Abstract
Background
A large body of research shows that psychologic distress and ineffective coping strategies substantially contribute to more severe pain and increased physical limitations among patients with orthopaedic disorders. However, little is known about the relationship between positive psychology (constructs that enable individuals to thrive and adapt to challenges) and pain and physical limitations in this population.
Questions/purposes
(1) Which positive-psychology factors (satisfaction with life, gratitude, coping through humor, resilience, mindfulness, and optimism) are independently associated with fewer upper-extremity physical limitations after controlling for the other clinical and demographic variables? (2) Which positive-psychology factors are independently associated with pain intensity after controlling for relevant clinical and demographic variables?
Methods
In a cross-sectional study, we recruited patients presenting for a scheduled appointment with an orthopaedic surgeon at a hand and upper-extremity clinic of a major urban academic medical center. Of 125 approached patients, 119 (44% men; mean age, 50 ± 17 years) met screening criteria and agreed to participate. Patients completed a clinical and demographic questionnaire, the Numerical Rating Scale to assess pain intensity, the Patient-reported Outcomes Measurement Information System (PROMIS) Upper Extremity Physical Function computerized adaptive test to assess physical limitations, and six measures assessing positive-psychology constructs: The Satisfaction with Life Scale, the Gratitude Questionnaire, the Coping Humor Scale, the Brief Resilience Scale, the Cognitive and Affective Mindfulness Scale-Revised, and the Life Orientation Test-Revised. We first examined bivariate associations among physical limitations, pain intensity, and all positive-psychology factors as well as demographic and clinical variables. All variables that demonstrated associations with physical limitations or pain intensity at p < 0.05 were included in two-stage multivariable hierarchical regression models.
Results
After controlling for the potentially confounding effects of prior surgical treatment and duration since pain onset (step1; R2 total = 0.306; F[7,103] = 6.50), the positive-psychology variables together explained an additional 15% (R2 change = 0.145, F change [5, 103] = 4.297, p = 0.001) of the variance in physical limitations. Among the positive-psychology variables tested, mindfulness was the only one associated with fewer physical limitations (β = 0.228, t = 2.293, p = 0.024, 4% variance explained). No confounding demographic or clinical variables were found for pain intensity in bivariate analyses. All positive-psychology variables together explained 23% of the variance in pain intensity (R2 = 0.23; F[5,106] = 6.38, p < 0.001). Among the positive-psychology variables, satisfaction with life was the sole factor independently associated with higher intensity (β = -0.237, t = -2.16, p = 0.033, 3% variance explained).
Conclusions
Positive-psychology variables explained 15% of the variance in physical limitations and for 23% of the variance in pain intensity among patients with heterogenous upper extremity disorders within a hand and upper extremity practice. Of all positive-psychology factors, mindfulness and satisfaction with life were most important for physical limitations and pain intensity, respectively. As positive-psychology factors are more easily modifiable through skills-based interventions than pain and physical limitations, results suggest implementation of such interventions to potentially improve outcomes in this population. Skills-based interventions targeting mindfulness and satisfaction with life may be of particular benefit.
Level of Evidence
Level II, prognostic study.
Introduction
Emotional distress (such as symptoms of depression and anxiety) and maladaptive coping strategies (like catastrophic thinking in response to nociception) are consistently associated with increased pain and physical limitations in heterogeneous patients with upper extremity disorders [7, 10, 25, 27, 34, 36]. However, assessing and addressing these factors within the normal flow of orthopaedic care is challenging, primarily as a result of the stigma associated with mental health concerns and surgeons’ lack of comfort in discussing these issues with their patients [38]. The positive-psychology framework, which focuses on cultivating individual strengths (versus focusing on deficiencies), may provide novel insight into the development of feasible and acceptable interventions for this population. The field of positive-psychology is not concerned merely with the absence of distress or maladaptive coping. Rather, it focuses on individual’s strengths and qualities of personal growth and flourishing. Interventions that follow positive-psychology principles are associated with increased well-being and improved function [12, 30]. Such interventions may foster effective communication between surgeons and patients, and may increase the likelihood that patients would participate in psychosocial interventions [39, 41].
