Abstract
Background
The complex interrelationship among physical health, mental health, and social health has gained the attention of the medical community in recent years. Poor social health, also called social deprivation, has been linked to more disease and a more-negative impact from disease across a wide variety of health conditions. However, it remains unknown how social deprivation is related to physical and mental health in patients presenting for orthopaedic care.
Questions/purposes
(1) Do patients living in zip codes with higher social deprivation report lower levels of physical function and higher levels of pain interference, depression, and anxiety as measured by Patient-Reported Outcomes Measurement Information System (PROMIS) at initial presentation to an orthopaedic provider than those from less deprived areas; and if so, is this relationship independent of other potentially confounding factors such as age, sex, and race? (2) Does the relationship between the level of social deprivation of a patient’s community and that patient’s physical function, pain interference, depression, and anxiety, as measured by PROMIS remain consistent across all orthopaedic subspecialties? (3) Are there differences in the proportion of individuals from areas of high and low levels of social deprivation seen by the various orthopaedic subspecialties at one large, tertiary orthopaedic referral center?
Methods
This cross-sectional evaluation analyzed 7500 new adult patients presenting to an orthopaedic center between August 1, 2016 and December 15, 2016. Patients completed PROMIS Physical Function-v1.2, Pain Interference-v1.1, Depression-v1.0, and Anxiety-v1.0 Computer Adaptive Tests. The Area Deprivation Index, a composite measure of community-level social deprivation, based on multiple census metrics such as income, education level, and housing type for a given nine-digit zip code was used to estimate individual social deprivation. Statistical analysis determined the effect of disparate area deprivation (based on most- and least-deprived national quartiles) for the entire sample as well as for patients categorized by the orthopaedic subspecialty providing care. Comparisons of PROMIS scores among these groups were based on an MCID of 5 points for each PROMIS domain (Effect size 0.5).
Results
Patients living in zip codes with the highest levels of social deprivation had worse mean scores across all four PROMIS domains when compared with those living in the least-deprived quartile (physical function 38 +/- 9 versus 43 +/- 9, mean difference 4, 95% CI, 3.7–5.0; p < 0.001; pain interference 64 +/- 8 versus 60+/-8, mean difference -4, 95% CI, -4.8 to -3.7; p < 0.001; depression 50+/-11 versus 45+/-8, mean difference -5, 95% CI, -6.0 to -4.5; p < 0.001; anxiety 56+/-11 versus 50 +/-10, mean difference -6, 95% CI, -6.9 to -5.4; p < 0.001). There were no differences in physical function, pain interference, depression, or anxiety PROMIS scores between patients from the most- and least-deprived quartiles who presented to the subspecialties of spine (physical function, mean 35+/-7 versus 35+/-7; p = 0.872; pain interference, 67+/-7 versus 66+/-7; p = 0.562; depression, 54+/-12 versus 51 +/-10; p = 0.085; and anxiety, 60+/-11 versus 58 +/-9; p = 0.163), oncology (physical function, mean 33+/-9 versus 38 +/-13; p = 0.105; pain interference, 68+/-9 versus 64+/-10; p = 0.144; depression, 51+/-10 versus 52+/-13; p = 0.832; anxiety, 59+/-11 versus 59+/-10 p = 0.947); and trauma (physical function, 35+/-11 versus 32+/-10; p = 0.268; pain interference, 66+/-7 versus 67+/-6; p = 0.566; depression, 52+/-12 versus 53+/-11; p = 0.637; and anxiety, 59+/-12 versus 60+/-9 versus; p = 0.800). The social deprivation-based differences in all PROMIS domains remained for the subspecialties of foot/ankle, where mean differences ranged from 3 to 6 points on the PROMIS domains (p < 0.001 for all four domains), joint reconstruction where mean differences ranged from 4 to 7 points on the PROMIS domains (p < 0.001 for all four domains), sports medicine where mean differences in PROMIS scores ranged from 3 to 5 between quartiles (p < 0.001 for all four domains), and finally upper extremity where mean differences in PROMIS scores between the most- and least-deprived quartiles were five points for each PROMIS domain (p < 0.001 for all four domains). The proportion of individuals from the most- and least-deprived quartiles was distinct when looking across all seven subspecialty categories; only 11% of patients presenting to sports medicine providers and 17% of patients presenting to upper extremity providers were from the most-deprived quartile, while 39% of trauma patients were from the most-deprived quartile (p < 0.001).
Conclusions
Orthopaedic patients must be considered within the context of their social environment because it influences patient-reported physical and mental health as well as has potential implications for treatment and prognosis. Social deprivation may need to be considered when using patient-reported outcomes to judge the value of care delivered between practices or across specialties. Further studies should examine potential interventions to improve the perceived health of patients residing in communities with greater social deprivation and to determine how social health influences ultimate orthopaedic treatment outcomes.
Level of Evidence
Level II, prognostic study.
Introduction
In recent years, an expanding body of evidence has emphasized the inter-relationship between psychologic distress and poor orthopaedic outcomes [7, 18, 20, 25, 31, 32, 36, 37, 53]. However, more broadly across medicine, research suggests that not only are mental and physical health interrelated, but also that social health represents another facet of life, one often outside of the individual’s control, that may influence all other health domains [23]. Increased social deprivation is associated with a greater prevalence of colorectal cancer, cardiac disease, weight gain, musculoskeletal pain as well as increased mortality rates [26, 30, 42, 48, 52]. Additionally, patients living in areas of increased social deprivation report increased levels of depressive symptoms as well as overall lower levels of self-reported well-being [16, 27, 33, 38, 43, 45].
Within the last decade, use of the Patient-Reported Outcomes Measurement Information System (PROMIS) has become increasingly more common as a method of assessing mental and physical health domains in patients, both singly and in groups. PROMIS physical function scores correlate well with traditional orthopaedic patient-reported outcomes, such as the QuickDASH for upper extremity patients and the short Musculoskeletal Assessment form for trauma patients. Various domains of PROMIS have demonstrated effectiveness in orthopaedic patient populations [1, 9, 12, 22, 41, 49, 51], providing an efficient way for orthopaedic physicians to assess patient perceptions regarding their physical and mental health and well-being. PROMIS assessments are not disease- or diagnosis-specific and thus represent a potential consensus measurement system to quantify the relative value of care delivered across medical and surgical specialties.
