Abstract
Background
Current brace weaning criteria for adolescents with idiopathic scoliosis (AIS) are not well defined. Risser Stage 4, ≥ 2 years since the onset of menarche, and no further increase in body height over 6 months are considered justifications for stopping bracing. However, despite adherence to such standards, curve progression still occurs in some patients, and so better criteria for brace discontinuation are needed.
Questions/purposes
(1) Is no change in height measurements over 6 months and Risser Stage 4 sufficient for initiating brace weaning? (2) What is the association between larger curves (45°) at brace weaning and the progression risk? (3) Are a more advanced Risser stage, Sanders stage, or distal radius and ulna classification associated with a decreased risk of curve progression? (4) When should we wean patients with AIS off bracing to reduce the time for brace wear while limiting the risk of postweaning curve progression?
Methods
All AIS patients who were weaned off their braces from June 2014 to March 2016 were prospectively recruited and followed up for at least 2 years after weaning. A total of 144 patients were recruited with mean followup of 36 ± 21 months. No patients were lost to followup. Patients were referred for brace weaning based on the following criteria: they were Risser Stage 4, did not grow in height in the past 6 months of followup, and were at least 2 years postmenarche. Skeletal maturity was assessed with Risser staging, Sanders staging, and the distal radius and ulna classification. Curve progression was determined as any > 5° increase in the Cobb angle between two measurements from any subsequent six monthly followup visits. All radiographic measurements were performed by spine surgeons independently as part of their routine consultations and without knowledge of this study. Statistical analyses included an intergroup comparison of patients with and without curve progression, binomial stepwise logistic regression analysis, odds ratios (ORs) with their 95% confidence intervals (CIs), and a risk-ratio calculation. A reasonable protective maturity stage would generate an OR < 1.
Results
Among patients braced until they had no change in height for 6 months, were 2 years postmenarche for girls, and Risser Stage 4, 29% experienced curve progression after brace weaning. Large curves (≥ 45°) were associated with greater curve progression (OR, 5.0; 95% CI, 1.7–14.8; p = 0.002) as an independent risk factor. Patients weaned at Sanders Stage 7 (OR, 4.7; 95% CI, 2.1–10.7; p < 0.001), radius Grade 9 (OR, 3.9; 95% CI, 1.75–8.51; p = 0.001), and ulna Grade 7 (OR, 3.1; 95% CI, 1.27–7.38; p = 0.013) were more likely to experience curve progression. The earliest maturity indices with a reasonable protective association were Sanders Stage 8 (OR, 0.21; 95% CI, 0.09–0.48; p < 0.001), and radius Grade 10 (OR, 0.42; 95% CI, 0.19–0.97; p = 0.042) with ulna Grade 9 (no patients with curve progression).
Conclusion
Brace weaning indications using Risser staging are inadequate. Curve progression is expected in patients with large curves, irrespective of maturity status. Bone age measurement by either Sanders staging or the distal radius and ulna classification provides clearer guidelines for brace weaning, resulting in the least postweaning curve progression. Weaning in patients with Sanders Stage 8 and radius Grade 10/ulna Grade 9 provides the earliest and most protective timepoints for initiating brace weaning.
Level of Evidence
Level II, prognostic study.
Introduction
The most frequently used and evidence-based method to prevent curve progression in adolescent idiopathic scoliosis (AIS) is bracing [41]. Despite the benefits of bracing, prolonged and indiscriminate use in children has been shown to reduce spinal mobility, lead to poor body image and self-esteem, and worse self-perception of function, pain, appearance, and mental health [13, 14, 17, 29, 30, 37, 38]. Treatment for AIS should be considered successful only if good patient-perceived outcomes are achieved in addition to preventing curve progression [15, 16, 43]. Hence, it is important to reduce unnecessary brace wear by limiting its use to only the period in which there is a risk of curve progression.
The growth potential of a patient with AIS determines the risk of curve progression. The greatest risk occurs during the pubertal growth spurt [12], and multiple radiological parameters exist to predict this timepoint [6, 7, 10, 11, 19, 33, 34, 36]. However, the risk of progression still exists throughout the adolescent growth period until skeletal maturity. To standardize when brace wear should be initiated, the Scoliosis Research Society (SRS) has created treatment guidelines [32]. However, no such guidelines exist for when brace wear should be terminated because the onset of skeletal maturity determined by growth parameters is not well understood. Stopping brace treatment when growth stops prevents overuse [22, 23, 31]. One study suggested that brace weaning may be initiated in patients with a Risser Stage of 4, those who are 12 months postmenarche, and those with lack of growth in height [4]. Another study recommended weaning in patients with a Risser Stage ≥ 4, those who are more than 2 years postmenarche, and those with no growth between two visits of unknown duration [35]. However, both studies observed that some patients had curve progression beyond brace weaning, suggesting that these weaning criteria are imperfect. Therefore, we wished to investigate the risk of curve progression using various maturity parameters and to redefine brace-weaning criteria for patients with AIS, using standardized skeletal maturity parameters.
Specifically, we asked: (1) Is no change in height measurements over 6 months and Risser Stage 4 sufficient for initiating brace weaning? (2) What is the association between larger curves (45°) at brace weaning and the progression risk? (3) Are a more-advanced Risser stage, Sanders stage, or distal radius and ulna classification associated with a decreased risk of curve progression? (4) When should we wean patients with AIS off bracing to reduce the time for brace wear while limiting the risk of postweaning curve progression?
