Abstract
Background
Osteoarthritis is common and debilitating, in part because it often affects more than one large weightbearing joint. The likelihood of undergoing more than one total joint arthroplasty has not been studied in a heterogeneous, multicenter population in the United States.
Questions/purposes
We used prospectively collected data of patients with osteoarthritis from the multicenter Osteoarthritis Initiative (OAI) project to ask (1) What is the likelihood of a subsequent THA or TKA after primary TKA or THA? (2) What risk factors are associated with undergoing contralateral TKA after primary TKA?
Methods
Longitudinally maintained data from the OAI were used to identify 332 patients who underwent primary TKA and 132 patients who underwent primary THA for osteoarthritis who did not have a previous TKA or THA in this retrospective study. OAI was a longitudinal cohort study of knee osteoarthritis conducted at five centers in the United States (Columbus, OH, USA; Pittsburgh, PA, USA; Baltimore, MD, USA; Pawtucket, RI, USA; and San Francisco, CA, USA). In this study, the mean follow-up time was 4.0 ± 2.3 years, with 24% (112 of 464) followed for less than 2 years. The primary outcome was the cumulative incidence of subsequent arthroplasty calculated using the Kaplan-Meier method. Age, BMI, gender, and contralateral Kellgren-Lawrence grade, medial joint space width, and hip-knee-ankle angles were modeled as risk factors of contralateral TKA using Cox proportional hazards.
Results
Using the Kaplan-Meier method, at 8 years the cumulative incidence of contralateral TKA after the index TKA was 40% (95% CI 31 to 49) and the cumulative incidence of any THA after index TKA was 13% (95% CI 5 to 21). The cumulative incidence of contralateral THA after the index THA was 8% (95% CI 2 to 14), and the cumulative incidence of any TKA after index THA was 32% (95% CI 15 to 48). Risk factors for undergoing contralateral TKA were younger age (HR 0.95 for each year of increasing age [95% CI 0.92 to 0.98]; p = 0.001) and loss of medial joint space width with a varus deformity (HR 1.26 for each 1 mm loss of joint space width at 1.6o varus [1.06 to 1.51]; p = 0.005).
Conclusion
Patients who underwent TKA or THA for osteoarthritis had a high rate of subsequent joint arthroplasties in this study conducted at multiple centers in the United States. The rate of subsequent joint arthroplasty determined in this study can be used to counsel patients in similar settings and institutions, and may serve as a benchmark to assess future osteoarthritis disease-modifying interventions.
Level of Evidence
Level III, therapeutic study.
Introduction
Osteoarthritis (OA) is a leading cause of disability in the United States and worldwide, affecting nearly half of the population [4, 12]. For knee and hip OA, total joint arthroplasty reduces pain and improves function, and has a low failure rate, and leads to an improved overall quality of life [1, 14]. In 2010, approximately 7 million Americans were living with a total joint arthroplasty of the knee or hip [9], and more than 620,000 TKAs and 260,000 THAs were performed for OA [23]. The prevalence of OA is increasing because of an aging population and the increasing prevalence of obesity, and it is presumed that the number of patients undergoing total joint arthroplasty every year will rise as well [8, 12, 23].
Often, multiple joints are affected in patients with OA, with approximately 80% of patients with knee or hip OA on one side having radiographic evidence of OA on the contralateral side [5]. Accordingly, reports show a 36% to 46% likelihood of contralateral TKA after the initial TKA [11, 15, 16, 18, 21] and a 17% to 35% likelihood of contralateral THA after the initial THA at 10 years postoperatively [16, 17, 19, 21]. In the context of TKA and THA, contralateral arthroplasty of the cognate joint (the same joint on the opposite side) is more commonly performed than arthroplasty of a non-cognate joint [3]. However, the validity and generalizability of these studies may be limited. Prior studies have typically analyzed retrospectively collected data, were conducted by a single surgeon or institution [11, 15, 20, 21], studied homogeneous populations [3, 16], or had limited follow-up [22]. Understanding the likelihood of a subsequent total joint arthroplasty can help guide patient care and management after the first arthroplasty and can serve as a benchmark for assessing the efficacy of disease-modifying interventions.