Although we have made strides in assessing patients’ psychologic well-being, the effect of social deprivation on physical and mental health in orthopaedic patients has not been well defined. A large proportion of orthopaedic care can be viewed as elective, in the sense that it is neither life-saving nor life-prolonging. In light of the potential for serious harm to patients in this setting, it seems appropriate to identify possible barriers to achieving good outcomes, and address them before definitive management. It is therefore critical to understand if and how social health affects patient-reported physical and mental health ratings and where interventions may be needed. Therefore, this study aimed to answer the following questions.
(1) Do patients living in zip codes with higher social deprivation report lower levels of physical function and higher levels of pain interference, depression, and anxiety as measured by PROMIS at initial presentation to an orthopaedic provider than those from less deprived areas; and if so, is this relationship independent of other potentially confounding factors such as age, gender, and race? (2) Does the relationship between the level of social deprivation of a patient’s community and that patient’s physical function, pain interference, depression, and anxiety, as measured by PROMIS remain consistent across all orthopaedic subspecialties? (3) Are there differences in the proportion of individuals from areas of high and low levels of social deprivation seen by the various orthopaedic subspecialties at one large, tertiary orthopaedic referral center?
Patients and Methods
Approval for this study was obtained from our institutional review board with a waiver of informed consent for all patients. This cross-sectional study collected data from 9737 new patient visits to the outpatient offices of a single, tertiary orthopaedic practice. Patients presented to five different clinical sites, two in zip codes with high levels of social deprivation, and three in zip codes with low levels of deprivation. Most patients were seen at two of the sites, one in a zip code of high deprivation, and one in a zip code of low deprivation. All specialty divisions are represented by at least one clinical site in an area of high deprivation, and one in an area of low deprivation, with the exception of trauma, where all clinical sites are in areas of high deprivation. Patients presented to any of the 61 providers in the department, as well as to the resident-run clinic site. Data were collected at the time of the visit for all new adult patients presenting between August 1, 2016 and December 15, 2016.
All adult (18 years of age or older) new patient visits to the practice during this study period were eligible for inclusion. During this study period, the PROMIS completion rate was 91% for all orthopaedic patients with completion of PROMIS Pain Interference and Physical Function required for study inclusion. Patients without a nine-digit zip code matched to their self-reported address or those whose address did not correlate with an Area Deprivation Index (ADI) number such as a PO Box were excluded. For patients presenting as a new patient to multiple providers within our group during the study dates, only the first visit was included with all subsequent visits removed from the data set. After applying all study participation requirements, 7500 patients remained eligible for inclusion (Fig. 1).
Fig. 1.
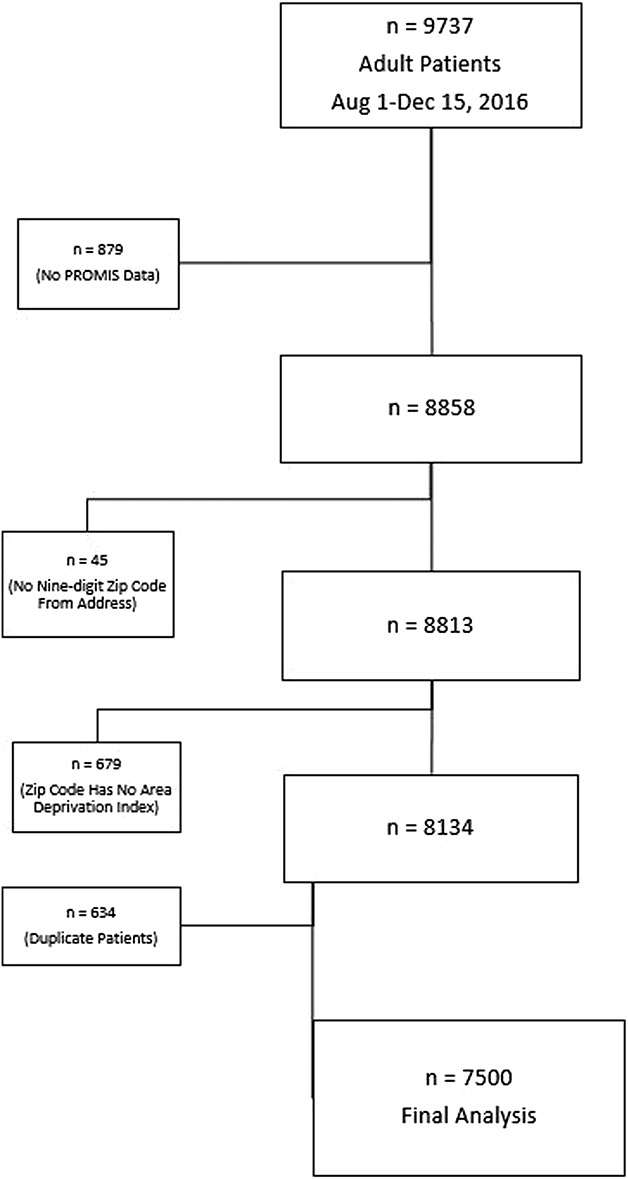
The flowsheet demonstrates patient inclusion and exclusion in the study, resulting in the final number for analysis, 7500.
As part of our institution’s standard practice, all patients completed the PROMIS Physical Function-v1.2, PROMIS Pain Interference-v1.1, PROMIS Depression-v1.0, and PROMIS Anxiety-v1.0 at presentation to their provider. Patients also completed a variety of demographic forms that include self-reported age, gender, race, and home address.
Our institution’s electronic medical record and administrative databases were queried for age, sex, race, home address (including nine-digit zip code), provider visited, and PROMIS Computer Adaptive Test (CAT) scores (pain interference, physical function, depression, and anxiety). Gender was obtained from the medical record and is self-reported as man or woman at the time of registration. Race is similarly self-reported at the time of registration. Patients were categorized as white, black, Asian, or other for study analysis. Home address is self-reported with the nine-digit zip code generated automatically during registration. Using the provider seen, participants were grouped by the orthopaedic subspecialty that provided care (foot/ankle, joint reconstruction [hip and knee], sports medicine, spine, trauma, oncology, upper extremity, and nonoperative providers).
