Abstract
Background
The goals of lower limb reconstruction are to restore alignment, to improve function, and to reduce pain. However, it remains unclear whether alignment of the lower limb and hindfoot are associated because an accurate assessment of hindfoot deformities has been limited by superposition on plain radiography. Consequently, surgeons often overlook hindfoot deformity when planning orthopaedic procedures of the lower limb. Therefore, we used weight-bearing CT to quantify hindfoot deformity related to lower limb alignment in the coronal plane.
Questions/purposes
(1) Is lower-limb alignment different in varus than in valgus hindfoot deformities for patients with and without tibiotalar joint osteoarthritis? (2) Does a hindfoot deformity correlate with lower-limb alignment in patients with and without tibiotalar joint osteoarthritis? (3) Is joint line orientation different in varus than in valgus hindfoot deformities for patients with tibiotalar joint osteoarthritis? (4) Does a hindfoot deformity correlate with joint line orientation in patients with tibiotalar joint osteoarthritis?
Methods
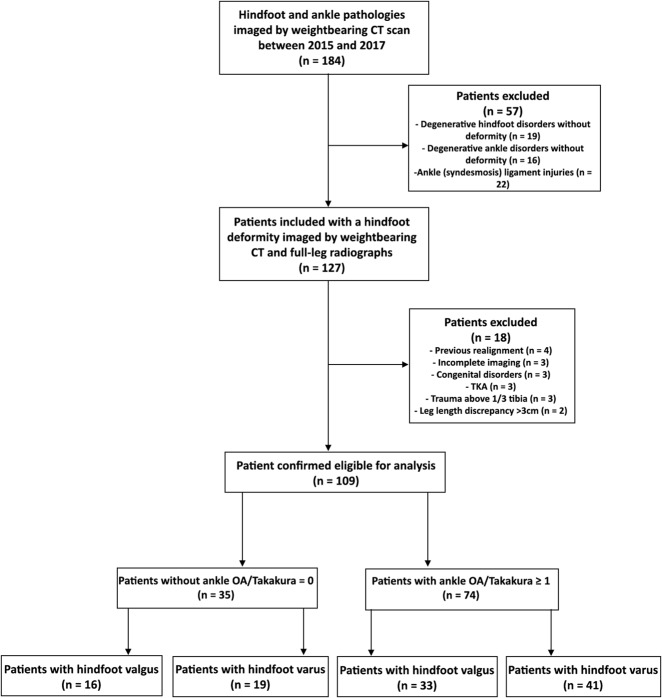
Between January 2015 and December 2017, one foot and ankle surgeon obtained weightbearing CT scans as second-line imaging for 184 patients with ankle and hindfoot disorders. In 69% (127 of 184 patients) of this cohort, a combined weightbearing CT and full-leg radiograph was performed when symptomatic hindfoot deformities were present. Of those, 85% (109 of 127 patients) with a median (range) age of 53 years (23 to 75) were confirmed eligible based on the inclusion and exclusion criteria of this retrospective comparative study. The Takakura classification was used to divide the cohort into patients with (n = 74) and without (n = 35) osteoarthritis of the tibiotalar joint. Lower-limb measurements, obtained from the full-leg radiographs, consisted of the mechanical tibiofemoral angle, mechanical tibia angle, and proximal tibial joint line angle. Weightbearing CT images were used to determine the hindfoot’s alignment (mechanical hindfoot angle), the tibiotalar joint alignment (distal tibial joint line angle and talar tilt angle) and the subtalar joint alignment (subtalar vertical angle). These values were statistically assessed with an ANOVA and a pairwise comparison was subsequently performed with Tukey’s adjustment. A linear regression analysis was performed using the Pearson correlation coefficient (r). A reliability analysis was performed using the intraclass correlation coefficient.
Results
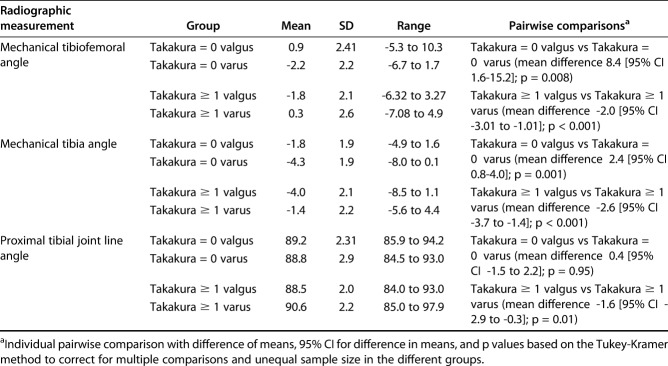
Lower limb alignment differed among patients with hindfoot deformity and among patients with or without tibiotalar joint osteoarthritis. In patients with tibiotalar joint osteoarthritis, we found knee valgus in presence of hindfoot varus deformity and knee varus in presence of hindfoot valgus deformity (mechanical tibiofemoral angle 0.3 ± 2.6° versus -1.8 ± 2.1°; p < 0.001; mechanical tibia angle -1.4 ± 2.2° versus -4.3 ± 1.9°; p < 0.001). Patients without tibiotalar joint osteoarthritis demonstrated knee varus in the presence of hindfoot varus deformity compared with knee valgus in presence of hindfoot valgus deformity (mechanical tibiofemoral angle -2.2 ± 2.2° versus 0.9 ± 2.4°; p < 0.001; mechanical tibia angle -1.8 ± 2.1° versus -4.3 ± 1.9°; p < 0.001). Patients with more valgus deformity in the hindfoot tended to have more tibiofemoral varus (r = -0.38) and tibial varus (r = -0.53), when tibiotalar joint osteoarthritis was present (p < 0.001). Conversely, patients with more valgus deformity in the hindfoot tended to have more tibiofemoral valgus (r = 0.4) and tibial valgus (r = 0.46), when tibiotalar joint osteoarthritis was absent (p < 0.001). The proximal joint line of the tibia had greater varus orientation in patients with a hindfoot valgus deformity compared with greater valgus orientation in patients with a hindfoot varus deformity (proximal tibial joint line angle 88.5 ± 2.0° versus 90.6 ± 2.2°; p < 0.05). Patients with more valgus deformity in the hindfoot tended to have more varus angulation of the proximal tibial joint line angle (r = 0.31; p < 0.05).
Conclusions
In patients with osteoarthritis of the tibiotalar joint, varus angulation of the knee was associated with hindfoot valgus deformity and valgus angulation of the knee was associated with hindfoot varus deformity. Patients without tibiotalar joint osteoarthritis exhibited the same deviation at the level of the knee and hindfoot. These distinct radiographic findings were most pronounced in the alignment of the tibia relative to the hindfoot deformity. This suggests a detailed examination of hindfoot alignment before knee deformity correction at the level of the proximal tibia, to avoid postoperative increase of pre-existing hindfoot deformity. Other differences detected between the radiographic parameters were less pronounced and varied within the subgroups. Future research could identify prospectively which of these parameters contain clinical relevance by progressing osteoarthritis or deformity and how they can be altered by corrective treatment.
Level of Evidence
Level III, prognostic study.
