Abstract
Background
In contrast to best practice guidelines for knee osteoarthritis (OA), findings from several different healthcare settings have identified that nonsurgical treatments are underused and TKA is overused. Empirical evidence and qualitative observations suggest that patients’ willingness to accept nonsurgical interventions for knee OA is low. A qualitative investigation of why patients may feel that such interventions are of little value may be an important step toward increasing their use in the treatment of knee OA
Questions/purposes
This qualitative study was embedded in a larger study investigating patient-related factors (beliefs/attitudes toward knee OA and its treatment) and health-system related factors (access, referral pathways) known to influence patients’ decisions to seek medical care. In this paper we focus on the patient-related factors with the aim of exploring why patients may feel that nonsurgical interventions are of little value in the treatment of knee OA.
Methods
A cross-sectional qualitative study was conducted in a single tertiary hospital in Australia. Patients with endstage knee OA on the waiting list for TKA were approached during their preadmission appointment and invited to participate in one-to-one interviews. As prescribed by the qualitative approach, data collection and data analysis were performed in parallel and recruitment continued until the authors agreed that the themes identified would not change through interviews with subsequent participants, at which point, recruitment stopped. Thirty-seven patients were approached and 27 participated. Participants were 48% female; mean age was 67 years. Participants’ beliefs about knee OA and its treatment were identified in the interview transcripts. Beliefs were grouped into five belief dimensions: identity beliefs (what knee OA is), causal beliefs (what causes knee OA), consequence beliefs (what the consequences of knee OA are), timeline beliefs (how long knee OA lasts) and treatment beliefs (how knee OA can be controlled).
Results
All participants believed that their knee OA was “bone on bone” (identity beliefs) and most (> 14 participants) believed it was caused by “wear and tear” (causal beliefs). Most (> 14 participants) believed that loading the knee could further damage their “vulnerable” joint (consequence beliefs) and all believed that their pain would deteriorate over time (timeline beliefs). Many (>20 participants) believed that physiotherapy and exercise interventions would increase pain and could not replace lost knee cartilage. They preferred experimental and surgical treatments which they believed would replace lost cartilage and cure their knee pain (treatment beliefs).
Conclusions
Common misconceptions about knee OA appear to influence patients’ acceptance of nonsurgical, evidence-based treatments such as exercise and weight loss. Once the participants in this study had been “diagnosed” with “bone-on-bone” changes, many disregarded exercise-based interventions which they believed would damage their joint, in favor of alternative and experimental treatments, which they believed would regenerate lost knee cartilage. Future research involving larger, more representative samples are needed to understand how widespread these beliefs are and if/how they influence treatment decisions. In the meantime, clinicians seeking to encourage acceptance of nonsurgical interventions may consider exploring and targeting misconceptions that patients hold about the identity, causes, consequences, timeline, and treatment of knee OA.
Level of Evidence
Level II, prognostic study.
Introduction
Evidence-based nonsurgical interventions such as weight loss and exercise can reduce pain and disability associated with knee osteoarthritis (OA) [10, 25, 27]. Best-practice guidelines recommend that such interventions should be underpinned by behavior changes, in addition to nonopioid medications [15, 28]. Surgeons offer TKA in appropriately selected patients when nonsurgical interventions no longer alleviate the pain and functional limitations of endstage knee OA. Engaging in a nonsurgical intervention can delay or even avoid the need for surgery in most patients with moderate-to-severe knee OA [24]. However, studies from several countries have documented care that is inconsistent with best-practice guidelines [13, 16]. In an Australian community setting, 50% of people with knee OA had never participated in an exercise intervention, and 38% had never attempted weight loss, despite being overweight [14]. In the Australian primary care setting, general practitioners are more likely to refer patients with knee OA for surgical opinion (12% of the time), than to a nonsurgical intervention (< 4% of the time) [3]. A qualitative study among Australian general practitioners identified patient beliefs and expectations as key barriers to referral for nonsurgical intervention [9]. Referral to surgery for those who may need nonsurgical intervention first, places a burden on orthopaedic services, increasing surgical and outpatient waiting list times. Among patients on the orthopaedic waiting list at a metropolitan, tertiary-level public hospital in Australia, 39% had not previously engaged in nonpharmacological, nonsurgical intervention [12]. It is possible that some patients in Australia do not present to primary care until they have endstage knee OA and have severe disability from pain or dysfunction that necessitates TKA. It is also possible that some patients are unwilling to participate in a nonsurgical intervention.