The ADI quantified the social deprivation of each patient’s community according to the nine-digit home zip code. The ADI is a validated measure of social deprivation developed by George Singh that accounts for 17 US Census measures across the domains of poverty, education, housing, and employment, which mirror those used in other countries to measure social deprivation [8, 26, 46, 47]. Assessment of the index validity and reliability are detailed by Singh [47] in his paper describing creation of the ADI. The ADI of each geographic area is determined by the sum of each included socioeconomic factor multiplied by its predetermined factor coefficient; scores are then standardized so that the index mean is 100 with a SD of 20. After standardization, index values range from -53 to 129 with increasing values indicating increasing levels of social deprivation; a patient whose zip code translates to an ADI of 110 is from a more deprived area than someone with an ADI of 20. Socioeconomic disadvantage is a complex entity that indicates a combination of low income, limited education, poor living conditions, and decreased social support. Area deprivation affects both the individual and those around them [26]. Using a composite index such as the ADI, which encompasses multiple domains that contribute to disadvantage, is therefore more robust than choosing a single metric such as income or education to assess social disadvantage [47]. In addition to using each person’s address-based ADI score for analysis, we categorized patients according to established break points defining national quartiles of deprivation to allow for direct comparison between the most- and least-deprived groups of individuals, which is consistent with previous investigations of social deprivation [2, 10, 15, 24, 26, 47, 48]. While socioeconomic position and social status can be studied using a variety of metrics such as individual income, individual education level, or even composite metrics of these individual data points, we have chosen to use a zip-code based metric for deprivation as it serves as a proxy for individual social position while also characterizing the social condition of the surrounding community, which may have a further impact on health [17].
All patients presenting to our institution’s orthopaedic clinics are provided a computer tablet (iPad mini; Apple, Cupertino, CA, USA) at check-in that is preloaded with PROMIS Physical Function-v1.2, PROMIS Pain Interference-v1.1, PROMIS Depression-v1.0, and PROMIS Anxiety-v1.0. PROMIS scores are automatically generated and uploaded into the patient’s electronic health record on module completion. PROMIS CATs are scored such that a score of 50 represents the normative population mean with a SD of 10 [6]. A higher score represents a higher level of a given metric such that a higher physical function score indicates better function, whereas a higher depression score indicates more depression. PROMIS has been well validated in many different patient populations, including a variety of orthopaedic populations [3, 21, 39, 49, 51]. Additionally, the PROMIS CATs, particularly physical function and pain interference, have been compared with multiple orthopaedic legacy measures of pain and function and found to correlate highly, often with less unexplained variance and less floor and ceiling effects than the traditional measures [12, 22, 51]. Pain interference is an assessment that measures how pain impacts an individual’s activities and function as opposed to simply measuring pain magnitude. Thus, pain interference blends elements of pain tolerance, coping, and functional demands.
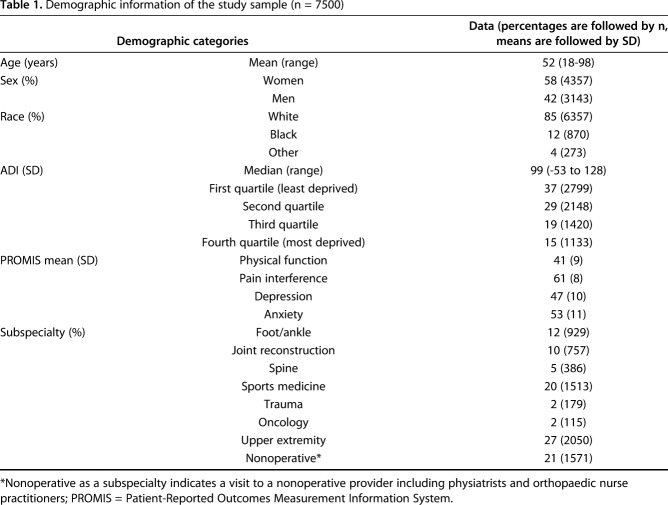
Patient age was widely distributed in our study population (mean, 52 years; range, 18-98 years) and home addresses indicated residence in 33 different states (Table 1). Most patients were white (85%). Area deprivation scores ranged from -53 to 128, a range comparable to the national range (-53 to 129). The median ADI was 99 (30th percentile nationally) indicating more patients from more socially advantaged areas. A total of 2799 patients (37%) were categorized within the least-deprived national quartile, and 1133 patients (15%) were categorized within the most-deprived national quartile.
Table 1.
Demographic information of the study sample (n = 7500)
Statistical Analysis
Univariate descriptive statistics were produced to characterize continuous and categorical variables of interest: patient demographic data, PROMIS scores, ADI frequencies, and the percentage of visits to each subspecialty from the four ADI quartiles. Student’s t-tests compared mean PROMIS scores between individuals in the most- and least-deprived quartiles of the population, similar to other studies of social deprivation in which primary analysis compared the most- and least-deprived groups [26, 30, 42, 47, 48]. An estimated minimal clinically important difference (MCID) of 5 points on PROMIS assessments was used as a conservative proxy for clinically relevant between-group differences based on previous studies that have attempted to define MCID values for PROMIS short forms and CATs in various populations [1, 29, 50, 57]. The same statistical tests were performed to satisfy our secondary aim of comparing the impact of ADI among orthopaedic surgical subspecialties, excluding nonoperative providers. The Kruskal-Wallis test was used to compare the proportions of individuals in the most- and least-deprived quartiles presenting to the different subspecialties with pairwise comparison post hoc analysis using the Dunn-Bonferroni method. One-way analysis of variance was used to compare mean PROMIS scores among the different subspecialty groups with Bonferroni pairwise post-hoc analysis. Linear regression was used to model the impact of age, sex, race, subspecialty, and deprivation quartile on each PROMIS domain. All patients were included in the regression from all four quartiles. The regression models were based on forward entry of each of the independent variables with the α level set at 0.05 for entry into the model. Statistical analyses were performed using SPSS statistical software (Version 23; IBM, New York, NY, USA). Statistical significance was set at p < 0.05. Any missing data elements were excluded from analysis with no imputation performed.