Positive-psychology constructs such as satisfaction with life (one’s level of individual subjective well-being [9]), gratitude (one’s tendency to recognize and respond with grateful emotion to general life events [23]), coping through humor (seeing mirth within stressful experiences [22]), resilience (the ability to bounce back or recover from stress [32]), mindfulness (the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment to moment [13, 18]), and optimism (the ability to remain positive in the face of stress [28]) have been consistently shown to confer beneficial effects for mental health and in coping with stress and chronic illness [4]. Our team has shown that among patients with upper extremity conditions, greater overall mindfulness is associated with lower pain intensity [2] and that a 60-second mindfulness-based video exercise can improve momentary pain, anxiety, depression, and anger in this group [40]. We have also shown that satisfaction with life buffers the effect of pain in individuals with upper extremity musculoskeletal disorders [33]. However, no prior studies have comprehensively assessed multiple positive-psychology factors simultaneously in this population. This information is needed to determine the individual and combined role of positive-psychology constructs and thus inform novel interventions.
In the current work, we asked the following research questions: (1) Which positive-psychology factors (satisfaction with life, gratitude, coping through humor, resilience, mindfulness, and optimism) are independently associated with fewer upper-extremity physical limitations after controlling for the other clinical and demographic variables? (2) Which positive-psychology factors are independently associated with pain intensity after controlling for relevant clinical and demographic variables?
Patients and Methods
After institutional review board approval, we invited 125 patients presenting for a scheduled appointment with an orthopaedic surgeon at a hand and upper extremity clinic of a major urban academic medical center to participate in this cross-sectional study. Patients were approached regardless of visit type (for example, new patient or followup). Research assistants were on-site 1 day a week between April 2017 and June 2017. We only approached English-speaking patients who were aged 18 years or older. Exclusion criteria were being pregnant and having self-reported serious mental illness (for example, active substance abuse, untreated bipolar disorder, schizophrenia, or psychotic symptoms) because these populations were precluded by our institutional review board. After verbal informed consent was provided, patients completed self-report measures on a tablet computer through the sure web-based research platform RedCap (Vanderbilt University, Nashville, TN, USA) [15].
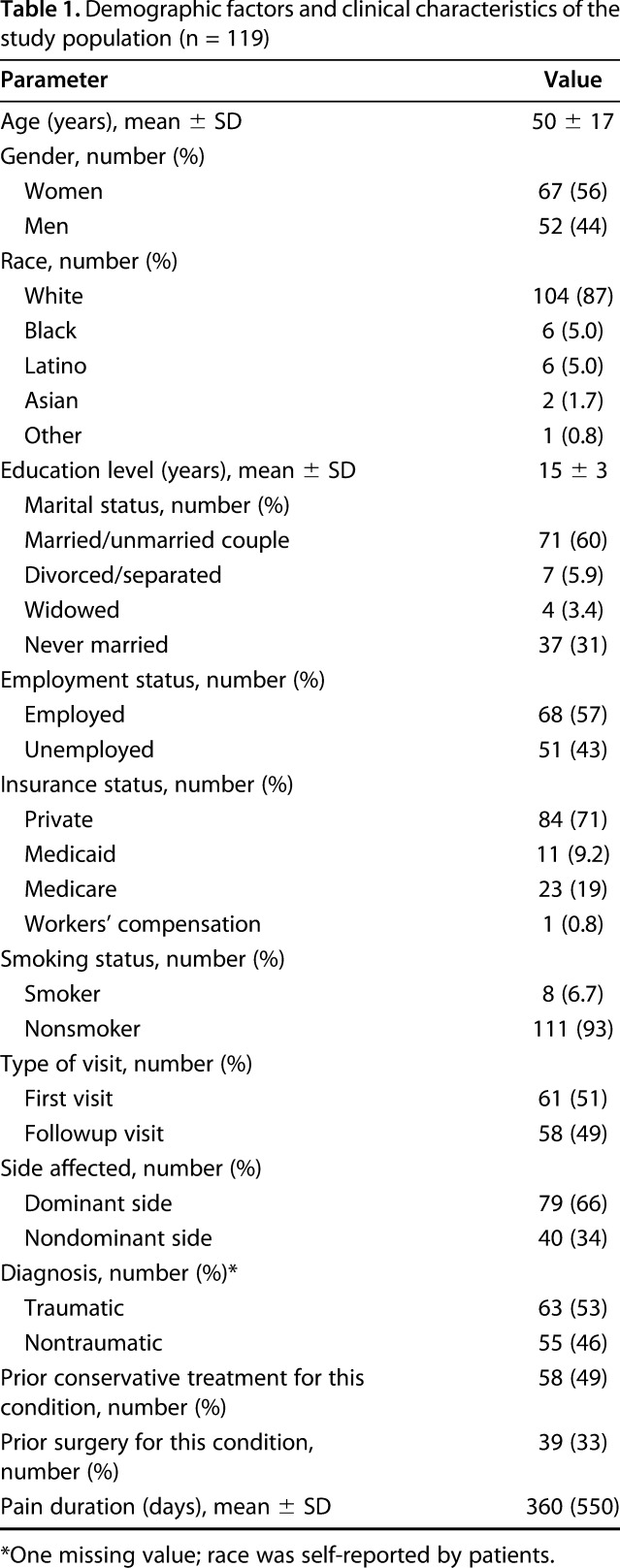
All participants (n = 125) who were approached and screened met inclusion and exclusion criteria; however, six declined. The main reasons for declining were no time for participation or lack of interest in the research project. Our final sample included the 119 patients who agreed to participate and provided informed consent. A total of 56% of the patients were women (n = 67) and had a mean age of 50 years (SD = 17). Most patients were white (n = 104; 87%) and all (n = 119; 100%) had insurance. Race was self-reported by patients. Eight percent of the patients (n = 10) had less than a high school diploma. Fifty-seven percent of patients (n = 68) were employed (Table 1).
