Abstract
The importance of the labrum in the biomechanics of the hip joint is well documented. Labral tears are the most common pathology in patients undergoing hip arthroscopy and therefore appropriate labral management is vital. Labral preservation has been advocated as a superior alternative to labral excision in terms of clinical outcomes. While reconstruction of the labrum is recommended for irreparable tears, labral augmentation is a viable alternative for labral function restoration under certain indications. This Technical Note will describe a method for arthroscopic hip labral augmentation using an anterior tibialis tendon allograft and the pull-through technique.
The chondrolabral seal is essential for the function of a normal hip joint.1, 2, 3, 4 In the case of irreparable labral tears, labral reconstruction is the recommended procedure to reestablish the “seal,” the vacuum effect that imparts joint stability.5, 6 Not all irreparable tears, however, are the same. In some tears, the inner-most circumferential labral fibers are well preserved and identifiable arthroscopically. Consequently, it may be suitable to maintain those fibers by adding structural tissue reinforcement via tissue augmentation.7, 8, 9 A hypoplastic labrum may also warrant augmentation, in which case the diminutive native labrum would similarly be reinforced by the graft tissue.7, 8 Potential indications and contraindications for labral augmentation are listed in Table 1. We present our arthroscopic labral augmentation technique with important variations from previous descriptions.9 First, the use of an allograft tendon avoids the risk of donor side morbidity. Second, the pull-through technique previously described for labral reconstruction avoids the need to measure the labral defect and eliminates length mismatch.10 Other advantages and disadvantages are presented in Table 2.
Table 1.
Surgical Indications and Contraindications for Arthroscopic Labral Augmentation
| Indications |
| Irreparable tears with native labral circumferential fibers in good macroscopic conditions |
| Hypoplastic labrum |
| Contraindications |
| Reparable tears |
| Intraoperative findings of non-viable or irreparable labral tear with compromised circumferential fibers |
| Completely calcified labrum |
Table 2.
Advantages and Disadvantages for Arthroscopic Labral Augmentation
| Advantages |
| Labral “suction seal” restored |
| Measurement of the labral defect is unnecessary |
| Restoration of labral functions |
| Preservation of the native circumferential labral fibers |
| Allograft reduces donor-side morbidity |
| Disadvantages |
| Technically demanding procedure |
| Longer surgical time |
| Possible increase of inherent arthroscopic complications |
Surgical Technique
Patient Preparation and Positioning
General anesthesia is administered to achieve skeletal relaxation. The patient is placed in the modified supine position on a traction table (Supine Hip Positioning System; Smith & Nephew, Andover, MA) with an extra padded post. Extra padding to the feet is provided (Fig 1A). Once the patient is secured:
-
1.
Manual bilateral traction is simultaneously applied to achieve full contact between the perineum and the padded post.
-
2.
The operative leg is positioned to neutral rotation and adduction, whereas the nonoperative leg is placed in 30° of abduction.
-
3.
The operative table is transitioned from 0° to 10° of Trendelenburg inclination. Pelvic tilt is corrected by lateralizing the operative table such that both anterosuperior iliac spines are parallel to the floor.
Fig 1.
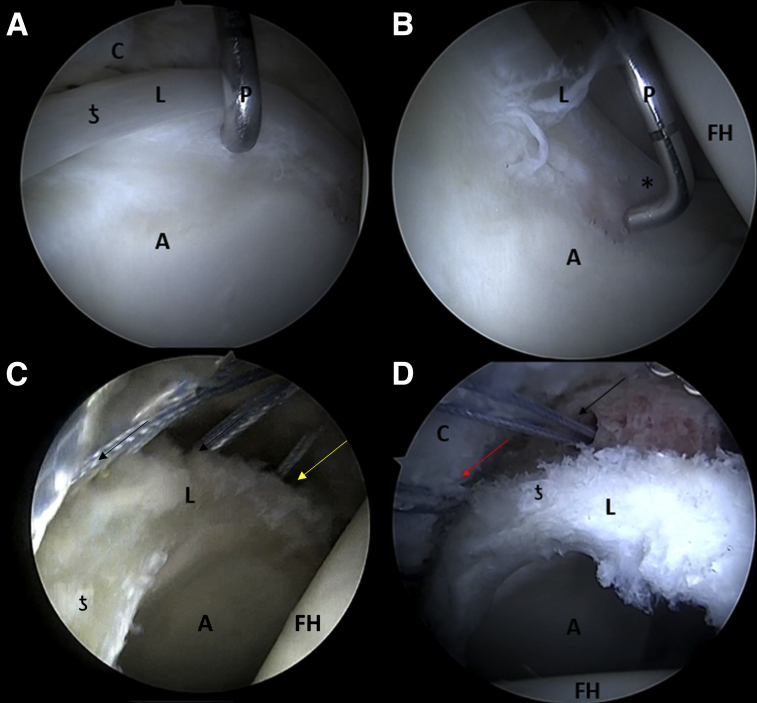
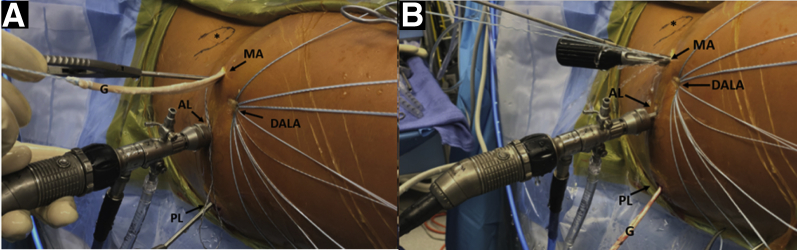
(A) Patient is positioned in the modified supine position. Patient's head is to the left, and feet are to the right, anterior inferior iliac spine is marked (*). (B) Right hip with patient's head to the left and feet to the right. The four portals used are identified: anterolateral (AL), mid-anterior (MA), distal anterolateral accessory (DALA), posterolateral (PL). Anterior inferior iliac spine (*) is also identified. (C) Central compartment of a right hip viewed from the AL portal with the 70° arthroscope. The following anatomic structures are identified, acetabulum (A), capsule (C), labrum (L), and femoral head (FH). The 3 o'clock position is noted. The probe (P) is coming through the MA portal and reveals an irreparable labral tear with intact circumferential inner fibers. (D) An assembled anterior tibialis tendon allograft (G), the red arrow identifies the end with the PushLock anchor (PUL) for the most medial point of fixation, the blue arrow identifies the free Fiberloop limbs after Krackow stiches.