To understand why some patients with knee OA may be unwilling to participate in a nonsurgical intervention, a qualitative approach is warranted. In contrast to quantitative research which focuses on estimates of prevalence and strength of associations between variables to test a priori hypotheses, qualitative research focuses on “why” and “how” questions without prior assumptions about the answers to these questions. Qualitative research seeks to generate hypotheses about a phenomenon through an in-depth understanding of the perspectives of a small number of individuals who are experiencing the phenomenon. These hypotheses can be tested later through quantitative approaches involving larger, more generalizable samples.
The aim of this qualitative study was to investigate the patient-related cognitive factors (beliefs/attitudes toward knee OA and its treatment) and health system-related factors (access, referral pathways) known to influence treatment decisions. In this paper we focus on the patient-related factors with the aim of exploring why patients may feel that nonsurgical interventions are of little value in the treatment of knee OA.
Patients and Methods
Study Design and Setting
This qualitative study was performed in the orthopaedic clinic of a large tertiary hospital in a metropolitan region of Australia. The clinic performs a high volume of TKA and receives statewide referrals.
Participants
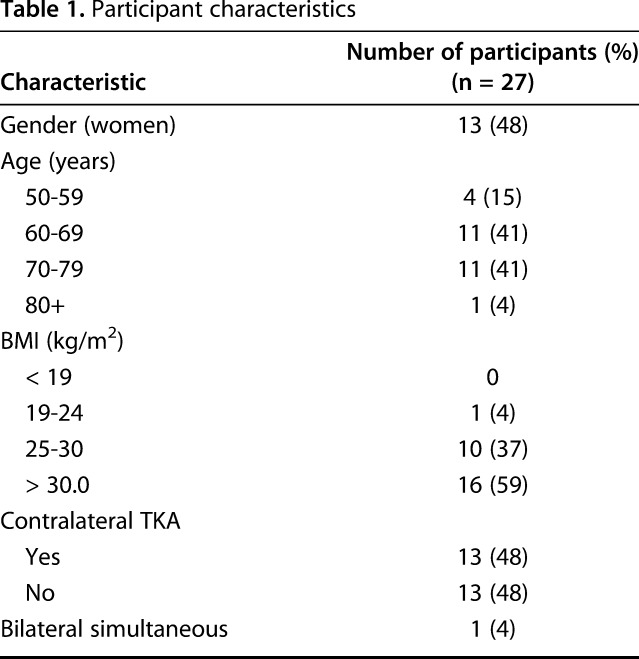
Patients on the waiting list for TKA attending the orthopaedic preadmission clinic were approached to participate. We recruited people with endstage knee OA on the waiting list for TKA because we expected these individuals to have a range of experiences to draw from and to be able to reflect on how their beliefs/attitudes had changed over time. Although we expected most of these individuals to have engaged in nonsurgical interventions before being on the waiting list, this also presented an opportunity to understand if and why some patients may be approaching the point of surgery without having previously engaged in nonsurgical interventions. A research assistant (POB) approached the patients and provided a verbal explanation of the study in addition to a study information sheet. Patients were eligible for inclusion if they were older than 18 years, spoke English, had a diagnosis of knee OA, and had consented to undergo primary TKA. Patients were ineligible if they needed an interpreter or were unable to provide independent informed consent for TKA because of cognitive impairment. Patients had no previous relationship with the research team; the researchers were not involved in patient care at this clinic. Between March and September 2018, 37 patients met our inclusion criteria and were approached to participate. Of those, four patients declined participation at the time of recruitment, two because of work commitments and two for unknown reasons. After agreeing to participate, four patients declined when called for the interview due to complex health conditions or changing their minds and deciding not to participate, and a further two were unable to be contacted. Twenty-seven patients agreed to participate and completed the interviews. The sample comprised of 48% women with a mean age of 68 years, a mean BMI of 33 kg/m2, and 48% had undergone a previous TKA (Table 1). Consistent with the qualitative approach, recruitment and data analysis were performed in parallel. This enabled us to identify patterns in the data and to stop recruiting when the research team were satisfied that these patterns would not change through interviews with subsequent participants (see data analysis for detail on how patterns were identified).
Table 1.