Table 1.
Demographic factors and clinical characteristics of the study population (n = 119)
Measures
PROMIS Upper Extremity Physical Function computerized adaptive test
The PROMIS Upper Extremity Physical Function computerized adaptive test (CAT) assesses patients’ abilities to engage in various activities that involve the hands and upper extremities (for example, tying shoelaces, holding a plate of food, reaching into a high cupboard) using a response scale from 1 (“without any difficulty”) to 5 (“unable to do”) [11]. CATs improve questionnaire administration by distributing only relevant items based on previous responses. The CAT generates a standardized T-score (mean = 50, SD = 10). Higher scores represent fewer physical limitations. The PROMIS Upper Extremity Physical Function CAT has been validated for use in patients with upper extremity disorders by multiple studies [1, 35]
Numerical Pain Rating Scale
Patients rated their pain intensity on a scale ranging from 0 (“no pain at all”) to 10 (“most severe pain”).
Satisfaction with Life Scale
The Satisfaction with Life Scale (SWLS) is a reliable and valid [26] five-item scale designed to measure the extent to which patients are satisfied with their life on a 7-point Likert scale [9]. Items were added to generate a total score; higher scores represented higher satisfaction with life. Internal consistency in the current sample was good (α = 0.87) [14].
Gratitude Questionnaire-Six Item Form
The Gratitude Questionnaire-Six Item Form (GQ-6) is a reliable and valid [24] six-item measure of the general tendency to experience gratitude. Patients rated the extent to which they agree (1 = “strongly disagree”; 7 = “strongly agree”) with six statements about gratitude [23]. Negatively worded items were reverse-scored, and all items were then added to generate a total score, and higher scores represented a greater tendency toward optimism [24] . Internal consistency in the current sample was adequate (α = 0.74) [14] .
Coping Humor Scale
The Coping Humor Scale (CHS) is a reliable and valid [22] seven-item measure of the extent to which individuals use humor as a means of coping with difficult situations or adversity. Respondents rated the degree to which each agree (1 = “strongly disagree”; 4 = “strongly agree”) with each statement. Negatively worded items were reverse-scored, and all items were added to generate a total score; higher scores represented a higher tendency to use humor for coping. Internal consistency in the current sample was adequate (α = 0.67)[14] .
Brief Resilience Scale
The Brief Resilience Scale (BRS) is a reliable and valid [32] six-item self-report measure that assesses the extent to which individuals recover quickly from stress or adversity. Patients rate how much they agree (1 = “strongly disagree”; 5 = “strongly agree”) with each statement. Negatively worded items were reverse-scored, and all items were then added to generate a total score. Higher scores represented greater resilience [32]. Internal consistency in the current sample was good (α = 0.84) [14].
