Abstract
Background
The use of traction during hip arthroscopy is commonly used to provide safe joint access and to improve visualization. However, traction during hip arthroscopy has been associated with complications ranging from transient neuropraxias to devastating soft-tissue necrosis. Trendelenburg positioning may be helpful, but the degree to which this is true is not well understood.
Questions/purposes
To determine whether there would be a reduction in perineal pressure at 5°, 10°, and 15° of Trendelenburg compared with baseline (0° of Trendelenburg) while in the modified supine position during hip arthroscopy.
Methods
A consecutive cohort of 50 patients treated with hip arthroscopy by a single, high-volume orthopaedic surgeon was analyzed. There were 30 females and 20 males in this study, with a mean age of 36 ± 16 years (range, 14 to 66 years); mean BMI was 26 kg/m2. In the operating room, patients were placed in the modified supine position on a traction extension table with a well-padded perineal post. A standard blood pressure cuff was secured to the post to measure pressure exerted on the perineum as traction was applied to distract the hip. For each patient, pressure against the perineum was measured at four different positions using a digital level: 0°, 5°, 10°, and 15° of Trendelenburg. These positions were tested in a random order for each patient. Mean pressure was compared within patients under the four-period crossover design using a repeated-measure (mixed) ANOVA model. Examination of the residual error quantile plot showed that the pressure data followed a normal distribution, making the use of a parametric model appropriate. Tests were made for period and order effects.
Results
Compared with baseline (0° or no Trendelenburg) there was a reduction in pressure of 4.4 (15.5%) at 5° of Trendelenburg (p = 0.203), 8 (28%) at 10° of Trendelenburg (p = 0.022) and 13.1 (46%) at 15° (p = 0.006). These results were maintained regardless of the sequence of positions used in each patient (0°, 5°, 10°, 15°).
Conclusions
Trendelenburg positioning of 10° and 15° during hip arthroscopy resulted in decreased perineal pressure compared with the neutral (0°) position. This technique is intended to harness gravity to exert the majority of countertraction while retaining the perineal post as a backup patient stabilizer. Routine introduction of Trendelenburg during hip arthroscopy reduces perineal pressure against the post, which may decrease complications related to traction and perineal pressure. Future studies should assess whether the observed differences in perineal pressure will reduce the frequency of post-related complications after hip arthroscopy.
Level of Evidence
Level II, therapeutic study.
Introduction
Recent studies have reported a dramatic rise in the number of arthroscopic hip procedures performed in the United States [26]. Reports indicate increased usage of between 300% and 500% among patients aged 18 to 64 years from 2005 to 2013 [20, 29]. But with any new medical procedure comes new complications. Because the hip is a constrained ball-and-socket joint with a thick soft-tissue envelope, distraction is used to allow visualization of the central compartment during hip arthroscopy. A traction table, with a perineal post used for countertraction, is commonly used to distract the hip. Post-related complications have been reported ranging from 2% to 30% [8, 13]. Neurovascular injury to the pudendal, sciatic, and perineal nerves [4, 6, 27] as well as compression-related injuries to soft tissue structures such as the labia and scrotum have been described [5, 11, 19, 30]. Factors contributing to traction complications include entrapment of perineal tissue during initial traction, using an unpadded perineal post, and prolonged traction times during surgery [13]. Some studies have noted the amount of traction, not the traction time, as the greatest risk factor for nerve-related injury during hip arthroscopy [30], and a new post-free hip distraction table developed by Mei-Dan et al. [22] has been developed to reduce traction-related complications.
To reduce traction-related complications such as pudendal nerve palsy, Trendelenburg positioning has been used to reduce perineal pressure against the post by harnessing the force of gravity to provide countertraction. However, the effectiveness of this approach has not been well characterized.
We therefore sought to determine whether there would be a reduction in perineal pressure at 5°, 10°, and 15° of Trendelenburg compared with baseline (0° of Trendelenburg) while in the modified supine position during hip arthroscopy.
Patients and Methods
Data were prospectively collected on 50 consecutive patients who underwent hip arthroscopy during January and February 2018. We included all patients who underwent hip arthroscopy in whom we used traction for hip access. Any patient on whom the senior author (BGD) operated was invited to participate in an ongoing registry; any patient who did not consent to have his or her data included in the registry was excluded. During the period in question, randomization of the sequence of Trendelenburg position was part of routine care, and the Institutional Review Board was aware of this. All patients participated in the American Hip Institute Hip Preservation Registry.