Participant characteristics
Data Collection
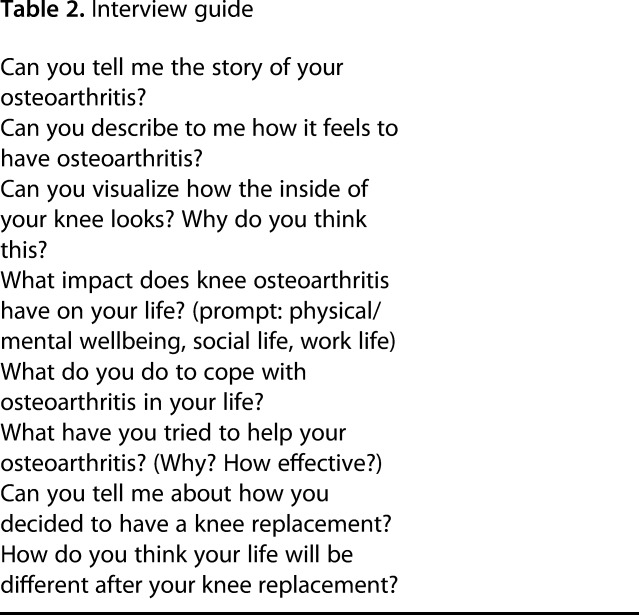
Individuals who provided informed consent were invited to participate in an interview at a time convenient to them. They were offered the option of a face-to-face interview at the orthopaedic clinic or a phone interview to accommodate any mobility issues. Seven face-to-face interviews and 20 phone interviews were conducted. We observed no differences in the length or quality of interviews between face-to-face and phone interviews. Interviews were conducted by one of two qualitative researchers (POB, a research assistant and SB, a postdoctoral researcher). Both have extensive experience in conducting face-to-face and phone interviews for qualitative health research. An interview guide explored patient-related cognitive factors (beliefs/attitudes towards knee OA and its treatment) and health-system related factors (access, referral pathways) shown in the evidence to influence patients’ treatment decisions [8] (Table 2). Interviews lasted 30 minutes on average. They were audio recorded and transcribed before analysis.
Table 2.
Interview guide
Data Analysis
Data were analyzed following a Framework Approach [23], which involves five steps. In step 1, two authors (POB, SB) independently became familiar with transcripts. In step 2, they independently coded all interview data related to patient-related factors. Coded data were uploaded into NVivo 10 (QSR International, Melbourne, Australia) to facilitate further analysis. In step 3, we developed a coding framework comprising five belief dimensions: (1) Identity Participants’ understanding of what knee OA is and pathoanatomical changes to their knee; (2) Cause: Beliefs about the cause of their knee OA; (3) Consequences: Beliefs about the consequences of knee OA; (4) Timeline: Beliefs about the trajectory of knee OA; (5) Treatment beliefs: Beliefs about treatments for knee OA, including experiences of treatment, their perceived effectiveness, and expectations for TKA. This coding framework was informed by a widely validated health belief theory, the Common Sense Model, which describes how people draw on these five belief dimensions to evaluate symptoms that represent a threat to health and decide what to do about them [17]. One author (SB) applied this coding framework to all transcripts. In step 4, coded data were charted on a matrix with belief dimensions as row headings and participant identifiers as column headings to facilitate the identification of patterns [23]. In step 5, we searched for relationships between the belief dimensions for each participant and for patterns in the belief dimensions and relationships between participants. As is inherent to the qualitative approach, the identification of patterns was a subjective process that involved group discussion among the multidisciplinary research team. The resulting patterns were described as themes.
In the results, these themes are presented for each belief dimension, supported by quotes indexed by the participant identification number, gender, and age; for example, Participant 2, man, 79 years old; Participant 9, woman, 60 years old. Consistent with our qualitative approach, our aim was not to quantify the responses. However, to provide readers with an indication of the frequency of endorsement of each theme we have used the terms “all”; “many” (> 20 participants); “most” (> 14 participants); “some” (7-14 participants); “a few” (< 7 participants). At the same time, we emphasize that the absence of a belief in a transcript is not the same as a lack of endorsement.
Results
Belief Dimension: Identity Beliefs
The main theme identified under identity beliefs was “Knee OA is bone on bone.” When asked about their knee OA, all participants described their knee as “bone on bone”: “It’s bone on bone, the cartilage is gone in it,” Participant 10, man, 70 years old. According to all participants, rubbing of the two bone surfaces was the source of their knee pain: “The two bones of my knee are rubbing each other the wrong way,” Participant 11, woman, 60 years old. One participant attributed a sharp increase in knee pain severity to the moment his knee joint became bone on bone: “One day I was walking good, the next day bang … the bone was catching on bone. You can feel it actually grinding,” Participant 19, man, 65 years old. Indeed, some participants attributed the sensations and sounds in their knee to bone on bone: “It clicks every now and then so I’m thinking something is rubbing on something,” Participant 5, woman, 77 years old. When asked how they visualized their knee, participants commonly used metaphors such as “raw bone” Participant 6, woman, 55 years old; “an empty shell” Participant 20, woman, 80 years old; and “two bald bones,” Participant 21, woman, 52 years old. When asked why she visualized her knee as two bald bones, Participant 21 responded: “They’ve shown me the pictures of the inside of my knees, it is literally just two round circles—balls—with nothing on them.”