Cognitive and Affective Mindfulness Scale-Revised
The 10-item version of the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R) is a reliable and valid [13] self-report measure of the frequency (0 = “rarely/not at all”; 3 = “almost always”) with which patients use mindfulness behaviors (for example, noticing thoughts without judgment) in their daily lives. Negatively worded items were reverse-scored, and all items were added to generate a total score; higher scores represented greater levels of mindfulness. Internal consistency in the current sample was good (α = 0.86) [14].
Life Orientation Test-Revised
The Life Orientation Test-Revised (LOT-R) is a reliable and valid [29] 10-item measure of a general tendency toward optimism or pessimism. Patients rated the extent to which they agree (0 = “strongly disagree”; 4 = “strongly agree”) with six statements about optimism or pessimism. Four filler items were discarded, leaving six items that comprised the scale. Negatively worded items were reverse-scored, and the six scored items were added to generate a total score. Higher scores represented higher levels of optimism. Internal consistency in the current sample was adequate (α = 0.74) [14].
Demographic and Clinical Variables
Patients self-reported demographics, such as age, gender, race/ethnicity, education level, marital status, employment status, insurance status, and smoking status. Patients also self-reported their visit type (new versus followup), whether they were seeking care for a traumatic injury, the duration of their pain, and whether they had received prior surgical treatment for the current chief disorder.
Statistical Analysis
Bivariate tests
First, we summarized descriptive statistics for demographic and clinical variables. Second, we examined bivariate Pearson correlations among physical limitations, pain intensity, and all positive-psychology factors as well as continuous demographic and clinical variables. For categorical factors (for example, gender, marital status, smoking status), we conducted univariate analyses of variance to assess differences in pain intensity and physical limitations. In bivariate correlations, higher satisfaction with life (r = 0.272, p = 0.003), gratitude (r = 0.248, p = 0.007), humor (r = 0.197, p = 0.033), mindfulness (r = 0.394, p < 0.001), optimism (r = 0.224, p = 0.017) and longer duration of pain (r = 0.233, p = 0.011) were associated with fewer physical limitations. Physical limitations were also lower among patients who had not received prior surgical treatment for their chief complaint (M = 38.966, SD = 8.483) compared with those who had received surgery (M = 32.729, SD = 7.639; F(1,117)=13.87 p < 0.001). Higher satisfaction with life (r = -0.411, p < 0.001), gratitude (r = -0.271, p = 0.003), resilience (r = -0.262, p = 0.004), mindfulness (r = -330, p < 0.000), and optimism (r = -0.364, p < 0.001) were associated with lower pain intensity. All other bivariate analyses were not significant.
Multivariable models
We determined a priori that all variables that demonstrated associations with physical activity limitations or pain intensity at p < 0.05 would be included in two-stage multivariable hierarchical regression models. The significant demographic and clinical variables were entered at the first stage of the hierarchical model and the significant positive-psychology factors were entered in the second stage to identify unique contributions of positive-psychology factors beyond clinical and demographic variables, and to determine which positive-psychology construct(s) were most important for both pain and physical function. We used an α level of p < 0.05 to determine statistical significance and the squared semipartial correlation (sr2) as a measure of variance in outcomes explained by each individual variable in the multivariable regression for this cross-sectional data with imposed predictors (demographics, clinical variables, and positive-psychology variables) and outcomes (pain and physical function. The R2 was calculated to show the entire amount of variance explained by all variables in the model, and R2 change was calculated to depict the amount of variance explained by the positive-psychology variables together over and above demographics and clinical variables.
Power analyses
An a priori analysis indicated that a sample size of 116 patients would provide 90% statistical power (α = 0.05) to detect a medium effect size (Cohen’s f2 = 0.15) in a multivariable linear regression model with five tested predictors. The regression models met assumptions with regard to sample size, multicollinearity (minimum r = 0.20, maximum r = 0.561 between positive-psychology factors), and heteroskedasticity.