Data such as patient demographics, intraoperative findings, and surgical procedures were collected for all patients as part of the registry. There were 30 females and 20 males, and there were 16 left hips operated on and 34 right hips. Mean age was 36 ± 16 years (range, 14 to 66 years), and mean BMI was 26 kg/m2 (Table 1). Mean traction time was 51 minutes (range, 25 to 92 minutes). Most patients underwent labral repair (70%), femoroplasty (98%), and acetabuloplasty (78%). One patient underwent microfracture drilling, and nine (19%) underwent iliopsoas fractional lengthening (Table 2).
Table 1.
Demographics

Table 2.
Intraoperative procedures (number [%])

Perineal pressure was measured for each patient using a digital manometer at different angles of Trendelenburg (0°, 5°, 10°, and 15°). Before study initiation, each patient was randomly assigned to a random sequence of Trendelenburg positions. All data collection received institutional review board approval before initiating this study.
Before surgery, all patients underwent comprehensive physical and radiographic examinations during their clinic appointments. Hips were assessed for ROM [1] and signs of femoroacetabular impingement.
We obtained an MRI or MR arthrogram on all patients before surgery as well as the following series of radiographs: upright and supine AP pelvic, modified Dunn view, and false-profile [9, 25, 31]. We used GE Healthcare’s Picture Archiving and Communication System (GE Healthcare, Fairfield, CT, USA) to obtain various measurements from these radiographs, which illustrated the health and structural anatomy of the hip. Acetabular inclination was measured using the lateral center-edge angle and the anterior center-edge angle; acetabular version was assessed based on crossover and ischial spine signs [16, 17]; the extent of osteoarthritis was recorded based on Tönnis grade; and cam-type impingement was identified by an elevated alpha angle or decreased femoral offset measurement [14].
Surgical Technique
The senior author (BGD) performed all procedures at a tertiary referral center dedicated to hip arthroscopy. Procedures were performed under general endotracheal anesthesia and with the patient positioned supine on a traction extension table with a well-padded perineal post. The operative leg was then prepared and draped sterilely, and manual traction was applied to both legs. To break the suction seal of the joint, the hip was vented using a spinal needle under fluoroscopic guidance.
Before taking the patient to the operating room, a blood pressure cuff (Prestige Medical, Northridge, CA, USA) was wrapped around the perineal post of the Smith & Nephew traction table (Smith & Nephew, London, UK). Durapore Silk Tape (3M, Maplewood, MN, USA) was used to secure the blood pressure cuff to the post, which was then wrapped with cotton undercast padding wrap to ensure a well-padded post. The tube from the blood pressure cuff then was connected to a digital manometer (TPI 621 Dual Differential Input Manometer [TPI Inc, Beaverton, OR, USA]). Using the bulb of the pressure cuff, a standard amount of pressure was introduced into the cuff. This initial introduction of pressure was not precise nor was it measured; although it typically was around 30 mmHg, for purposes of this experiment, it does not matter, since it would be zeroed out on the digital manometer to accurately measure the difference in pressure once traction was applied at each of the Trendelenburg angles we studied.
The pressure valve was closed and the tube was folded onto itself and a hemostat was used to clamp the tube to ensure that no air would leak from the system.
Before the study began, we conducted and validated multiple trials to make sure that no air would leak from the setup because it would reduce final pressure measurements and invalidate this study. In our trials, even at extremes of pressures and for extended periods of time, no decrease in pressure was observed ensuring no air leak. Once a standard pressure was introduced, this would serve as a baseline. As mentioned, this would be zeroed out on the digital manometer. A digital level was used to measure different angles and was fixed to the side of the bed. Once the bed was leveled, the digital level was also zeroed out to serve as the baseline. Once the patient was positioned, sufficient traction was applied so the patient came to rest snugly against the post. After the joint was vented, traction was applied at different Trendelenburg angles in a randomized fashion (0°, 5°, 10°, and 15° of Trendelenburg).
