Abstract
Background
The incidence of revision THA continues to increase and there is a need to identify risk factors contributing to postoperative complications. Anesthesia type has been shown to be associated with complication rates in patients who undergo primary THA, but it is not clear whether the same is true among patients undergoing revision THA.
Questions/purposes
(1) After controlling for confounding variables, in the setting of a large-database analysis, is spinal anesthesia associated with a lower risk of death, readmission, reoperation, postoperative transfusion, thromboembolic events, surgical site infection (SSI), and re-intubation among patients undergoing revision THA?
Methods
The American College of Surgeons-National Surgical Quality Improvement (ACS-NSQIP) database was queried for patients undergoing aseptic, revision THA with either spinal or general anesthesia. Coarsened exact matching was used to match patients based on several baseline characteristics, including age, sex, body mass index, surgery type (Current Procedural Terminology code), and the modified Frailty Index score. Coarsened exact matching is a statistical method of exact matching that matches on chosen characteristics, in which continuous variables may be temporarily coarsened (such as, into discrete categorical variables) to facilitate matching. This method is an alternate to and requires less estimation than traditional propensity score matching. Then, using a model controlling for baseline patient characteristics and operative time, we performed multivariate logistic and linear regression analyses of matched cohorts to examine differences in mortality, readmission, reoperation, thromboembolic events, transfusion, SSI, and re-intubation.
Results
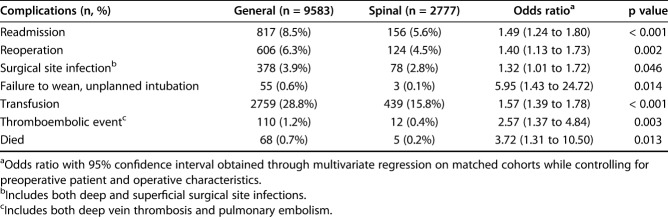
After statistical matching and controlling for baseline demographic variables, surgery type (one- or two-component revision), surgical time and modified Frailty Index we found that patients receiving general anesthesia had higher odds of mortality (OR 3.72 [95% CI 1.31 to 10.50]; p = 0.013), readmission (OR 1.49 [95% CI 1.24 to 1.80]; p < 0.001), reoperation (OR 1.40 [95% CI 1.13 to 1.73]; p = 0.002), thromboembolic events (OR 2.57 [95% CI 1.37 to 4.84]; p = 0.003), SSI (OR 1.32 [95% CI 1.01 to 1.72]; p = 0.046), postoperative transfusion (OR 1.57 [95%CI 1.39 to 1.78]; p < 0.001) and unplanned intubation or failure to wean off intubation (OR 5.95 [95% CI 1.43 to 24.72]; p = 0.014).
Conclusions
In patients undergoing revision THA, spinal anesthesia is associated with a decreased risk of several complications. The current investigation suggests that, when practical (such as when long surgical times or changes to the surgical plan are not anticipated), spinal anesthesia should be considered for use during revision THA.
Level of Evidence
Level III, therapeutic study.
Introduction
THA represents one of the most successful orthopaedic procedures performed and its incidence continues to rise [24, 25, 27]. Although general anesthesia is commonly used for patients undergoing THA, recent data support the efficacy and safety of spinal anesthesia in patients undergoing this procedure [3, 8-11, 13, 16, 29, 38]. In primary THA patients, spinal anesthesia has been shown to reduce operative time, postoperative opiate consumption, thromboembolic events, surgical site infection (SSI), and blood transfusions [3, 8, 11, 28].
Although robust data exist to support the use of neuraxial anesthesia in patients who undergo primary THA [3, 8, 10, 11], the same data do not exist for patients undergoing revision THA. Several studies have examined the risk factors associated with SSI [36], length of stay, and readmission [21] in patients undergoing revision arthroplasty, but anesthesia type was not specifically examined. One study found general anesthesia to be independently associated with “major complications” after revision THA; however, specific complications were not examined [26]. It should be noted that analysis of pooled, dissimilar complications can be misleading and thus, further clarification is needed [5]. Because revision THA is associated with higher a proportions of complication than primary THA, it is important to determine the effect of anesthesia type in the revision THA patient cohort.
Therefore, we asked (1) After controlling for confounding variables, in the setting of a large-database analysis, is spinal anesthesia associated with a lower risk of death, readmission, reoperation, thromboembolic events, SSI, postoperative transfusion, and re-intubation among patients undergoing revision THA?
