Abstract
Background
The choice of reconstructive procedure to restore limb function is challenging after internal hemipelvectomy. Hip transposition arthroplasty, also known as resection arthroplasty, removes a malignant or aggressive tumor of the pelvis and acetabulum after which the remaining femoral head is moved proximally to the lateral surface side of the sacrum or the underside of the resected ilium after internal hemipelvectomy. It may provide reasonable functional results and have some advantages such as lowering the risk of an infected implant compared with other reconstructions because no foreign implants are used. Hip transposition is generally managed with prolonged bed rest or immobilization postoperatively to stabilize the soft tissue surrounding the remaining femur. Because enabling patients to be mobile while the soft tissues heal might be advantageous, we reviewed our experience with an external fixation for this procedure.
Questions/purposes
(1) Does temporary external fixation facilitate postoperative physiotherapy in patients who undergo hip transposition arthroplasty? (2) What functional Musculoskeletal Tumor Society (MSTS) scores were achieved at short term in a small series of patients treated with hip transposition and temporary external fixation? (3) What were the complications of using external fixation in a small series of patients who received it for malignant tumors?
Methods
Between 2008 and 2012, we treated seven patients (three men and four women; median age, 37 years; age range, 18–53 years) with acetabular resection for malignant bone tumors; all were managed with a hip transposition, initially stabilized using external fixation. No other types of procedures were used for this indication in this period. Minimum followup in this retrospective study was 45 months, except for one patient who died at 18 months (range of followup duration, 18–90 months; median followup, 57 months), and no patients were lost to followup. The pins for external fixation were inserted into the affected side of the femur and the healthy contralateral ilium. External fixation was removed 6 weeks postoperatively and weightbearing was started at that time. Preoperative chemotherapy was administrated in four patients, but postoperative chemotherapy was delayed since it was given after external fixation removal in three patients. The postoperative rehabilitation course and functional results were assessed by chart review, functional results were determined using MSTS scores, tallied by physiotherapists who were not part of the surgical team, and complications were ascertained through chart review. Major complications were defined as complications that were treated with additional operations, such as deep infection, or ones that could cause severe postoperative dysfunction, such as nerve injury.
Results
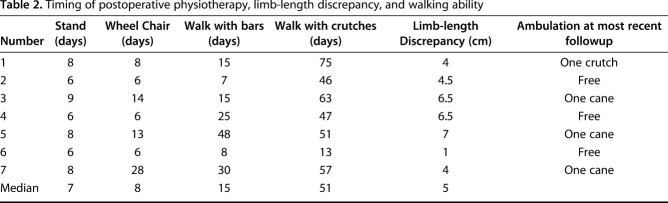
With temporary external fixation, standing next to a bed was achieved in median 7 days (range, 6–9 days) postoperatively, transferring to a wheel chair in median 8 days (range, 6–28 days), and gait training using parallel bars in median 15 days (range, 7–48 days). At most recent followup, three patients could walk without a crutch or cane, three could walk with a cane, and one could walk with a crutch. The median MSTS score at most recent followup (median, 57 months) was 63%. Two patients had complications that resulted in reoperations; one had a wound dehiscence, and one had an abdominal herniation that gradually developed, and which was reconstructed using polypropylene mesh 2 years after pelvic resection. Two patients had nerve palsies that recovered by the end of the first year. All patients had pin tract infections that resolved with nonsurgical approaches.
Conclusions
Hip transposition with temporary external fixation can stabilize the bone soft tissue after pelvic resection. Although we did not have a comparison group of patients, we believe that external fixation facilitates early postoperative physiotherapy and rehabilitation and provides good functional results without major surgical complications. Because it delays the resumption of chemotherapy, more patients with longer followup are needed to determine whether this will be associated with poorer oncologic results.
Level of Evidence
Level IV, therapeutic study.