Introduction
The contribution of constitutional and acquired femoral and tibial deformities, especially of the hip and the knee, has been studied in detail [4, 35, 39, 41]. The mechanical tibiofemoral angle is commonly used to express this relationship and is considered a reference for evaluating overall lower-limb alignment in the coronal plane [12, 50]. The importance is reflected in the numerous joint-preserving and joint-replacing orthopaedic procedures that rely on this measurement [1, 22, 31, 35]. Despite its relevance, one crucial drawback of the mechanical tibiofemoral angle is its failure to account for hindfoot alignment because the caudal reference point of the mechanical tibial axis ends at the middle of the tibiotalar joint. Moreover, when hindfoot alignment is considered in clinical studies, a major change in the lower limb axis often occurs [16, 34, 52]. Computer-based studies have confirmed the influence of the hindfoot’s position on lower-limb alignment in the coronal plane [15].
Lower limb osteoarthritis may affect axial alignment and joint line orientation, either directly or indirectly [4, 35, 39, 41]. In a cohort of patients with osteoarthritic knee deformities, Norton et al. [36] found valgus hindfoot orientation in a varus knee deformity and the opposite in a valgus knee deformity. This mechanism, presumably one of compensation, particularly occurs in the subtalar joint [47]. Correspondingly, in a cohort of patients with tibiotalar joint arthritis, the subtalar joint’s orientation differed by up to 50% from the overall alignment of the hindfoot [57]. However, not every hindfoot with a deformity has this compensatory mechanism, and the exact occurrence rate is debatable [14, 25]. This may be partially attributed to difficulty in hindfoot imaging, which is limited by superposition and rotational errors encountered with plain radiographs [24]. The recent advent of weightbearing conebeam CT has allowed imaging of the foot and ankle at a lower radiation dose than conventional CT imaging [3, 32]. This technology accurately analyzes articular configurations and can account for rotational errors [13, 43]. Measurement techniques to assess hindfoot alignment and joint line orientation on weightbearing conebeam CT images have been described, with a concomitant reliability analysis and reference values [6, 8, 11, 26]. However, the relationship between hindfoot deformity and lower-limb alignment in the coronal plane remains unclear.
In this study, we asked: (1) Is lower-limb alignment different in varus than in valgus hindfoot deformities for patients with and without tibiotalar joint osteoarthritis? (2) Does a hindfoot deformity correlate with lower-limb alignment in patients with and without tibiotalar joint osteoarthritis? (3) Is joint line orientation different in varus than in valgus hindfoot deformities for patients with tibiotalar joint osteoarthritis? (4) Does a hindfoot deformity correlate with joint line orientation in patients with tibiotalar joint osteoarthritis?
Patients and Methods
Study Design and Setting
Between January 2015 and December 2017, one foot and ankle surgeon (KB) requested a weightbearing CT scan of 184 patients as second-line imaging. Of those, 69% (127 of 184 patients) had a combined full-leg radiograph and weightbearing conebeam CT examination. In general, we ordered both tests in patients with persistent signs and symptoms of hindfoot varus and valgus deformities despite previous conservative or surgical treatment. Heel inversion with peroneal tendon/lateral ankle ligament tenderness was considered for hindfoot varus deformities and heel eversion with tibial posterior tendon/deltoid ligament for hindfoot valgus deformities. Of those, 85% (109 out of 127 patients) were included in this retrospective comparative study (Fig. 1).
Fig. 1.
This flowchart shows the study enrollment process.
Participants
The study population consisted of 57 male and 52 female patients with a median (range) age of 54 years (23 to 75) (Table 1). The inclusion criteria were patients between 18 and 75 years old with hindfoot deformity imaged by both a full-leg radiograph and weightbearing conebeam CT. The exclusion criteria were congenital disorders affecting lower-limb alignment such as cerebral palsy, rickets, and achondroplasia; absence of or an incomplete full-leg radiograph and weightbearing conebeam CT images; previous hindfoot surgery or knee realignment; posttraumatic deformities above the distal third of the tibia; TKA; or a leg-length discrepancy of more than 3 cm. Patients’ records and radiographs were reviewed by two orthopaedic surgeons (KB, a foot and ankle surgeon with 20 years of experience, and ABMB, an orthopaedic resident with 6 years of experience). Our institutional review board approved this study, and the need to obtain informed consent was waived.
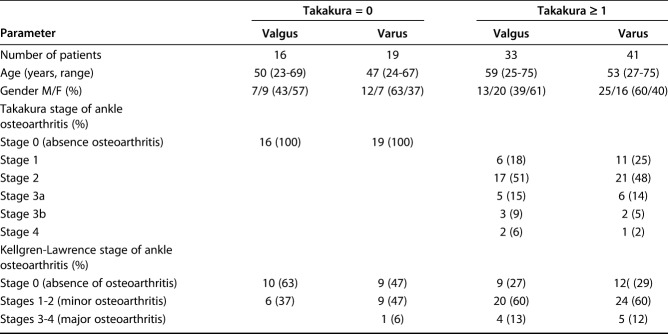
Table 1.
Baseline demographic and radiographic information
Variables, Outcome Measures, Data Sources, and Bias
Weightbearing full-leg radiographs were obtained with patients standing barefoot with both feet together and the patella facing forward as described by Paley et al. [41], using an Ysio® digital radiography system (Siemens, Erlangen, Germany) at 85 kV and a focus-to-detector distance of 3 meters. Measurements were performed using OsiriX® v1.6.2 software (Osirix, Geneva, Switzerland) [45].
Weightbearing CT images were obtained with a PedCAT® device (Curvebeam, Warrington, PA, USA) and patients were positioned according to the same protocol as for the full-leg radiographs. The following imaging protocol and settings were used for weightbearing conebeam CT: tube voltage: 96 kV; tube current: 7.5 mAs; CTDIvol: 4.3 mGy; matrix: 160 x 160 x 130; pixel size: 0.4 mm; and slice interval: 0.4 mm.
The axial radiographic alignment is noted as a deviation from 180°; positive values represent valgus alignment and negative values represent varus alignment.
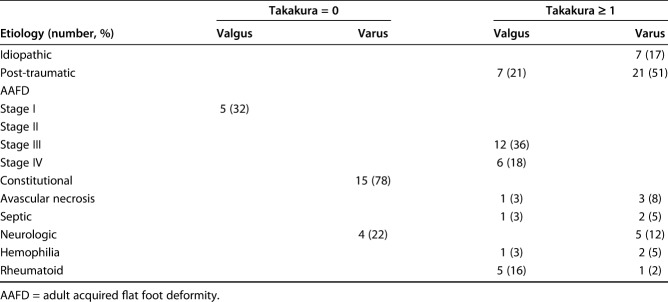
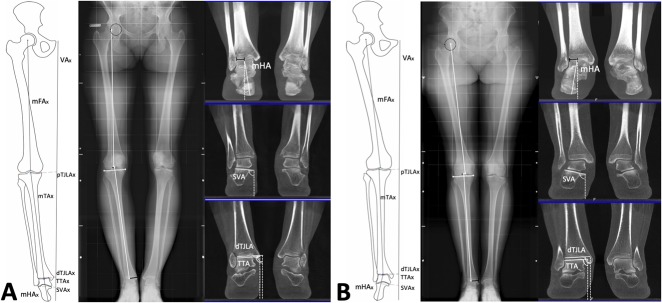
The joint line’s orientation is referenced toward the vertical axis perpendicular to the floor and noted as at least 90° (valgus alignment) or less than 90° (varus alignment) (Fig. 2A).