Belief Dimension: Causal Beliefs
The main theme identified under causal beliefs was “OA is due to excessive loading through the knee.” Although knee OA was perceived by many to be a normal part of aging: “I’m in my 60s, you’re supposed to be worn out,” Participant 3, man, 63 years old, “most participants believed that their previously active lifestyles had caused wear and tear that had led to knee OA: “I always did a lot of gardening and dancing in my youth, maybe some of that contributed as well,” Participant 12, woman, 75 years old. Men commonly attributed wear and tear to a life of hard physical work: “Look, it’s wear and tear ... I expected this, I’m a hard worker,” Participant 15, man, 79 years old; “I knew I was going to get it because every second person that works in the yard has got arthritis because of the way we work,” Participant 16, man, 69 years old. Participant 21 (woman, 52 years old) had had a workplace injury on her left knee and believed that “compensating” for this injury had led to wear and tear in the right knee. She said: “I was constantly carrying weight on that side, to compensate for the other leg. So now it seems to have deteriorated, it’s just shot.” Increased load through the knee was commonly cited as a cause of wear and tear: “I used to have a fruit shop and jump up and down off the tray truck, I don’t reckon that did any good. That probably started the arthritis at that stage,” Participant 4, man, 77 years old. Carrying excess body weight was also cited as a reason for wear and tear in the knee: “Putting on weight doesn’t help your knees. Because you’ve got to carry it around,” Participant 10, man, 70 years old.
Belief Dimension: Consequence Beliefs
The main theme under consequence beliefs was “Fear of falling and damaging the joint.” Most participants described a lack of confidence in their knee. Some felt that their knee went “out of place” during turning movements such as getting in and out of cars: “Sometimes if I turn, you’ll hear this big crack. And then it’s as if it comes out of its socket, I don’t know if it pops out but there’s a loud cracking sound,” Participant 6, woman, 55 years old. Many participants felt as if their knee could “give way” on them: “I’m scared it’s going to give way,” Participant 9, woman, 60 years old. Several participants had fallen: “Just when you try to walk, boom, it gives up on you and you fall,” Participant 15, man, 79 years old. Some participants feared that falling would further harm their “vulnerable” joint, which had no cartilage to protect it, and therefore adopted behavior that reduced “stress” on the knee: “I’m very careful about the way I put my leg, so it doesn’t go out of place,” Participant 17, woman, 66 years; “I know I can balance well [with a walker] because I am worried about doing more harm if I fell,” Participant 12, woman, 75 years old.
Belief Dimension: Timeline Beliefs
Three themes were identified under timeline beliefs: “OA as a downward trajectory,” “The urgency to do something,” and “Arriving at the end of the road.” All participants perceived that their symptoms were worsening over time: “I can feel it getting worse. Just doing things, you can feel it clicking and it rubs against one another,” Participant 18, woman, 72 years old. All participants believed that knee OA was a downward trajectory and that bone loss over time was inevitable: “If I keep going the way I am going, it’s just going to get worse. It will just rub, rub away,” Participant 2, man, 79 years old. Often this belief was reinforced by health professionals: “When he looked at the x-rays, he showed me the left-hand side is just bone on bone, there’s nothing there. He said it’s not going to get any better, as a matter of fact it’s going to get worse,” Participant 8, man, 70 years old. A sense of urgency was noted in the participants’ narratives, a sense that they needed to do something before it was “too late”: “The physiotherapist said, ‘You’ve got to see your GP. Get a referral before it’s too late,’” Participant 5, woman, 77 years old. Many described having arrived at the end of the road, believing their knee was “past its expiry date”: “The knee has already past its used-by date, so it has to have something to replace it,” Participant 11, woman, 60 years old. For a few, the used-by date had been reached before they sought care (see further elaboration in theme “Exercise interventions” below).
Belief Dimension: Treatment Beliefs
Four themes were identified under treatment beliefs: “The weight loss dilemma,” “Physiotherapy can’t help bone on bone,” “Replacing the cartilage,” and “A mechanical problem requires a mechanical fix.” While many participants articulated that weight loss would help their knee pain by reducing load through the joint, they perceived that their ability to lose weight was limited. Participant 3 (man, 63 years old) described a vicious cycle in which knee pain limited his ability to exercise, leading to weight gain, which in turn increased knee pain: “One of the worst parts about it is that if I was more active, I could lose a bit of weight and take weight off [the knee]. But you’re buggered because you can’t do something as simple as walk down the street.” Indeed, only a few participants reported taking active measures to reduce their weight. Among these, a key motivation for losing weight was to “preempt” advice from the surgeon and present as better candidates for surgery: “I knew that when I went to see the surgeon he’d probably say, ‘lose a bit of weight’ so I was trying to preempt that,” Participant 23, man, 59 years old.