Patients and Methods
Study Design
This was a prospective study of all patients with AIS at our institution who underwent brace weaning during the period between June 2014 and February 2016. Patients were referred for brace weaning based on the following criteria: they were Risser Stage 4, had no growth in body height, sitting height, and arm span in the past 6 months of followup, and were at least 2 years postmenarche. The Risser staging is based on the ossification stages of the right iliac crest. Stage 0 indicates no ossification, Stage 1 indicates ossification of the anterior lateral quarter, Stage 2 indicates ossification of the anterolateral half, Stage 3 indicates ossification of the anterior three-quarters, Stage 4 indicates complete ossification, Stage 4+ indicates capped apophysis, and Stage 5 indicates complete fusion. We chose 6 months of followup and 2 years postmenarche as more stringent criteria for brace weaning. All patients were followed up for at least 2 years after they were weaned off their braces, with interval followup assessments every 6 months to identify any postweaning deterioration. None were lost to followup.
In our institution, all patients with AIS are administered a brace according to the following standardized brace referral criteria, as suggested by the SRS [32]: initial age between 10 and 14 years, major curve magnitude of 25° to 40°, less than 1 year postmenarche, Risser Stages 0 to 2, and no treatment history. The mean Cobb angle before brace treatment initiation was 32 ± 5°. All patients were prescribed an underarm (Boston) bracing.
For our recruited patients, all reported that they used their brace for more than 16 hours at the time of weaning, and they had regular recent visits to an orthotist for brace assessments. To maintain consistency of brace weaning for our recruited patients, our exclusion criteria were anyone who did not adhere to our brace weaning protocol, who had measured growth gain during the followup period after brace weaning, and those who were unable to complete the followup protocol. Braces were discarded on the day of brace weaning to avoid further use and to adhere to our study protocol. All 144 patients ready for brace weaning were recruited during this study period and no patients were lost to followup. All patients adhered to our study protocol. Hence, no patient was excluded from the study (Table 1). Our local institutional review board approved the study protocol.
Table 1.
Patient baseline demographics at date of brace weaning decision
Sample Size Calculation and Power Analysis
We used the guidelines based on the work of Hsieh et al. [21] to determine the a priori sample size calculation for logistic regression using G*Power (version 3.1.9.2; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany). Based on the proportion of minimal curve progression rate in large curves (16 of 144 patients = 0.11), a sample size of 126 is adequate to achieve α = 0.05 and power of 0.8. Post-hoc analysis was also performed and determined the power (0.82–0.96; α = 0.05) to be satisfactory for all produced ORs.
Outcome Measures
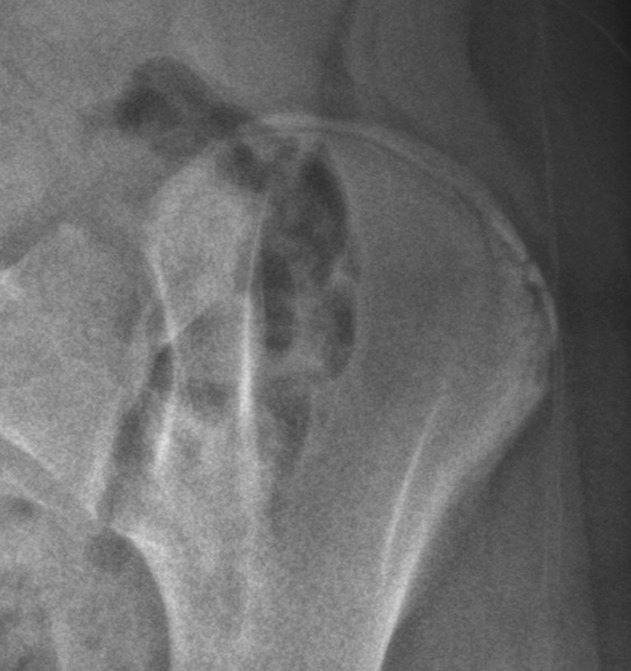
At baseline (the date of recruitment or brace weaning), we collected data on the following parameters: body height, sitting height and arm span measured in centimeters, magnitude of the major coronal Cobb angle, Lenke classification and location of major curve (thoracic or thoracolumbar/lumbar), timing of menarche, Risser stage [2], and bone age assessment via Sanders staging [34], as well as the distal radius and ulna classification [8, 9]. The Risser Stages (Fig. 1) were 4, 4+, and 5 based on the ossification of the iliac apophysis. Risser Stage 4+ was defined as capping of the apophysis and was included for further grade segregation. The Sanders Stages ranged from 1 to 8, and the distal radius and ulna classification was divided into radius Grades 1 to 11 and ulna Grades 1 to 9. Sanders staging is a simplified method to measure bone age by assessment of the epiphyseal-metaphyseal bone complexes of all digits in the hand and radius. The distal radius and ulna classification measures bone age by appearance of the distal radius and ulna physes. Both systems consider capping of the epiphysis (digits, radius, or ulna) to indicate the pubertal growth spurt and closing of the physeal plate to indicate skeletal maturity. However, each has a different set of grading specific to certain growth periods and hence one Sanders staging may coincide with multiple different radius or ulna grades. For example, a patient with Sanders 7 could also be classified as radius Grade 9 and ulna Grade 8 (Fig. 2) or as radius Grade 10 and ulna Grade 9 (Fig. 3). Standing whole-spine posteroanterior radiographs were obtained to measure the Cobb angles and Risser stages. For the baseline radiograph, all patients stopped using the brace for at least 24 hours beforehand to allow proper rebound to the real Cobb angle. In the same setting, a radiograph of the left hand and wrist was obtained to assess the bone age. Subsequently, at all other followup timepoints, height, arm span, and the Cobb angle were also measured. A designated clinic nurse who usually performs these tasks at our scoliosis clinic obtained all height and arm span measurements. These measurements were necessary to prove there was no further growth, and any patient with further growth was excluded from the study. All radiographic measurements were performed by spine surgeons independently as part of their routine consultations, without knowledge of this study.