Results
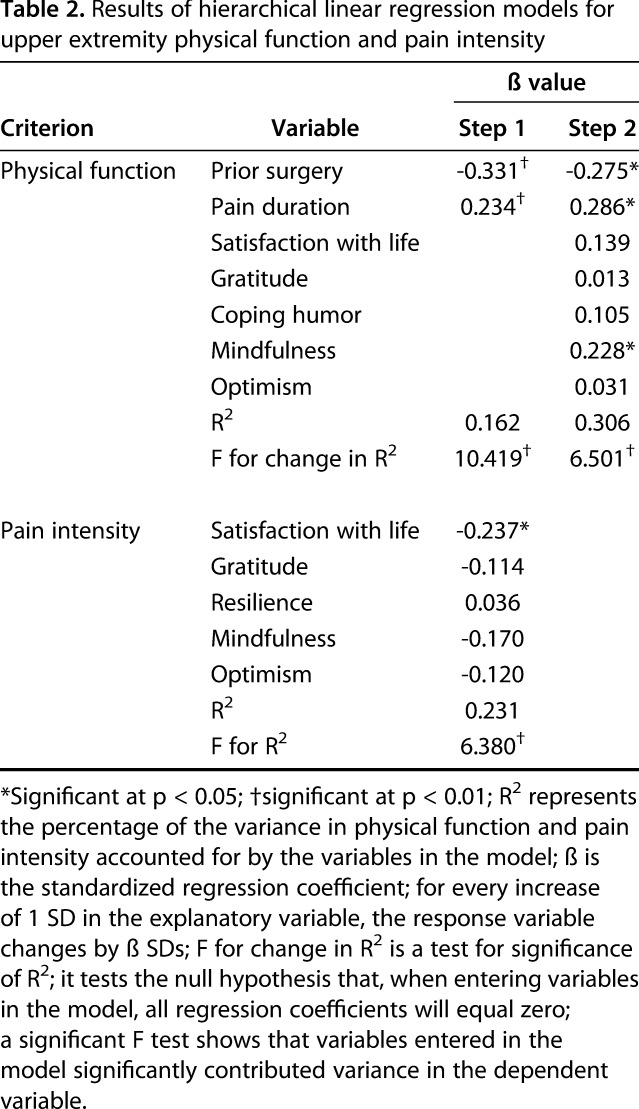
Of the positive-psychology variables examined, mindfulness was the only factor we examined that was associated with lower physical limitations (ß = 0.228, t = 2.293, p = 0.024; sr2 = 0.0353; 4% variance explained). Lack of prior surgical treatment and longer duration since pain onset were associated with fewer physical limitations in step one of the hierarchical model and explained 16% of the variance in physical limitations (R2 = 0.162; F[2,108] = 10.42, p < 0.001; Table 2). After controlling for these confounding clinical variables in step 1 of the model, all the positive-psychology variables were added in step 2 and together explained an additional 15 % (R2 change = 0.145, F change [5,103] = 4.297; p = 0.001) of the variance in physical limitations, beyond that explained by the clinical variables alone. The entire model explained 31% (16% in step 1 and 15% in step 2) of the variance (R2 total = 0.306; F[7,103] = 6.50) in physical limitations. Of the positive-psychology variables, satisfaction with life was the only factor associated with higher pain intensity (ß = -0.237, t = -2.16, p = 0.03; 3% variance explained). Given that there were no observed differences in pain intensity according to any demographic or clinical variables, the multivariable model was a single-stage regression model in which all positive-psychology variables were entered simultaneously (Table 2; F[5,106] = 6.38, p < 0.001). All positive-psychology factors together explained 23% of the variance in pain intensity (R2 = 0.231).
Table 2.
Results of hierarchical linear regression models for upper extremity physical function and pain intensity
Discussion
Distress and less-effective coping strategies contribute to increased pain intensity and greater magnitude of limitations among patients with orthopaedic injuries [7, 10, 25, 27, 34, 36]. Addressing these deficiencies has been historically challenging with this population because of the stigma associated with these problems. Using a positive-psychology lens, with its focus on strengths rather than deficits, is a novel approach that may be better received by this population. After controlling for potential demographic and clinical confounding variables, we found that mindfulness was the sole positive-psychology factor associated with fewer physical limitations, and satisfaction with life was the sole positive-psychology factor associated with pain intensity. Although the other positive-psychology factors did not show an association with pain or physical limitations after controlling for confounding variables, positive-psychology factors did contribute to a substantial increase in the amount of variance explained in both pain and physical function.