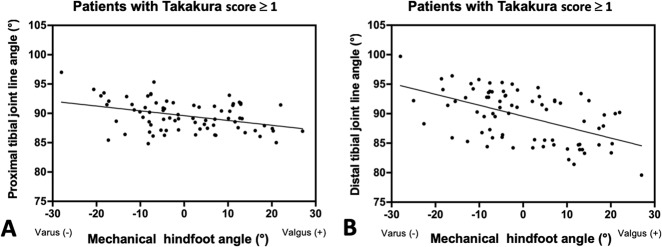
Fig. 2A-D.
Measurements were made on full-leg radiographs and weightbearing CT images. (A) The mechanical tibiofemoral angle (mTFA) was demonstrated on the right limb and obtained by the intersection of the mechanical femoral axis (mFAx) and mechanical tibia axis (mTAx). The mechanical tibia angle (mTA) and proximal tibial joint line angle (pTJLA) are depicted on the left limb and were determined by the intersection of their concomitant axes and the vertical axis (VAx) connecting the center of the pubic symphysis perpendicular to the floor. (B) The mechanical hindfoot angle (mHA) was determined by the intersection between the vertical axis and the mechanical hindfoot axis (mHAx) connecting the midpoint of the superior talar facet with the inferior point of the calcaneus. (C) The subtalar vertical angle (SVA) was determined as the intersection between the vertical axis and the subtalar vertical axis (SVAx), parallel to the posterior facet of the subtalar joint. (D) The distal tibial joint line angle (dTJLA) was defined as the intersection between the vertical axis and the axis parallel to the distal joint surface of the tibia, and the talar tilt angle (TTA) was defined as the intersection between the vertical axis and the talar tilt axis (TTAx) parallel to the superior facet of the talus.
Three angles were determined on each full-leg radiograph in the coronal plane by two authors (ABMB, EV): the mechanical tibiofemoral angle, mechanical tibia angle, and the proximal tibial joint line angle. The mechanical tibiofemoral angle was used to assess the lower limb’s alignment and was defined by the intersection of the mechanical femur axis and mechanical tibia axis [12]. The mechanical femur axis was obtained by connecting the center of the femoral head, determined by a concentric digital template, with the apex of the femoral notch (Fig. 2A) [12, 33]. The mechanical tibia axis was obtained by connecting the midpoint between the tip of the medial and lateral intercondylar tubercles with the midpoint between the tibia and fibula at the plafond [23]. The mechanical tibia angle was determined by the intersection of the mechanical tibia axis and the vertical axis. The mechanical tibia angle was assessed separately from the mechanical tibiofemoral angle because hindfoot alignment is often referenced toward the tibia [12, 33]. The proximal tibia joint line axis was determined by the line tangential to the medial and lateral tibial plateau and was intersected with the vertical axis to obtain the concomitant proximal tibia joint line angle (Fig. 2A) [56].
Two authors (ABMB, PD) determined the following radiographic parameters on weightbearing conebeam CT images in the coronal plane: the hindfoot alignment containing the mechanical hindfoot axis; the tibiotalar joint alignment, consisting of the distal tibial joint line axis and talar tilt axis; and the subtalar joint alignment, defined by the subtalar vertical axis [6, 8, 19, 43]. All axes were measured toward the vertical axis to obtain the concomitant angle. We used the multiplanar reconstruction mode to allow simultaneous assessment of orthogonal CT-slices in the coronal, axial, and sagittal planes. This post-imaging process accounted for rotational errors in patient positioning, by aligning each foot along the longitudinal axis of the second metatarsal in the axial plane, commonly used as a reference position [2, 11, 26].
On combined CT slices, digitally reconstructed AP ankle radiographs were generated by the weightbearing conebeam CT software [8, 29]. We used the corresponding reconstructed radiograph in the coronal plane to define the mechanical hindfoot axis by connecting the most inferior point of the calcaneus with the midpoint of the superior facet of the talus (reported normal value: 0.61 ± 2.9° of valgus) (Fig. 2B) [6, 8].
On single CT slices, we determined the most superior point of the talar dome in the sagittal plane using the multiplanar reconstruction mode. The corresponding CT image in the coronal plane was used to define the distal tibial joint line axis, as the axis parallel to the distal joint surface of the tibia, and the talar tilt axis, as the axis parallel to the superior facet of the talus (reported normal value of the distal tibial joint line angle: 88.1 ± 3.1° of varus; talar tilt angle: 87.6 ± 3.9° of varus) (Fig. 2C) [6].
Further on single CT slices, we determined the midpoint of the posterior subtalar joint’s facet in the sagittal plane using the multiplanar reconstruction mode. We used the corresponding CT image in the coronal plane to define the subtalar vertical axis as the axis parallel to the posterior subtalar joint’s facet (reported normal value of the subtalar vertical angle: 98° of valgus (range 85 to 114) (Fig. 2D) [11].
Accounting for All Patients
We used the Takakura classification system to determine the degree of tibiotalar joint osteoarthritis on digitally reconstructed AP ankle radiographs [17]. The cohort was divided into patients without radiographic signs of tibiotalar joint osteoarthritis (Takakura stage 0; n = 35) and patients with radiographic signs of tibiotalar joint osteoarthritis (Takakura stage 1 or above; n = 74) containing different etiologies (Table 2). The median (range) age of patients without tibiotalar joint osteoarthritis was 48 years (23 to 64) and the mean (range) age of patients with tibiotalar joint osteoarthritis was 57 years (27 to 75). Patients in the hindfoot valgus group were subdivided according to whether the mechanical hindfoot angle was positive, and patients in the hindfoot varus group were subdivided according to whether the mechanical hindfoot angle was negative (Fig. 1). These groups were used to perform the proposed comparisons and correlation analysis using the aforementioned radiographic measurements.
Table 2.
Etiology of hindfoot deformities
We assessed knee osteoarthritis using the Kellgren-Lawrence classification system [23]. To account for correlated data in the study population, we included only one lower limb from each patient in the analysis [46, 50]. The right limb was selected for patients with a bilateral hindfoot deformity with or without tibiotalar joint osteoarthritis. The concomitant limb of the affected side was selected in patients with a unilateral hindfoot deformity with or without tibiotalar joint osteoarthritis.
Statistical Analysis, Study Size
A Kolmogorov-Smirnov normality test was conducted for each radiographic outcome and demonstrated a p value greater than 0.05, indicating normal distribution of the data and the need for further parametric testing. Comparison of the angular outcomes among the four groups was performed using a one-way ANOVA. When the global F-test result of the ANOVA was statistically significant, a further analysis was undertaken by performing pairwise comparisons. This was conducted using the Tukey-Kramer post-hoc test to control for the overall Type I error rate and the unequal sample size among the different groups. The correlation between the full-leg radiographic and weightbearing CT hindfoot measurements was assessed with the Pearson coefficient (r). A linear regression analysis was performed using a corresponding scatter plot. The interobserver and intraobserver observer variability were determined using the interclass correlation coefficient (ICC) at 1-month intervals in 23 patients (20% of the study population) who were randomly selected by the statistical software in accordance with the method of a previous study [26]. Interpretations were as follows: ICC < 0.4: poor; ICC 0.4 to 0.59: acceptable; ICC 0.6 to 0.74: good; and ICC > 0.74, excellent [51]. The SPSS statistical package (version 25.0.0. standard version, SPSS Inc, Chicago, IL, USA) was used to analyze the results. A p value < 0.05 was considered significant. A statistical power analysis using the SAS® Power and Sample Size application (SAS Inc, Cary, NC, USA) was performed to estimate the sample size, based on previously reported data regarding the primary parameter associated with alignment of the lower limb: mechanical tibiofemoral angle [44]. A minimal sample size of 12 patients needed to be enrolled in each subgroup to reach the calculated effect size (f = 1.8), with a power level of 0.8 and level of significance of 0.05.