Fig. 1.
This radiograph demonstrates the appearance of Risser Stage 4, which is identified as ossification of the whole length of the iliac apophysis that is not yet fused to the ilium.
Fig. 2.

This radiograph shows Sanders Stage 7 with closure of all digital physes except for the distal radius and ulna. On this same radiograph, the distal radius and ulna classification is considered radius Grade 9 (narrowing of the whole physeal plate without fusion) and ulna Grade 8 (fusion of > 50% of the medial ulna physis).
Fig. 3.

On this hand and wrist radiograph, the Sanders stage is still 7 because the distal radius physis is white; however, for the distal radius and ulna classification, the radius grade is 10 (fused physis but scar still seen) while the ulna grade is 9 (complete fusion of the physeal plate).
Statistical Analysis
Descriptive statistics for measurements are presented as the mean ± SD. Curve progression was determined as any > 5° increase in the Cobb angle between two measurements during the subsequent followup visits. Statistical analyses included an intergroup comparison of patients with curve progression and those without, for which we used an independent samples t-test and nonparametric Mann-Whitney U test for age, curve type and the Cobb angle at the time patients were weaned off their braces. We set the cutoff angle for larger curves as ≥ 45° [40, 42], as measured at the time of weaning, and we specifically assessed larger curves as a risk factor for progression, in addition to maturity grading.
We performed a chi-square test of independence [27] to test for any association between curve progression and sex, and curve magnitude (< 45° or ≥ 45°) as well as each skeletal maturity index. The relationship of curve magnitude at weaning and curve progression was tested using point-biserial correlation test. Based on these results from the bivariate analyses, in which any parameters having associations (p < 0.2) [18] with curve progression were identified, these parameters were then included in a subsequent regression analyses.
A binomial logistic regression analysis was performed to determine the associations of these parameters on the likelihood of curve progression. ORs per maturity index grading system were used to predict the risk of postweaning curve progression, given that statistically significant regression models were established. We performed step-wise logistic regression analyses to assess the individual relationships of associated factors on curve progression, before examining these factors together as covariates. Covariates used for the multivariate model included a large curve magnitude at brace weaning and sex. Within each individual maturity index, we assessed the relative risk (RR) for various grades or stages. In addition, Cobb angle as a continuous variable was also used for multivariate analyses with covariates of each skeletal maturity grade and sex. Relationships between the various maturity indices were mapped to show the interactions with regards to curve progression rate (Fig. 4). Because Sanders stage 8 was the highest grade in the classification system, we used it to illustrate the change in the risk of curve progression from radius Grades 10 and 11, and from ulna Grades 7 to 9. Statistical significance was set at p < 0.05, and 95% confidence intervals (CIs) are reported. Data analyses were conducted using SPSS Windows 23.0 (IBM SPSS Inc, Chicago, IL, USA).
Fig. 4.

We mapped the curve progression rate for Risser staging, Sanders staging and the distal radius and ulna classification. The arrows indicate the direction in decreasing curve progression rate with advancements in skeletal maturity. The curve progression rate was 0% in those with radius Grade 10/ulna Grade 7 and ulna Grade 9, Radius Grade 10/ulna Grade 8 in those with Risser Stage 5, and at radius Grade 11.
Results
Up to 29% (42 of 144) of patients still experienced curve progression after brace weaning despite being ≥ 2 years postmenarche for girls, Risser stage 4, and having no height or arm span gain for the previous 6 months. Most patients who were weaned had a Risser stage of 4+ (82 of 144 [57%]), followed by those with radius Grade 9 or 10 (123 of 144 [85%]), those with ulna Grade 8 (92 of 144 [64%]), and those with Sanders Stage 8 (79 of 144 [55%]). The mean degree of curve progression after weaning was 8.3 ± 3.0°. No association was identified between curve type and curve progression (p = 0.094).
Larger curve magnitudes (≥ 45°) at the time of brace weaning were associated with a greater risk of further >5° of curve progression (OR, 5.0; 95% CI, 1.7–14.8; p = 0.002). Among the patients with large curves (those ≥ 45° at the time of brace weaning), 10 of 16 (63%) experienced curve progression (Table 2).We observed a difference in Cobb angle between those who experienced curve progression and those who did not (37.4° versus 34.7°, p = 0.047) (Table 3). Specifically testing curve magnitude in relation to curve progression, we found that the correlation coefficient was 0.166 (p = 0.047). Patients with lower maturity index grades (Sanders Stage 7, radius Grade 9, and ulna Grade 7) who experienced curve progression had larger Cobb angles than did their counterparts without curve progression. We observed no differences for the Risser stages. The overall change in Cobb angle for these 16 patients with large curves was 6.3 ± 3.5°. For their outcomes, 7 of 16 (44%) were still under observation, and 9 of 16 (56%) were offered surgery.