Patients and Materials
Patient Selection
Patients included in the present study were selected from the American College of Surgeons-National Surgical Quality Improvement (ACS-NSQIP) database. More than 700 hospitals contribute to the ACS-NSQIP database and these centers are located in 49 states and nine different countries [1]. This database has grown in both the number of participating hospitals and in use in previous studies [3, 40, 42, 47, 48]. The database contains high-quality data and captures 95% of postoperative complications and outcomes by employing multiple collection techniques and quality assurance measures. The database collects several preoperative and operative variables associated with a patient’s hospital stay, including 30-day postoperative complications and 30-day readmissions.
Patients in the present study were selected from the database using the following Current Procedural Terminology (CPT) codes: 27134 (revision THA, both components), 27137 (revision THA, acetabular component only), and 27138 (revision THA, femoral component only). Given the nature of the ACS-NSQIP database and its inability to discern the precise type of revision performed in patients with sepsis (modular revision, one-stage, or two-stage), CPT codes 27090 (removal of hip prosthesis) and 27091 (removal of prothesis, with or without spacer placement) were not included in this study. To further ensure that patients undergoing revision for infection were excluded, we excluded those with the appropriate ICD-9 and ICD-10 codes (ICD-9 codes 996.66 and T84.5). All patients who underwent the above procedures under either general anesthesia or spinal anesthesia (not including epidural anesthesia) were initially included in the study. Patients who underwent revision THA under other anesthesia types were excluded. The following exclusion criteria were additionally applied: patients with sepsis or pre-sepsis on arrival, preoperative malignancy, emergent status, and those with missing data.
Patient Demographics
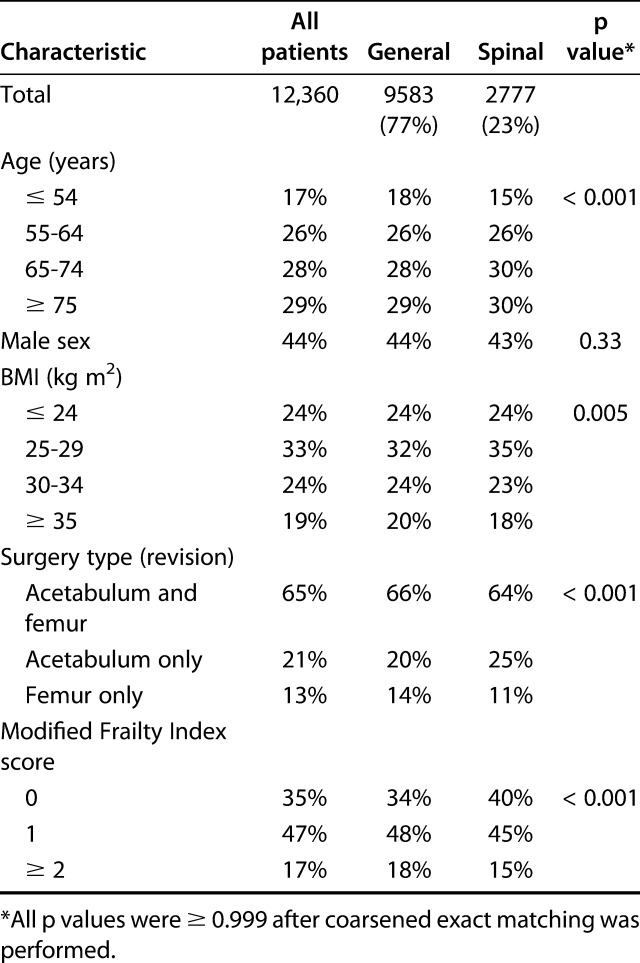
After the inclusion and exclusion criteria were applied, 3694 patients were excluded, resulting in 12,360 patients who were included in the study. Seventy-seven percent (9583 of 12,360 patients) underwent surgery with general anesthesia. There were differences in preoperative characteristics between the groups (Table 1). The general anesthesia group included patients who were younger (more patients ≤ 54 years old), frailer (more patients with a modified Frailty Index score ≥ 2), and heavier (more patients with BMI ≥ 35 kg/m2). General anesthesia was used for more femur-only revisions (14% versus 11%, general versus spinal; p < 0.001) than for acetabulum-only revisions (20% versus 25%; p < 0.001). We performed coarsened exact matching to account for these preoperative differences. Coarsened exact matching is a method of statistical matching that temporarily coarsens data (in this case, for example, age from a continuous variable into discrete categorical groups) for the purposes of exact matching. Coarsened exact matching allows for less assumption than other matching methods, including propensity score matching and provides less sample imbalance in many cases. Its use has been validated in both simulated and real datasets [14, 15]. After matching with coarsened exact matching, further analysis can then be conducted on the matched cohorts with typical multivariable analysis. Coarsened exact matching achieved group balance with no differences between the groups (p > 0.999) (Table 1).