This study had several limitations. First, this is a cross-sectional study and although we imposed predictors and outcomes as required by the regression analyses, causal inferences cannot be made. Prior research in patients with chronic pain depicts a bidirectional association between pain/limitations on one hand, and psychosocial variables on the other [33, 34] . In line with this, it is likely that positive-psychology constructs in the current sample influence pain and limitations, which, in turn, influence positive-psychology constructs. However, it is important to mention that the positive-psychology factors are more easily modifiable than pain and physical limitations [5, 16, 19, 21, 31]. Thus, addressing these factors can foster recovery and stop a potential vicious cycle of pain and disability in this population. Second, we recruited patients from a single academic medical center in the northeast United States. Our sample, albeit representative of patients seen in our medical center, was primarily white and highly educated. This may limit generalizability, as it is uncertain whether patients at other locations, who may differ in clinical and demographic characteristics, would exhibit similar associations between positive-psychology constructs and levels of pain and physical limitations. Future studies should replicate our findings through prospective studies with more diverse patient populations. In addition, PROMIS-upper extremity (UE) may have limitations, including substantial ceiling effects [3]. The PROMIS-UE, however, is one of the few questionnaires that have been validated specifically for use in patients with upper extremity disorders.
Mindfulness was the only positive-psychology factor correlated with physical function after controlling for clinical and demographic variables (Table 2) such that patients with higher mindfulness also reported fewer physical limitations. Mindfulness might therefore be the most-promising factor to target in interventions focused on decreasing physical limitations. Mindfulness-based interventions appear to reduce the severity of physical limitations [8, 20, 37]. Among patients with upper extremity conditions, brief mindfulness exercises have been found to be feasible, accepted, and associated with a substantial decrease in pain and distress in both open and randomized controlled trials [6, 40]. A primary emphasis of mindfulness is facing experiences with acceptance and without judgment rather than striving to control and change the experiences, particularly those that are beyond our control [17]. Although the current work cannot offer causal inference, it is likely that fostering such an accepting and nonjudgmental attitude in the face of orthopaedic injury may help decrease physical limitations. Our results support mindfulness-based interventions as means of reducing physical limitations in orthopaedic patients. Recent evidence suggests that mindfulness training can measurably improve other positive-psychology constructs besides mindfulness, including satisfaction with life, optimism, gratitude, and resilience [5, 16, 19, 21, 31]. Mindfulness independently explained 4% of the variance in physical function, but this should be considered in the context of the interrelation between the rest of the positive-psychology constructs. Its 4% contribution is thus in addition to that derived from the other positive-psychology factors, which together explained a substantial 15% of the variance in physical function. These positive-psychology constructs, and particularly mindfulness, thus may provide an opportunity to improve function in this population.
Satisfaction with life was the only positive-psychology variable we found that was independently associated with pain (Table 2). This supports previous research indicating that satisfaction with life plays an important role among orthopaedic patients in moderating the indirect effect of pain intensity on pain interference [33]. These results coupled with those of the current study reinforce the need to account for the interrelation of pain with satisfaction with life in understanding reports of pain in orthopaedic patients. Similar to our findings for physical limitations, although satisfaction with life was the only factor we investigated that was associated with pain after controlling for relevant confounding variables, the rest of the positive-psychology variables explained a substantial amount of variance in pain intensity suggesting that they, too, are important in understanding reports of pain in this population. Our study has important implications for clinical care. Positive-psychology factors are more-easily modifiable through skills-based interventions than are pain or physical limitations. Psychosocial interventions used as an adjunct to medical care may benefit from focusing on teaching positive-psychology skills. A primary focus should be on mindfulness-based interventions that can measurably improve positive-psychology constructs in addition to mindfulness. Such interventions focused on cultivating strengths rather than eliminated deficiencies are likely to be feasible, acceptable and efficacious, as evidenced by prior reports [6, 40]. There is thus a tremendous opportunity for improving pain and physical function in this population.
Acknowledgments
We thank Mr. Ryan Mace for his contribution to some of the statistical procedures performed in this study.
Footnotes
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
One of the authors certifies that he (DR), or a member of his or her immediate family, has received or may receive payments or benefits, during the study period; in an amount of USD 10,000 to USD 100,000 from Skeletal Dynamics; in an amount of USD 10,000 to USD 100,000 from Wright Medical; in an amount of less than USD 10,000 from Clinical Orthopaedics and Related Research®; in an amount of less than USD 10,000 from universities and hospitals; and an amount of USD 10,000 to USD 100,000 from lawyers.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Massachusetts General Hospital, Boston, MA, USA.