Table 2.
Comparison of curve magnitude at brace weaning for each skeletal maturity index
Table 3.
Comparison of curve progression and no curve progression patients
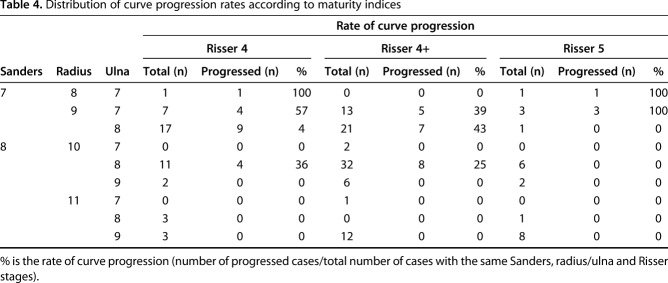
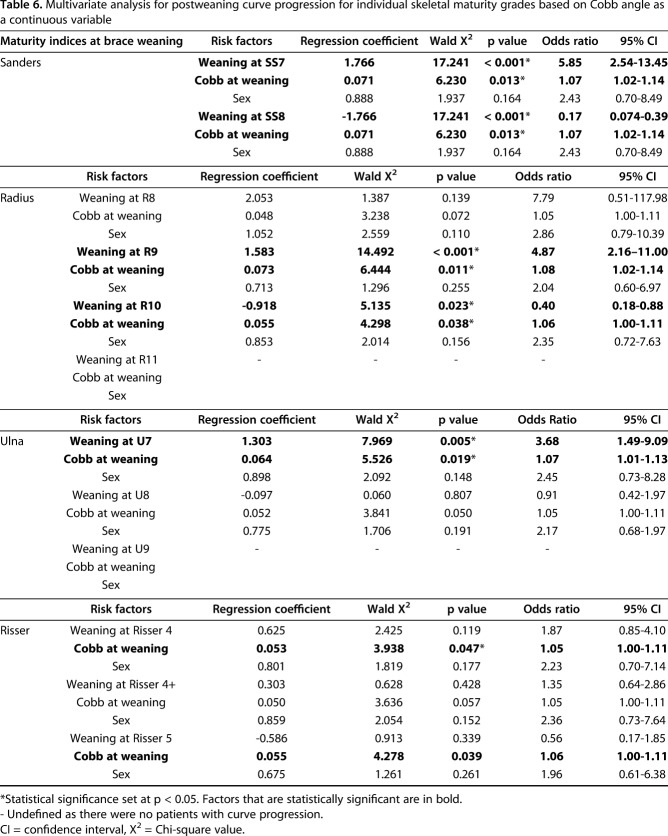
Curve progression proportions were lower for patients in the advanced stages of maturity including Risser Stage 5, Sanders Stage 8, radius Grade 11 and ulna Grade 9 (Table 4). However, we still observed curve progression in patients with Risser Stage 5. Hence, no statistically significant model could be generated for Risser staging. For patients weaned at earlier stages, Sanders stage 7 (OR, 4.7; 95% CI, 2.1–10.7; p < 0.001), radius Grade 9 (OR, 3.9; 95% CI, 1.75–8.51; p = 0.001), and ulna Grade 7 (OR, 3.1; 95% CI, 1.27–7.38; p = 0.013) were more likely to experience curve progression (Table 5). Using Cobb angle as a continuous variable, we observed similar findings with reduced ORs with advancing maturity grades (Table 6). Regarding Sanders staging, 30 of 65 (46%) experienced curve progression with stage 7 at the time of weaning while only 12 of 79 (15%) patients with Stage 8 experienced curve progression. In an independent observation of the distal radius and ulna classification, 28 of 62 (45%) patients weaned at radius Grade 9 and 14 of 29 (48%) patients weaned at ulna Grade 7 had curve progression. The progression rate decreased to 12 of 61 (20%) for radius Grade 10 and 28 of 92 (30%) for ulna Grade 8. For the interactions between different maturity parameters, any of the Sanders Stages (7 and 8) and distal radius and ulna classification (radius Grades 8 to 11 and ulna Grades 7 to 9) grades coexisted with Risser stage 4, 4+, and 5. No radius Grade 10 or 11, or ulna Grade 9 were observed in those with Sanders Stage 7 (Table 4) and hence were used to further segregate Sanders Stage 8 into different stages (Fig. 4).
Table 4.
Distribution of curve progression rates according to maturity indices
Table 5.
Adjusted odds ratio for postweaning curve progression for individual skeletal maturity grades
Table 6.