Results
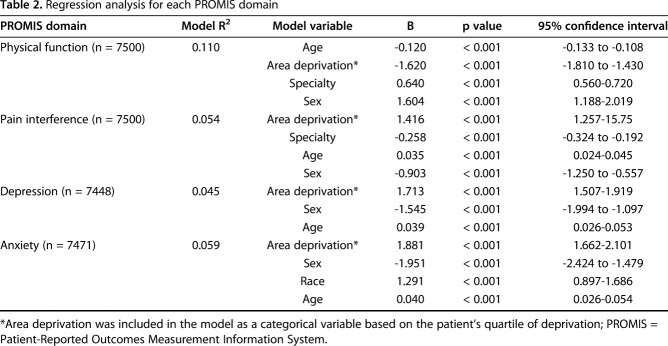
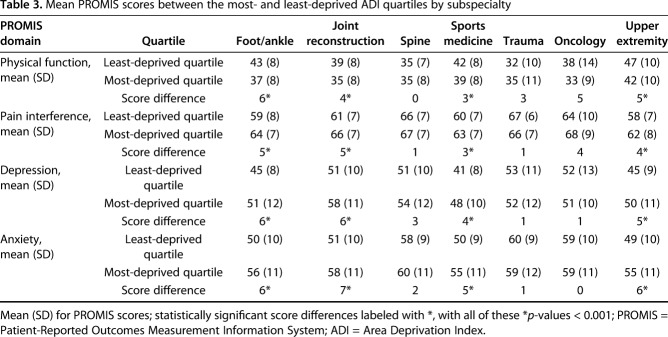
Patients from the most-deprived quartile had higher levels of pain interference, depression, and anxiety and lower levels of physical function, as measured by PROMIS, compared with patients from the least-deprived quartile (Fig. 2). Mean PROMIS physical function was 38 (SD 9) in the most-deprived quartile compared to 43 (SD 9) in the least-deprived quartile for a mean difference of 4 (95% CI, 3.7 to 5.0; p < 0.001). PROMIS pain interference measured 64 (SD 8) in the most-deprived quartile and 60 (SD 8) in the least-deprived quartile for a mean difference of -4 (95% CI, -4.8 to -3.7; p < 0.001). PROMIS depression and anxiety were 50 (SD 11) and 56 (SD 11), respectively, in the most-deprived quartile and only 45 (SD 9) and 50 (SD 10), respectively, in the least-deprived quartile for a mean difference of -5 for depression (95% CI, -6.0 to -4.5; p < 0.001) and a mean difference of -6 for anxiety (95% CI, -6.9 to -5.4; p < 0.001). These differences are at the level of our conservative MCID of 5 points, and must be interpreted with caution. A linear regression model was also created to analyze the impact of ADI on each PROMIS domain while controlling for potentially confounding factors. The ADI quartile remained in the regression model as a predictor of the PROMIS score even after accounting for age, race, gender, and orthopaedic specialty providing care, in all four PROMIS domains analyzed (Table 2). Residence in the most-deprived ADI quartile predicted a lower physical function score and higher pain interference, depression, and anxiety PROMIS scores. The relationship between social deprivation and PROMIS scores was not consistent for different orthopaedic subspecialties. Patients in the most-deprived quartile who were evaluated by the foot/ankle, joint reconstruction, sports medicine, and upper extremity providers had worse physical function, pain interference, depression, and anxiety PROMIS scores compared with those in the least-deprived quartile (Table 3). The score differences varied from 3 to 6 points for each domain, at the level of our conservative MCID of 5, indicating that some caution must be taken in interpreting this significance (Table 3). Among patients visiting spine, trauma, and oncology specialists, PROMIS scores for each PROMIS domain were not different in patients from the highest and lowest quartiles of social deprivation (Table 3). In fact, without consideration for social deprivation, mean PROMIS scores themselves varied among specialties. For example, for the PROMIS domain of anxiety, spine, trauma, and oncology patients’ mean PROMIS scores were 59 (+/-10), 59 (+/-11), and 58 (+/-10), respectively, all about one SD above the normative mean PROMIS score (set at 50). However, for the foot/ankle, sports medicine, and upper extremity patients, the mean PROMIS anxiety scores were 52 (+/-10), 52 (+/-10) and 51 (+/-11), all much closer to the normative mean PROMIS score of 50 and different from the anxiety scores in spine, trauma, and oncology patients (p < 0.001 for ANOVA comparison).
Fig. 2.
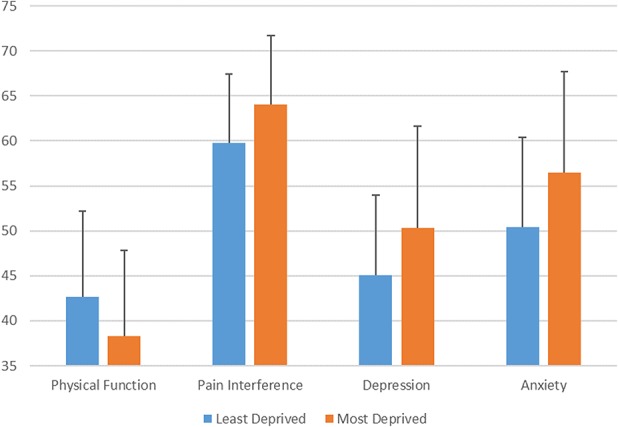
The graph demonstrates the mean PROMIS score for least- and most-deprived ADI quartiles for each PROMIS domain with error bars indicating the SD for each mean. The difference between the mean PROMIS score in patients from the most- and the least-deprived quartile was statistically significant for each PROMIS domain (p < 0.001).
Table 2.
Regression analysis for each PROMIS domain
Table 3.