Results
Is Lower-limb Alignment Different in Varus Than in Valgus Hindfoot Deformities for Patients With and Without Tibiotalar Joint Osteoarthritis?
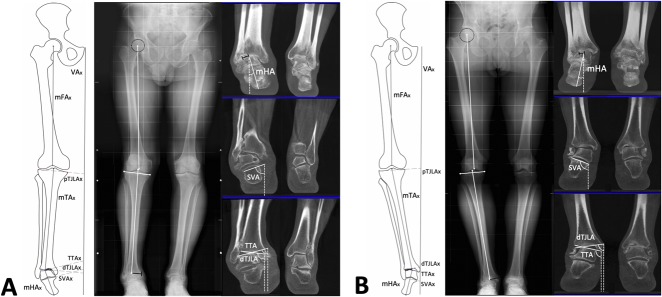
Lower limb alignment differed among patients with hindfoot deformity and among patients with or without tibiotalar joint osteoarthritis. In patients with tibiotalar joint osteoarthritis we found knee valgus (Fig. 3A) in presence of hindfoot varus deformity and knee varus (Fig. 3B) in presence of hindfoot valgus deformity (mechanical tibiofemoral angle 0.3 ± 2.6° versus -1.8 ± 2.1°; mechanical tibia angle -1.4 ± 2.2° versus -4.3 ± 1.9°) (Table 3; p < 0.001). Patients without tibiotalar joint osteoarthritis demonstrated knee varus (Fig. 4A) in the presence of hindfoot varus deformity compared with knee valgus (Fig. 4B) in the presence of hindfoot valgus deformity (mechanical tibiofemoral angle -2.2° ± 2.2° versus 0.9 ± 2.4°; mechanical tibia angle -4.3 ± 1.9° versus -1.8 ± 2.1°) (Table 3; p < 0.001).
Fig. 3A-B.
Full-leg radiographs and weightbearing CT measurements were taken in patients with tibiotalar joint osteoarthritis. (A) Axial alignment of the right hindfoot was measured with the mechanical hindfoot angle (mHA) and demonstrated that a varus deformity was present. The associated joint lines of the hindfoot, measured with the talar tilt angle (TTA) at the superior facet of the talus and the subtalar vertical angle (SVA) at the posterior facet of the subtalar joint, are orientated in varus. The mechanical tibia angle (mTA), proximal tibial joint line angle (pTJLA), and distal tibial joint line angle were orientated in valgus, and were associated with opposing angulation toward axial alignment and orientation of the joint line in patients with a hindfoot deformity. (B) The opposite pattern is demonstrated in a patient with a valgus deformity of the right hindfoot; the axial alignment (mechanical hindfoot angle) and orientation of the joint lines (talar tilt angle and subtalar vertical angle) demonstrated that valgus alignment was present. The axial alignment of the tibia (mechanical tibia angle) and orientation of the proximal and distal joint line of the tibia (proximal and distal tibial joint line angle) demonstrated presence of a varus alignment and were associated with opposing angulation towards the hindfoot deformity.
Table 3.
ANOVA of radiographic lower limb alignment measurements of a valgus and varus hindfoot in patients with and without tibiotalar joint osteoarthritis
Fig. 4A-B.
Full-leg radiographs and weightbearing CT measurements were taken in patients without tibiotalar joint osteoarthritis. (A) Varus alignment of the hindfoot is demonstrated by the mechanical hindfoot angle (mHA) and was associated with varus alignment of the lower limb by the mechanical tibiofemoral angle (mTFA) (B) Conversely, valgus alignment of the hindfoot was associated with valgus alignment of the lower limb.
Does a Hindfoot Deformity Correlate With Lower-limb Alignment in Patients With and Without Tibiotalar Joint Osteoarthritis?
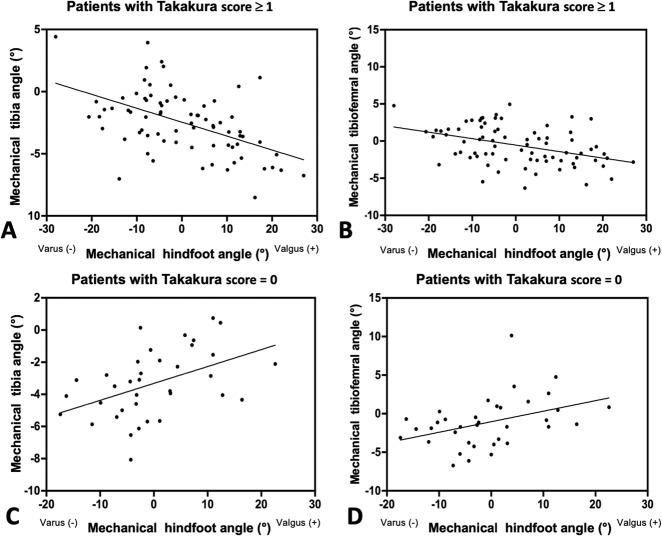
Patients with more valgus deformity in the hindfoot tended to have more tibial varus (r = -0.53; p < 0.001; Fig. 5A) and tibiofemoral varus (r = -0.38; p < 0.001; Fig. 5B), when tibiotalar joint osteoarthritis was present. Conversely, patients with more valgus deformity in the hindfoot tended to have more tibial valgus (r = 0.46; p < 0.001; Fig. 5C) and tibiofemoral valgus (r = 0.4; p < 0.001; Fig. 5D), when tibiotalar joint osteoarthritis was absent.
Fig. 5A-D.
A linear regression analysis was performed between the mechanical hindfoot angle and both the mechanical tibia angle and mechanical tibiofemoral angle. These images show (A) the correlation between the mechanical tibia angle and hindfoot alignment in patients with tibiotalar joint osteoarthritis (r = -0.46, y = 0.12, x - 3.2; p < 0.001), (B) the correlation between the mechanical tibiofemoral angle and hindfoot alignment in patients with tibiotalar joint osteoarthritis (r = -0.4, y = 0.14, x - 1.0; p < 0.001), (C) the correlation between the mechanical tibia angle and hindfoot alignment in patients without tibiotalar joint osteoarthritis (r = 0.53, y = -0.12, x - 2.5; ; p < 0.001), and (D) the correlation between the mechanical tibiofemoral angle and hindfoot alignment in patients without tibiotalar joint osteoarthritis (r = 0.38, y = -0.09, x - 0.6; p < 0.001).
Is the Tibial Joint Line’s Orientation Different in Varus than in Valgus Hindfoot Deformities for Patients with Tibiotalar Joint Osteoarthritis?