Introduction
A variety of reconstructive and ablative approaches have been used to manage patients after acetabular resections for malignant tumors. Hindquarter (external) hemipelvectomy is an accepted surgical treatment for primary malignant pelvic tumors [4, 22]. However, this treatment has cosmetic and functional disadvantages because the loss of a limb is associated with a high proportion of morbidity. Although internal hemipelvectomy with tumor resection and lower extremity sparing has been performed during the last several decades, reconstructive approaches vary according to the complicated anatomical location of the pelvis, extent of resection, functional demands of the patient, and individual surgeon preference. Reconstructive options after acetabular tumor resection include iliofemoral arthrodesis or pseudoarthrodesis, combined use of hip arthroplasty with a massive allograft or a recycled bone, and use of a pelvic and saddle prosthesis [2, 5, 9, 11, 18, 26]. No particular reconstruction method has been shown to be superior to another nor, for that matter, superior to leaving the hip flail [3, 5, 16, 25]. The choice of a reconstructive procedure to restore limb function is also challenging, and there is a high risk of mechanical, infectious, and neurovascular complications after internal hemipelvectomy [1, 10, 13, 23, 24, 26, 27]. The use of implants such as allografts, arthroplasties, or both has been associated with a high likelihood of postoperative infection because of the extent of dissection, inadequate soft tissue coverage, and a large dead space [16]. The surgical time required for resection arthroplasty is usually shorter than that when an implant is used, and the technique is usually less demanding and possibly associated with a lower complication rate than are more complex reconstructive procedures.
Hip transposition is a reconstructive technique that stabilizes the bone and soft tissues after resection of the acetabulum without adding implants. The femoral head is moved proximally to the lateral side of the sacrum or the underside of the resected ilium after tumor resection [12, 16]. Hillman et al. [15] reported that hip transposition had the lowest risk of complications after acetabular resection compared with the use of a prosthesis alone or a prosthesis and an allograft. Another report suggests that hip transposition provides better quality of life and functional results compared with other types of reconstruction [16]. The absence of large implants and allografts may help to reduce surgical time and may decrease infection risk.
However, patients treated with hip transposition usually have been managed with immobilization in bed for 2 weeks followed by an additional cast or soft splint for 4 weeks postoperatively to stabilize the soft tissue surrounding the remaining femur [12], and this is an obvious disadvantage. Because of this, we began to apply temporary external fixation in patients who underwent hip transposition after resection of a periacetabular tumor to stabilize the new articulation and facilitate early postoperative physiotherapy. To our knowledge, results using an external fixator for this indication have not been reported.
We therefore asked: (1) Does temporary external fixation facilitate postoperative physiotherapy in patients who undergo hip transposition arthroplasty? (2) What functional Musculoskeletal Tumor Society (MSTS) scores were achieved at short term in a small series of patients treated with hip transposition and temporary external fixation? (3) What were the complications of using external fixation in a small series of patients who received it for malignant tumors?
Patients and Methods
Study Design and Setting
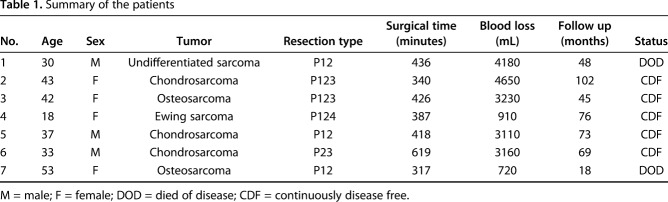
Between 2008 and 2012, we treated seven patients (three men and four women; median age, 37 years; age range, 18–53 years) with acetabular resection for malignant bone tumors; all were managed using a hip transposition, initially stabilized using external fixation (Table 1). Minimum followup in this retrospective study was 51 months, except for one patient who died at 18 months (range of followup duration, 18–102 months; median followup, 69 months), and no patients were lost to followup. The study was approved by the institutional review board of our institute.
Table 1.
Summary of the patients
During this time period, we did not use any other form of reconstruction in patients who underwent acetabular resection for a sarcoma. Our indication for hip transposition arthroplasty with temporary external fixation was simply a malignant primary bone tumor involving or located close to the acetabulum and for which we needed to excise the acetabulum completely (including at least P2 resection) to achieve a tumor-free margin. There were no current or previous patients who were treated this way who did not have external fixation for comparison.