Fluoroscopy Technique
-
1.
The C-arm is draped in sterile fashion and positioned on the nonoperative side of the patient.
-
2.
A true anterior-posterior image of the pelvis is obtained by tilting the C-arm to compensate for the Trendelenburg inclination. The joint seal is broken before traction is applied.
Portals Placement
Anterolateral (AL), mid-anterior (MA), distal anterolateral accessory (DALA), and posterolateral (PL) portals are created as previously described10 (Fig 1B).
Diagnostic Arthroscopy and Labral Assessment
Systematic diagnostic arthroscopy is performed to assess the ligamentum teres, acetabular notch, presence of iliopsoas impingement sign, labral and chondrolabral junction conditions, and acetabular and femoral head cartilage. In the case of irreparable labral tears, labral augmentation is indicated over reconstruction if macroscopic evidence of preserved native circumferential labral fibers is noted during labral assessment7 (Fig 1C and Video 1).
Labral Augmentation Technique
Graft Preparation
A 6- to 7-mm single-stranded anterior tibialis tendon allograft is used for this augmentation. Three to four Krackow stiches are placed at both ends of the graft with 2.0 Fiberloop (Arthrex, Naples, FL). One side is prepared with a 2.9-mm PushLock anchor (Arthrex), and the other side remains free. Preserve the loop of the suture on the free end (Fig 1D).
The authors of the present technique use 3.0-mm Knotless SutureTak anchors (Arthrex) for graft fixation. The knotless pull-through technique previously described and published by the senior author for labral reconstruction avoids the need to measure the defect.10
Acetabular Rim Preparation
The AL portal is used as the viewing portal, whereas the MA and DALA portals are working ones. A shaver and radiofrequency device are used to elevate the capsule from the acetabulum. A traction stitch can be placed between the 12- to 1-o'clock positions through the MA portal. From the DALA portal, a 5.5-mm burr is used to trim a predetermined amount of the acetabular rim. Exercise caution not to detach the remaining circumferential labral fibers. Be sure always to maintain adequate visualization of instruments when removing any frayed peripheral labral tissue (Video 1).
Anchors Drilling and Placement
Anchor holes are drilled medial to lateral. The first drill hole is intended for the PushLock anchor, which must be inserted from the MA portal to perform the knotless pull-through technique. Despite being the most medial anchor and first to be drilled, the PushLock anchor is placed only after all other Knotless SutureTaks are in place.
From the DALA portal, Knotless SutureTaks are placed sequentially, approximately 5 mm apart. Sutures from the anchors must be secured to the drape and ordered appropriately for suture management (Fig 2). The number of anchors needed depends on the defect size.
Fig 2.
Right hip, patient's head is to the left and feet to the right, anterior superior iliac spine is marked (*). Portals are identified by the black arrows: anterolateral (AL), mid-anterior (MA), distal anterolateral accessory (DALA), posterolateral (PL). SutureTak anchors are sequentially placed from medial to lateral through the DALA portal and attached to the external drape, inferior to superior. In this image, 8 SutureTak anchors are enumerated. In the video, 5 are used.
Graft Pull-Through
After all the Knotless SutureTaks are in place (Fig 3), the graft must be “pulled-through” the hip joint through the MA and out the PL portal (Fig 4 and Video 1). It is critical to proceed as follows:
-
1.
A 4-mm switching stick is placed through the PL portal, positioning it posterior to the suture of the most posterior anchor. Once in place, pass in the halfpipe and replace the switching stick with a grasper.
-
2.