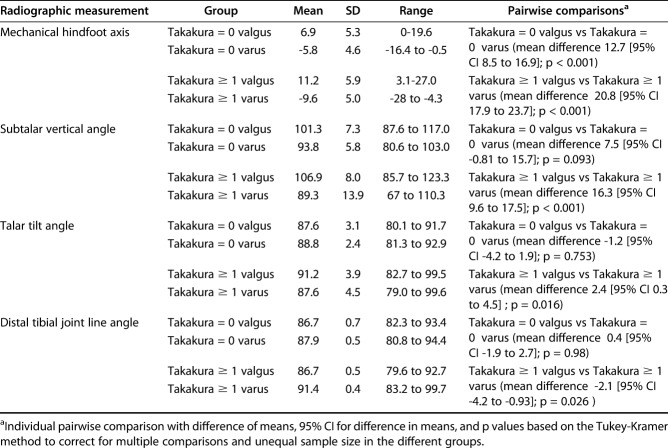
The joint line orientation at both ends of the tibia demonstrated greater varus angulation in patients with hindfoot valgus deformity and differed from greater valgus angulation at both ends of the tibia in patients with hindfoot varus deformity (proximal tibial joint line angle 88.5 ± 2.0° versus 90.6 ± 2.2° and distal tibial joint line angle 86.7 ± 0.5° versus 91.4 ± 0.4°) (p < 0.05; Table 4). The joint line orientation of hindfoot deformities demonstrated greater valgus orientation of the superior facet of the talus and posterior facet of the subtalar joint in patients with hindfoot valgus, which differed from greater varus orientation in patients with hindfoot varus (talar tilt angle 91.2° ± 3.9° versus 87.6 ± 4.5°; subtalar vertical angle 106.9 ± 8.0° versus 89.3 ± 13.9°) (p < 0.001; Table 4).
Table 4.
ANOVA of radiographic hindfoot alignment measurements of valgus and varus hindfoot deformities in patients with and without tibiotalar joint osteoarthritis
Does a Hindfoot Deformity Correlate with the Tibial Joint Line’s Orientation in Patients with Tibiotalar Joint Osteoarthritis?
Patients with more valgus deformity in the hindfoot tended to have more varus angulation of the proximal tibial joint line (r =-0.31; p < 0.05; Fig. 6A) and distal tibial joint line (r =-0.51; p < 0.001; Fig. 6B).
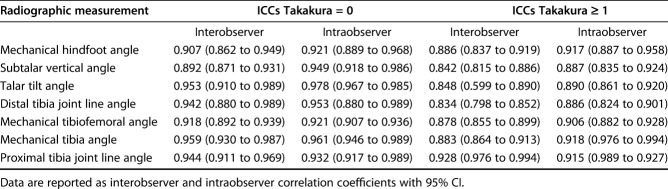
Fig. 6A-B.
A linear regression analysis was performed between the mechanical hindfoot angle and both the proximal and distal tibial joint line angle. These images show (A) the correlation between the mechanical tibia angle and hindfoot alignment in patients with tibiotalar joint osteoarthritis (r = -0.31, y = -0.08, x + 89.6; p < 0.05), (B) the correlation between the mechanical tibiofemoral angle and hindfoot alignment in patients with tibiotalar joint osteoarthritis (r = -0.51, y = -0.19, x + 89.6; p < 0.001).
Other Relevant Findings
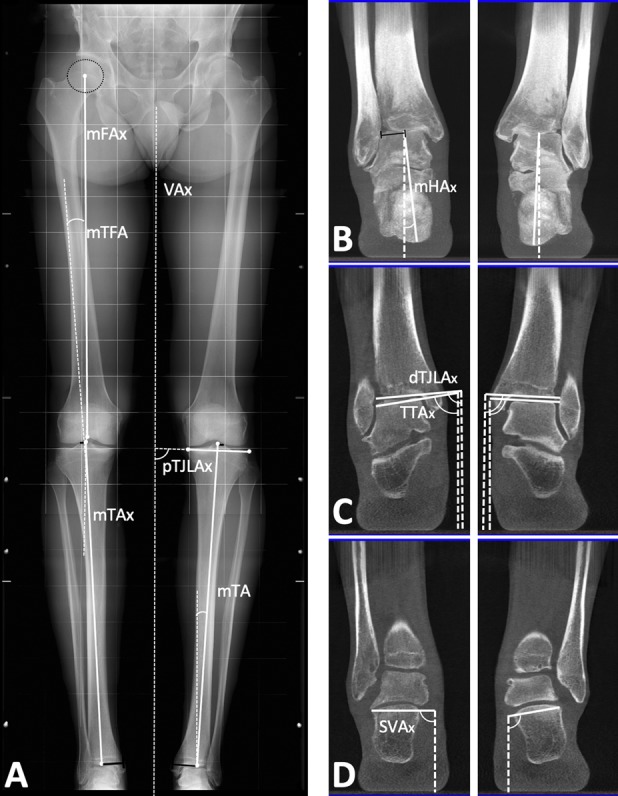
The mean Kellgren-Lawrence score was 0.57 ± 0.7 in the group of patients without tibiotalar joint osteoarthritis. This was lower than the mean Kellgren-Lawrence score of 1.26 ± 0.9 in patients with tibiotalar joint osteoarthritis (95% CI -0.99 to -0.38; p < 0.001). The intraclass correlation coefficients (ICCs) for both groups were excellent. The ICCs of the lower limb and hindfoot measurements in the group of patients without tibiotalar joint osteoarthritis (range 0.892 to 0.978) were higher than those in the group of patients with tibiotalar joint osteoarthritis (range 0.834 to 0.928) (Table 5).
Table 5.
Interobserver and intraobserver reliability for measurement of alignment of the hindfoot and lower limb
Discussion
The relation between osteoarthritic knee deformities and their hindfoot alignment has been demonstrated previously [36]. However, the opposite relationship, between hindfoot deformities and lower-limb alignment, has not been investigated. Moreover, an accurate analysis of axial alignment and orientation of the joint line using plain radiographs is limited by superposition encountered on plain radiographs. Weightbearing conebeam CT was used to overcome this restriction and enable a detailed evaluation of the hindfoot’s alignment. We found an association in patients with tibiotalar joint osteoarthritis between varus alignment of the knee in those with a hindfoot valgus deformity and with valgus alignment of the knee in those with a hindfoot varus deformity. Lower limb alignment in patients without tibiotalar joint osteoarthritis was associated with similar deviations at the level of the knee and hindfoot.
Several limitations were encountered during the study. First, we used a control group of patients who did not have tibiotalar joint osteoarthritis, but we did not control for hindfoot deformities. However, using a control group sampled from the general population, with absence of tibiotalar joint osteoarthritis and a hindfoot deformity would require both full-leg radiographic and weightbearing CT imaging, resulting in a level of radiation exposure that would be difficult to justify. To resolve this issue, we used reference values from previous studies for comparison [8, 9, 26, 56]. Second, the results were limited to one measurement of each radiographic parameter in the coronal plane, omitting sagittal deformities and axial rotations. In addition, radiographic analysis was limited to 2-D measurements of anatomical structures or deformities, which are 3-D in nature [20, 21, 47]. To overcome this shortcoming, other imaging modalities that generate 3-D models can be used, either ranging from the ankle to the pelvis or from the foot to the distal femur [42, 53]. However, debate remains on the exact methodology of translating established radiographic 2-D measurements to computed 3-D angles [5, 7, 30]. Third, the study design is retrospective, and important clinical data such as the ligament conditions (stiffness or laxity), ROM (assessed in the knee, ankle, as well as hindfoot- and midfoot joints) and the exact occurrence of a hindfoot deformity in relation to knee malalignment were not typically reported or available. However, the aim of this study was to evaluate the radiographic association at presentation to a clinical practice. Nevertheless, prospective research should assess if patients with ligament laxity or stiffness impose different types of deformities or other compensatory mechanisms [27]. Fourth, the classification of hindfoot varus and valgus alignment was based on a narrow range, potentially resulting in a misclassification of the hindfoot deformity. However, rater reliability was high, and all patients were considered during the correlation analysis, regardless of whether they had a varus or valgus deformity. Similarly, the division in tibiotalar joint osteoarthritis was based on one stage difference and no further subgroup analysis could performed based on the sample size calculation. This can be addressed in future research by increasing patient cohort size to allow stratification according to the degree of ankle or knee osteoarthritis.