We therefore sought to use multicenter prospectively collected data from the Osteoarthritis Initiative (OAI) database to ask, (1) What is the likelihood of a subsequent THA or TKA after primary TKA or THA? (2) What risk factors are associated with undergoing contralateral TKA after primary TKA?
Patients and Methods
Data Source
Data from this retrospective study were longitudinally maintained as part of the OAI [13]. The OAI was a study of knee osteoarthritis that included 4796 men and women aged 45 to 79 years who had or were at risk of having symptomatic tibiofemoral OA at five US centers (Columbus, OH, USA; Pittsburgh, PA, USA; Baltimore, MD, USA; Pawtucket, RI, USA; and San Francisco, CA, USA). OAI was funded by the NIH, GlaxoSmithKline (Brentford, UK), Merck & Co. (Kenilworth, NJ, USA), Novartis Pharmaceuticals Co. (Basel, Switzerland), and Pfizer (New York, NY, USA). Detailed inclusion and exclusion criteria are described in the OAI study protocol [13]. Patients were recruited from February 2004 to May 2006 and were observed for 9 years. Investigators at each site collected medical history questionnaires annually. Images were collected annually for the first 4 years and biannually until study completion. The OAI used the annual patient questionnaires and adjudication through medical records to track TKAs and THAs throughout the study period. The OAI database is available for public access; therefore, this study was deemed exempt from approval by the various institutional review boards.
Study Design
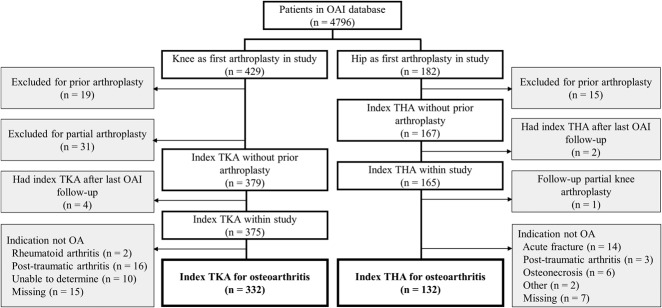
We reviewed 611 patients participating in the OAI study who underwent primary TKA or THA. We excluded patients if they underwent total joint arthroplasty before enrollment in the OAI study (6%, 34 of 611), underwent partial knee arthroplasty (5%, 30), had total joint arthroplasty after the last OAI follow-up (1%, 6 of 611), or if OA was not the primary diagnosis (for example, acute fracture) before the first joint arthroplasty (13%, 77 of 611). Partial knee arthroplasties were excluded to increase internal validity of the study. Thus, 332 patients who underwent primary TKA and 132 patients who underwent primary THA were included for analysis in this study (Fig. 1).
Fig. 1.
This figure shows patient selection from the OAI cohort.
Measured Outcomes and Variables
The primary outcome in this study was the Kaplan-Meier cumulative incidence of a subsequent arthroplasty after the index total joint arthroplasty (either TKA or THA). The date of surgery for the primary procedures was treated as the index time, after which the time until a cognate contralateral total joint arthroplasty or arthroplasty of a non-cognate joint (either ipsilateral or contralateral) was measured. Patients with follow-up less than the maximum who did not undergo a subsequent surgery were right-censored at their last follow-up visit with the OAI.