Mean PROMIS scores between the most- and least-deprived ADI quartiles by subspecialty
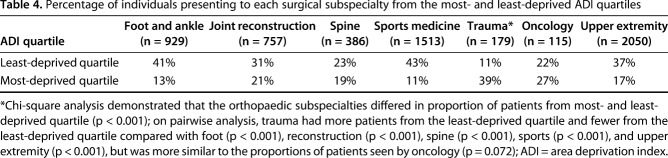
The proportion of individuals presenting from the most- and least-deprived quartiles were also distinct when looking across all seven subspecialty categories (Table 4). Patients presenting to a sports medicine provider were less likely to be from areas of high social deprivation with 43% of patients falling into the least-deprived quartile and only 11% of patients falling into the most-deprived quartile. Trauma patients, on the other hand, were more often from socially deprived areas with 39% of patients falling into the most-deprived quartile and only 11% falling into the least-deprived quartile. This was different than all other specialties, but most similar to oncology, where 27% of patients came from the most deprived quartile and only 22% of patients came from the least-deprived quartile (Table 4).
Table 4.
Percentage of individuals presenting to each surgical subspecialty from the most- and least-deprived ADI quartiles
Discussion
Background and Rationale
In 2014, the Institute of Medicine stated that the inclusion of social and mental health measures will provide the most-effective strategy to improve our nation’s health [23]. Understanding the interrelationship of social health with physical and mental health domains is therefore integral to achieving this mission. Social circumstances are increasingly recognized as a factor that directly impacts physical and mental health with studies linking social deprivation to cancer incidence, cardiovascular and pulmonary health, and even depression [26, 30, 42, 43]. However, the effect of social deprivation on health in orthopaedic patients has not been well defined. We used PROMIS scores to assess self-reported physical and mental health in a large group of orthopaedic patients at their initial presentation to our facility. We found that patients presenting for orthopaedic care who live in the most-socially deprived areas have lower baseline PROMIS scores for physical function and higher scores for pain interference, depression, and anxiety when compared with individuals from the least-socially deprived areas. We found that the impact of social deprivation on physical and mental health measures varied among the orthopaedic subspecialties as did the proportion of individuals from high- and low-deprivation areas.
Limitations
This study has several limitations. Because our data are the experience of one academic tertiary referral center, and a largely white population, there is inherent selection bias and it may not generalize to all populations. However, our large sample size of 7500 patients with home residence spread across 33 states, and a wide spectrum of ADI values, helps to improve the generalizability and mitigate the selection biases of this study. It is unclear if this racial preponderance could magnify or diminish the impact of social deprivation on patient-reported health. Using the ADI to measure social deprivation also adds selection bias to our study, as it does not account for individuals who have a PO box or no address, who likely have the highest levels of social deprivation. Loss of the extremely deprived population likely biases us toward underestimating the impact of social deprivation. We also acknowledge that basing this study on new patient visits identified by International Classification of Diseases, 10th Revision E/M codes disproportionately reduced the number of eligible visits to our trauma surgeons, because many patients are treated emergently, then present for the first time to the clinic as postoperative patients, and therefore were not included in this study. The multiply injured polytrauma patient requiring hospital admission is likely a very different patient than most orthopaedic patients presenting to clinic, and therefore we feel that not accounting for these patients is appropriate in the current study.
Data analysis and conclusions may be affected by missing data, although with a 91% completion rate for PROMIS in our clinics, we suspect the chance of substantial bias that would alter conclusions would be low. There may be other factors relevant to the relationship between social deprivation and both mental and physical health such as medical comorbidities or duration of symptoms before accessing the health system, which were not accounted for in this study. Although we could not account for this in the current study, others have suggested that social deprivation does not impact the duration of symptoms before presentation for treatment of carpal tunnel syndrome [56]. Similarly, in a prior study examining insurance status as a proxy for socioeconomic status among patients arriving at our center for orthopaedic upper extremity care, patients who were under- or uninsured traveled greater distances to access care but did not present with more complex diagnoses [8]. Our study encompasses patients seen at five different clinic locations, including sites that are located in both the highest- and lowest-deprivation quartile communities for the spectrum of specialties, which should further reduce any biases regarding access to care that could also be related to the relationship between PROMIS scores and social deprivation. Although a detailed examination of these additional factors would be possible in a smaller study, our goal in this study was to describe the broader population of patients presenting for orthopaedic care as opposed to a small patient subset in which manual chart review or medical interview would have been feasible. Finally, changing social environments could produce misclassification by the most-recent version of the ADI measure because it is based on 2000 Census data.
Social Deprivation and Outcomes Scores
Few studies have looked at the interrelationship among patient-reported pain, function, and psychologic distress with social health in orthopaedic populations. A large population-based study in the United Kingdom found that as area deprivation increased, so did the proportion of the population reporting any type of musculoskeletal complaint and the magnitude of pain reported by each individual [52]. Among 307 patients undergoing unicompartmental knee arthroplasty, patients with increased social deprivation had worse knee function preoperatively based on objective ROM assessments [5]. Additionally, socioeconomic status, including employment and self-reported social support, is inversely associated with the development of depression after orthopaedic trauma [4]. Our data are consistent with these studies and demonstrate specifically that PROMIS scores for physical and mental health are sensitive to the effects of social deprivation in a large population of patients presenting for orthopaedic care. Our data demonstrate differences in PROMIS scores that approximated what we considered a conservative estimate for the minimal clinically important difference on PROMIS assessments. We interpret this as indicating that social deprivation is associated with a difference in perceived health that is clinically relevant. The modest change in scores was anticipated as it would be unusual to see any factor not directly related to a musculoskeletal condition produce a large effect size difference in perceived physical function. However, even a 4-point difference on PROMIS physical function score can represent a change in the most likely answers to each question that would measurably impact function (see Figure, Supplemental Digital Content 1, http://links.lww.com/CORR/A157). Studies across all subspecialties of orthopaedics have shown that psychologic distress, including symptoms of anxiety and depression, is related to poor clinical outcomes, including persistent pain, heightened disability, and low patient satisfaction [13, 20, 28, 44]. In our study, patients in the most-deprived quartile of our population had higher levels of anxiety and depression as measured by PROMIS than those in the least-deprived quartile. This baseline difference in psychologic health based on ADI is a concerning finding given the potential for both social deprivation and poor mental health to worsen treatment outcomes. Across all surgical fields, a substantial amount of variability persists in patient outcomes that cannot be explained by clinical factors, such as disease severity and patient comorbidities; differences in patients’ mental and social health may account for much of this variability [44]. Our study did not examine treatment outcomes, but took the necessary first step to demonstrate that even at initial presentation, social deprivation has already impacted patient physical and mental health PROMIS scores.