Demographics, Description of Study Population
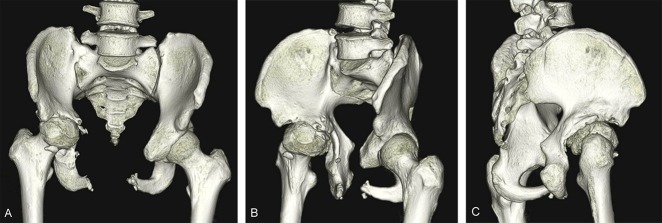
The pathological diagnoses were three chondrosarcomas, two osteosarcomas (one conventional and one postradiation), one Ewing sarcoma, and one undifferentiated sarcoma. Preoperative and postoperative chemotherapy was given to the patients with the two osteosarcomas (modified Neoadjuvant Chemotherapy for Osteosarcoma [NECO-95] protocol), the Ewing sarcoma (EUROpean Ewing tumour Working Initiative of National Groups [EURO-EWING] Ewing Tumour Studies 1999 protocol), and the undifferentiated sarcoma (ifosfamide 10 g/m2/Days1-5 and doxorubicin 60 mg/m2/Days 1-2). Radiotherapy (54.4 Gy) was conducted preoperatively on the Ewing sarcoma. One patient with osteosarcoma (Patient 7) underwent preoperative selective arterial embolization to reduce intraoperative blood loss. Acetabular lesions were excised according to the classification system proposed by Enneking and Dunham (Fig. 1) [7], describing the various subtypes based on the portion of bone removed. A P12 resection was performed on three patients, P123 resection on two, P124 resection on one, and P23 resection on one.
Fig. 1.
A classification system proposed by Enneking and Dunham [8] was generally used for pelvic tumor resection.
Description of Experiment, Treatment, or Surgery
All patients underwent en bloc resection with an adequate wide margin, planned previously according to Kawaguchi’s classification guidelines [19]. The patient was placed in a loose lateral position, which allows the patient to be flipped forward and backward to provide better visualization of the front and back of the pelvis. The extended ilioinguinal or iliofemoral approach was used depending on the involvement of the anterior part of the pelvis.
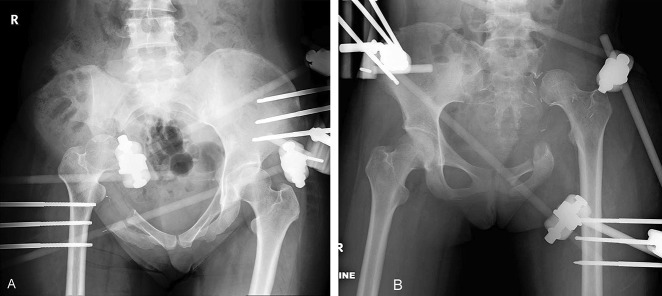
After tumor resection, a modified hip transposition procedure, as reported by Gebert et al. [12], was conducted for resection hip arthroplasty (Fig. 2). The femoral head was moved proximally to the lateral surface side of the sacrum or the underside of the resected ilium. The remaining soft tissue, such as muscle on the femur, sacrum, or remaining pelvis, was sutured to stabilize the proximally-moved femoral head on the sacrum or the remaining ilium. If enough of the gluteus maximus and/or medius remained, the suture of those muscles to the abdominal wall muscles could result in good stability. We avoided using a polyethylene terephthalate mesh tube, which can be used to reconstruct the capsule of the new hip, as reported previously [12, 15], because artificial materials present a possible cause of deep infection. After skin closure, the patient was placed in the supine position. The pins for external fixation were inserted into the affected side of the femur (subtrochanteric region) and the healthy contralateral ilium (iliac crest) under an image intensifier (Fig. 3). The affected femoral head was pressed to the lateral surface of the sacrum or the underside of the resected ilium, and external fixation was applied and tightened (Fig. 4), with the new hip articulation in 20° of flexion and 20° of abduction. The median total surgical duration was 418 minutes (range, 317–619 minutes), and the median duration to apply external fixation was 39 minutes (range, 37–50 minutes). The median intraoperative blood loss was 3160 mL (range, 720–4650 mL).
Fig. 2.

This scheme illustrates hip transposition arthroplasty.
Fig. 3 A-B.
An AP radiograph at 3 weeks postoperatively of (A) a 43-year-old patient with chondrosarcoma (Patient 2) and (B) an 18-year-old patient with Ewing sarcoma (Patient 4), which show external fixation with pins inserted into the affected femur and the contralateral healthy ilium.