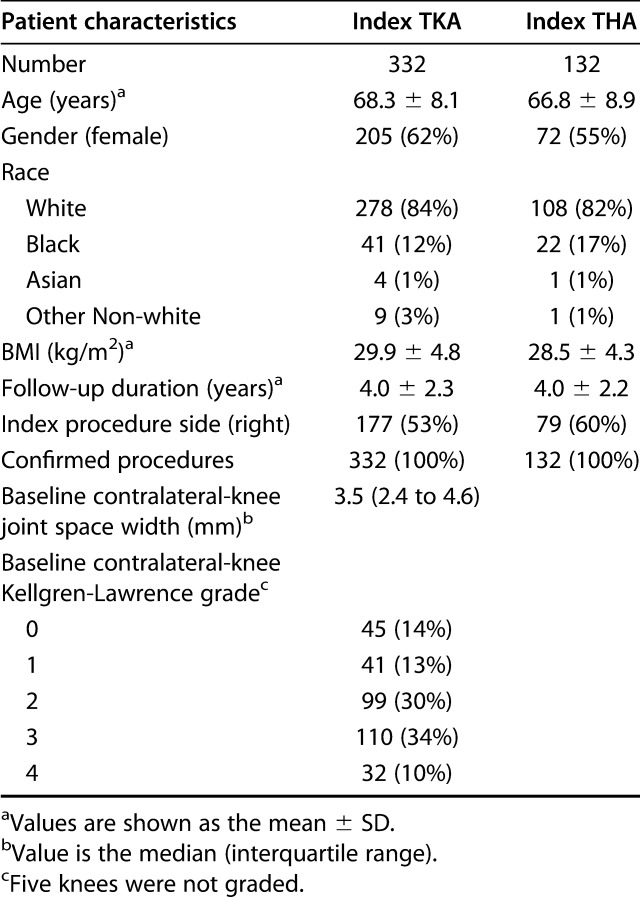
Patient demographic information and clinical data were extracted from the OAI database for inclusion in the analysis (Table 1). Age, gender, race, and BMI were collected for each patient as well as Kellgren-Lawrence grade, joint space width, and hip-knee-ankle angle of the contralateral knee after the index TKA. The most recent Kellgren-Lawrence grade, joint space width, and hip-knee-ankle angle measurements of the contralateral knee before the first TKA were used. The Kellgren-Lawrence grade is a categorical variable (range 0 to 4) that describes the severity of radiographic OA [7] and was evaluated using serial radiographs by trained readers as part of the OAI. The tibiofemoral joint space width is commonly used to quantify the progression of OA and represents the extent of articular cartilage loss [6]. The joint space width was assessed by the OAI with a validated protocol using serial fixed flexion radiographs and measured digitally at different points in the joint [2]. The minimum medial compartment joint space width was included for analysis. Hip-knee-ankle angles to assess alignment of the knee were evaluated up to the 48-month visit using a weightbearing AP radiograph.
Table 1.
Characteristics of patients in the index TKA and THA groups
Statistical Analysis
The cumulative incidence of subsequent arthroplasty after the index TKA or THA was calculated using the Kaplan-Meier method, which we selected instead of a competing risks estimator because only 3% (14 of 464) of the patients died before undergoing a subsequent arthroplasty.
To identify risk factors of contralateral TKA after the index TKA, we constructed a Cox proportional hazards model. The model assessed the association between the contralateral Kellgren-Lawrence grade, contralateral joint space width, and contralateral hip-knee-ankle angle and the time to contralateral TKA after adjusting for age, gender, and BMI. Multicollinearity was assessed with variance inflation factors, with a variance inflation factor greater than 5 indicating collinearity. The assumptions of linearity in the log hazard and proportional hazards model were assessed with martingale residuals and standardized score processes, respectively. A priori, we investigated the possibility that the joint space width depends on the hip-knee-ankle angle, which we explored using a cross-product term in the model. The Kellgren-Lawrence grade was included as a numeric variable in the primary model; however, to explore the impact of this decision on the results, we performed a sensitivity analysis, fitting the model with the Kellgren-Lawrence grade as a five-level categorical variable. Wald tests were used to assess predictors at a significance level of 0.05. The cumulative incidence of subsequent surgery and hazard ratios are reported with 95% confidence intervals. The statistical analysis was performed using JMP Pro 14.1.0 or SAS 9.4 (SAS Institute Inc, Cary, NC, USA).
The Cox proportional hazards model predicted the time to contralateral TKA after the index TKA (p < 0.001), and because of missing measurements, included 246 index TKAs (74% of all index TKAs) with 68 contralateral TKAs.