Differences Across Specialties in Relationship Between Deprivation and PROMIS Scores
There may be certain subsets of the orthopaedic population in which social deprivation has less effect on self-reported function, pain, and psychologic distress. Patients seeking care from the spine, oncology, and trauma divisions reported worse physical and mental health scores that were not affected by their level of social deprivation. Trauma patients are known to have high rates of depression, anxiety, and emotional distress; it is possible that these patients may have such a high level of suffering from their disease process alone that the effect of social deprivation is lost [55]. The incidence of psychologic distress has also been reported to be very high in spine patient populations, as high as 80% in one study conducted through the VA Hospital System [40]. This is consistent with our finding of higher depression and anxiety scores in our trauma, spine, and oncology patients. The interaction of social deprivation and physical and mental health has not been well studied in any orthopaedic population. In one study looking at factors related to quality of life and mental health in patients with metastatic bone disease, unemployment was found to impact the quality of life score but not anxiety, depression, or pain interference. Being single only affected depression scores, not anxiety or pain interference [54]. Employment status and household size are factors that contribute to social deprivation, and support our findings that anxiety, depression, and pain interference are not affected by social status in orthopaedic oncology patients. Furthermore, their data demonstrated that quality of life, anxiety, and pain interference measures were all lower in patients with metastatic bone disease than the general population. Our study similarly found that orthopaedic oncology patients have lower PROMIS scores at baseline then individuals presenting to other subspecialties. Future studies are needed to understand why these specific groups of orthopaedic patients have lower physical and mental health scores than other groups, and why these scores are not affected by social health.
Differences in Levels of Social Deprivation Across Specialties
In the current US healthcare environment, which is moving toward emphasis on pay for performance, it is important to understand how patient-reported outcome metrics are influenced by social deprivation. Healthcare disparities already exist in the field of orthopaedics. Income level negatively impacts the likelihood that a patient with hip or knee osteoarthritis will obtain a joint replacement [19]. Studies have also demonstrated the effect of socioeconomic status on ACL treatment choice with individuals with lower socioeconomic status less likely to undergo operative treatment [11, 34]. Our study found that only 11% of patients presenting to a sports medicine provider came from the most-deprived quartile of the population, a lower percentage of deprived patients than other departmental subspecialties. Conversely, a high proportion of trauma patients, 39%, were from the most-socially deprived quartile of the population. There is certainly a difference between the more urgent care provided by orthopaedic trauma surgeons and the elective, quality-of-life-focused procedures in much of orthopaedics, where most of the socioeconomic disparity exits. It is therefore critical that we understand the relationship between social deprivation and patient-reported outcomes in orthopaedic patients so that adjustments can be made before relating any type of reimbursement to patient-reported outcomes. Without this appreciation, individuals serving deprived populations may be penalized, potentially leading to further limitations in access to care for elective orthopaedic procedures and worsening of existing healthcare disparities [51]. Our institution’s experience is not unique as even in the universal health care system of Canada, disparities exist in use of specialty care based on individuals’ socioeconomic status [14]. Thus, there may something inherent to social deprivation that affects a patient’s desire or ability to access elective specialty care. Because our department offers all specialties within clinics that are placed in areas of both greater and less social deprivation, we suspect that social deprivation influences the types of conditions that will prompt an individual to seek elective surgical care. However, the reason behind this finding is unclear.
Conclusions
Social deprivation influences baseline physical function, pain interference, depression, and anxiety PROMIS scores in patients with musculoskeletal complaints with individuals from the most-deprived areas scoring more poorly on all four of these domains. Knowing that a socially based differential in patient-perceived physical and mental health exists at presentation to an orthopaedic provider indicates that patients are not independent of their social environment. It is something that we as orthopaedic surgeons must consider when discussing treatment options and prognosis with our patients, the same way we might consider medical comorbidities or smoking status. Future studies are needed to determine why socially deprived patients have worse physical and mental health, if social deprivation influences the magnitude of change in physical and mental health after treatment, and how changing social environments may influence patient-perceived physical and mental health. Socioeconomic disparities already exist with fewer individuals from deprived areas presenting for care to certain subspecialties. Social deprivation’s effect on physical and mental health should be considered when delivering orthopaedic care and in the interpretation of patient-reported health metrics, or we run the risk of worsening such existing healthcare disparities.
Acknowledgments
We thank Emily Camden for her assistance in formatting the references used in the manuscript.