Multivariate analysis for postweaning curve progression for individual skeletal maturity grades based on Cobb angle as a continuous variable
Brace wear weaning at Sanders Stage 8 (OR, 0.21; 95% CI, 0.09–0.48), and radius Grade 10 (OR, 0.42; 95% CI, 0.19–0.97) and ulna Grade 9 (no patients with curve progression) provided the most protective association for any further curve progression (Table 5). Ulna Grade 8 had a borderline protective association, with an OR of 1.07 (p > 0.05). Based on the adjusted RR between individual maturity stages (Table 7), brace weaning at Sanders Stage 7 was associated with (OR: 4.73; 95% CI, 2.09–10.72; p < 0.001) curve progression compared with Stage 8. Brace weaning at radius Grade 9 was associated with (OR, 3.29; 95% CI, 1.43–7.59; p = 0.005) curve progression compared with Grade 10. Radius Grade 10 was the earliest grade at which we observed a 0% progression rate when combined with either Risser Stage 4 and ulna Grade 9 or with Risser Stage 4+ and ulna Grade 7. No patients experienced curve progression when weaned at radius Grade 10 and ulna Grade 9 or at radius Grade 11.
Table 7.
Relative risk and adjusted relative risk for skeletal maturity grades
Discussion
Although bracing has proven benefits for preventing curve progression in AIS, it should not be used indiscriminately because prolonged brace treatment may lead to spinal stiffness and poor self-esteem and self-perceived body image [13, 37, 38]. Bracing should be weaned as close to growth cessation as possible to reduce the risk of curve progression and that of prolonged brace treatment. Our ability to correctly determine skeletal maturity is crucial for accomplishing this. The traditional guidelines for brace weaning—Risser Stage 4, no height gain within 6 months of followup, and being at least 2 years postmenarche for girls—are inadequate as our study suggests that nearly one-third of patients still experience curve progression after brace weaning. Although curve progression is expected in patients with large curves irrespective of maturity status, bone age assessment with either the Sanders staging or the distal radius and ulna classification provides clearer indicators for when braces should be weaned. Weaning at Sanders Stage 8 and radius Grade 10/ulna Grade 9 results in the least amount of curve progression after weaning.
A main limitation of this study is the uneven distribution of grades in each classification system. Some grade combinations, such as Risser Stage 5, Sanders Stage 8, radius Grade 10, and ulna Grade 7 lack data for comparison. Although this factor limits the extent of comparative data, it also reveals the intimate relationship among the studied maturity parameters. Another limitation is the lack of information on the apical rotation of the curves and flexibility. These may both influence the risk of further curve progression. Although we applied a standardized protocol of bracing, assessments, and weaning criteria, there were variations in the timing of bracing and its association with changing curve behavior. The degree of vertebral wedging and rotation may also influence the risk of future curve progression and should be addressed in a further study. The use of 2-year followup in this study may not necessarily indicate skeletal maturity. Nevertheless, as there was no further height gain observed, it is likely that no further spine growth occurred. Furthermore, patients’ bracing compliance before weaning was self-reported, and there may be concerns regarding its accuracy. This may affect the influence of stated maturity parameters in predicting further curve progression. The time of brace wear may also be important because it may affect changes in curve flexibility. A stiffer spine may be less susceptible to curve progression. Whether the brace may have improved the curve magnitude and hence changed the natural history of disease is also unknown.
The current brace-weaning approaches (no height gain measurements, 2 years postmenarche, and Risser Stage 4) are flawed because the curve progression rate in this study was still substantial (42 of 144 [29%]). Height measurements only reflect previous growth rates and are not useful for predicting future growth. Body height and arm span are frequently used to indicate growth, but neither truly represents spine growth. A previous study has identified mismatches between growth rates and curve progression rates, suggesting that body height changes do not fully reflect spine growth [11]. Sitting height eliminates the lower limb component, but it still does not directly represent spine growth. It is also easily affected by changes in curve magnitude. Although we used body height, sitting height, and arm span measurements as stringent criteria for study inclusion, curve progression still occurred. Similarly, the use of menarche as a criterion is also flawed. It is markedly variable at onset, and delayed menarche is not uncommon [5]. Risser staging is also inadequate to determine brace weaning because 75.2% of children continue to grow, despite apophyseal capping [20]. Some studies also suggested that the iliac apophysis may not fuse until adulthood, which limits the ability of Risser Stage 4 to represent remaining growth potential [24, 25, 39]. There is also evidence that children reach skeletal maturity earlier than past generations [3]. In essence, accurate bone age assessment is far more crucial for maturity assessment, and there is a greater need to rely on these radiological tools as compared with chronological age for initiating skeletal growth driven interventions.
We found that large curves (≥ 45°) was an independent factor associated with curve progression after brace weaning. Specifically identifying the 45° cutoff appears to amplify this relationship as 63% of patients with curves ≥ 45° at the time of brace weaning had further progression, compared with only 25% of patients with curves < 45°. It is important to note, however, that the difference in Cobb angle between patients with curve progression and those who did not was only minimal (37.4° vs 34.7°). Since all patients in this study were compared for this intergroup difference, it would have included patients of varying maturity status. The correlation between curve magnitude and curve progression was also small (rpb = 0.166), which highlights this discrepancy. Nevertheless, it appears that the natural history or disease process dictates whether a curve continues to progress despite patients reaching skeletal maturity [40, 41] as curve progression is evident even in patients weaned at later maturity stages (Risser Stage 5 and Sanders Stage 8). Hence, it was crucial to control for this covariate in the risk analysis. This also tends to confirm the findings suggested by Weinstein et al. [40, 42] regarding large curves of ≥ 45°. These findings further emphasizes the necessity for encouraging good brace compliance and early interventions. Aulisa et al. [1] has shown that long-term results of patients with 30° at the time of brace weaning do not deteriorate. Patients who do reach the threshold of 45° at the time of brace weaning should be warned of their poor prognosis to better manage expectations. This group of patients should be further studied to determine which curve type is at-risk of further deterioration and may ultimately require surgical intervention.