References
- 1.Beckmann JT, Hung M, Voss MW, Crum AB, Bounsanga J, Tyser AR. Evaluation of the Patient-Reported Outcomes Measurement Information System Upper Extremity Computer Adaptive Test. J Hand Surg Am . 2016;41:739–744.e4. [DOI] [PubMed] [Google Scholar]
- 2.Beks R, Mellema J, Menendez M, Chen N, Ring D, Vranceanu A. Does mindfulness correlate with physical function and pain intensity in patients with upper extremity illness? Hand (N Y). 2018;13:237-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beleckas CM, Padovano A, Guattery J, Chamberlain AM, Keener JD, Calfee RP. Performance of Patient-Reported Outcomes Measurement Information System (PROMIS) Upper Extremity (UE) Versus Physical Function (PF) Computer Adaptive Tests (CATs) in Upper Extremity Clinics. J Hand Surg Am . 2017;42:867–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E. Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health. 2013;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med . 2008;31:23–33. [DOI] [PubMed] [Google Scholar]
- 6.Chad-Friedman E, Talaei-Khoei M, Ring D, Vranceanu A-M. First use of a brief 60-second mindfulness exercise in an orthopedic surgical practice; results from a pilot study. Arch Bone Jt Surg . 2017;5:400–405. [PMC free article] [PubMed] [Google Scholar]
- 7.Das De S, Vranceanu AM, Ring DC. Contribution of kinesophobia and catastrophic thinking to upper-extremity-specific disability. J Bone Joint Surg Am . 2013;95:76–81. [DOI] [PubMed] [Google Scholar]
- 8.de Vibe M. Mindfulness based stress reduction (MBSR) for improving health, quality of life, and social functioning in adults. Campbell Syst Rev . 2012;13. [Google Scholar]
- 9.Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. J Pers Assess . 1985;49:71–75. [DOI] [PubMed] [Google Scholar]
- 10.Dimitriadis Z, Kapreli E, Strimpakos N, Oldham J. Do psychological states associate with pain and disability in chronic neck pain patients? J Back Musculoskelet Rehabil . 2015;28:797–802. [DOI] [PubMed] [Google Scholar]
- 11.Döring AC, Nota SPFT, Hageman MGJS, Ring DC. Measurement of upper extremity disability using the patient-reported outcomes measurement information system. J Hand Surg Am . 2014;39:1160–1165. [DOI] [PubMed] [Google Scholar]
- 12.Duckworth A, Steen T, Seligman MEP. Positive psychology in clinical practice. Annu Rev Clin Psychol . 2005;1:629–651. [DOI] [PubMed] [Google Scholar]
- 13.Feldman G, Hayes A, Kumar S, Greeson J, Laurenceau JP. Mindfulness and emotion regulation: The development and initial validation of the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R). J Psychopathol Behav Assess . 2007;29:177–190. [Google Scholar]
- 14.George D, Mallery P. SPSS for Windows step by step: A simple guide and reference. 11.0 update. 4th ed. Boston: Allyn & Bacon; 2003. [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform . 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoge EA, Bui E, Marques L, Metcalf CA, Morris LK, Robinaugh DJ, Worthington JJ, Pollack MH, Simon NM. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: effects on anxiety and stress reactivity. J Clin Psychiatry. 2013;74:786–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York: Delta Trade; 1990. [Google Scholar]
- 18.Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clin Psychol Sci Pract . 2003;10:144–156. [Google Scholar]
- 19.Kiken LG, Shook NJ. Looking up: Mindfulness increases positive judgments and reduces negativity bias. Soc. Psychol. Personal. Sci. 2011;2:425–431. [Google Scholar]
- 20.Lengacher C, Johnso-Mallard V, Post-White J, Moscoso M, Jacobsen P, Klein T, Widen R, Fitzgerald S, Shelton M, Barta M, Goodman M, Cox C, Kip K, Johnson-Mallard V. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psychooncology . 2009;18:1261–1272. [DOI] [PubMed] [Google Scholar]
- 21.Mackenzie CS, Poulin PA, Seidman-Carlson R. A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Appl Nurs Res . 2006;19:105–109. [DOI] [PubMed] [Google Scholar]