To ensure the same amount of joint distraction at all the desired angles, the amount of distraction was measured as a ratio of joint distraction to the diameter of the femoral head. Measuring along an axis parallel to the pubic symphysis, the maximum distraction and the diameter of the femoral head were measured [cm]. This ratio was calculated for each patient in each Trendelenburg position, and it was used as a check to ensure the same amount of distraction was obtained at different angles given that fluoroscopic magnification would change at different angles. The setup and all the measurements were conducted by the same two individuals and the same three devices were used for all patients to minimize variability.
A standard diagnostic arthroscopy was performed. Labral tears were repaired, partially débrided, or reconstructed using tibialis anterior allograft, depending on the viability of the labral tissue. Acetabuloplasty and femoroplasty were performed under fluoroscopic guidance to correct pincer and cam morphology, respectively. When there was extensive damage, microfracture drilling was performed to stimulate articular cartilage restoration. A recession-type fractional lengthening of the iliopsoas was performed to treat patients with internal snapping hip syndrome. Additional procedures were performed to address a patient’s specific pathology, including ligamentum teres débridement, notchplasty, subspine decompression, loose body removal, trochanteric bursectomy, or gluteus medius repair. Patients with evidence of hip instability, defined by borderline dysplasia or ligamentous laxity, underwent capsular repair or plication, and patients with evidence of stiffness underwent capsular release.
Statistical Analysis
Before study initiation, each patient was randomly assigned to a random sequence of Trendelenburg positions. Mean pressure was compared within patients under the four-period crossover design using a repeated-measure (mixed) ANOVA model. Examination of the residual error quantile plot showed that the pressure data followed a normal distribution, making the use of a parametric model appropriate. Tests were made for period and order effects.
Examination of the residual error quantile plot showed that the pressure data followed a normal distribution, making the use of a parametric model appropriate (Fig. 1).
Fig. 1.
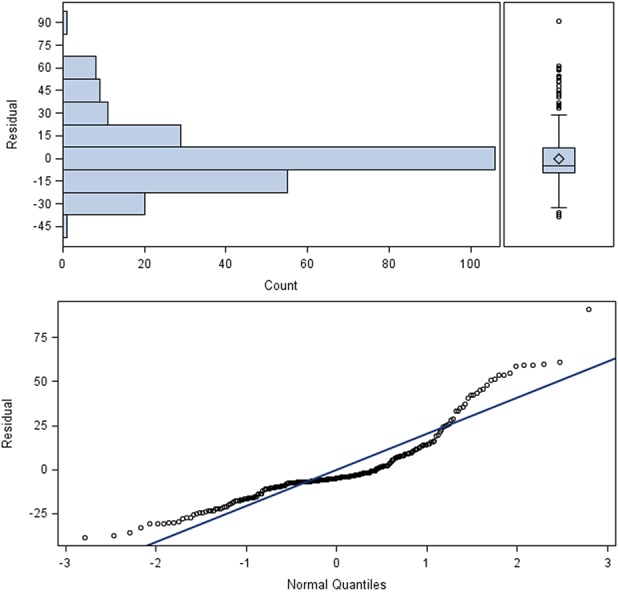
Examination of the residual error quantile plot showed that the pressure data followed a normal distribution, making the use of a parametric model appropriate.
Results
The mean traction pressure at each table position was 28 ± 5 mm Hg, 24 ± 4 mm Hg, 20 ± 4 mm Hg and 15 ± 4 mm Hg at 0°, 5°, 10°, and 15° of Trendelenburg, respectively. Compared with baseline (0° or no Trendelenburg) there was a reduction in pressure of 4.4 (15.5%) at 5° of Trendelenburg (p = 0.203), 8 (28%) at 10° of Trendelenburg (p = 0.022) and 13.1 (46%) at 15° (p = 0.006) (Fig. 2). These results were robust regardless of the sequence of positions used in each patient (0°, 5°, 10°, 15°). This finding demonstrates that the crossover design was successful (Table 3).
Fig. 2.