Fig. 4.

This postoperative photograph demonstrates the appearance of external fixation.
Aftercare
Patient who underwent external fixation started physiotherapy by transferring to a wheelchair and performing gait training with 10-kg partial weightbearing on the affected limb immediately after surgery. External fixation removal was planned 6 weeks after tumor resection. Pin tracts were managed with cleaning using wound antiseptic and dressing changes every 1 or 2 days by doctors or nurses. At the time of removal, the stability between the femoral head and remaining pelvis was assessed with an image intensifier. After external fixation removal, flexion of the new hip articulation and full weightbearing on the affected leg was sufficient to begin physiotherapy. Because the two patients (one osteosarcoma and one Ewing sarcoma) who were supposed to get postoperative chemotherapy demonstrated good response to preoperative chemotherapy and there would be some risks of deep infection due to early start of postoperative chemotherapy, we decide, along with these patients and their families, that chemotherapy should be given immediately after external fixation removal. One patient with undifferentiated sarcoma simply refused postoperative chemotherapy until he could move around by himself.
Variables, Outcome Measures, Data Sources, and Bias
Postoperative functional recovery, such as standing, transferring to a wheelchair, and gait training, was abstracted by chart review performed by physiotherapists or occupational therapists in charge of the patient’s rehabilitation.
Patients were followed every 3 to 6 months, mainly so we could evaluate for local and distant relapse with imaging. On the same day of their visit to our clinic, they presented to the department of rehabilitation to undergo physical, psychological, and social examinations. A physiotherapist or occupational therapist measured limb length discrepancy and function, and we analyzed data collected from the patient records. The MSTS scoring system for the lower limb [8] was used to assess functional outcomes at the outpatient clinic every 3 to 6 months. The physiotherapist or occupational therapist evaluated the MSTS score. The MSTS scoring system is based on the analysis of six factors: pain, emotional acceptance, restriction, walking distance, support, and gait. Each variable is given a value ranging from 0 to 5 according to specific criteria. The overall score is expressed as the sum of all variables, and is then converted into a percentage of the maximum possible score.
Major complications were defined as a complication that was treated with an additional operation, such as deep infection, or that could cause severe postoperative dysfunction, like a nerve injury. Minor complications were defined as a complication that was treated conservatively, such as superficial wound infection, or that was not directly related to postoperative function. Complications were abstracted by chart review performed by the treating surgeons (TK, TF).
Oncologic Results
A postoperative evaluation of the surgical margin demonstrated an adequately wide margin (at least 2 cm in width) in six patients and a marginal margin in one (Patient 7). The patient with osteosarcoma (Patient 7) had local recurrence 8 months postoperatively, which was treated with carbon ion radiotherapy; however, this patient developed multiple lung metastases. The patient with an undifferentiated sarcoma (Patient 1) developed multiple lung metastases 33 months after tumor resection and underwent three metastasectomies. The two patients with lung metastases died of their disease at 18 and 48 months after primary tumor resection. These two patients were functionally assessed at the time of the most recent outpatient clinic visit. The remaining five patients were continuously disease-free.
Results
Timing of postoperative physiotherapy varied for each patient (Table 2). The patients treated with temporary external fixation were able to stand next to a bed within median 7 days (range, 6–9 days) after surgery, transfer to a wheel chair within median 8 days (range, 6–28 days), and begin gait training using parallel bars within median 15 days (range, 7–48 days) (Fig. 5). External fixation was removed under general anesthesia at 42 days (6 weeks) after surgery. At the time external fixation was removed, the image intensifier demonstrated that all new articulations between the femoral head and resected surface of the pelvis were sufficiently stable to allow passive mobilization at 90° flexion and 40° abduction. After removal, all patients started gait training with full weightbearing and continued postoperative physiotherapy. Gait training with two crutches was started within median 51 days (range, 13–75 days) after the initial surgery.
Table 2.
Timing of postoperative physiotherapy, limb-length discrepancy, and walking ability
Fig. 5 A-B.