Table 1.
Demographic, operative, and comorbidity characteristics
Patient Demographics and the Modified Frailty Index
To control for baseline characteristics, we evaluated the following variables for each patient: age, sex, BMI, and the modified Frailty Index score (mFI). As mentioned above, these variables were used in matching patients and were subsequently also used as controls in the multivariate model. Because frailty can affect outcomes after THA [4, 44], we collected and calculated the mFI score for each patient. This five-item index has been shown to retain its predictive power compared with its 11-item counterpart [42] and has been used successfully in multiple areas of orthopaedics, including THA [41, 44, 48]. The mFI score is calculated (1 point per item present; range 0 to 5) based on the presence or absence of the following five items: history of diabetes mellitus, congestive heart failure (new diagnosis or exacerbation of chronic congestive heart failure within 30 days of surgery), hypertension requiring medication, chronic obstructive pulmonary disease or pneumonia; and non-independent functional status (partially or completely dependent in activities of daily living). This score, in addition to the above baseline patient characteristics, was used as a control and to ensure similar baseline characteristics between the groups.
Surgical Complexity, Outcomes, and Complication Data
We compared surgical times between patients receiving general and spinal anesthesia. Specifically, we compared operative time, which was defined as time from incision to skin closure. The mean operative time for those undergoing general anesthesia was 153 ± 78 minutes and for those receiving spinal anesthesia was 119 ± 61 minutes. Adjusted analysis on matched cohorts found a difference of 32.6 minutes (95% CI 29.3 to 35.8; p < 0.001) between groups.
Several factors contribute to operative time. Surgical complexity varies in patients who undergo revision THA and has a major influence on many of our chosen outcome variables and clearly influences operative time. Although previous reports have demonstrated that spinal anesthesia shortens operative time compared with general anesthesia in primary THA [3], to limit selection bias, we assumed that anesthesia type had no influence on operative time in revision THA. Instead, the effect of case complexity, as well as surgeon and center variability were felt to likely have a much larger influence on operative time. As mentioned above, we found operative time to be different between groups on multivariate linear regression performed on matched cohorts, and, therefore, we included it as a control in the multivariate analysis assessing our primary outcomes. This was done to limit the effect of the unmeasured variables (that is, surgeon efficiency and experience, case complexity, center efficiency).
To assess outcomes and complications, we collected 30-day postoperative complication data for each patient. These data included the following outcomes: mortality, unplanned intubation and failure to wean from ventilator, thromboembolic events (deep vein thrombosis and pulmonary embolism), SSI (deep and superficial), postoperative transfusion, readmission, and reoperation. (Table 2).
Table 2.
Link between general anesthesia and complications in revision THA, 2011-2017
Statistical Analysis
The statistical analysis for this study was performed using IBM SPSS Version 25 (IBM Corp, Armonk, NY, USA). We compared baseline characteristics between those who underwent surgery under spinal anesthesia and those with general anesthesia. We used coarsened exact matching to match patients for a number of patient-specific covariates (Table 1), balancing the data and controlling for the confounding influence of statistically different preoperative variables, thus reducing model dependence. We chose coarsened exact matching because it can produce matched data that has less model imbalance and statistical bias than other matching techniques, including propensity score matching [22]. Then, we performed a further analysis on matched groups using weights provided by the coarsened exact matching method. A multivariate logistic regression analysis was performed using a model that controlled for all the aforementioned baseline patient characteristics, mFI score, and operative time. Subgroup analysis was performed using the same model but included only patients in each modified frailty index category.
Results
Anesthesia Type and Postoperative Complications
After controlling for confounding variables like patient demographics (age, sex, BMI), modified frailty index, and operative characteristics (CPT code and operative time), we found that general anesthesia was associated with increased odds of complications. Specifically, when compared with those receiving spinal anesthesia, patients receiving general anesthesia had increased odds of the following: readmission (OR 1.49 [95% CI 1.24 to 1.80]; p < 0.001), reoperation (OR 1.40 [95% CI 1.13 to 1.73]; p = 0.002), SSI (OR 1.32 [95% CI 1.01 to 1.72]; p = 0.046), failure to wean from intubation or reintubation (OR 5.95 [95% CI 1.43 to 24.72]; p = 0.014), transfusion (OR 1.57 [95% CI 1.39 to 1.78]; p < 0.001), thromboembolic events (OR 2.57 [95% CI 1.37 to 4.84]; p = 0.003), and mortality (OR 3.72 [95% CI 1.31 to 10.50]; p = 0.013) (Table 2).