Similarly, only a few participants were currently engaging in an exercise intervention, the most common being hydrotherapy. Participant 10 (man, 70 years old) believed hydrotherapy was better than land-based exercises, which increased loading through his “nonexistent” knee: “I found the physiotherapy exercises where they get you to put pressure on your leg were difficult … I found [hydrotherapy] a lot better than putting pressure on the joint when there was no real joint there.” Many had engaged in physiotherapy in the earlier phases of their knee OA but had stopped when they learned their knee joint was bone on bone: “I’ve tried physio over the years … but they’re not able to help bone on bone when it gets to that stage,” Participant 9, woman, 60 years old. A few participants reported that their knee was already bone on bone by the time they sought care: “If I had seen the specialist early, then they could probably do an alternative treatment. But instead of going to the doctor, I thought oh well, it’s arthritis it doesn’t matter. Until I couldn’t bear the pain anymore, and then I went and found out it was too late,” Participant 25, man, 64 years old. As a result, these participants did not engage in any physiotherapy or exercise because they believed these interventions could not replace the cartilage: “I haven’t got the cartilage there, so [the physiotherapy] can’t do much about that … They can’t replace my cartilage: I’ve got to put the cushion back into my knee,” Participant 17, woman, 66 years old.
Most participants had taken dietary supplements, which they had heard could promote cartilage growth: “I tried chondroitin, it’s from fish. They tell you that it’s good to rebuild the cartilage of your knees,” Participant 13, man, 74 years old. Most participants had stopped taking dietary supplements after they did not observe any improvement: “The glucosamine is supposed to affect the cartilage in your knee and strengthen it, but whether it did or not, I don’t know. I just kept taking them until such a time that I decided it wasn’t doing me any good,” Participant 4, man, 77 years old.
Many participants had heard of experimental treatments offering hope that the cartilage in the knee could be replaced by minimally invasive methods: “[The doctor] told me it was a new technique, it was just an injection. They would inject it and then the two bones would stop rubbing each other. Two weeks later it was on the news, they were saying that it got everybody walking without any problems,” Participant 11, woman, 60 years old. Many expressed that if such interventions were available, they would prefer them to TKA: “I’ve heard people have this stuff they inject in. They take your fat cells and they grow it and they put it back in to the joint, so it’s just like a cartilage. I was hoping to get that, I would have preferred it, but the surgeon said it’s too far gone,” Participant 1, man, 65 years old.
Most participants articulated that their mechanical problem required a mechanical solution: “Well what’s the point in trying to do something when something’s worn out? I believe in nuts and bolts; if something’s worn out, you pull it out and put a new part in,” Participant 19, man, 65 years old. TKA was believed to be the only option to “cure” symptoms by replacing the damaged joint: “The arthritis is so bad that the knee has to be replaced, there is no other option,” Participant 25, man, 64 years old. TKA was also seen as the only option to put space back into the joint: “[TKA] will lift the two bones that have collapsed together to give it a bit of sponginess. Because it just feels all collapsed,” Participant 6, woman, 55 years old.
In contrast to the sense of urgency to address their bone on bone issue described under the theme “Timeline beliefs,” a few participants had been told that they were too young to have TKA. For these participants, delaying TKA was considering delaying the inevitable. They described feelings of despair at being left with no option but to “sit and wait” until they were old enough: “I’ve just been waiting, putting up with the pain, because all the doctors say I’m too young. But everyone in my family dies before 70. So, what, am I going to live for the rest of my life in pain? The x-rays clearly show that there’s no cartilage in my knee,” Participant 19, man, 65 years old. Now on the waiting list for TKA, these younger participants were optimistic that medical advancements would extend the longevity of the prosthesis: “They say that it only lasts for 10 years and that’s why they try to put it off as long as possible. I think it’ll last longer … I just think with how medical things improve all the time, they will make it better and make it last longer,” Participant 26, woman, 62 years old.