Is Lower-limb Alignment Different in Varus Than in Valgus Hindfoot Deformities for Patients With and Without Tibiotalar Joint Osteoarthritis?
We found that axial lower limb alignment differed between varus and valgus hindfoot deformities, and that the direction of the deformity differed depending on whether tibiotalar osteoarthritis was present. Thus, clinicians cannot assume from short knee radiographs that the hindfoot will be aligned in the same direction as the knee. In the setting of planned knee deformity correction at the level of the tibia by either knee arthroplasty or osteotomy, pre-existing osteoarthritic hindfoot deformities are important to detect as they are known to adversely affect clinical and radiographic outcome [10, 49]. In a previous study comparing hindfoot alignment in patients with osteoarthritic knee deformities, a varus knee deformity was associated with a hindfoot valgus angle and a valgus knee deformity was associated with a hindfoot varus angle [36]. However, that study’s cohort consisted of patients with end-stage knee arthritis, in contrast to the current study population, who had a mean Kellgren-Lawrence knee osteoarthritis score of 1.6. In addition, almost half of their cohort presented with a knee deformity of greater than 10°, which differed from the current study’s population, which consisted of only one patient with a knee deformity greater than 10°. In the current study, the radiographic differences were often small with a considerable variation within the subgroups. The difference in the mechanical tibiofemoral angle between hindfoot varus and valgus deformities in patients with osteoarthritis was 2.1°, which is of questionable clinical relevance. However, mechanical tibia angles in these patient groups differed by 3.4°, which is clinically relevant [28]. This discrepancy could be a consequence of differences in femoral alignment, which ranges from 4° to 12° of valgus and is unrelated to tibial alignment [19]. Other reasons for this variation can be attributed to the inhomogeneous distribution of patients with tibiotalar joint osteoarthritis according to the Takakura classification and differences in etiology of hindfoot deformities, as post-traumatic deformities present a distinct pathoanatomy compared with neurological or systemic etiologies [55]. This may alter findings in other patients groups and can be controlled in future studies by stratifying the hindfoot deformities according to sample size and etiology.
Does a Hindfoot Deformity Correlate With Axial Lower-limb Alignment in for Patients With and Without Tibiotalar Joint Osteoarthritis?
We detected different relationships between axial lower-limb alignment and hindfoot deformity, depending on the presence or absence of tibiotalar osteoarthritis. The hindfoot alignment in patients with tibiotalar joint osteoarthritis demonstrated more varus, while the lower limb alignment contained more valgus. This contradicts the previous assumption that hindfoot valgus is associated with valgus alignment of the lower limb and vice versa [38]. However, similar to the result of a previous study, we demonstrated a linear increase of the hindfoot angle in relation to increasing axial lower limb angles in patients without tibiotalar joint osteoarthritis [44]. This distinct relationship between patients with and without arthritis is currently not well understood, but it could be attributed to changes in bone morphology and soft-tissue laxity occurring in patients with osteoarthritis [18, 37, 54]. These changes may alter axial alignment and joint line orientation [54].
Is the Tibial Joint Line’s Orientation Different in Varus than in Valgus Hindfoot Deformities for Patients with Tibiotalar Joint Osteoarthritis?
We found that the orientation of the tibial joint line in the knee and ankle differed between varus and valgus hindfoot deformities with tibiotalar joint osteoarthritis. Tibial alignment was associated with opposing angulation of the mechanical axis and joint line orientation towards a hindfoot varus or valgus deformity. This has not been found on full-leg radiographs, but it could be detected on Mortise ankle images in patients who underwent realignment procedures for hindfoot varus and valgus deformities [40]. Opposing alignment between the hindfoot deformity and lower-limb alignment may have biomechanical benefits by reducing the amount of knee deviation towards the ground mechanical axis (connecting the center of the hip to the ground by including the inferior part of the calcaneus) [54].
The subtalar joint’s orientation was not associated with an opposing angulation relative to the hindfoot deformity. This suggests that not every hindfoot deformity is compensated for by the subtalar joint, which is in accordance with the findings of a previous study [17]. Future prospective research could help to identify at different time points the key mechanisms of the subtalar joint that determine which patients are able to compensate for hindfoot deformity. Currently, 3-D measurements are available and can be implemented to analyze joint line orientation in greater detail and provide additional assessment of the articular hindfoot configuration and shape, which has demonstrated to be associated with tibiotalar joint osteoarthritis [26, 48, 58].
Does a Hindfoot Deformity Correlate with the Tibial Joint Line’s Orientation in Patients with Tibiotalar Joint Osteoarthritis?
Our data showed a linear increase of the hindfoot angle in correspondence to a decreasing angulation of the tibial joint lines: the hindfoot alignment demonstrated more varus, while the tibial joint lines contained more valgus. The importance of joint line orientation of the tibia towards the hindfoot has been demonstrated after both knee arthroplasty and osteotomy [28, 36]. However, the relation between both was not investigated in detail but is important to assess, particularly in rigid hindfoot deformities that may be aggravated after deformity correction at the knee level [49]. Further studies could assess how joint line orientation differs within hindfoot deformities and how they interfere with corrective treatment either at the level of the knee or hindfoot.
In this cohort, the lower-limb alignment of patients with tibiotalar joint osteoarthritis was associated with varus alignment of the knee in those with a hindfoot valgus deformity and with valgus alignment of the knee in those with a hindfoot varus deformity. Conversely, patients without tibiotalar joint osteoarthritis had similar directions of coronal-plane deviations in the knee and hindfoot. These distinct radiographic findings were most pronounced in the alignment of the tibia relative to the hindfoot deformity. This suggests a detailed examination of hindfoot alignment before knee deformity correction at the level of the tibia may be valuable, to avoid postoperative increase of pre-existing hindfoot deformity. Other differences detected between the investigated radiographic parameters in this study were less pronounced and varied within the subgroups. Future research could assess patient cohorts prospectively to improve diagnosis by identifying which of the investigated radiographic parameters contain clinical relevance in progressive osteoarthritis or deformity. Treatment strategies could be improved by assessing how and at which level conservative or surgical corrective interventions alter these deformities.
Acknowledgments
We thank Maxwell Weinberg BSc, research coordinator in the Department of Orthopaedics at the University of Utah, for his editorial support. We also thank Stephanie De Buyser PhD, a statistician in the Department of Statistics at the University of Ghent, for the statistical analysis.
Footnotes
The institution of one or more of the authors (ABMB, AB, PD, EV, CLS, JV) has received, during the study period, funding from the LS-Peery Discovery Program in Musculoskeletal Research and the Research Foundation Flanders (V424118).
One of the authors certifies that he (ABMB), or a member of his immediate family, has received during the study period, an amount of less than USD 10,000 from Curvebeam LLC (Warrington, PA, USA). One of the authors certifies that he (AB), or a member of his immediate family, has received during the study period, an amount of USD 10,001 to USD 100,000 from Medartis AG (Basel, Switzerland).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
This work was performed at the University of Utah, Salt Lake City, UT, USA.