- 22.Martin RA, Lefcourt HM. Sense of humor as a moderator of the relation between stressors and moods. J Pers Soc Psychol . 1983;45:1313–1324. [Google Scholar]
- 23.McCullough ME, Emmons RA, Tsang JA. The grateful disposition: A conceptual and empirical topography. J Pers Soc Psychol . 2002;82:112–127. [DOI] [PubMed] [Google Scholar]
- 24.McCullough ME, Tsang JA, Emmons RA. Gratitude in intermediate affective terrain: links of grateful moods to individual differences and daily emotional experience. J Pers Soc Psychol . 2004;86:295–309. [DOI] [PubMed] [Google Scholar]
- 25.Özkan S, Zale EL, Ring D, Vranceanu AM. Associations between pain catastrophizing and cognitive fusion in relation to pain and upper extremity function among hand and upper extremity surgery patients. Ann Behav Med . 2017:51:547-554. [DOI] [PubMed] [Google Scholar]
- 26.Pavot W, Diener E, Colvin CR, Sandvik E. Further validation of the Satisfaction With Life Scale; evidence for the cross-method convergence of well-being measures. J Pers Assess . 1991;57:149–161. [DOI] [PubMed] [Google Scholar]
- 27.Ring D, Kadzielski J, Fabian L, Zurakowski D, Malhotra LR, Jupiter JB. Self-reported upper extremity health status correlates with depression. J Bone Joint Surg Am . 2006;88:1983–1988. [DOI] [PubMed] [Google Scholar]
- 28.Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol . 1985;4:219–247. [DOI] [PubMed] [Google Scholar]
- 29.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol . 1994;67:1063–1078. [DOI] [PubMed] [Google Scholar]
- 30.Seligman MEP, Csikszentmihalyi M. Positive psychology: An introduction. Am Psychol . 2000;55:5–14. [DOI] [PubMed] [Google Scholar]
- 31.Simão C, Seibt B. Friendly touch increases gratitude by inducing communal feelings. Front. Psychol. 2015;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med . 2008;15:194–200. [DOI] [PubMed] [Google Scholar]
- 33.Talaei-Khoei M, Chen N, Ring D, Vranceanu A-M. Satisfaction with life moderates the indirect effect of pain intensity on pain interference through pain catastrophizing. J Consult Clin Psychol . 2018;86:231–241. [DOI] [PubMed] [Google Scholar]
- 34.Talaei-Khoei M, Fischerauer SF, Lee S-G, Ring D, Vranceanu A-M. Pain catastrophizing mediates the effect of psychological inflexibility on pain intensity and upper extremity physical function in patients with upper extremity illness. Pain Pract . 2016;17:129–140. [DOI] [PubMed] [Google Scholar]
- 35.Tyser AR, Beckmann J, Franklin JD, Cheng C, Hon SD, Wang A, Hung M. Evaluation of the PROMIS physical function computer adaptive test in the upper extremity. J Hand Surg Am . 2014;39:2047–2051. [DOI] [PubMed] [Google Scholar]
- 36.Van Leeuwen WF, Van Der Vliet QMJ, Janssen SJ, Heng M, Ring D, Vranceanu AM. Does perceived injustice correlate with pain intensity and disability in orthopaedic trauma patients? Injury. 2016;47:1212–1216. [DOI] [PubMed] [Google Scholar]
- 37.Veehof MM, Oskam MJ, Schreurs KMG, Bohlmeijer ET. Acceptance-based interventions for the treatment of chronic pain: A systematic review and meta-analysis. Pain. 2011;152:533–542. [DOI] [PubMed] [Google Scholar]
- 38.Vranceanu AM, Beks RB, Guitton TG, Janssen SJ, Ring D. How do orthopaedic surgeons address psychological aspects of illness? Arch Bone Jt Surg . 2017;5:2–9 [PMC free article] [PubMed] [Google Scholar]
- 39.Vranceanu AM, Cooper C, Ring D. Integrating patient values into evidence-based practice: Effective communication for shared decision-making. Hand Clin . 2009;25:83–96. [DOI] [PubMed] [Google Scholar]
- 40.Westenberg RF, Zale EL, Heinhuis TJ, Özkan S, Nazzal A, Lee S-G, Chen NC, Vranceanu A-M. Does a brief mindfulness exercise improve outcomes in upper extremity patients? A randomized controlled trial. Clin Orthop Relat Res . 2018;476:790–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zale EL, Ring D, Vranceanu A-M. The future of orthopaedic care: Promoting psychosocial resilience in orthopaedic surgical practices. J Bone Joint Surg Am . 2018;100:e89. [DOI] [PubMed] [Google Scholar]