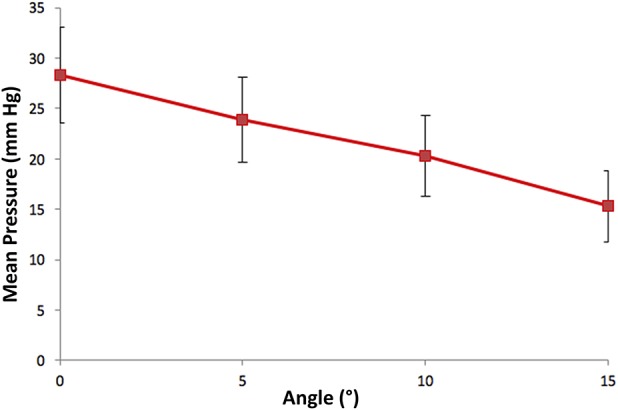
A decrease in pressure (Hg) with bed position at increasing angle of Trendelenburg is shown.
Table 3.
Period and order effect
Discussion
The use of traction during hip arthroscopy is currently used to distract the hip to provide joint access and to improve visualization. However, several studies have reported on traction-related complications ranging from 2% to 30% [8, 13]. In a recent review of 6277 hips among 5535 patients, Gupta et al. [13] documented 285 total complications (4.5%), of which nerve injury accounted for 36% (104 of 285). Those authors [13] recommended Trendelenburg positioning to decrease perineal pressure; however, the efficacy of Trendelenburg positioning to reduce perineal pressure has not been well characterized. We found that Trendelenburg positioning of 10° and 15° each resulted in measurable decrease in perineal pressure 28% and 46%, respectively.
The limitations of this study should be noted. We attempted to reproduce the same amount of joint distraction at all the desired angles of Trendelenburg by measuring the ratio of joint distraction to the diameter of femoral head. All measurements were obtained by the same two individuals (ACL, BGD) to minimize variability. Additionally, differences in patients’ sizes and in the angles of the fluoroscopic beam generate inherent variability. We attempted to minimize this by comparing our intraoperative images to a well-positioned AP pelvis radiograph obtained before surgery, but we acknowledge the presence of variability in measurement. Although this study reports a reduction in perineal pressure at 10° and 15° of Trendelenburg, it is unclear if this would have any clinical significance, and this study does not evaluate any complications that could arise from Trendelenburg positioning.
Because this study does not evaluate the clinical importance of the observed reduction in perineal pressure, nor does it address any potential complications thereof, the clinical importance of this finding is, at this moment, unknown. However, other work suggests that our findings may be important, and certainly others have suggested that minimizing traction force and time may help mitigate traction-related complications during hip arthroscopy. Most authors advocate limiting traction weight to less than 50 pounds [3, 12, 18] with the goal of achieving approximately 1 cm of joint space for access to the central compartment. Studies have also noted 2 hours [6, 15, 21, 28] as the upper limit of total traction time during hip arthroscopy. Experimental studies have determined the vacuum force between the femoral head and acetabulum related to the labral seal to be between 120 and 200 N with distraction forces of 200 pounds (90 kg) necessary for initial distraction [7]. Venting or distension of the joint has been shown to aid in breaking the suction seal and facilitate distraction, reducing these forces to 50 pounds [2, 7].
To avoid post-related complications altogether, several authors have proposed postless traction techniques. In 2007, Merrell et al. [24] described the use of a deflated bean bag contoured around the patient’s flank. Once the patient is secured, the post is removed, and manual traction is applied to both limbs. However, a critique of this technique is the tenuous setup design and multiple areas of potential failures such as tape breakage and distal slippage of the patient. In 2011, Flecher et al. [10] described the use of a skeletal distractor for joint distraction by insertion of threaded pins into the femoral diaphysis and acetabular roof. Although the authors did not report any neurologic complications in a series of 23 patients, there is a potential risk of pin site infection and hardware breakage. More recently, in 2013, Mei-Dan et al. [23] evaluated 170 patients undergoing hip arthroscopy without the use of a perineal post (against the perineum). The patients were placed supine in 15° to 20° of Trendelenburg. The operative limb was positioned with the perineal post 7 to 10 cm distal to the perineum against the medial thigh. Friction generated between the bed and torso during traction allowed for joint distraction without perineal contact. The authors reported no complications related to traction postoperatively. In 2018 Mei-Dan et al. [22] again reported on postless hip arthroscopy, this time without the use of a perineal post. It became quite clear the key to developing this postless technique was the Trendelenburg position, using gravity as a counterforce against applied skeletal traction.
