopic ossification. Int Orthop. 2017;41:1627-1632. [DOI] [PubMed] [Google Scholar]
- 8.Dellon AL. Review of treatment results for ulnar nerve entrapment at the elbow. J Hand Surg Am . 1989;14:688-700. [DOI] [PubMed] [Google Scholar]
- 9.Dunham CL, Castile R, Havlioglu N, Chamberlain AM, Lake SP. Temporal patterns of motion in flexion-extension and pronation-supination in a rat model of posttraumatic elbow contracture. Clin Orthop Relat Res . 2018;476:1878-1889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haglin JM, Kugelman DN, Christiano A, Konda SR, Paksima N, Egol KA. Open surgical elbow contracture release after trauma: results and recommendations. J Shoulder Elbow Surg. 2018;27:418-426. [DOI] [PubMed] [Google Scholar]
- 11.Hastings H, 2nd, Graham TJ. The classification and treatment of heterotopic ossification about the elbow and forearm. Hand Clin . 1994;10:417-437. [PubMed] [Google Scholar]
- 12.Hildebrand KA, Zhang M, Befus AD, Salo PT, Hart DA. A myofibroblast-mast cell-neuropeptide axis of fibrosis in post-traumatic joint contractures: an in vitro analysis of mechanistic components. J Orthop Res . 2014;32:1290-1296. [DOI] [PubMed] [Google Scholar]
- 13.Kodde IF, van Rijn J, van den Bekerom MP, Eygendaal D. Surgical treatment of post-traumatic elbow stiffness: a systematic review. J Shoulder Elbow Surg. 2013;22:574-580. [DOI] [PubMed] [Google Scholar]
- 14.Koh KH, Lim TK, Lee HI, Park MJ. Surgical treatment of elbow stiffness caused by post-traumatic heterotopic ossification. J Shoulder Elbow Surg. 2013;22:1128-1134. [DOI] [PubMed] [Google Scholar]
- 15.Kulkarni GS, Kulkarni VS, Shyam AK, Kulkarni RM, Kulkarni MG, Nayak P. Management of severe extra-articular contracture of the elbow by open arthrolysis and a monolateral hinged external fixator. J Bone Joint Surg Br. 2010;92:92-97. [DOI] [PubMed] [Google Scholar]
- 16.Leopold SS, Porcher R. Editorial: The Minimum Clinically Important Difference-the least we can do. Clin Orthop Relat Res. 2017;475:929-932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li D, Hu J, Wang T, Zhang X, Liu L, Wang H, Wu Y, Xu D, Wen F. Silymarin attenuates cigarette smoke extract-induced inflammation via simultaneous inhibition of autophagy and ERK/p38 MAPK pathway in human bronchial epithelial cells. Sci Rep. 2016;6:37751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li F, Liu S, Fan C. Lentivirus-mediated ERK2 siRNA reduces joint capsule fibrosis in a rat model of post-traumatic joint contracture. Int J Mol Sci. 2013;14:20833-20844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lindenhovius AL, Doornberg JN, Ring D, Jupiter JB. Health status after open elbow contracture release. J Bone Joint Surg Am . 2010;92:2187-2195. [DOI] [PubMed] [Google Scholar]
- 20.Liu S, Fan CY, Ruan HJ, Li FF, Tian J. Combination of arthrolysis by lateral and medial approaches and hinged external fixation in the treatment of stiff elbow. J Trauma. 2011;70:373-376. [DOI] [PubMed] [Google Scholar]
- 21.Mansat P, Morrey BF. The column procedure: a limited lateral approach for extrinsic contracture of the elbow. J Bone Joint Surg Am . 1998;80:1603-1615. [PubMed] [Google Scholar]
- 22.Morrey BF. Post-traumatic contracture of the elbow. Operative treatment, including distraction arthroplasty. J Bone Joint Surg Am . 1990;72:601-618. [PubMed] [Google Scholar]
- 23.Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63:872-877. [PubMed] [Google Scholar]
- 24.Ploumis A, Belbasis L, Ntzani E, Tsekeris P, Xenakis T. Radiotherapy for prevention of heterotopic ossification of the elbow: a systematic review of the literature. J Shoulder Elbow Surg. 2013;22:1580-1588. [DOI] [PubMed] [Google Scholar]
- 25.Ranganathan K, Loder S, Agarwal S, Wong VW, Forsberg J, Davis TA, Wang S, James AW, Levi B. Heterotopic ossification: basic-science principles and clinical correlates. J Bone Joint Surg Am. 2015;97:1101-1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Revicki D, Hays RD, Cella D, Sloan J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol. 2008;61:102-109. [DOI] [PubMed] [Google Scholar]
- 27.Ring D, Adey L, Zurakowski D, Jupiter JB. Elbow capsulectomy for posttraumatic elbow stiffness. J Hand Surg Am . 2006;31:1264-1271. [DOI] [PubMed] [Google Scholar]