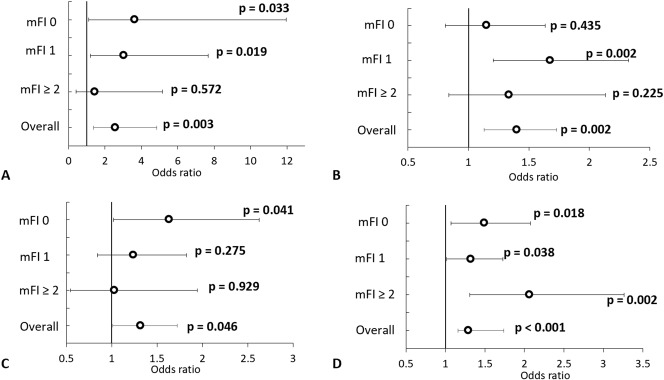
Subgroup analysis of patients in each mFI category (0, 1, ≥ 2) revealed that general anesthesia was associated with increased odds of certain complications in both the frail (mFI ≥ 2) and not frail (mFI ≤ 1) patients. This analysis was performed for readmission, reoperation, thromboembolic events, and SSI. Specifically, in those with a mFI score of 0, general anesthesia was associated with increased odds of readmission (OR 1.49 [95% CI 1.07 to 2.08]; p = 0.018), thromboembolic events (OR 3.65 [95% CI 1.11 to 11.96]; p = 0.033), and SSI (OR 1.64 [95% CI 1.02 to 2.62]; p = 0.041). Those with a mFI score of 1, had increased odds of readmission (OR 1.32 [95% CI 1.02 to 1.73]; p = 0.038), thromboembolic events (OR 3.04 [95% CI 1.20 to 7.68]; p = 0.019), and reoperation (OR 1.67 [95% CI 1.21 to 2.3]; p = 0.002). Last, frail patients (mFI ≥ 2) had increased risk of readmission (OR 2.06 [95% CI 1.31 to 3.26]; p = 0.002) (Fig. 1 A-D).
Fig. 1 A-D.
This forest plot demonstrates the adjusted probability (odds ratio and 95% confidence interval) of (A) thromboembolic event, (B) reoperation (C) SSI, and (D) reoperation as it relates to the patient modified Frailty Index score and anesthesia type. Results shown compare general anesthesia to spinal anesthesia with odds ratios > 1 indicating increased odds of an event when patients received general anesthesia. mFI = modified Frailty Index.
Discussion
The incidence of revision THA continues to increase in the United States and abroad [6, 24, 25, 27, 37] and complication rates remain higher than those observed in primary joint arthroplasty [26]. Therefore, there is a need to identify risk factors contributing to complications in patients undergoing revision THA, with an emphasis on risk reduction. In patients undergoing primary THA there is a great amount of evidence to support that spinal anesthesia is associated with lower risk than general anesthesia [3, 8-11, 13, 28, 29, 38]. The same has been demonstrated in revision TKA [47]. However, in patients undergoing revision THA, this relationship has been examined minimally. The current investigation used the prospectively collected ACS-NSQIP data to examine the effect of anesthesia type on outcomes after revision THA and found that general anesthesia was associated with increased odds of multiple complications compared with spinal anesthesia. This was true for both frail and healthy patients included in the study. The results of this study, therefore, would suggest that in the appropriate patient, spinal anesthesia is preferable to general anesthesia for revision THA.
There are several limitations to this study, most of which are inherent to the general limitations of large database investigations, specifically the ACS-NSQIP database. First, the ACS-NSQIP database does not include any information regarding surgical complexity beyond documentation of CPT codes (for example, one- versus two-component revision). This is potentially problematic, as surgical complexity undoubtedly has a large influence on most of our outcome variables. To mute this effect, we used coarsened exact matching to statistically match the groups (general and spinal anesthesia) and then controlled for baseline patient demographic variables, CPT codes, and operative time in our final analysis. Despite these efforts, it must be acknowledged that there are multiple unmeasured variables that remain uncontrolled in our analysis. For example, surgeon and center experience and volume are not reported in this dataset and these variables are known to influence outcomes [18-20, 39, 46, 49]. It is possible that higher-volume centers, with perhaps better perioperative management and processes, preferentially chose spinal anesthetics, leading to observed differences between groups not completely explained by anesthetic choice. Similarly, given the retrospective nature of this investigation, only associations can be identified, and causality cannot be determined. Specifically, we caution readers from interpreting the observed difference of 33 minutes in operative time as a result of only anesthetic choice. Basques et al. [2] previously demonstrated shorter operative times in primary THA with spinal anesthesia [3]; however, their analysis was similarly limited by unmeasured confounding. Additionally, in the setting of revision THA, providers may make their anesthetic choice, at least in part, based on anticipated surgical time, further biasing this analysis. Therefore, for the purposes of our analysis, operative time was viewed as a variable to be controlled for, not an outcome.