Discussion
Excessive and inappropriate use of resources for knee OA places a burden on orthopaedic services. We adopted a qualitative approach to gain insight into why patients may be unwilling to accept nonsurgical interventions for knee OA. In this paper, we described beliefs about knee OA and its treatment through interviews with 27 people on the waiting list for TKA and found that patients’ beliefs may play in role in their reluctance to accept nonsurgical interventions. Believing that one’s knee joint was bone on bone, caused by wear and tear that was exacerbated by increased loading through the knee and would only get worse over time, motivated participants to minimize loading through the knee and seek treatments they perceived would replace worn cartilage (Fig. 1).
Fig. 1.

The beliefs of participants with endstage knee OA are shown.
Limitations
Health beliefs are formed from personal experiences of a health condition, observing others with the condition, and from external sources such as the media, general practitioners and orthopaedic surgeons [1]. Alongside general practitioners, it is the role of surgeons to address unhelpful beliefs about OA and its nonsurgical management. As we only recruited patients from one orthopaedic service, it is possible that the beliefs of this sample reflect the efforts of the surgeons in this service and are not generalizable to patients on the waiting list for TKA at other orthopaedic services. We recruited people on the waiting list for TKA as we expected these individuals to have a range of experiences to draw from and to be able to reflect on how their beliefs/attitudes had changed over time. However, we did not list all the nonsurgical interventions the participants had previously engaged in and instead relied on the participants’ recall of these experiences. Future qualitative research exploring the beliefs of primary care patients is warranted to inform primary care interventions targeting unhelpful beliefs to increase uptake of nonsurgical care before patients enter orthopaedic services.
Consistent with the qualitative approach, we did not randomly recruit our sample but approached people who met the eligibility criteria and asked them to participate. As a result, our small sample of 27 participants may have differed from the wider population in important ways. For instance, we excluded people who did not speak English, and given that beliefs are situated in the cultural context of the individual [1], the beliefs described in this sample may not reflect the beliefs of people from nonEnglish speaking backgrounds. Further, it is possible that the people who agreed to take part in this study felt more confident about communicating their perceptions and experiences in a 30-minute interview and, therefore, had higher levels of health literacy. Given that lower health literacy is associated with poorer health beliefs [11], it is possible that the findings from this sample are reflective of more positive beliefs than those held by the wider population. Despite these limitations, we note considerable overlap between our findings and those from a previous study involving a community-based sample in the United Kingdom [21], and the beliefs we identified resonate with what members of a multidisciplinary team (including an orthopaedic surgeon, orthopaedic nurse, general practitioner and physiotherapist) observe in their clinical practice.
In this study the belief that one had bone on bone changes in the knee appeared to be a key misconception associated with the patient’s lack of acceptance of nonsurgical care for OA. Once participants had bone on bone changes, physiotherapy and exercise interventions were disregarded in favor of alternative and experimental treatments that many believed could regenerate lost knee cartilage. Although participants believed that exercise and activities that involved loading the knee could further damage their vulnerable joint, systematic review evidence suggests that loading exercise is not harmful to articular cartilage in people with knee OA [4]. In contrast to available evidence for alternative and experimental treatments, and contrary to what patients believe, there is high-quality evidence that exercises to load the knee can reduce pain and improve quality of life and function in people with knee OA [10, 18]. Furthermore, fear of joint damage can lead to activity avoidance and in turn, loss of muscle strength, lack of confidence, and fear of falling [6, 29]. Educating patients on the benefits of weightbearing exercise and the consequences of avoidance behavior should be a key objective for clinicians during the clinical encounter. Our findings point to a need to educate general practitioners, physiotherapists and orthopaedic surgeons about the benefits of nonsurgical interventions for knee OA. A perceived lack of nonsurgical treatment alternatives among orthopaedic surgeons has been suggested to play a role in surgical decision making [5], and some general practitioners perceive that land-based exercises and joint loading activities are also detrimental [9].
Consistent with popular belief in the community and among clinicians, the study participants believed that OA is characterized by a downward trajectory. However, evidence has shown that multiple trajectories exist in knee OA, including trajectories of stability and even recovery [7]. These trajectories can be influenced by nonoperative interventions. Findings from an uncontrolled cohort study [27] and a randomized controlled trial [25] show that participation in an exercise and education intervention while on the waiting list for TKA may cause some patients with endstage OA to gain sufficient control over the pain so that they no longer feel they need surgery. Providing nonsurgical interventions to patients on the waiting list for TKA would potentially have substantial cost implications. The average cost of a TKA is AUSD 21,000 and the total annual of cost of TKA in Australia AUSD 1.3 billion [20]. If as few as 3% or 4% of patients on the waiting list avoided TKA because of participating in a psychological or exercise-based intervention, at a cost of just AUSD 600 to AUSD 700 per person, such interventions would be cost neutral within 12 months.