(A) One patient sitting on a wheel chair with external fixation is shown here. (B) Another patient is shown performing a walking exercise using parallel bars at the time of postoperative physiotherapy with external fixation.
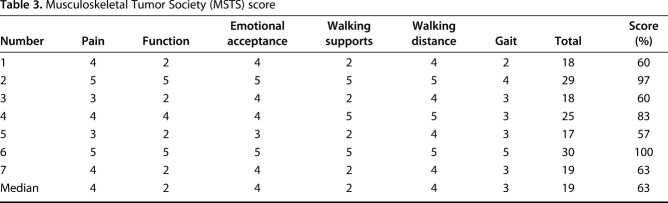
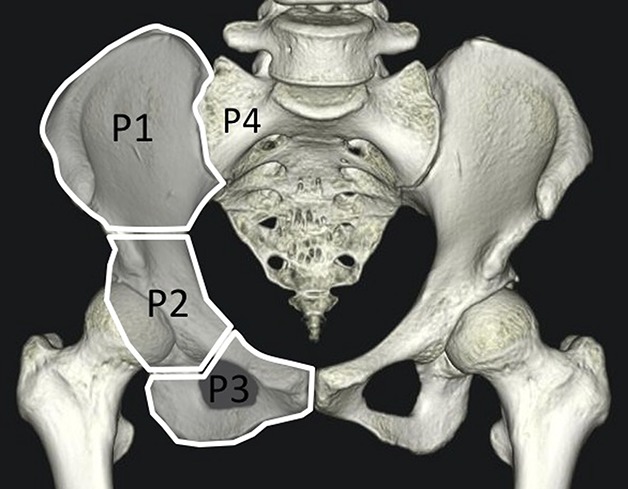
Median MSTS score was 63% (range, 57%–100%) (Table 3). Postoperative function improved until about 1 year after surgery, and since then MSTS score showed little change in all patients. All patients remained ambulatory after surgery and walked into our outpatient clinic at the latest followup examination (median 69 months postoperatively; Fig.6). Three patients were able to ambulate without a cane or crutch and two could walk using a heightened shoe heel because of limb length discrepancy due to the transposition of the femoral head (Fig. 7). The remaining four patients used one crutch or cane with an elevated shoe heel. In our series, there was no deterioration of MSTS score during the followup period. Patient 6, who underwent P23 resection with the round osteotomy around the acetabulum like rotational acetabular osteotomy, showed 100% of MSTS score (Fig. 8).
Table 3.
Musculoskeletal Tumor Society (MSTS) score
Fig. 6 A-C.
(A) An AP view of a radiograph of Patient 2 taken 1 month after removal of external fixation. An AP view of the same patient at 1 year after surgical resection (B), and at 4 years after surgical resection (C) show that the femoral head slightly indicated an osteoarthritic change at 4 years after surgery. The patient is able to walk without a crutch or cane at the most recent followup (9 years postoperatively).
Fig. 7 A-B.
Three-dimensional CT imaging show the limb length discrepancy of (A) Patient 2 at 9 years postoperatively and of (B) Patient 4 at 6 years postoperatively.
Fig. 8 A-C.
An AP view (A) and oblique view (B, C) of three-dimensional CT imaging show semicircular resection of the acetabulum with the remaining posterior part of the posterior column of the pelvis at 2 years 9 months postoperatively of Patient 6.
Two patients had complications resulting in reoperations. One patient had a wound dehiscence; this patient had preoperative chemotherapy and radiotherapy and underwent surgical débridement to treat the dehiscence. Another patient had an abdominal herniation that developed gradually; it was reconstructed using polypropylene mesh 2 years after pelvic resection. Transient nerve palsy was identified postoperatively in two patients; one had femoral nerve palsy and one had peroneal nerve palsy, both of which recovered within 1 year of surgery. All patients demonstrated pin tract infections that healed after débridement and simple suture after external fixation removal. No patients developed a deep infection related to pelvic resection or temporary external fixation. The median limb length discrepancy among all patients was 5 cm (range, 1–7cm), and five of the seven patients used an elevated shoe heel (median 5cm, range; 3–6.5cm) when walking.