Results
Likelihood of Subsequent Arthroplasty after Primary TKA or THA
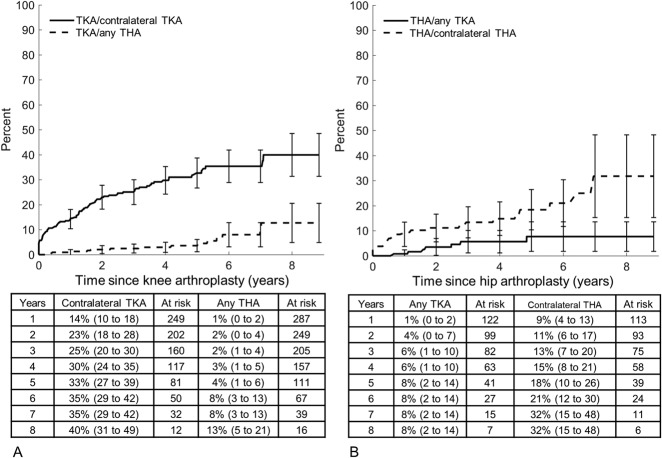
Using the Kaplan-Meier method, the cumulative incidence of contralateral TKA was 14% at 1 year (95% CI 10 to 18), 33% at 5 years (95% CI 27 to 39), and 40% at 8 years after index TKA (95% CI 31 to 49) (Fig. 2A). The cumulative incidence of any THA was 1% at 1 year (95% CI 0 to 2), 4% at 5 years (95% CI 1 to 6), and 13% at 8 years (95% CI 5 to 21). After 332 index TKAs performed to treat knee OA, there were 93 contralateral TKAs and 15 THAs during the study period. The mean follow-up time was 4.0 ± 2.3 years with 24% (81 of 332) followed for less than two years (Table 1).
Fig. 2 A-B.
This figure shows the patient’s likelihood of undergoing subsequent arthroplasty after (A) the index TKA and (B) the index THA. Error bars indicate 95% CIs. Values in charts are the rate (95% CI).
With the Kaplan-Meier method, the cumulative incidence of contralateral THA was 9% at 1 year (95% CI 4 to 13), 18% at 5 years (95% CI 10 to 26), and 32% at 8 years after the index THA (95% CI 15 to 48) (Fig. 2B). The cumulative incidence of any TKA was 1% at 1 year (95% CI 0 to 2), 8% at 5 years (95% CI 2 to 14), and 8% at 8 years (95% CI 2 to 14). After 132 index THAs performed to treat hip OA, there were 22 contralateral THAs and seven TKAs. The mean follow-up time was 4.0 ± 2.2 years with 23% (31 of 132) followed for less than 2 years (Table 1).
Risk Factors for Subsequent Arthroplasty
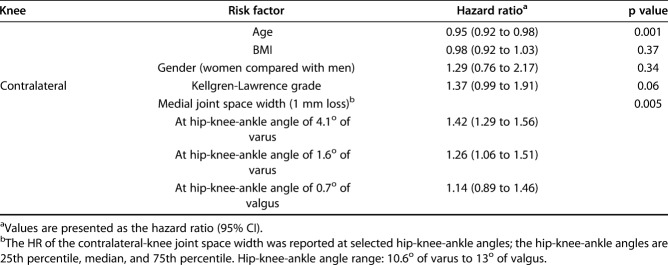
Younger age and loss of the medial joint space width in patients with varus knee alignment were identified as risk factors of contralateral TKA (Table 2). For each year of increasing age, there was a 5% decrease in the likelihood of undergoing a contralateral TKA (HR 0.95 [95% CI 0.92 to 0.98]; p = 0.001). The likelihood of contralateral TKA varied based upon the contralateral joint space width at different contralateral hip-knee-ankle angles. A 1 mm loss of the joint space width increased the likelihood of TKA by 42% at 4.1o of varus alignment (HR 1.42 [95% CI 1.29 to 1.56]; p = 0.005), 26% at 1.6o of varus alignment (HR 1.26 [95% CI 1.06 to 1.51]; p = 0.005), and 14% at 0.7o of valgus alignment (HR 1.14 [95% CI 0.89 to 1.46]; p = 0.005) (Fig. 3). No association was found for BMI (HR 0.98 for each unit increase [95% CI 0.92 to 1.03]; p = 0.37), gender (HR 1.29 for women compared with men [95% CI 0.76 to 2.2]; p = 0.34), or Kellgren-Lawrence grade (HR 1.37 [95% CI 0.99 to 1.91]; p = 0.06). The sensitivity analysis, which treated the Kellgren-Lawrence grade as a categorical variable, did not change the results of the Wald tests or dramatically modify model parameters. We observed that the increase in rate associated with an increase in the Kellgren-Lawrence grade was not constant between categories, as was assumed in the numeric model.