There is increasing interest in improving clinician-patient communication in orthopaedics. Previous qualitative work [2] and a recent commentary piece [26] have identified the term “bone on bone” as having a problematic, unintended meaning among patients with OA. In an editorial, Ring et al. [22] considered the way that orthopaedic surgeons talk to patients and how this may influence treatment decision making. They cite the common phrase “the patient failed conservative treatment and required joint replacement” and argue that this conveys to patients the sense that nonsurgical treatment is a stage to pass through on the road to success that ends with surgery, with the word “required” inferring an absence of options. Emerging evidence suggests that language adjustments by clinicians can influence treatment decision making in patients. Using hypothetical scenarios in a nonpatient population, McCaffery et al. [19] showed that the use of the term “noninvasive cancer” compared with “abnormal cells” increased participants’ perceptions of illness severity and led them to choose more invasive interventions. While in the musculoskeletal setting, alternative terms to describe changes within the joint space such as “narrowing” or “tightening” [26] have been proposed, future qualitative research is needed to evaluate how alternative terms are understood by patients and if or how adjustments to what clinicians say and how they say it may influence treatment decision making in people with OA.
Conclusions
This qualitative study has described how believing that one has bone on bone changes in the knee caused by wear and tear that will only get worse over time can motivate patients to minimize loading through the knee and seek surgical intervention. The findings suggest that there may be a need to correct misconceptions among clinicians that are being passed on to their patients and a need to improve clinician communication so that they do not inadvertently perpetuate misconceptions that patients present with. Based on these findings, we suggest that general practitioners and orthopaedic surgeons consider asking patients about their understanding of knee OA, its causes and consequences, as well as their beliefs about treatment and recovery, to identify and target any misconceptions and encourage wider acceptance of nonsurgical interventions. Future quantitative studies are needed to extend our understanding of the relationship between beliefs about knee OA and treatment decisions and if targeting unhelpful beliefs can increase the use of nonsurgical interventions and ease the burden on orthopaedic services.
Acknowledgments
We thank the participants for giving their time to participate in this study.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article. One of the authors (MD) holds a National Health & Medical Research Council (NHMRC) Career Development Fellowship (1122526) and one or more of the authors (MD, PC, JG) hold an NHMRC Center for Research Excellence Grant in Total Joint Replacement (1116325). The funders had no role in the conduct of this study.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the University of Melbourne, St Vincent’s Hospital Melbourne, Victoria, Australia.
References
- 1.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143-164. [DOI] [PubMed] [Google Scholar]
- 2.Barker KL, Reid M, Minns Lowe CJ. What does the language we use about arthritis mean to people who have osteoarthritis? A qualitative study. Disabil Rehabil. 2013;36:367-372. [DOI] [PubMed] [Google Scholar]
- 3.Brand CA, Harrison C, Tropea J, Hinman RS, Britt H, Bennell K. Management of osteoarthritis in general practice in Australia. Arthritis Care Res. 2014;66:551-558. [DOI] [PubMed] [Google Scholar]
- 4.Bricca A, Juhl C, Steultjens M, Wirth W, Roos E. Impact of knee joint loading exercise on MRI-assessed articular cartilage, in knee osteoarthritis: a systematic review of randomised controlled trials. Br J Sports Med. 2018;52. [DOI] [PubMed] [Google Scholar]
- 5.Bunzli S, Nelson E, Scott A, French S, Choong P, Dowsey M. Barriers and facilitators to orthopaedic surgeons’ uptake of decision aids for total knee arthroplasty: A qualitative study. BMJ Open. 2017;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bunzli S, Smith A, Schutze R, Lin I, O’Sullivan P. Making sense of low back pain and pain related fear. J Orthop Sports Phys Ther. 2017;47:628-636. [DOI] [PubMed] [Google Scholar]