Discussion
Hip transposition arthroplasty, one type of resection arthroplasty, is a good option for some patients given the frequent complications associated with prosthetic reconstructions. However, this procedure is usually accompanied by a lengthy convalescence period during which time the patient can hardly walk, which itself can cause complications associated with recumbency [6, 12, 15, 25]. We therefore began to use external fixation in these patients. However, results with this approach have not, to our knowledge, been reported. In the present study, hip transposition with temporal external fixation led to good postoperative function such as reasonably quick mobilization and decent MSTS scores at about 4 years. There were some complications, although they were less common than one would expect from major surgery.
This study had several important limitations. First, there was no comparison group or randomization in this study. We described patients who underwent external fixation, and we cannot compare our result of hip transposition using temporary external fixation with the results of that without external fixation, or of other types of periacetabular reconstructions, because all patients included in this study had a single clinical indication and only one treatment was used for this indication. Owing to the small number of patients with pelvic tumors involving the acetabulum who underwent internal hemipelvectomy, we are unable to provide a control group for comparison. Multicenter trials may be able to compare groups of patients in the future. Second, the small number of patients is not likely to adequately represent uncommon complications and outcomes, which are less likely to be detected in a study of this size.
In the present study, the patients were able to mobilize the day after the surgery, stand next to a bed with partial weightbearing at a median 7 days after surgery, and transfer to a wheelchair by a median 8 days after surgery. Temporary external fixation for pelvic reconstruction combined with resection arthroplasty was first reported by Kusuzaki et al. [20]. Their patients were able to move using a walker 3 weeks postoperatively, and after the external fixator was removed at 6 weeks, the patients used an additional hip abduction brace and began to walk with double crutches at 10 weeks. In their series of five patients, three could walk without a cane or brace. External fixation can provide adequate stability between the femoral head and remaining pelvis that is sufficient to allow early rehabilitation, which appears to be an improvement over the 4 to 6 weeks of bedrest that has been reported [6, 12]. Assessment using an image intensifier at 6 weeks showed that the transferred femoral head was located in the same position during its traction, flexion, and abduction; thus, the external fixator was removed at that time. All patients then began physiotherapy with full weightbearing, without the use of a hip brace. Temporary external fixation can effectively facilitate early postoperative physiotherapy and stabilize the new hip articulation after hip transposition.
We found MSTS scores to be generally good (median, 63%; range 57%–100%) at a median followup of nearly 5 years. Hoffmann et al. [16] evaluated postoperative function on 20 patients treated with hip transposition and reported mean 61% of MSTS score at median followup of 69 months, which is similar to the present study. They concluded that hip transposition resulted in better function and fewer complications than other procedures such as prosthetic reconstruction. The joint capsule for hip transposition arthroplasty was originally reconstructed with a polyethylene terephthalate mesh tube [16], and inducing local scarring of the soft tissue could also facilitate stable reconstruction [12]. Although we did not use the mesh tube, hip transposition with temporary external fixation might provide good postoperative function without prolonged bed rest and brace.
We had several serious complications, including two patients who underwent further surgery (one for a wound dehiscence, and one for a large abdominal hernia), as well as two patients who had neurapraxias that resolved within a year of surgery. We believe that these major complications were caused by surgical resection of pelvic tumor and hip transposition, not by temporary external fixation. The current study also demonstrated that the application of temporary external fixation without the use of a tube resulted in no postoperative deep wound infections in our patients, even in those treated with high-dose adjuvant chemotherapy. This is in stark contrast to one previous study, in which infection was seen in a large proportion of patients treated with hip transposition and reconstruction with polyethylene terephthalate mesh tubes [13]. They reported postoperative deep infection in 10 of 36 Type IIa hip transposition arthroplasties, resulting in mesh tube removal in five patients. Other studies regarding resection arthroplasty or flail hip without the use of artificial mesh reported no postoperative deep infection [17, 25]. Bearing in mind that the high infection rate in that previous series may have partially been caused by the use of an artificial tube, and because external fixation without the tube could provide adequate stability for a new hip articulation, we did not use tubes. Other studies have found high proportion of complications ranging from 55% to 77% of patients [1, 2, 3, 5, 13, 14, 18, 21]; main documented complications are wound healing problems, implant loosening, and deep infection. One study on 62 patients with hip transposition demonstrated 14 wound healing problems, 18 deep infection, six neurological deficits and 25 revision surgeries [13]. The incidence of complications in pelvic tumor surgery is generally higher than that in extremity tumor surgery, since pelvic tumor surgery has a longer operative time and more extensive soft tissue dissection, and results in massive blood loss.