Further, because the ACS-NSQIP database is a general surgical database, the available outcomes are primarily medical in nature, and orthopaedic outcomes (such as implant position on radiographs, pain scores, and functional outcomes) could not be analyzed. Another weakness is that in the current investigation, patients undergoing revision arthroplasty with epidural anesthesia or for septic indications were excluded. Although this allowed for a cleaner analysis of outcomes, our results may not be generalizable to patients undergoing revision with epidural anesthetic or for periprosthetic joint infection. Lastly, as mentioned above, it may have been difficult to truly isolate anesthesia type in the analysis. However, we conducted our analysis using matched cohorts and controlled for available patient demographic and comorbidity information, isolating anesthesia type to the greatest possible extent.
Despite these limitations, the results of this investigation are important and must be viewed in the context of existing evidence. We found that use of spinal anesthesia was associated with lower odds of thromboembolic events than was general anesthesia in patients undergoing revision THA. Although perhaps not surprising, as neuraxial anesthesia has previously been associated with decreased risk of thromboembolic events [2, 13, 30, 33, 43, 50], this is the first paper to demonstrate a similar benefit in revision THA. Although a prior analysis of the NSQIP database in primary hip arthroplasty showed no difference in thromboembolic events on adjusted analysis [3], the incidence of thromboembolic events observed in that study varied from ours—especially in the general anesthesia group (general anesthesia: 1.2% in revision THA versus 0.6% in primary THA [3]; spinal anesthesia: 0.4% in revision THA versus 0.6% in primary [3] THA). This observed difference could be a result of baseline patient differences or the fundamentally more extensive procedure, with longer associated operative times, that is revision surgery. The reason for the observed decreased occurrence of thromboembolic events in the spinal group is likely multifactorial. General anesthesia has previously been demonstrated to interfere with fibrinolysis and the coagulation cascade [32]. Additionally, spinal anesthetic invokes less surgical stress response relative to general anesthesia and its vasodilatory effects are thought to increase peripheral blood flow, leading to hemodilution and decreased blood viscosity [23, 31].
Our results also indicated that spinal anesthesia is associated with lower odds of failure to wean from or unplanned intubation, SSI, and postoperative transfusion. Prior work has demonstrated an association between increased pulmonary complications and general anesthesia in patients with orthopaedic conditions, specifically those undergoing THA [3, 11, 13]. Therefore, although not previously reported for revision THA patients, our study’s finding that there are increased odds of prolonged or unplanned intubation with general anesthesia is not entirely unanticipated. Similarly, SSI has been previously reported to be increased with general anesthesia when compared with neuraxial anesthesia [8, 11, 34, 35]. This relationship has been demonstrated in primary THA [11] but not in the revision THA cohort. Although our results nearly missed significance, there are several reasons that spinal anesthesia may influence infection rates, including a reduction in the autonomic pain response, decreasing local vasoconstriction and increasing tissue oxygen delivery [7, 8, 45]; decreased surgical stress response that avoids preoccupation of the immune system [8], and immune cell dysfunction as a result of volatile anesthetic use [23]. Lastly, transfusion rates have also been repeatedly associated with anesthetic choice in the orthopaedic patient, including in primary THA and revision TKA [3, 13, 34, 35, 38, 47]. Decreased surgical blood loss with neuraxial anesthesia is thought to occur mostly as a result of sympathetic blockade, which decreases peripheral vascular resistance, venous return and as a result cardiac output. This hypotensive anesthesia leads to less surgical blood loss- translating into lower transfusion rates as observed in this study.[12, 17]
Given these increased rates of complications, our observed increased odds of readmission, reoperation, and mortality are not unexpected. Database evaluation of neuraxial anesthesia in primary THA patients has not demonstrated a mortality benefit [3, 11]. Similar to the discussion of thromboembolic events above, the incidence of mortality with general anesthesia after revision THA in our study is much higher than that reported after primary THA (0.71% versus 0.15% [3], respectively). It seems most likely that any differences between treatments are enhanced in the revision setting with longer, more invasive procedures. It should be noted that although the incidence rates of the outcomes included in this study are low, the adjusted differences between groups was often large, making these differences clinically important.