Table 2.
Results of the Cox proportional hazards model of contralateral TKA after the initial TKA
Fig. 3.

This image shows the hazard ratio for reduction of the joint space width of 1 mm for the time to contralateral TKA, based on the hip-knee-ankle angle.
Discussion
OA of the knee and hip are physically debilitating, and account for most of the joint arthroplasties performed worldwide. The clinical implications of knowing the course of OA across large lower-extremity joints are numerous, including the ability to counsel patients about disease progression and the potential to evaluate the efficacy of disease-modifying interventions. Previous studies have been limited because they used data from a single surgeon [15] or a single institution [20], while larger studies have examined homogenous populations using historical data [16] through joint arthroplasty registries [3, 16] or have had only 1-year follow-up intervals [22]. This study demonstrates the progression of end-stage OA in large joints using a multicenter, longitudinally maintained dataset in the United States. Specifically, the results showed that after TKA, one of three patients underwent a TKA on their other knee within 5 years, whereas one of 25 underwent any THA. After THA, approximately one of five patients underwent THA of their other hip within 5 years, and approximately one of 10 underwent any TKA.
This study has some limitations. The indications for total joint arthroplasty vary widely across regions, institutions, and among individual surgeons. The results of this study should be considered in light of the institutions at which the arthroplasties were performed. We evaluated the likelihood of subsequent total joint arthroplasty after arthroplasty for OA but not for other surgical indications (for example, rheumatoid arthritis) because of the composition of the OAI cohort. Additionally, the rate of subsequent TKA after the index THA may be higher in our cohort than in the general population because the group consisted primarily of individuals with knee OA or with a high risk of having knee OA. This study included relatively few patients compared with previous studies. Finally, there were relatively few incident events after THA, which limited our ability to construct a model assessing risk factors after the initial THA. Despite these limitations, we demonstrated the likelihood of subsequent joint arthroplasties with longitudinally maintained data and are the first to show that the likelihood of contralateral TKA is associated with the contralateral joint space width and hip-knee-ankle angle at the time of the initial TKA.
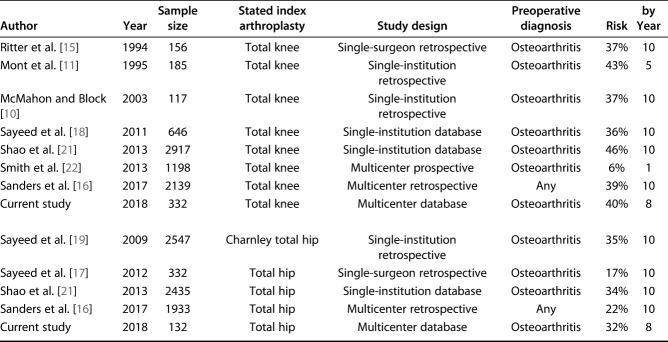
After the initial TKA, we found a 33% likelihood of contralateral TKA by 5 years and a 40% likelihood by 8 years postoperatively, which is consistent with the range of 36% to 46% by 10 years noted in other reports [10, 11, 15, 16, 18, 21, 22] (Table 3). Additionally, we found a higher rate of contralateral TKA than any THA, which is also consistent with previous findings [3, 16]. Sanders et al. [16] performed a historical cohort study of patients who underwent TKA or THA between 1969 and 2008 to assess the rates of subsequent TKA or THA. Similar to our study, the authors reported that at 20 years after the initial TKA, the likelihood of a contralateral TKA was 45%. However, the likelihood of a contralateral or ipsilateral THA was 3% and 2%, respectively, which is lower than the rate in our cohort. This discrepancy may reflect changes in arthroplasty rates over time, variations across institutions, or it may exist because of missing medical record data.
Table 3.