Footnotes
One of the authors (RO) reports other from Fate Therapeutics, nonfinancial support from Bone, and nonfinancial support from the American Orthopaedic Association, outside the submitted work. One of the authors (RPC) reports grants from research funding from Medartis, outside the submitted work.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Amtmann D, Kim J, Chung H, Askew RL, Park R, Cook KF. Minimally important differences for Patient Reported Outcomes Measurement Information System pain interference for individuals with back pain. J Pain Res. 2016;9:251-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barnard J, Grant SW, Hickey GL, Bridgewater B. Is social deprivation an independent predictor of outcomes following cardiac surgery? An analysis of 240,221 patients from a national registry. BMJ Open. 2015;5:e008287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bartlett SJ, Orbai AM, Duncan T, DeLeon E, Ruffing V, Clegg-Smith K, Bingham CO., 3rd Reliability and validity of selected PROMIS measures in people with rheumatoid arthritis. PLoS One. 2015;10:e0138543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Becher S, Smith M, Ziran B. Orthopaedic trauma patients and depression: a prospective cohort. J Orthop Trauma. 2014;28:e242-246. [DOI] [PubMed] [Google Scholar]
- 5.Bennett D, Hill J, Beverland D, Kee F. The influence of area level social deprivation on preoperative disease severity and postoperative outcomes following unicompartmental knee joint replacement. Knee. 2015;22:653-658. [DOI] [PubMed] [Google Scholar]
- 6.Bevans M, Ross A, Cella D. Patient-Reported Outcomes Measurement Information System (PROMIS): efficient, standardized tools to measure self-reported health and quality of life. Nurs Outlook. 2014;62:339-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burton AK, Tillotson KM, Main CJ, Hollis S. Psychosocial predictors of outcome in acute and subchronic low back trouble. Spine (Phila Pa 1976). 1995;20:722-728. [DOI] [PubMed] [Google Scholar]
- 8.Carstairs V, Morris R. Deprivation: explaining differences in mortality between Scotland and England and Wales. BMJ. 1989;299:886-889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S, Cook K, Devellis R, DeWalt D, Fries JF, Gershon R, Hahn EA, Lai JS, Pilkonis P, Revicki D, Rose M, Weinfurt K, Hays R, Group PC. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010;63:1179-1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen R, Crichton S, McKevitt C, Rudd AG, Sheldenkar A, Wolfe CD. Association between socioeconomic deprivation and functional impairment after stroke: the South London Stroke Register. Stroke. 2015;46:800-805. [DOI] [PubMed] [Google Scholar]
- 11.Collins JE, Katz JN, Donnell-Fink LA, Martin SD, Losina E. Cumulative incidence of ACL reconstruction after ACL injury in adults: role of age, sex, and race. Am J Sports Med. 2013;41:544-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doring AC, Nota SP, Hageman MG, Ring DC. Measurement of upper extremity disability using the Patient-Reported Outcomes Measurement Information System. J Hand Surg Am. 2014;39:1160-1165. [DOI] [PubMed] [Google Scholar]
- 13.Duivenvoorden T, Vissers MM, Verhaar JA, Busschbach JJ, Gosens T, Bloem RM, Bierma-Zeinstra SM, Reijman M. Anxiety and depressive symptoms before and after total hip and knee arthroplasty: a prospective multicentre study. Osteoarthritis Cartilage. 2013;21:1834-1840. [DOI] [PubMed] [Google Scholar]
- 14.Dunlop S, Coyte PC, McIsaac W. Socio-economic status and the utilisation of physicians' services: results from the Canadian National Population Health Survey. Soc Sci Med. 2000;51:123-133. [DOI] [PubMed] [Google Scholar]
- 15.Dy CJ, Lane JM, Pan TJ, Parks ML, Lyman S. Racial and socioeconomic disparities in hip fracture care. J Bone Joint Surg Am. 2016;98:858-865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fernandez-Nino JA, Manrique-Espinoza BS, Bojorquez-Chapela I, Salinas-Rodriguez A. Income inequality, socioeconomic deprivation and depressive symptoms among older adults in Mexico. PLoS One. 2014;9:e108127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 2). J Epidemiol Community Health. 2006;60:95-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gatchel RJ, Polatin PB, Mayer TG. The dominant role of psychosocial risk factors in the development of chronic low back pain disability. Spine (Phila Pa 1976). 1995;20:2702-2709. [DOI] [PubMed] [Google Scholar]
- 19.Hawkins K, Escoto KH, Ozminkowski RJ, Bhattarai GR, Migliori RJ, Yeh CS. Disparities in major joint replacement surgery among adults with Medicare supplement insurance. Popul Health Manag. 2011;14:231-238. [DOI] [PubMed] [Google Scholar]
- 20.Hobby JL, Venkatesh R, Motkur P. The effect of psychological disturbance on symptoms, self-reported disability and surgical outcome in carpal tunnel syndrome. J Bone Joint Surg Br. 2005;87:196-200. [DOI] [PubMed] [Google Scholar]
- 21.Hung M, Franklin JD, Hon SD, Cheng C, Conrad J, Saltzman CL. Time for a paradigm shift with computerized adaptive testing of general physical function outcomes measurements. Foot Ankle Int. 2014;35:1-7. [DOI] [PubMed] [Google Scholar]
- 22.Hung M, Stuart AR, Higgins TF, Saltzman CL, Kubiak EN. Computerized adaptive testing using the PROMIS physical function item bank reduces test burden with less ceiling effects compared with the Short Musculoskeletal Function Assessment in orthopaedic trauma patients. J Orthop Trauma. 2014;28:439-443. [DOI] [PubMed] [Google Scholar]
- 23.Institute of Medicine. Capturing Social and Behavioral Domains in Electronic Health Records: Phase 1 . Washington, DC: The National Academies Press; 2014. [PubMed] [Google Scholar]
- 24.Jenkins PJ, Watts AC, Duckworth AD, McEachan JE. Socioeconomic deprivation and the epidemiology of carpal tunnel syndrome. J Hand Surg Eur Vol. 2012;37:123-129. [DOI] [PubMed] [Google Scholar]
- 25.Khatib Y, Madan A, Naylor JM, Harris IA. Do Psychological Factors Predict Poor Outcome in Patients Undergoing TKA? A Systematic Review. Clin Orthop Relat Res. 2015;473:2630-2638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kind AJ, Jencks S, Brock J, Yu M, Bartels C, Ehlenbach W, Greenberg C, Smith M. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161:765-774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kinderman P, Tai S, Pontin E, Schwannauer M, Jarman I, Lisboa P. Causal and mediating factors for anxiety, depression and well-being. Br J Psychiatry. 2015;206:456-460. [DOI] [PubMed] [Google Scholar]