Use of the Trendelenburg position during hip arthroscopy allows for a decrease in pressure exerted on the perineum at 10° and 15° of Trendelenburg compared with neutral (0° of Trendelenburg). This technique is intended to harness gravity to exert the majority of countertraction while retaining the perineal post as a backup patient stabilizer. Routine introduction of Trendelenburg during hip arthroscopy reduces perineal pressure against the post, which may decrease complications related to traction and perineal pressure. Future studies should assess whether the observed differences in perineal pressure will reduce the frequency of post-related complications after hip arthroscopy.
Acknowledgments
We thank Jeffrey Gornbein PhD, for his assistance with statistical analysis.
Footnotes
One of the authors certifies that he (BGD), or a member of his immediate family, has or may receive payments or benefits, during the study period, in an amount of USD 10,000–USD 100,000 from Arthrex Inc (Naples, FL, USA); in an amount of USD 100,001–USD 1,000,000 from DJO Global Inc (Vista, CA, USA); in an amount of USD 10,000–USD 100,000 from Medacta International (Chicago, IL, USA); in an amount of less than USD 10,000 from Orthomerica Products Inc (Orlando, FL, USA); in an amount of less than USD 10,000 from Pacira Pharmaceuticals Inc (Parsippany-Troy Hills, NJ, USA); and in an amount of USD 100,001–USD 1,000,000 from Stryker Corp (Kalamazoo, MI, USA).
One of the authors certifies that he (ACL), or a member of his immediate family, has or may receive payments or benefits, during the study period, in an amount of USD 10,000–USD 100,000 from Arthrex Inc (Naples, FL, USA); in an amount of less than USD 10,000 from Medwest Associates (Chicago, IL, USA); in an amount of USD 10,000–USD 100,000 from Smith & Nephew, Inc (London, UK); and in an amount of less than USD 10,000 from Stryker Corp (Kalamazoo, MI, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the American Hip Institute, Des Plaines, IL, USA.
References
- 1.Byrd JT. Physical Examination. In: Byrd JT, ed. Operative Hip Arthroscopy. New York: Springer; 2005:36–50. [Google Scholar]
- 2.Byrd JW. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10:275–280. [DOI] [PubMed] [Google Scholar]
- 3.Byrd JW, Chern KY. Traction versus distension for distraction of the joint during hip arthroscopy. Arthroscopy. 1997;13:346–349. [DOI] [PubMed] [Google Scholar]
- 4.Byrd JW, Pappas JN, Pedley MJ. Hip arthroscopy: an anatomic study of portal placement and relationship to the extra-articular structures. Arthroscopy. 1995;11:418–423. [DOI] [PubMed] [Google Scholar]
- 5.Callanan I, Choudhry V, Smith H. Perineal sloughing as a result of pressure necrosis from the traction post during prolonged bilateral femoral nailing. Injury. 1994;25:472. [DOI] [PubMed] [Google Scholar]
- 6.Clarke MT, Arora A, Villar RN. Hip arthroscopy: complications in 1054 cases. Clin Orthop Relat Res . 2003:84–88. [DOI] [PubMed] [Google Scholar]
- 7.Dienst M, Seil R, Gödde S, Brang M, Becker K, Georg T, Kohn D. Effects of traction, distension, and joint position on distraction of the hip joint: an experimental study in cadavers. Arthroscopy . 2002;18:865–871. [DOI] [PubMed] [Google Scholar]
- 8.Dippmann C, Thorborg K, Kraemer O, Winge S, Hölmich P. Symptoms of nerve dysfunction after hip arthroscopy: an under-reported complication? Arthroscopy . 2014;30:202–207. [DOI] [PubMed] [Google Scholar]
- 9.Dunn DM. Anteversion of the neck of the femur; a method of measurement. J Bone Joint Surg Br . 1952;34-B:181–186. [DOI] [PubMed] [Google Scholar]
- 10.Flecher X, Dumas J, Argenson J-N. Is a hip distractor useful in the arthroscopic treatment of femoroacetabular impingement? Orthop Traumatol Surg Res. 2011;97:381–388. [DOI] [PubMed] [Google Scholar]