In conclusion, in patients undergoing revision THA, spinal anesthesia is associated with a decreased risk of multiple complications, including thromboembolic events, SSI, postoperative transfusion and mortality. Although the current investigation cannot determine causality, the results suggest that when practical (such as when long surgical times or changes to the surgical plan are not anticipated), spinal anesthesia should be strongly considered for patients undergoing revision THA when it is not otherwise clinically contraindicated.
Acknowledgments
None.
Footnotes
One of the authors (TLB) certifies that he has received payments or benefits in an amount of USD < 10,000 from Zimmer-Biomet (Warsaw, IN, USA); payments or benefits in an amount of < 10,000 from Smith & Nephew (London, UK); payments or benefits in an amount of USD < 10,000 from OrthoSensor (Dania Beach, FL, USA); and payments or benefits in an amount of < 10,000 from TJO Inc (Salt Lake City, UT, USA), all outside the submitted work. One of the authors (GG) certifies that he has received payments or benefits in an amount of USD < 10,000 from Smith & Nephew; payments or benefits in an amount of USD < 10,000 from KCI (San Antonio, TX, USA); and payments or benefits in an amount of USD < 10,000 for TJO Inc, all outside the submitted work.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his institution waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.American College of Surgeons. User Guide for the 2015 ACS NSQIP Participant Use File (PUF). https://www.facs.org/∼/media/files/quality%20programs/nsqip/nsqip_puf_userguide_2016.ashx. Accessed May 20, 2016.
- 2.Basques BA, Bohl DD, Golinvaux NS, Samuel AM, Grauer JG. General versus spinal anaesthesia for patients aged 70 years and older with a fracture of the hip. Bone Joint J. 2015;97-B:689-695. [DOI] [PubMed] [Google Scholar]
- 3.Basques BA, Toy JO, Bohl DD, Golinvaux NS, Grauer JN. General compared with spinal anesthesia for total hip arthroplasty. J Bone Joint Surg Am. 2015;97:455-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bellamy JL, Runner RP, Vu CCL, Schenker ML, Bradbury TL, Roberson JR. Modified Frailty Index is an effective risk assessment tool in primary total hip arthroplasty. J Arthroplasty. 2017;32:2963-2968. [DOI] [PubMed] [Google Scholar]
- 5.Bohl DD, Singh K, Grauer JN. Nationwide databases in orthopaedic surgery research. J Am Acad Orthop Surg. 2016;24:673-682. [DOI] [PubMed] [Google Scholar]
- 6.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128-133. [DOI] [PubMed] [Google Scholar]
- 7.Buggy DJ, Doherty WL, Hart EM, Pallett EJ. Postoperative wound oxygen tension with epidural or intravenous analgesia: a prospective, randomized, single-blind clinical trial. Anesthesiology. 2002;97:952-958. [DOI] [PubMed] [Google Scholar]
- 8.Chang CC, Lin HC, Lin HW, Lin HC. Anesthetic management and surgical site infections in total hip or knee replacement: a population-based study. Anesthesiology. 2010;113:279-284. [DOI] [PubMed] [Google Scholar]
- 9.Davis FM, Laurenson VG, Gillespie WJ, Wells JE, Foate J, Newman E. Deep vein thrombosis after total hip replacement. A comparison between spinal and general anaesthesia. J Bone Joint Surg Br. 1989;71:181-185. [DOI] [PubMed] [Google Scholar]
- 10.Donauer K, Bomberg H, Wagenpfeil S, Volk T, Meissner W, Wolf A. Regional vs. general anesthesia for total knee and hip replacement: An analysis of postoperative pain perception from the international PAIN OUT registry. Pain Pract. 2018;18:1036-1047. [DOI] [PubMed] [Google Scholar]
- 11.Helwani MA, Avidan MS, Ben Abdallah A, Kaiser DJ, Clohisy JC, Hall BL, Kaiser HA. Effects of regional versus general anesthesia on outcomes after total hip arthroplasty: a retrospective propensity-matched cohort study. J Bone Joint Surg Am. 2015;97:186-193. [DOI] [PubMed] [Google Scholar]
- 12.Holte K, Foss NB, Svensen C, Lund C, Madsen JL, Kehlet H. Epidural anesthesia, hypotension, and changes in intravascular volume. Anesthesiology. 2004;100:281-286. [DOI] [PubMed] [Google Scholar]