Summary of previous studies reporting risk of contralateral total joint arthroplasty of the cognate joint
There is variability in the likelihood of contralateral THA after an initial THA, ranging from 17% to 35% at 10 years [16, 17, 19, 21] (Table 3). Our results suggest that the likelihood is at the higher end of this range, and some studies may underestimate the likelihood because of incomplete follow-up data. After the initial THA, we found an 18% chance of contralateral THA by 5 years and 32% by 8 years. The rate of TKA after the initial THA was 8% by 5 and 8 years, exceeding the 2% to 6% rate reported by Sanders et al. [16] and may again reflect differences in arthroplasty rates over time, regional variability, or underestimation because of missing data. Additionally, these findings suggest that patients undergoing joint arthroplasty were more likely to undergo subsequent arthroplasty on the contralateral side in the same joint than on the other joint, highlighting the tendency of OA to affect pairs of joints. The mechanism underlying this association warrants further study.
We demonstrated that the rate of contralateral TKA after the initial TKA decreased with age and increased with loss of the medial compartment joint space width for varus hip-knee-ankle angles. We suspect that the decrease in likelihood associated with aging could be owing to decreased activity with age or worsening medical status, or because the benefit of TKA diminishes as patients near the end of their life and the procedure is less likely to be performed. We also showed that as the contralateral medial joint space width decreased, the likelihood of contralateral TKA increased for patients with varus knee alignment. In patients with valgus knee alignment, loss of medial joint space width was not associated with increased risk of contralateral TKA. In fact, at higher valgus angles, such as 4o or greater, a wider medial joint space width may increase the likelihood of TKA, because the increase in the medial joint space width probably represents lateral compartment narrowing and increased joint degeneration. Therefore, the effect of narrowing of the medial compartment joint space width on the likelihood of joint arthroplasty depends on the hip-knee-ankle angle. The Kellgren-Lawrence grade was not associated with subsequent TKA in this study despite an earlier report [10], suggesting that the joint space width and hip-knee-ankle angle explained much of the variability accounted for by the Kellgren-Lawrence grade. Furthermore, the joint space width and hip-knee-ankle angle may be better metrics than the Kellgren-Lawrence grade because they are objective and quantitative measurements. However, we cannot rule out the possibility that the model did not have the power to demonstrate the Kellgren-Lawrence grade as a valuable predictor.
Identifying the likelihood of subsequent joint arthroplasty for patients with OA can help clinicians to counsel patients about their disease progression. Using longitudinally maintained multicenter data from the United States, we demonstrated that patients are at a high risk of undergoing a subsequent total joint arthroplasty after the first procedure, especially on the contralateral side of the same joint. Furthermore, this study revealed that at the time of the initial knee arthroplasty, the joint space width and joint alignment of the contralateral knee was associated with the risk of contralateral TKA. Findings from this study may be used as a benchmark for similar populations in future studies evaluating the efficacy of potential disease-modifying interventions in delaying the progression of OA.
Acknowledgments
We thank Amy Nowacki PhD for her assistance with statistical analysis.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, Beard DJ. Knee replacement. Lancet . 2012;379:1331–1340. [DOI] [PubMed] [Google Scholar]
- 2.Duryea J, Li J, Peterfy CG, Gordon C, Genant HK. Trainable rule-based algorithm for the measurement of joint space width in digital radiographic images of the knee. Med Phys. 2000;27:580–591. [DOI] [PubMed] [Google Scholar]
- 3.Gillam MH, Lie SA, Salter A, Furnes O, Graves SE, Havelin LI, Ryan P. The progression of end-stage osteoarthritis: analysis of data from the Australian and Norwegian joint replacement registries using a multi-state model. Osteoarthr Cartil . 2013;21:405–412. [DOI] [PubMed] [Google Scholar]