- 11.Frandsen L, Lund B, Grønbech Nielsen T, Lind M. Traction-related problems after hip arthroscopy. J Hip Preserv. Surg. 2017;4:54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glick JM, Sampson TG, Gordon RB, Behr JT, Schmidt E. Hip arthroscopy by the lateral approach. Arthroscopy . 1987;3:4–12. [DOI] [PubMed] [Google Scholar]
- 13.Gupta A, Redmond JM, Hammarstedt JE, Schwindel L, Domb BG. Safety measures in hip arthroscopy and their efficacy in minimizing complications: a systematic review of the evidence. Arthroscopy . 2014;30:1342–1348. [DOI] [PubMed] [Google Scholar]
- 14.Harris MD, Kapron AL, Peters CL, Anderson AE. Correlations between the alpha angle and femoral head asphericity: Implications and recommendations for the diagnosis of cam femoroacetabular impingement. Eur J Radiol . 2014;83:788–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ilizaliturri VM. Complications of arthroscopic femoroacetabular impingement treatment: a review. Clin Orthop Relat Res . 2009;467:760–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign.” J Orthop Res . 2007;25:758–765. [DOI] [PubMed] [Google Scholar]
- 17.Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis : a new sign for acetabular retroversion. Clin Orthop Relat Res . 2008;466:677–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21:1496–1504. [DOI] [PubMed] [Google Scholar]
- 19.Lo Y-P, Chan Y-S, Lien L-C, Lee MSS, Hsu K-Y, Shih C-H. Complications of hip arthroscopy: analysis of seventy three cases. Chang Gung Med J . 2006;29:86–92. [PubMed] [Google Scholar]
- 20.Maradit Kremers H, Schilz SR, Van Houten HK, Herrin J, Koenig KM, Bozic KJ, Berry DJ. Trends in utilization and outcomes of hip arthroscopy in the United States between 2005 and 2013. J Arthroplasty. 2017;32:750–755. [DOI] [PubMed] [Google Scholar]
- 21.Mason JB, McCarthy JC, O’Donnell J, Barsoum W, Mayor MB, Busconi BD, Krebs VE, Owens BD. Hip arthroscopy: surgical approach, positioning, and distraction. Clin Orthop Relat Res . 2003:29–37. [DOI] [PubMed] [Google Scholar]
- 22.Mei-Dan O, Kraeutler MJ, Garabekyan T, Goodrich JA, Young DA. Hip distraction without a perineal post: a prospective study of 1000 hip arthroscopy cases. Am J Sports Med . 2018;46:632–641. [DOI] [PubMed] [Google Scholar]
- 23.Mei-Dan O, McConkey MO, Young DA. Hip arthroscopy distraction without the use of a perineal post: prospective study. Orthopedics. 2013;36:e1-5. [DOI] [PubMed] [Google Scholar]
- 24.Merrell G, Medvecky M, Daigneault J, Jokl P. Hip arthroscopy without a perineal post: a safer technique for hip distraction. Arthroscopy. 2007;23:107.e1–3. [DOI] [PubMed] [Google Scholar]
- 25.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res . 2006;445:181–185. [DOI] [PubMed] [Google Scholar]
- 26.Montgomery SR, Ngo SS, Hobson T, Nguyen S, Alluri R, Wang JC, Hame SL. Trends and Demographics in Hip Arthroscopy in the United States. Arthroscopy. 2013;29:661–665. [DOI] [PubMed] [Google Scholar]
- 27.Park M-S, Yoon S-J, Kim Y-J, Chung W-C. Hip arthroscopy for femoroacetabular impingement: the changing nature and severity of associated complications over time. Arthroscopy. 2014;30:957–963. [DOI] [PubMed] [Google Scholar]
- 28.Sampson TG. Complications of hip arthroscopy. Clin Sports Med . 2001;20:831–835. [DOI] [PubMed] [Google Scholar]
- 29.Sing DC, Feeley BT, Tay B, Vail TP, Zhang AL. Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy . 2015;31:2307-2313.e2. [DOI] [PubMed] [Google Scholar]
- 30.Telleria JJM, Safran MR, Harris AHS, Gardi JN, Glick JM. Risk of sciatic nerve traction injury during hip arthroscopy—is it the amount or duration? An intraoperative nerve monitoring study. J Bone Joint Surg Am . 2012;94:2025–2032. [DOI] [PubMed] [Google Scholar]
- 31.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am . 1999;81:1747–1770. [DOI] [PubMed] [Google Scholar]