- 13.Hu S, Zhang ZY, Hua YQ, Li J, Cai ZD. A comparison of regional and general anaesthesia for total replacement of the hip or knee: a meta-analysis. J Bone Joint Surg Br. 2009;91:935-942. [DOI] [PubMed] [Google Scholar]
- 14.Iacus S, King G, Porro G. Multivariate Matching Methods That Are Monotonic Imbalance Bounding. Journal of the American Statistical Association. 2011;106:345-361. [Google Scholar]
- 15.Iacus S, King G, Porro G. Causal inference without balance checking: coarsened exact matching. Political Analysis. 2012;20:1-24. [Google Scholar]
- 16.Indelli PF, Grant SA, Nielsen K, Vail TP. Regional anesthesia in hip surgery. Clin Orthop Relat Res. 2005;441:250-255. [DOI] [PubMed] [Google Scholar]
- 17.Juelsgaard P, Larsen UT, Sorensen JV, Madsen F, Soballe K. Hypotensive epidural anesthesia in total knee replacement without tourniquet: reduced blood loss and transfusion. Reg Anesth Pain Med. 2001;26:105-110. [DOI] [PubMed] [Google Scholar]
- 18.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004;86:1909-1916. [DOI] [PubMed] [Google Scholar]
- 19.Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2001;83:1622-1629. [DOI] [PubMed] [Google Scholar]
- 20.Katz JN, Mahomed NN, Baron JA, Barrett JA, Fossel AH, Creel AH, Wright J, Wright EA, Losina E. Association of hospital and surgeon procedure volume with patient-centered outcomes of total knee replacement in a population-based cohort of patients age 65 years and older. Arthritis Rheum. 2007;56:568-574. [DOI] [PubMed] [Google Scholar]
- 21.Keswani A, Lovy AJ, Robinson J, Levy R, Chen D, Moucha CS. Risk factors predict increased length of stay and readmission rates in revision joint arthroplasty. J Arthroplasty. 2016;31:603-608. [DOI] [PubMed] [Google Scholar]
- 22.King G, Neilsen R. Why propensity scores should not be used for matching. Political Analysis. 2019:1-20. [Google Scholar]
- 23.Kurosawa S, Kato M. Anesthetics, immune cells, and immune responses. J Anesth. 2008;22:263-277. [DOI] [PubMed] [Google Scholar]
- 24.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-785. [DOI] [PubMed] [Google Scholar]
- 25.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606-2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liodakis E, Bergeron SG, Zukor DJ, Huk OL, Epure LM, Antoniou J. Perioperative Complications and Length of Stay After Revision Total Hip and Knee Arthroplasties: An Analysis of the NSQIP Database. J Arthroplasty. 2015;30:1868-1871. [DOI] [PubMed] [Google Scholar]
- 27.Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, Jiranek WA, Berry DJ. Prevalence of Total Hip and Knee Replacement in the United States. J Bone Joint Surg Am. 2015;97:1386-1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mauermann WJ, Shilling AM, Zuo Z. A comparison of neuraxial block versus general anesthesia for elective total hip replacement: a meta-analysis. Anesth Analg. 2006;103:1018-1025. [DOI] [PubMed] [Google Scholar]
- 29.Maurer SG, Chen AL, Hiebert R, Pereira GC, Di Cesare PE. Comparison of outcomes of using spinal versus general anesthesia in total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2007;36:E101-106. [PubMed] [Google Scholar]
- 30.McKenzie PJ, Wishart HY, Gray I, Smith G. Effects of anaesthetic technique on deep vein thrombosis. A comparison of subarachnoid and general anaesthesia. Br J Anaesth. 1985;57:853-857. [DOI] [PubMed] [Google Scholar]
- 31.Mitchell D, Friedman RJ, Baker JD, 3rd, Cooke JE, Darcy MD, Miller MC., 3rd Prevention of thromboembolic disease following total knee arthroplasty. Epidural versus general anesthesia. Clin Orthop Relat Res. 1991:109-112. [PubMed] [Google Scholar]
- 32.Modig J, Borg T, Bagge L, Saldeen T. Role of extradural and of general anaesthesia in fibrinolysis and coagulation after total hip replacement. Br J Anaesth. 1983;55:625-629. [DOI] [PubMed] [Google Scholar]
- 33.Modig J, Borg T, Karlstrom G, Maripuu E, Sahlstedt B. Thromboembolism after total hip replacement: role of epidural and general anesthesia. Anesth Analg. 1983;62:174-180. [PubMed] [Google Scholar]