Our analysis found that assessments of bone age with both Sanders staging and the distal radius and ulna classification provide better parameters for initiating brace weaning than Risser staging. Although Risser Stage 5 had an apparent protective association (OR, 0.68) at the time of brace weaning, there was still a 20% curve progression rate, and there were no differences between Risser Stage 5 and Stages 4 and 4+. Our findings are already some of the lowest curve progression rates reported with Risser staging based indications for brace weaning [1, 26, 35, 44]. Additonally, the timing of Risser Stage 5 does not appear to coincide chronologically compared with Sanders staging and distal radius and ulna classification. Such deviances have been identified before [28]. Any of the Sanders stages and radius and ulna grades may coexist with Risser Stages 4, 4+, or 5. There is no clear distinction or linear relationship between risk and protection for Risser staging. Capping of the apophysis (Risser Stage 4+) was added as an intervening stage between Risser Stages 4 and 5 to further segregate the growth stages and provide a more precise classification. However, this did not lead to a gradual reduction of the curve progression risk. Our testing reveals that the Risser staging system has a lack of consistency and accuracy, thus limiting its use for guiding brace weaning. As reported by Shi et al. [35], nearly 50% of patients experienced curve progression after brace weaning using Risser staging as the weaning indicator.
Based on our findings, we recommend using Sanders Stage 8, radius Grade 10, and ulna Grade 9 as indicators for initiating brace weaning. There is a clear distinction in the ORs for further curve progression between these and earlier stages. Although weaning should not be performed at Sanders Stage 7, curve progression was still observed in 15% of patients weaned at Stage 8. Alternatively, if patients continued to use a brace beyond Stage 8 to avoid this progression risk, there were no further grades for clinicians to monitor later maturity. In our study, 85% of patients without curve progression may have used a brace for longer than necessary. Because Sanders Stage 8 is the final stage of the classification system, its use is limited if the objective is to define the most precise guideline and wean patients as early as possible without the further risk of curve progression. Nevertheless, Sanders Stage 8 was shown to be protective, and the curve progression rate was relatively low. One of the main differences between the Sanders staging and the distal radius and ulna classification is the additional grade segregation during the growth cessation period. The distal radius and ulna classification has four radius Grades (8 to 11) and three ulna Grades (7 to 9) compared with only two Sanders stages. Hence, this may provide a finer scale for initiating brace weaning. Although no patients experienced further curve progression after achieving a radius Grade 11, it is unnecessary and not ideal to wean patients at the end grade because we aim to reduce the effective bracing time, and radius Grade 10 is already protective, with an OR of 0.42. The advantage of this system is using the ulna for the matched assessment, which helps reduce the progression risk further. Because of the limited number of patients with ulna Grade 7 within radius Grade 10, and because there was a residual progression risk in those with ulna Grade 8, it is not reliable to use these grades as indicators. There may always be some mismatch between radius and ulna grades; therefore, it is most appropriate to consider both radius Grade 10 and ulna Grade 9 as the earliest timepoint for initiating brace weaning with the least curve progression risk. Despite our recommendations, our results need to be validated in other study populations. Whether curve type, degree of disc wedging, apical rotation and flexibility of the spine before bracing influences the accuracy of prediction for these various maturity indices remain to be explored. It is also important to note that spinal growth and height gain may have mismatches and the relationship between curve progression and growth near skeletal maturity should also be addressed [11].
Based on our findings, our study has three main implications. First, conventional recommendations [4, 35] based on clinical parameters, postmenarche years, and Risser staging are inadequate for preventing curve progression in patients with AIS after brace weaning. Second, bone age measurements of the hand and wrist supercede Risser staging as the maturity parameter to define growth cessation and the point of brace weaning. Either Sanders Stage 8 or radius Grade 10/ulna Grade 9 (Fig. 3) can be used to provide better indications for terminating brace treatment compared with Risser staging. Both systems have a clear distinct grade where it becomes protective for any curve progression. Radius Grade 10/ulna Grade 9 has an additional advantage because it is not the end grade compared with Sanders Stage 8, which may provide an earlier and perhaps more precise timing for brace weaning. Finally, the association of large curves appears to be independent of maturity status, and patients should be warned of the risk of continued progression into adulthood with the risk of surgical intervention, even in patients in whom bracing was previously successful. Further long-term studies with other ethnic groups should be performed to validate our findings.
Acknowledgments
None.
Footnotes
The institution of one or more of the authors (JPYC) has received, during the study period, funding from the General Research Fund of the Research Grants Council #17156416.