- 28.Ring D, Hotchkiss RN, Guss D, Jupiter JB. Hinged elbow external fixation for severe elbow contracture. J Bone Joint Surg Am. 2005;87:1293-1296. [DOI] [PubMed] [Google Scholar]
- 29.Salazar D, Golz A, Israel H, Marra G. Heterotopic ossification of the elbow treated with surgical resection: risk factors, bony ankylosis, and complications. Clin Orthop Relat Res. 2014;472:2269-2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sardelli M, Tashjian RZ, MacWilliams BA. Functional elbow range of motion for contemporary tasks. J Bone Joint Surg Am. 2011;93:471-477. [DOI] [PubMed] [Google Scholar]
- 31.Shan L, Shan B, Graham D, Saxena A. Total hip replacement: a systematic review and meta-analysis on mid-term quality of life. Osteoarthritis Cartilage. 2014;22:389-406. [DOI] [PubMed] [Google Scholar]
- 32.Sharma S, Rymaszewski LA. Open arthrolysis for post-traumatic stiffness of the elbow: results are durable over the medium term. J Bone Joint Surg Br. 2007;89:778-781. [DOI] [PubMed] [Google Scholar]
- 33.Shin NR, Park JW, Lee IC, Ko JW, Park SH, Kim JS, Kim JC, Ahn KS, Shin IS. Melatonin suppresses fibrotic responses induced by cigarette smoke via downregulation of TGF-beta1. Oncotarget. 2017;8:95692-95703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shin R, Ring D. The ulnar nerve in elbow trauma. J Bone Joint Surg Am. 2007;89:1108-1116. [DOI] [PubMed] [Google Scholar]
- 35.Singh JA. Smoking and outcomes after knee and hip arthroplasty: a systematic review. J Rheumatol . 2011;38:1824-1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sun Y, Cai J, Li F, Liu S, Ruan H, Fan C. The efficacy of celecoxib in preventing heterotopic ossification recurrence after open arthrolysis for post-traumatic elbow stiffness in adults. J Shoulder Elbow Surg. 2015;24:1735-1740. [DOI] [PubMed] [Google Scholar]
- 37.Sun Z, Xiong H, Fan C. Impact of different glucose metabolism status on clinical outcomes of open arthrolysis for post-traumatic elbow stiffness. J Shoulder Elbow Surg. 2018;27:1072-1077. [DOI] [PubMed] [Google Scholar]
- 38.Veltman ES, Doornberg JN, Eygendaal D, van den Bekerom MP. Static progressive versus dynamic splinting for posttraumatic elbow stiffness: a systematic review of 232 patients. Arch Orthop Trauma Surg . 2015;135:613-617. [DOI] [PubMed] [Google Scholar]
- 39.Wang W, Jiang SC, Liu S, Ruan HJ, Fan CY. Stability of severely stiff elbows after complete open release: treatment by ligament repair with suture anchors and hinged external fixator. J Shoulder Elbow Surg. 2014;23:1537-1544. [DOI] [PubMed] [Google Scholar]
- 40.Wang W, Liu S, Jiang SC, Ruan HJ, He N, Fan CY. Limited medial and lateral approaches to treat stiff elbows. Orthopedics . 2015;38:e477-484. [DOI] [PubMed] [Google Scholar]
- 41.Wang W, Zhan YL, Yu SY, Zheng XY, Liu S, Fan CY. Open arthrolysis with pie-crusting release of the triceps tendon for treating post-traumatic contracture of the elbow. J Shoulder Elbow Surg . 2016;25:816-822. [DOI] [PubMed] [Google Scholar]
- 42.Yan H, He J, Chen S, Yu S, Fan C. Intrawound application of vancomycin reduces wound infection after open release of post-traumatic stiff elbows: a retrospective comparative study. J Shoulder Elbow Surg. 2014;23:686-692. [DOI] [PubMed] [Google Scholar]
- 43.Yu S, Chen M, Fan C. Team approach: Elbow contracture due to heterotopic ossification. JBJS Rev . 2017;5. [DOI] [PubMed] [Google Scholar]
- 44.Zheng W, Chen S, Song J, Liu J, Fan C. The influence of body mass index on outcome of open arthrolysis for post-traumatic elbow stiffness. J Shoulder Elbow Surg. 2017;26:809-814. [DOI] [PubMed] [Google Scholar]
- 45.Zheng W, Song J, Sun Z, Liu J, Chen S, Fan C. Effect of disease duration on functional outcomes and complications after arthrolysis in patients with elbow stiffness. J Shoulder Elbow Surg . 2018;27:381-386. [DOI] [PubMed] [Google Scholar]
- 46.Zhou Y, Cai JY, Chen S, Liu S, Wang W, Fan CY. Application of distal radius-positioned hinged external fixator in complete open release for severe elbow stiffness. J Shoulder Elbow Surg. 2017;26:e44-e51. [DOI] [PubMed] [Google Scholar]