- 34.Park YB, Chae WS, Park SH, Yu JS, Lee SG, Yim SJ. Comparison of short-term complications of general and spinal anesthesia for primary unilateral total knee arthroplasty. Knee Surg Relat Res. 2017;29:96-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S, Callaghan JJ. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg Am. 2013;95:193-199. [DOI] [PubMed] [Google Scholar]
- 36.Pugely AJ, Martin CT, Gao Y, Schweizer ML, Callaghan JJ. The iIncidence of and risk factors for 30-day surgical site infections following primary and revision total joint arthroplasty. J Arthroplasty. 2015;30:47-50. [DOI] [PubMed] [Google Scholar]
- 37.Rajaee SS, Campbell JC, Mirocha J, Paiement GD. Increasing burden of total hip arthroplasty revisions in patients between 45 and 64 years of age. J Bone Joint Surg Am. 2018;100:449-458. [DOI] [PubMed] [Google Scholar]
- 38.Rashiq S, Finegan BA. The effect of spinal anesthesia on blood transfusion rate in total joint arthroplasty. Can J Surg. 2006;49:391-396. [PMC free article] [PubMed] [Google Scholar]
- 39.Ravi B, Jenkinson R, Austin PC, Croxford R, Wasserstein D, Escott B, Paterson JM, Kreder H, Hawker GA. Relation between surgeon volume and risk of complications after total hip arthroplasty: propensity score matched cohort study. BMJ. 2014;348:g3284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Runner RP, Bellamy JL, Vu CCL, Erens GA, Schenker ML, Guild GN., 3rd Modified Frailty Index is an effective risk assessment tool in primary total knee arthroplasty. J Arthroplasty. 2017;32:S177-S182. [DOI] [PubMed] [Google Scholar]
- 41.Segal DN, Wilson JM, Staley C, Michael KW. The 5-item modified Frailty Index is predictive of 30-day postoperative complications in patients undergoing kyphoplasty vertebral augmentation. World Neurosurg. 2018;116:e225-e231. [DOI] [PubMed] [Google Scholar]
- 42.Subramaniam S, Aalberg JJ, Soriano RP, Divino CM. New 5-factor modified Frailty Index using American College of Surgeons NSQIP data. J Am Coll Surg. 2018;226:173-181 e178. [DOI] [PubMed] [Google Scholar]
- 43.Thorburn J, Louden JR, Vallance R. Spinal and general anaesthesia in total hip replacement: frequency of deep vein thrombosis. Br J Anaesth. 1980;52:1117-1121. [DOI] [PubMed] [Google Scholar]
- 44.Traven SA, Reeves RA, Sekar MG, Slone HS, Walton ZJ. New 5-Factor Modified Frailty Index predicts morbidity and mortality in primary hip and knee arthroplasty. J Arthroplasty. 2019;34:140-144. [DOI] [PubMed] [Google Scholar]
- 45.Treschan TA, Taguchi A, Ali SZ, Sharma N, Kabon B, Sessler DI, Kurz A. The effects of epidural and general anesthesia on tissue oxygenation. Anesth Analg. 2003;96:1553-1557, table of contents. [DOI] [PubMed] [Google Scholar]
- 46.Tsai TC, Joynt KE, Orav EJ, Gawande AA, Jha AK. Variation in surgical-readmission rates and quality of hospital care. N Engl J Med. 2013;369:1134-1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wilson JM, Farley KX, Erens GA, Guild GN., 3rd General vs spinal anesthesia for revision total knee arthroplasty: Do complication rates differ? J Arthroplasty. 3/2019, E-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- 48.Wilson JM, Holzgrefe RE, Staley CA, Schenker ML, Meals CG. Use of a 5-item modified Frailty Index for risk stratification in patients undergoing surgical management of distal radius fractures. The Journal of hand surgery. 2018;43:701-709. [DOI] [PubMed] [Google Scholar]
- 49.Yasunaga H, Tsuchiya K, Matsuyama Y, Ohe K. High-volume surgeons in regard to reductions in operating time, blood loss, and postoperative complications for total hip arthroplasty. J Orthop Sci. 2009;14:3-9. [DOI] [PubMed] [Google Scholar]
- 50.Zhou LY, Gu W, Liu Y, Ma ZL. Effects of inhalation anesthesia vs. total intravenous anesthesia (TIVA) vs. spinal-epidural anesthesia on deep vein thrombosis after total knee arthroplasty. Med Sci Monit. 2018;24:67-75. [DOI] [PMC free article] [PubMed] [Google Scholar]