- 4.Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, Kelly-Hayes M, Wolf PA, Kreger BE, Kannel WB. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health . 1994;84:351–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Günther KP, Stürmer T, Sauerland S, Zeissig I, Sun Y, Kessler S, Scharf HP, Brenner H, Puhl W. Prevalence of generalised osteoarthritis in patients with advanced hip and knee osteoarthritis: The Ulm Osteoarthritis Study. Ann Rheum Dis . 1998;57:717–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Illingworth KD, Bitar Y El, Siewert K, Scaife SL, El-Amin S, Saleh KJ. Correlation of WOMAC and KOOS scores to tibiofemoral cartilage loss on plain radiography and 3 Tesla MRI: data from the osteoarthritis initiative., Knee Surgery, Sport Traumatol Arthrosc. 2014;22:1649–1658. [DOI] [PubMed] [Google Scholar]
- 7.Kellgren JH, Lawrence JS. Radiological Assessment of Osteo-Arthrosis. Ann Rheum Dis. 1957;16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of Primary and Revision Hip and Knee Arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am . 2007;89:780-785. [DOI] [PubMed] [Google Scholar]
- 9.Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, Jiranek WA, Berry DJ. Prevalence of Total Hip and Knee Replacement in the United States. J Bone Joint Surg Am . 2015;97:1386–1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McMahon M, Block JA. The risk of contralateral total knee arthroplasty after knee replacement for osteoarthritis. J Rheumatol . 2003;30:1822–1824. [PubMed] [Google Scholar]
- 11.Mont MA, Mitzner DL, Jones LC, Hungerford DS. History of the contralateral knee after primary knee arthroplasty for osteoarthritis. Clin Orthop Relat Res . 1995;321:145–150. [PubMed] [Google Scholar]
- 12.Neogi T, Zhang Y. Epidemiology of Osteoarthritis. Rheum Dis Clin North Am . 2013;39:1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nevitt MC, Felson DT, Lester G. The Osteoarthritis Initiative: Protocol for the Cohort Study. 2006: 10-14. https://oai.epi-ucsf.org/datarelease/docs/StudyDesignProtocol.pdf. Accessed July 8, 2019. [Google Scholar]
- 14.Pivec R, Johnson AJ, Mears SC, Mont MA. Hip arthroplasty. Lancet . 2012;380:1768–1777. [DOI] [PubMed] [Google Scholar]
- 15.Ritter MA, Carr KD, Keating EM, Faris PM. Long-term outcomes of contralateral knees after unilateral total knee arthroplasty for osteoarthritis. J Arthroplasty . 1994;9:347–349. [DOI] [PubMed] [Google Scholar]
- 16.Sanders TL, Maradit Kremers H, Schleck CD, Larson DR, Berry DJ. Subsequent total joint arthroplasty after primary total knee or hip arthroplasty: a 40-year population-based study. J Bone Joint Surg Am. 2017;99:396–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sayeed SA, Johnson AJ, Jaffe DE, Mont MA. Incidence of contralateral THA after index THA for osteoarthritis. Clin Orthop Relat Res. 2012;470:535–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sayeed SA, Sayeed YA, Barnes SA, Pagnano MW, Trousdale RT. The risk of subsequent joint arthroplasty after primary unilateral total knee arthroplasty, a 10-year study. J Arthroplasty. 2011;26:842–846. [DOI] [PubMed] [Google Scholar]
- 19.Sayeed SA, Trousdale RT, Barnes SA, Kaufman KR, Pagnano MW. Joint arthroplasty within 10 years after primary Charnley total hip arthroplasty. Am J Orthop. 2009;38: E141-143. [PubMed] [Google Scholar]
- 20.Shakoor N, Block JA, Shott S, Case JP. Nonrandom evolution of end-stage osteoarthritis of the lower limbs. Arthritis Rheum . 2002;46:3185–3189. [DOI] [PubMed] [Google Scholar]
- 21.Shao Y, Zhang C, Charron KD, MacDonald SJ, McCalden RW, Bourne RB. The fate of the remaining knee(s) or hip(s) in osteoarthritic patients undergoing a primary TKA or THA. J Arthroplasty . 2013;28:1842–1845. [DOI] [PubMed] [Google Scholar]
- 22.Smith HK, Wylde V, Lingard EA, Blom A, Metcalfe C, Ben-Shlomo Y. The effect of pain after total knee arthroplasty on the contralateral, nonreplaced knee. J Bone Joint Surg Am . 2013;95:315–322. [DOI] [PubMed] [Google Scholar]
- 23.Steiner C, Andrews R, Barrett M, Weiss A. HCUP Projections: Mobility/Orthopedic Procedures 2003 to 2012. U.S. Agency for Healthcare Research and Quality; 2012. Report # 2012-03. https://www.hcup-us.ahrq.gov/reports/projections/2012-03.pdf. Accessed July 15, 2019. [Google Scholar]