- 28.Koorevaar RC, van 't Riet E, Gerritsen MJ, Madden K, Bulstra SK. The influence of preoperative and postoperative psychological symptoms on clinical outcome after shoulder surgery: a prospective longitudinal cohort study. PLoS One. 2016;11:e0166555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee AC, Driban JB, Price LL, Harvey WF, Rodday AM, Wang C. Responsiveness and minimally important differences for 4 Patient-Reported Outcomes Measurement Information System short forms: physical function, pain interference, depression, and anxiety in knee osteoarthritis. J Pain. 2017;18:1096-1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lian M, Schootman M, Doubeni CA, Park Y, Major JM, Stone RA, Laiyemo AO, Hollenbeck AR, Graubard BI, Schatzkin A. Geographic variation in colorectal cancer survival and the role of small-area socioeconomic deprivation: a multilevel survival analysis of the NIH-AARP Diet and Health Study Cohort. Am J Epidemiol. 2011;174:828-838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.London DA, Stepan JG, Boyer MI, Calfee RP. The impact of depression and pain catastrophization on initial presentation and treatment outcomes for atraumatic hand conditions. J Bone Joint Surg Am. 2014;96:806-814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lozano Calderon SA, Paiva A, Ring D. Patient satisfaction after open carpal tunnel release correlates with depression. J Hand Surg Am. 2008;33:303-307. [DOI] [PubMed] [Google Scholar]
- 33.Mair C, Diez Roux AV, Galea S. Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. J Epidemiol Community Health. 2008;62:940-946, 948 p following 946. [DOI] [PubMed] [Google Scholar]
- 34.Nordenvall R, Marcano AI, Adami J, Palme M, Mattila VM, Bahmanyar S, Fellander-Tsai L. The effect of socioeconomic status on the choice of treatment for patients with cruciate ligament injuries in the knee: a population-based cohort study. Am J Sports Med. 2017;45:535-540. [DOI] [PubMed] [Google Scholar]
- 35.Northwestern University. Health measures - transforming how health is measured. 2018. Northwestern University. Funding for HealthMeasures was provided by the National Institutes of Health grant Northwestern University; Available at http://www.healthmeasures.net. Accessed November 5, 2018. [Google Scholar]
- 36.Nunez F, Vranceanu AM, Ring D. Determinants of pain in patients with carpal tunnel syndrome. Clin Orthop Relat Res. 2010;468:3328-3332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oflazoglu K, Mellema JJ, Menendez ME, Mudgal CS, Ring D, Chen NC. Prevalence of and factors associated with major depression in patients with upper extremity conditions. J Hand Surg Am. 2016;41:263-269 e261-267. [DOI] [PubMed] [Google Scholar]
- 38.Paczkowski MM, Galea S. Sociodemographic characteristics of the neighborhood and depressive symptoms. Curr Opin Psychiatry. 2010;23:337-341. [DOI] [PubMed] [Google Scholar]
- 39.Papuga MO, Mesfin A, Molinari R, Rubery PT. Correlation of PROMIS physical function and pain CAT instruments with Oswestry Disability Index and Neck Disability Index in spine patients. Spine (Phila Pa 1976). 2016;41:1153-1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patton CM, Hung M, Lawrence BD, Patel AA, Woodbury AM, Brodke DS, Daubs MD. Psychological distress in a Department of Veterans Affairs spine patient population. Spine J. 2012;12:798-803. [DOI] [PubMed] [Google Scholar]
- 41.Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, Group PC. Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS(R)): depression, anxiety, and anger. Assessment. 2011;18:263-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Powell-Wiley TM, Ayers C, Agyemang P, Leonard T, Berrigan D, Ballard-Barbash R, Lian M, Das SR, Hoehner CM. Neighborhood-level socioeconomic deprivation predicts weight gain in a multi-ethnic population: longitudinal data from the Dallas Heart Study. Prev Med. 2014;66:22-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Richardson R, Westley T, Gariepy G, Austin N, Nandi A. Neighborhood socioeconomic conditions and depression: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1641-1656. [DOI] [PubMed] [Google Scholar]
- 44.Rosenberger PH, Jokl P, Ickovics J. Psychosocial factors and surgical outcomes: an evidence-based literature review. J Am Acad Orthop Surg. 2006;14:397-405. [DOI] [PubMed] [Google Scholar]
- 45.Saito M, Kondo K, Kondo N, Abe A, Ojima T, Suzuki K, group J. Relative deprivation, poverty, and subjective health: JAGES cross-sectional study. PLoS One. 2014;9:e111169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Salmond C, Crampton P, Sutton F. NZDep91: A New Zealand index of deprivation. Aust N Z J Public Health. 1998;22:835-837. [DOI] [PubMed] [Google Scholar]
- 47.Singh GK. Area deprivation and widening inequalities in US mortality, 1969-1998. Am J Public Health. 2003;93:1137-1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Singh GK, Kogan MD. Widening socioeconomic disparities in US childhood mortality, 1969 2000. Am J Public Health. 2007;97:1658-1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stone AA, Broderick JE, Junghaenel DU, Schneider S, Schwartz JE. PROMIS fatigue, pain intensity, pain interference, pain behavior, physical function, depression, anxiety, and anger scales demonstrate ecological validity. J Clin Epidemiol. 2016;74:194-206. [DOI] [PubMed] [Google Scholar]
- 50.Swanholm E, McDonald W, Makris U, Noe C, Gatchel R. Estimates of minimally important differences (MIDs) for two Patient-Reported Outcomes Measurement Information System (PROMIS) computer-adaptive tests in chronic pain patients. J Appl Biobehav Res. 2014;19:217-232. [Google Scholar]
- 51.Tyser AR, Beckmann J, Franklin JD, Cheng C, Hon SD, Wang A, Hung M. Evaluation of the PROMIS physical function computer adaptive test in the upper extremity. J Hand Surg Am. 2014;39:2047-2051 e2044. [DOI] [PubMed] [Google Scholar]
- 52.Urwin M, Symmons D, Allison T, Brammah T, Busby H, Roxby M, Simmons A, Williams G. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis. 1998;57:649-655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Utrillas-Compaired A, De la Torre-Escuredo BJ, Tebar-Martinez AJ, Asunsolo-Del Barco A. Does preoperative psychologic distress influence pain, function, and quality of life after TKA? Clin Orthop Relat Res. 2014;472:2457-2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.van der Vliet QM, Paulino Pereira NR, Janssen SJ, Hornicek FJ, Ferrone ML, Bramer JA, van Dijk CN, Schwab JH. What factors are associated with quality of life, pain interference, anxiety, and depression in patients with metastatic bone disease? Clin Orthop Relat Res. 2017;475:498-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vincent HK, Horodyski M, Vincent KR, Brisbane ST, Sadasivan KK. Psychological distress after orthopedic trauma: prevalence in patients and implications for rehabilitation. PM R. 2015;7:978-989. [DOI] [PubMed] [Google Scholar]
- 56.Wright MA, Beleckas CM, Calfee RP. Mental and physical health disparities in patients with carpal tunnel syndrome living with high levels of social deprivation. J Hand Surg Am. 2018. 10.1016/j.jhsa.2018.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yost KJ, Eton DT, Garcia SF, Cella D. Minimally important differences were estimated for six Patient-Reported Outcomes Measurement Information System-Cancer scales in advanced-stage cancer patients. J Clin Epidemiol. 2011;64:507-516. [DOI] [PMC free article] [PubMed] [Google Scholar]