Our study showed that temporary external fixation can yield good stability between the femoral head and remaining pelvis and facilitate postoperative physiotherapy in the early postoperative period in patients treated with hip transposition after pelvic sarcoma resection. The MSTS scores at a median of nearly 5 years after surgery reflected good function among our small group of patients, and the complications we observed were not surprising in the setting of major pelvic surgery for a life-threatening diagnosis. Future studies might evaluate the long-term functional outcome and complications in more patients treated with hip transposition and temporal external fixation and the possibility of reducing the time required for temporal external fixation. Because it delays the resumption of chemotherapy, more patients with longer followup are also needed to determine whether this technique might be associated with poorer oncologic results. Since it might be extremely difficult to analyze clinical outcome sufficiently on such rare disease as pelvic sarcoma, a multicenter study should be conducted to compare each group of reconstructions.
Acknowledgments
We thank all the staff (doctors, physiotherapists, and occupational therapists) at the Department of Rehabilitation, Okayama University Hospital, Okayama, Japan, who conducted physiotherapy and rehabilitation of patients treated with hip transposition for helping us study their functional outcome.
Footnotes
Each author certifies that neither he, nor any member of his immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Okayama University Hospital, Okayama, Japan.
References
- 1.Angelini A, Drago G, Trovarelli G, Calabro T, Ruggieri P. Infection after surgical resection for pelvic bone tumors: an analysis of 270 patients from one institution. Clin Orthop Relat Res. 2014;472:349-359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bell RS, Davis AM, Wunder JS, Buconjic T, McGoveran B, Gross AE. Allograft reconstruction of the acetabulum after resection of stage-IIB sarcoma. Intermediate-term results. J Bone Joint Surg Am. 1997;79:1663-1674. [DOI] [PubMed] [Google Scholar]
- 3.Brown TS, Salib CG, Rose PS, Sim FH, Lewallen DG, Abdel MP. Reconstruction of the hip after resection of periacetabular oncological lesions: a systematic review. Bone Joint J . 2018;100-B(1 Supple A):22-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carter SR, Eastwood DM, Grimer RJ, Sneath RS. Hindquarter amputation for tumours of the musculoskeletal system. J Bone Joint Surg Br . 1990;72:490-493. [DOI] [PubMed] [Google Scholar]
- 5.Dominkus M, Darwish E, Funovics P. Reconstruction of the pelvis after resection of malignant bone tumours in children and adolescents. Recent Results Cancer Res. Fortschritte der Krebsforschung. Progres dans les recherches sur le cancer. 2009;179:85-111. [DOI] [PubMed] [Google Scholar]
- 6.Eilber FR, Grant TT, Sakai D, Morton DL. Internal hemipelvectomy--excision of the hemipelvis with limb preservation. An alternative to hemipelvectomy. Cancer. 1979;43:806-809. [DOI] [PubMed] [Google Scholar]
- 7.Enneking WF, Dunham WK. Resection and reconstruction for primary neoplasms involving the innominate bone. J Bone Joint Surg Am. 1978;60:731-746. [PubMed] [Google Scholar]
- 8.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993:241-246. [PubMed] [Google Scholar]
- 9.Farfalli GL, Albergo JI, Ritacco LE, Ayerza MA, Muscolo DL, Aponte-Tinao LA. Oncologic and clinical outcomes in pelvic primary bone sarcomas treated with limb salvage surgery. Musculoskelet Surg. 2015;99:237-242. [DOI] [PubMed] [Google Scholar]