- 7.Collins JE, Katz JN, Dervan EE, Losina E. Trajectories and risk profiles of pain in persons with radiographic, symptomatic knee osteoarthritis: data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2014;22:622-630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, Hsu R, Katbamna S, Olsen R, Smith L, Riley R, Sutton AJ. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006;6:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Egerton T, Nelligan RK, Setchell J, Atkins L, Bennell KL. General practitioners’ views on managing knee osteoarthritis: a thematic analysis of factors influencing clinical practice guideline implementation in primary care. BMC Rheumatology. 2018;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med. 2015;49:1554-1557. [DOI] [PubMed] [Google Scholar]
- 11.Hadden K, Prince L, Bushmiaer M, Watson J, Lowry Barnes C. Health literacy and surgery expectations in total hip and knee arthroplasty patients. Patient Educ Couns. 2018;101:1823-1827. [DOI] [PubMed] [Google Scholar]
- 12.Haskins R, Henderson JM, Bogduk N. Health professional consultation and use of conservative management strategies in patients with knee or hip osteoarthritis awaiting orthopaedic consultation. Aust J Prim Health. 2014;20:305-310. [DOI] [PubMed] [Google Scholar]
- 13.Healey E, Afolabi E, Lewis M, Edwards J, Jordan K, Finney A, Jinks C, Hay E, Dziedzic K. Uptake of the NICE osteoarthritis guidelines in primary care: a survey of older adults with joint pain. BMC Musculoskelet Disord. 2018;19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hinman R, Nicolson P, Dobson F, Bennell K. Use of nondrug, nonoperative interventions by commnity-dwelling people with hip and knee osteoarthritis. Arthritis Care Res. 2015;67:305-309. [DOI] [PubMed] [Google Scholar]
- 15.Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, Towheed T, Welch V, Wells G, Tugwell P. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care & Research. 2012;64:465-474. [DOI] [PubMed] [Google Scholar]
- 16.Hunter D, Neogi T, Hochberg MC. Quality of osteoarthritis management and the need for reform in the US. Arthritis Care Res. 2011;63:31-38. [DOI] [PubMed] [Google Scholar]
- 17.Leventhal H, Phillips L, Burns E. The Common Sense Model of Self Regulation (CSM): a dynamic framework for understanding illness self management. J Behav Med. 2016;39:935-946. [DOI] [PubMed] [Google Scholar]
- 18.McAlindon T, Bannuru R, Sullivan M, Arden N, Berenbaum F, Bierma-Zienstra S, Hawker G, Henrotin Y, Hunter D, Kawaguchi H, Kwoh K, Lohmander S, Rannou F, Roos E, Underwood M. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22:363-388. [DOI] [PubMed] [Google Scholar]
- 19.McCaffery K, Nickel B, Moynihan R, Hersch J, Teixeira-Pinto A, Irwig L, Barratt A. How different terminology for ductal carcinoma in situ impacts women's concern and treatment preferences: a randomised comparison within a national community survey. BMJ Open. 2015;5:e008094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peel T, Cheng A, Liew D, Buising K, Lisik J, Carroll K, Choong P, Dowsey M. Direct hospital cost determinants following hip and knee arthroplasty. Arthritis Care Res. 2015;67:782-790. [DOI] [PubMed] [Google Scholar]
- 21.Pouli N, Das Nair R, Lincoln NB, Walsh D. The experience of living with knee osteoarthritis: exploring illness and treatment beliefs through thematic analysis. Disabil Rehabil. 2014;36:600-607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ring DC, Dobbs MB, Gioe TJ, Manner PA, Leopold SS. Editorial: How the words we use affect the care we deliver. Clin Orthop Relat Res. 2016;474:2079-2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Burgess R, ed. Analyzing qualitative data. London: New York: Routledge; 1994:173-194. [Google Scholar]
- 24.Skou S, Roos E, Laursen M, Rathleff M, Arendt-Nielsen L, Rasmussen S, Simonsen O. Total knee replacement and non-surgical treatment of knee osteoarthritis: 2-year outcome from two parallel randomized controlled trials. Osteoarthritis Cartilage. 2018;26:1170-1180. [DOI] [PubMed] [Google Scholar]
- 25.Skou ST, Roos EM, Laursen MB, Rathleff MS, Arendt-Nielsen L, Simonsen O, Rasmussen S. A randomized, controlled trial of total knee replacement. N Engl J Med. 2015;373:1597-1606. [DOI] [PubMed] [Google Scholar]
- 26.Stewart M, Loftus S. Sticks and Stones: The impact of language in musculoskeletal rehabilitation. J Orthop Sports Phys Ther. 2018;48:519-522. [DOI] [PubMed] [Google Scholar]
- 27.Teoh L, Eyeles J, Makovey J, Williams MT, Kwoh C, Hunter D. Observational study of the impact of an individualized multidisciplinary chronic care program for hip and knee osteoarthritis treatment on willingness for surgery. Int J Rheum Dis. 2017;20:1383-1392. [DOI] [PubMed] [Google Scholar]
- 28.Victorian Musculoskeletal Clinical Leadership Group. Victorian model of care for osteoarthritis of the hip and knee. Melbourne, Australia: MOVE muscle, bone & joint health; 2018. [Google Scholar]
- 29.Vlaeyen J, Linton S. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85:317-332. [DOI] [PubMed] [Google Scholar]