References
- 1.Abu-Rajab RB, Deakin AH, Kandasami M, McGlynn J, Picard F, Kinninmonth AW. Hip–knee–ankle radiographs are more appropriate for assessment of post-operative mechanical alignment of total knee arthroplasties than standard AP knee radiographs. J Arthroplasty. 2015;30:695-700. [DOI] [PubMed] [Google Scholar]
- 2.Barg A, Amendola RL, Henninger HB, Kapron AL, Saltzman CL, Anderson AE. Influence of ankle position and radiographic projection angle on measurement of supramalleolar alignment on the anteroposterior and hindfoot alignment views. Foot Ankle Int. 2015;36:1352-1361. [DOI] [PubMed] [Google Scholar]
- 3.Barg A, Bailey T, Richter M, de Cesar Netto C, Lintz F, Burssens A, Phisitkul P, Hanrahan CJ, Saltzman CL. Weightbearing computed tomography of the foot and ankle: emerging technology topical review. Foot Ankle Int. 2018;39:376-386. [DOI] [PubMed] [Google Scholar]
- 4.Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat Award: Is neutral mechanical alignment normal for all patients?: The concept of constitutional varus. Clin Orthop Relat Res. 2012;470:45-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bernasconi A, Cooper L, Lyle S, Patel S, Cullen N, Singh D, Welck M. Intraobserver and interobserver reliability of cone beam weightbearing semi-automatic three-dimensional measurements in symptomatic pes cavovarus. Foot Ankle Surg. [Published online ahead of print July 26, 2019]. DOI: 10.1016/j.fas.2019.07.005. [DOI] [PubMed]
- 6.Burssens A, Peeters J, Buedts K, Victor J, Vandeputte G. Measuring hindfoot alignment in weight bearing CT: A novel clinical relevant measurement method. Foot Ankle Surg. 2016;22:233-238. [DOI] [PubMed] [Google Scholar]
- 7.Burssens A, Peeters J, Peiffer M, Marien R, Lenaerts T, Vandeputte G, Victor J, ISG W. Reliability and correlation analysis of computed methods to convert conventional 2D radiological hindfoot measurements to a 3D setting using weightbearing CT. Int J Comput Assist Radiol Surg. 2018;13:1999-2008. [DOI] [PubMed] [Google Scholar]
- 8.Burssens A, Van Herzele E, Leenders T, Clockaerts S, Buedts K, Vandeputte G, Victor J. Weightbearing CT in normal hindfoot alignment—Presence of a constitutional valgus? Foot Ankle Surgery. 2018;24:213-218. [DOI] [PubMed] [Google Scholar]
- 9.Cherian JJ, Kapadia BH, Banerjee S, Jauregui JJ, Issa K, Mont MA. Mechanical, anatomical, and kinematic axis in TKA: concepts and practical applications. Curr Rev Musculoskelet Med. 2014;7:89-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choi GW, Yang JH, Park JH, Yun HH, Lee YI, Chae JE, Yoon JR. Changes in coronal alignment of the ankle joint after high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2017;25:838-845. [DOI] [PubMed] [Google Scholar]
- 11.Colin F, Horn Lang T, Zwicky L, Hintermann B, Knupp M. Subtalar joint configuration on weightbearing CT scan. Foot Ankle Int. 2014:35:1057-1062. [DOI] [PubMed] [Google Scholar]
- 12.Cooke TDV, Sled EA, Scudamore RA. Frontal plane knee alignment: a call for standardized measurement. J Rheumatol. 2007;34:1796. [PubMed] [Google Scholar]
- 13.de Cesar Netto C, Schon LC, Thawait GK, da Fonseca LF, Chinanuvathana A, Zbijewski WB, Siewerdsen JH, Demehri S. Flexible adult acquired flatfoot deformity: comparison between weight-bearing and non-weight-bearing measurements using cone-beam computed tomography. J Bone Joint Surg Am. 2017;99:e98. [DOI] [PubMed] [Google Scholar]
- 14.Desai SS, Shetty GM, Song H-R, Lee SH, Kim TY, Hur CY. Effect of foot deformity on conventional mechanical axis deviation and ground mechanical axis deviation during single leg stance and two leg stance in genu varum. Knee. 2007;14:452-457. [DOI] [PubMed] [Google Scholar]
- 15.Duggal N, Paci GM, Narain A, Bournissaint LG, Nazarian A. A computer assessment of the effect of hindfoot alignment on mechanical axis deviation. Comput Methods Programs Biomed. 2014;113:126-132. [DOI] [PubMed] [Google Scholar]
- 16.Guichet J-M, Javed A, Russell J, Saleh M. Effect of the foot on the mechanical alignment of the lower limbs. Clin Orthop Relat Res. 2003;415:193-201. [DOI] [PubMed] [Google Scholar]
- 17.Hayashi K, Tanaka Y, Kumai T, Sugimoto K, Takakura Y. Correlation of compensatory alignment of the subtalar joint to the progression of primary osteoarthritis of the ankle. Foot Ankle Int. 2008;29:400-406. [DOI] [PubMed] [Google Scholar]
- 18.Hintermann B, Knupp M, Barg A. Peritalar instability. Foot Ankle Int. 2012;33:450-454. [DOI] [PubMed] [Google Scholar]
- 19.Howell SM, Kuznik K, Hull ML, Siston RA. Longitudinal shapes of the tibia and femur are unrelated and variable. Clin Orthop Relat Res. 2010;468:1142-1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kido M, Ikoma K, Imai K, Maki M, Takatori R, Tokunaga D, Inoue N, Kubo T. Load response of the tarsal bones in patients with flatfoot deformity: in vivo 3D study. Foot Ankle Int. 2011;32:1017-1022. [DOI] [PubMed] [Google Scholar]
- 21.Kleipool RP, Dahmen J, Vuurberg G, Oostra RJ, Blankevoort L, Knupp M, Stufkens SA. Study on the three-dimensional orientation of the posterior facet of the subtalar joint using simulated weight-bearing CT. J Orthop Res. 2019;37:197-204. [DOI] [PubMed] [Google Scholar]
- 22.Kocabiyik A, Misir A, Kizkapan TB, Yildiz KI, Kaygusuz MA, Alpay Y, Ezici A. Changes in hip, knee, and ankle coronal alignments after total hip arthroplasty with transverse femoral shortening osteotomy for unilateral Crowe type IV developmental dysplasia of the hip. J Arthroplasty. 2017;32:3449-3456. [DOI] [PubMed] [Google Scholar]
- 23.Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res. 2016;474:1886-1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krähenbühl N, Horn-Lang T, Hintermann B, Knupp M. The subtalar joint: A complex mechanism. EFORT Open Rev. 2017;2:309-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krähenbühl N, Siegler L, Deforth M, Zwicky L, Hintermann B, Knupp M. Subtalar joint alignment in ankle osteoarthritis. Foot Ankle Surg. 2019;25:143-149. [DOI] [PubMed] [Google Scholar]
- 26.Krähenbühl N, Tschuck M, Bolliger L, Hintermann B, Knupp M. Orientation of the subtalar joint: measurement and reliability using weightbearing CT scans. Foot Ankle Int. 2016;37:109-114. [DOI] [PubMed] [Google Scholar]
- 27.Ledoux WR, Sangeorzan BJ. Clinical biomechanics of the peritalar joint. Foot Ankle Clin. 2004;9:663-683. [DOI] [PubMed] [Google Scholar]