- 10.Fisher NE, Patton JT, Grimer RJ, Porter D, Jeys L, Tillman RM, Abudu A, Carter SR. Ice-cream cone reconstruction of the pelvis: a new type of pelvic replacement: early results. J Bone Joint Surg Br. 2011;93:684-688. [DOI] [PubMed] [Google Scholar]
- 11.Fuchs B, O'Connor MI, Kaufman KR, Padgett DJ, Sim FH. Iliofemoral arthrodesis and pseudarthrosis: a long-term functional outcome evaluation. Clin Orthop Relat Res. 2002:29-35. [DOI] [PubMed] [Google Scholar]
- 12.Gebert C, Gosheger G, Winkelmann W. Hip transposition as a universal surgical procedure for periacetabular tumors of the pelvis. J Surg Oncol. 2009;99:169-172. [DOI] [PubMed] [Google Scholar]
- 13.Gebert C, Wessling M, Hoffmann C, Roedl R, Winkelmann W, Gosheger G, Hardes J. Hip transposition as a limb salvage procedure following the resection of periacetabular tumors. J Surg Oncol. 2011;103:269-275. [DOI] [PubMed] [Google Scholar]
- 14.Han I, Lee YM, Cho HS, Oh JH, Lee SH, Kim HS. Outcome after surgical treatment of pelvic sarcomas. Clin Orthop Surg. 2010;2:160-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hillmann A, Hoffmann C, Gosheger G, Rodl R, Winkelmann W, Ozaki T. Tumors of the pelvis: complications after reconstruction. Arch Orthop Trauma Surg. 2003;123:340-344. [DOI] [PubMed] [Google Scholar]
- 16.Hoffmann C, Gosheger G, Gebert C, Jurgens H, Winkelmann W. Functional results and quality of life after treatment of pelvic sarcomas involving the acetabulum. J Bone Joint Surg Am. 2006;88:575-582. [DOI] [PubMed] [Google Scholar]
- 17.Huth JF, Eckardt JJ, Pignatti G, Eilber FR. Resection of malignant bone tumors of the pelvic girdle without extremity amputation. Arch Surg. 1988;123:1121-1124. [DOI] [PubMed] [Google Scholar]
- 18.Jansen JA, van de Sande MA, Dijkstra PD. Poor long-term clinical results of saddle prosthesis after resection of periacetabular tumors. Clin Orthop Relat Res. 2013;471:324-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kawaguchi N, Ahmed AR, Matsumoto S, Manabe J, Matsushita Y. The concept of curative margin in surgery for bone and soft tissue sarcoma. Clin Orthop Relat Res. 2004:165-172. [DOI] [PubMed] [Google Scholar]
- 20.Kusuzaki K, Shinjo H, Kim W, Nakamura S, Murata H, Hirasawa Y. Resection hip arthroplasty for malignant pelvic tumor. Outcome in 5 patients followed more than 2 years. Acta Orthop Scand. 1998;69:617-621. [DOI] [PubMed] [Google Scholar]
- 21.Langlais F, Lambotte JC, Thomazeau H. Long-term results of hemipelvis reconstruction with allografts. Clin Orthop Relat Res. 2001:178-186. [DOI] [PubMed] [Google Scholar]
- 22.Masterson EL, Davis AM, Wunder JS, Bell RS. Hindquarter amputation for pelvic tumors. The importance of patient selection. Clin Orthop Relat Res. 1998:187-194. [PubMed] [Google Scholar]
- 23.O'Connor MI, Sim FH. Salvage of the limb in the treatment of malignant pelvic tumors. J Bone Joint Surg Am. 1989;71:481-494. [PubMed] [Google Scholar]
- 24.Schwameis E, Dominkus M, Krepler P, Dorotka R, Lang S, Windhager R, Kotz R. Reconstruction of the pelvis after tumor resection in children and adolescents. Clin Orthop Relat Res. 2002:220-235. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz AJ1, Kiatisevi P, Eilber FC, Eilber FR, Eckardt JJ. The Friedman-Eilber resection arthroplasty of the pelvis. Clin Orthop Relat Res. 2009;467:2825-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sys G, Uyttendaele D, Poffyn B, Verdonk R, Verstraete L. Extracorporeally irradiated autografts in pelvic reconstruction after malignant tumour resection. Int Orthop. 2002;26:174-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ueda T, Kakunaga S, Takenaka S, Araki N, Yoshikawa H. Constrained total hip megaprosthesis for primary periacetabular tumors. Clin Orthop Relat Res. 2013;471:741-749. [DOI] [PMC free article] [PubMed] [Google Scholar]