Each author certifies that neither he or she, nor any member of his or her immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Aulisa AG, Guzzanti V, Falciglia F, Galli M, Pizzetti P, Aulisa L. Curve progression after long-term brace treatment in adolescent idiopathic scoliosis: comparative results between over and under 30 Cobb degrees - SOSORT 2017 award winner. Scoliosis Spinal Disord . 2017;12:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bitan FD, Veliskakis KP, Campbell BC. Differences in the Risser grading systems in the United States and France. Clin Orthop Relat Res . 2005:190-195. [DOI] [PubMed] [Google Scholar]
- 3.Boeyer ME, Sherwood RJ, Deroche CB, Duren DL. Early maturity as the new normal: A century-long study of bone age. Clin Orthop Relat Res . 2018;476:2112-2122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Canavese F, Kaelin A. Adolescent idiopathic scoliosis: Indications and efficacy of nonoperative treatment. Indian J Orthop . 2011;45:7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang SH, Tzeng SJ, Cheng JY, Chie WC. Height and weight change across menarche of schoolgirls with early menarche. Arch Pediatr Adolesc Med . 2000;154:880-884. [DOI] [PubMed] [Google Scholar]
- 6.Charles YP, Dimeglio A, Canavese F, Daures JP. Skeletal age assessment from the olecranon for idiopathic scoliosis at Risser grade 0. J Bone Joint Surg Am . 2007;89:2737-2744. [DOI] [PubMed] [Google Scholar]
- 7.Cheung JP, Cheung PW, Samartzis D, Cheung KM, Luk KD. The use of the distal radius and ulna classification for the prediction of growth: peak growth spurt and growth cessation. Bone Joint J . 2016;98:1689-1696. [DOI] [PubMed] [Google Scholar]
- 8.Cheung JP, Samartzis D, Cheung PW, Cheung KM, Luk KD. Reliability analysis of the distal radius and ulna classification for assessing skeletal maturity for patients with adolescent idiopathic scoliosis. Global Spine J . 2016;6:164-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheung JP, Samartzis D, Cheung PW, Leung KH, Cheung KM, Luk KD. The distal radius and ulna classification in assessing skeletal maturity: a simplified scheme and reliability analysis. J Pediatr Orthop B . 2015;24:546-551. [DOI] [PubMed] [Google Scholar]
- 10.Cheung JPY, Cheung PWH, Samartzis D, Luk KD. APSS-ASJ Best Clinical Research Award: Predictability of curve progression in adolescent idiopathic scoliosis using the distal radius and ulna classification. Asian Spine J . 2018;12:202-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheung JPY, Cheung PWH, Samartzis D, Luk KD. Curve progression in adolescent idiopathic scoliosis does not match skeletal growth. Clin Orthop Relat Res . 2018;476:429-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheung JPY, Luk KD. Managing the pediatric spine: growth assessment. Asian Spine J . 2017;11:804-816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheung KM, Cheng EY, Chan SC, Yeung KW, Luk KD. Outcome assessment of bracing in adolescent idiopathic scoliosis by the use of the SRS-22 questionnaire. Int Orthop . 2007;31:507-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheung PWH, Wong CKH, Cheung JPY. An insight into the health-related quality of life of adolescent idiopathic scoliosis patients undergoing bracing, observation, and previously braced. Spine (Phila Pa 1976) . [Published online ahead of print November 1, 2018]. DOI: 10.1097/BRS.0000000000002918. [DOI]
- 15.Cheung PWH, Wong CKH, Lau ST, Cheung JPY. Responsiveness of the EuroQoL 5-dimension (EQ-5D) in adolescent idiopathic scoliosis. Eur Spine J . 2018;27:278-285. [DOI] [PubMed] [Google Scholar]
- 16.Cheung PWH, Wong CKH, Samartzis D, Luk KDK, Lam CLK, Cheung KMC, Cheung JPY. Psychometric validation of the EuroQoL 5-Dimension 5-Level (EQ-5D-5L) in Chinese patients with adolescent idiopathic scoliosis. Scoliosis Spinal Disord . 2016;11:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Climent JM, Sanchez J. Impact of the type of brace on the quality of life of adolescents with spine deformities. Spine (Phila Pa 1976). 1999;24:1903-1908. [DOI] [PubMed] [Google Scholar]
- 18.Concato J, Feinstein AR, Holford TR. The risk of determining risk with multivariable models. Ann Intern Med . 1993;118:201-210. [DOI] [PubMed] [Google Scholar]
- 19.Dimeglio A, Charles YP, Daures JP, de Rosa V, Kabore B. Accuracy of the Sauvegrain method in determining skeletal age during puberty. J Bone Joint Surg Am . 2005;87:1689-1696. [DOI] [PubMed] [Google Scholar]
- 20.Hoppenfeld S, Lonner B, Murthy V, Gu Y. The rib epiphysis and other growth centers as indicators of the end of spinal growth. Spine (Phila Pa 1976) . 2004;29:47-50. [DOI] [PubMed] [Google Scholar]
- 21.Hsieh FY, Bloch DA, Larsen MD. A simple method of sample size calculation for linear and logistic regression. Stat Med . 1998;17:1623-1634. [DOI] [PubMed] [Google Scholar]