- 28.Lee K, Chang C, Park M, Kang S-B, Kim T, Chung C. Changes of knee joint and ankle joint orientations after high tibial osteotomy. Osteoarthritis Cartilage. 2015;23:232-238. [DOI] [PubMed] [Google Scholar]
- 29.Lenz AL, Krähenbühl N, Howell K, Lisonbee R, Hintermann B, Saltzman CL, Barg A. Influence of the ankle position and X-ray beam angulation on the projection of the posterior facet of the subtalar joint. Skeletal Radiol. 2019;48:1581-1589. [DOI] [PubMed] [Google Scholar]
- 30.Lintz F, Welck M, Bernasconi A, Thornton B, James, Cullen NP, Singh D, Goldberg A. 3D biometrics for hindfoot alignment using weightbearing CT. Foot Ankle Int. 2017;38:684-689. [DOI] [PubMed] [Google Scholar]
- 31.Lobenhoffer P. the Rationale of osteotomy around the knee. J Knee Surg. 2017;30:386-392. [DOI] [PubMed] [Google Scholar]
- 32.Ludlow JB, Ivanovic M. Weightbearing CBCT, MDCT, and 2D imaging dosimetry of the foot and ankle. Int J Diag Imaging. 2014;1:1-9. [Google Scholar]
- 33.Moreland JR, Bassett L, Hanker G. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745-749. [PubMed] [Google Scholar]
- 34.Mullaji A, Shetty GM. Persistent hindfoot valgus causes lateral deviation of weightbearing axis after total knee arthroplasty. Clin Orthop Relat Res. 2011;469:1154-1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mullaji AB, Shetty GM, Lingaraju A, Bhayde S. Which factors increase risk of malalignment of the hip-knee-ankle axis in TKA? Clin Orthop Relat Res. 2013;471:134-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Norton AA, Callaghan JJ, Amendola A, Phisitkul P, Wongsak S, Liu SS, Fruehling-Wall C. Correlation of knee and hindfoot deformities in advanced knee OA: compensatory hindfoot alignment and where it occurs. Clin Orthop Relat Res. 2015;473:166-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nosewicz TL, Knupp M, Bolliger L, Henninger HB, Barg A, Hintermann B. Radiological morphology of peritalar instability in varus and valgus tilted ankles. Foot Ankle Int. 2014;35:453-462. [DOI] [PubMed] [Google Scholar]
- 38.Ohi H, Iijima H, Aoyama T, Kaneda E, Ohi K, Abe K. Association of frontal plane knee alignment with foot posture in patients with medial knee osteoarthritis. BMC Musculoskelet Disord. 2017;18:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ollivier M, Parratte S, Lecoz L, Flecher X, Argenson J-N. Relation between lower extremity alignment and proximal femur anatomy. Parameters during total hip arthroplasty. Orthop Traumatol Surg Res. 2013;99:493-500. [DOI] [PubMed] [Google Scholar]
- 40.Pagenstert GI, Hintermann B, Barg A, Leumann A, Valderrabano V. Realignment surgery as alternative treatment of varus and valgus ankle osteoarthritis. Clin Orthop Relat Res. 2007;462:156-168. [DOI] [PubMed] [Google Scholar]
- 41.Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of uniapical angular deformities of the tibia or femur. Clin Orthop Relat Res. 1992:48-64. [PubMed] [Google Scholar]
- 42.Rabe KG, Segal NA, Waheed S, Anderson DD. The effect of arch drop on tibial rotation and tibiofemoral contact stress in postpartum women. PM R. 2018;10:1137-1144. [DOI] [PubMed] [Google Scholar]
- 43.Richter M, Seidl B, Zech S, Hahn S. PedCAT for 3D-imaging in standing position allows for more accurate bone position (angle) measurement than radiographs or CT. Foot Ankle Surg. 2014;20:201-207. [DOI] [PubMed] [Google Scholar]
- 44.Riegger-Krugh C, Keysor JJ. Skeletal malalignments of the lower quarter: correlated and compensatory motions and postures. J Orthop Sports Phys Ther. 1996;23:164-170. [DOI] [PubMed] [Google Scholar]
- 45.Rosset A, Spadola L, Ratib O. OsiriX: an open-source software for navigating in multidimensional DICOM images. J Digit imaging. 2004;17:205-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sainani K. The importance of accounting for correlated observations. PM R. 2010;2:858-861. [DOI] [PubMed] [Google Scholar]
- 47.Sarrafian SK. Biomechanics of the subtalar joint complex. Clin Orthop Relat Res. 1993:17-26. [PubMed] [Google Scholar]
- 48.Schaefer KL, Sangeorzan BJ, Fassbind MJ, Ledoux WR. The comparative morphology of idiopathic ankle osteoarthritis. J Bone Joint Surg Am. 2012;94:e181. [DOI] [PubMed] [Google Scholar]
- 49.Shah SM, Roberts J, Picard F. Ankle and hindfoot symptoms after medial open wedge high tibial osteotomy. J Knee Surg. 2019;32:269-273. [DOI] [PubMed] [Google Scholar]
- 50.Sheehy L, Felson D, Zhang Y, Niu J, Lam Y-M, Segal N, Lynch J, Cooke TDV. Does measurement of the anatomic axis consistently predict hip-knee-ankle angle (HKA) for knee alignment studies in osteoarthritis? Analysis of long limb radiographs from the multicenter osteoarthritis (MOST) study. Osteoarthritis Cartilage. 2011;19:58-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420. [DOI] [PubMed] [Google Scholar]
- 52.Tanaka T, Takayama K, Hashimoto S, Kanzaki N, Hayashi S, Kuroda R, Matsumoto T. Radiographic analysis of the lower limbs using the hip–calcaneus line in healthy individuals and in patients with varus knee osteoarthritis. Knee. 2017;24:1146-1152. [DOI] [PubMed] [Google Scholar]
- 53.Thelen P, Delin C, Folinais D, Radier C. Evaluation of a new low-dose biplanar system to assess lower-limb alignment in 3D: a phantom study. Skeletal Radiol. 2012;41:1287-1293. [DOI] [PubMed] [Google Scholar]
- 54.Thienpont E, Schwab P-E, Cornu O, Bellemans J, Victor J. Bone morphotypes of the varus and valgus knee. Arch Orthop Trauma Surg. 2017;137:393-400. [DOI] [PubMed] [Google Scholar]
- 55.Valderrabano V, Horisberger M, Russell I, Dougall H, Hintermann B. Etiology of ankle osteoarthritis. Clin Orthop Relat Res. 2009;467:1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Victor JM, Bassens D, Bellemans J, Gürsu S, Dhollander AA, Verdonk PC. Constitutional varus does not affect joint line orientation in the coronal plane. Clin Orthop Relat Res. 2014;472:98-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang B, Saltzman CL, Chalayon O, Barg A. Does the subtalar joint compensate for ankle malalignment in end-stage ankle arthritis? Clin Orthop Relat Res. 2015;473:318-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wiewiorski M, Hoechel S, Anderson AE, Nowakowski AM, DeOrio JK, Easley ME, Nunley JA, Valderrabano V, Barg A. Computed tomographic evaluation of joint geometry in patients with end-stage ankle osteoarthritis. Foot Ankle Int. 2016;37:644-651. [DOI] [PubMed] [Google Scholar]