- 22.Katz DE, Durrani AA. Factors that influence outcome in bracing large curves in patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976) . 2001;26:2354-2361. [DOI] [PubMed] [Google Scholar]
- 23.Landauer F, Wimmer C, Behensky H. Estimating the final outcome of brace treatment for idiopathic thoracic scoliosis at 6-month follow-up. Pediatr Rehabil . 2003;6:201-207. [DOI] [PubMed] [Google Scholar]
- 24.Little DG, Song KM, Katz D, Herring JA. Relationship of peak height velocity to other maturity indicators in idiopathic scoliosis in girls. J Bone Joint Surg Am . 2000;82:685-693. [DOI] [PubMed] [Google Scholar]
- 25.Little DG, Sussman MD. The Risser sign: a critical analysis. J Pediatr Orthop . 1994;14:569-575. [DOI] [PubMed] [Google Scholar]
- 26.Maruyama T. Bracing adolescent idiopathic scoliosis: a systematic review of the literature of effective conservative treatment looking for end results 5 years after weaning. Disabil Rehabil . 2008;30:786-791. [DOI] [PubMed] [Google Scholar]
- 27.McHugh ML. The chi-square test of independence. Biochem Med (Zagreb). 2013;23:143-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Minkara A, Bainton N, Tanaka M, Kung J, DeAllie C, Khaleel A, Matsumoto H, Vitale M, Roye B. High risk of mismatch between Sanders and Risser staging in adolescent idiopathic scoliosis: Are we guiding treatment using the wrong classification? J Pediatr Orthop . [Published online ahead of print January 22, 2018]. DOI: 10.1097/BPO.0000000000001135. [DOI] [PubMed]
- 29.Noonan KJ, Dolan LA, Jacobson WC, Weinstein SL. Long-term psychosocial characteristics of patients treated for idiopathic scoliosis. J Pediatr Orthop . 1997;17:712-717. [PubMed] [Google Scholar]
- 30.Odermatt D, Mathieu PA, Beausejour M, Labelle H, Aubin CE. Electromyography of scoliotic patients treated with a brace. J Orthop Res . 2003;21:931-936. [DOI] [PubMed] [Google Scholar]
- 31.Rahman T, Bowen JR, Takemitsu M, Scott C. The association between brace compliance and outcome for patients with idiopathic scoliosis. J Pediatr Orthop . 2005;25:420-422. [DOI] [PubMed] [Google Scholar]
- 32.Rowe DE. The Scoliosis Research Society Brace Manual. Available at: http://www.srs.org/UserFiles/file/bracing-manual/section1.pdf. Accessed August 18, 2018.
- 33.Sanders JO, Browne RH, McConnell SJ, Margraf SA, Cooney TE, Finegold DN. Maturity assessment and curve progression in girls with idiopathic scoliosis. J Bone Joint Surg Am . 2007;89:64-73. [DOI] [PubMed] [Google Scholar]
- 34.Sanders JO, Khoury JG, Kishan S, Browne RH, Mooney JF, 3rd, Arnold KD, McConnell SJ, Bauman JA, Finegold DN. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am . 2008;90:540-553. [DOI] [PubMed] [Google Scholar]
- 35.Shi B, Guo J, Mao S, Wang Z, Yu FW, Lee KM, Ng BK, Zhu Z, Qiu Y, Cheng JC, Lam TP. Curve progression in adolescent idiopathic scoliosis with a minimum of 2 years' follow-up after completed brace weaning with reference to the SRS Standardized Criteria. Spine Deform . 2016;4:200-205. [DOI] [PubMed] [Google Scholar]
- 36.Sitoula P, Verma K, Holmes L, Jr., Gabos PG, Sanders JO, Yorgova P, Neiss G, Rogers K, Shah SA. Prediction of curve progression in idiopathic scoliosis: Validation of the Sanders Skeletal Maturity Staging System. Spine (Phila Pa 1976). 2015;40:1006-1013. [DOI] [PubMed] [Google Scholar]
- 37.Ugwonali OF, Lomas G, Choe JC, Hyman JE, Lee FY, Vitale MG, Roye DP., Jr Effect of bracing on the quality of life of adolescents with idiopathic scoliosis. Spine J . 2004;4:254-260. [DOI] [PubMed] [Google Scholar]
- 38.Vasiliadis E, Grivas TB, Savvidou O, Triantafyllopoulos G. The influence of brace on quality of life of adolescents with idiopathic scoliosis. Stud Health Technol Inform . 2006;123:352-356. [PubMed] [Google Scholar]
- 39.Wang WW, Xia CW, Zhu F, Zhu ZZ, Wang B, Wang SF, Yeung BH, Lee SK, Cheng JC, Qiu Y. Correlation of Risser sign, radiographs of hand and wrist with the histological grade of iliac crest apophysis in girls with adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2009;34:1849-1854. [DOI] [PubMed] [Google Scholar]
- 40.Weinstein SL, Dolan LA, Spratt KF, Peterson KK, Spoonamore MJ, Ponseti IV. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA . 2003;289:559-567. [DOI] [PubMed] [Google Scholar]
- 41.Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med . 2013;369:1512-1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am . 1983;65:447-455. [PubMed] [Google Scholar]
- 43.Wong CKH, Cheung PWH, Samartzis D, Luk KD, Cheung KMC, Lam CLK, Cheung JPY. Mapping the SRS-22r questionnaire onto the EQ-5D-5L utility score in patients with adolescent idiopathic scoliosis. PLoS One . 2017;12:e0175847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ylikoski M. Growth and progression of adolescent idiopathic scoliosis in girls. J Pediatr Orthop B . 2005;14:320-324. [DOI] [PubMed] [Google Scholar]