Place the switching stick from the MA portal, anterior to the sutures of the most anterior anchor. Leave the halfpipe in.
-
3.
Take the graft and grasp the free end with a suture retriever and insert it through the MA portal. At this point the graft should still be outside the joint (Fig 4A).
-
4.
With the grasper placed in the PL portal, grasp the free end and retrieve the graft, passing through MA portal and out the PL portal (Fig 4B).
Fig 3.
Intraoperative image of the labral augmentation using anterior tibialis tendon allograft and the pull-through technique in a right hip visualized with a 70° arthroscope from the anterolateral portal. (A) During diagnostic arthroscopy, a labral tear with a hypotrophic labrum (L) is found. Probe (P) is coming from the mid-anterior portal, and the 12 o'clock position (ƾ), acetabulum (A), and capsule (C) are identified. (B) A different perspective is achieved and the medial extension of the labral tear (L) can be seen. The 3 o'clock position (*) and femoral head (FH) are marked. (C) Elevation of the capsule has been performed, and Knotless SutureTak anchors (black arrows) have been placed using the distal anterolateral accessory portal. The most medial SutureTak anchor can be seen (yellow arrow). (D) From this perspective the most posterolateral anchor (red arrow) is visible. All anchors have been placed, and the allograft is to be passed in.
Fig 4.
Right hip in the supine position, with the patient's head to the left and feet to the right, anterior inferior iliac spine is marked (*). Portals are identified by black arrows: anterolateral (AL), mid-anterior (MA), distal anterolateral accessory (DALA), and posterolateral (PL). After all Knotless SutureTaks are placed, the anterior tibialis allograft (G) must be “pulled-through” the hip joint through the MA portal (A) and out the PL portal (B).
Graft Fixation
Graft fixation follows the same order of anchor placement, medial to lateral. With the 70° arthroscope still in the AL portal and the graft outside the PL portal, introduce the PushLock anchor (previously assembled with one of the graft's Fiberloop sutures) through the MA portal (Fig 5).
Fig 5.
Right hip in the supine position, patient's head is to the left and feet to the right. Portals are identified by the black arrows: anterolateral (AL), mid-anterior (MA), distal anterolateral accessory (DALA), posterolateral (PL). For the most medial point of fixation, the PushLock anchor (red arrow) is introduced through the MA portal. The PushLock is positioned and, after appropriate Fiberloop suture tension, the anterior tibialis allograft (G) is reinserted in the hip joint. The PushLock anchor is secured with gentle tapping.
The PushLock is inserted into the predrilled position. After applying appropriate Fiberloop suture tension, the graft is reinserted into the hip joint. The graft is then secured with gentle taping of the anchor (Video 1). Next, place a plastic cannula in the MA portal.
Working medial to lateral, the following steps are repeated for each Knotless SutureTak:
-
1.
Only unclamp from the drape the Knotless SutureTak that is about to be used.
-
2.
Working through the MA portal, arthroscopically identify the correct anchor and grasp only the “passing” suture and create a loop around the graft (Video 1).
-
3.
From the DALA portal, the assistant will hold both ends of the “shuttle” suture and identify the one without the loop. To do so, provide slight slack to both “shuttle” suture limbs. The assistant applies minimal tension on the end without the loop to distinguish between sutures.
-
4.
The “shuttle” limb suture with the loop is retrieved from the MA portal and assembled with the “passing” suture.
-
5.
Working through the DALA portal, traction is applied to the remaining “shuttle” suture limb, bringing the “passing” suture to the anchor locking mechanism.
-
6.
Desired tension is applied by the surgeon to the “passing” suture while the assistant provides gentle traction to the lateral end of the graft through the free Fiberloop in the PL portal. This applied force keeps the graft taut as it is fixated (Fig 6).
Fig 6.
Intraoperative images of the labral augmentation using anterior tibialis tendon allograft and the pull-through technique in a right hip visualized with a 70° arthroscope from the anterolateral portal. The hip is under traction and in the supine position. (A) The most medial fixation point for the graft (G) is achieved with the PushLock (red arrow). The suture from the first Knotless SutureTak has been passed behind the graft and through the native chondrolabral junction (yellow arrow) without tension. The 12 o'clock position (ƾ), femoral head (FH), and capsule (C) are identified. (B) Tension is applied to the suture of the first Knotless SutureTak, achieving fixation of the second point of the graft to the native labrum (G). Fibers of the native labrum can be seen (blue arrow). (C) In this view from the anterolateral portal, the 70° arthroscope is rotated 180° and the last Knotless SutureTak anchor can be seen (green arrow). The native labrum is marked (black arrow). The anterior tibialis allograft (G) of the augmentation construct is delineated from the native labrum (L) by the dotted line. The remaining excess of the G is amputated with a radiofrequency device (R). The 12 o'clock position (ƾ), acetabulum (A) and femoral head (FH) are identified. (D) Traction is released to restore the labral seal.
After all Knotless SutureTaks have been used and the appropriate segment of the defect has been covered by the graft, the excess graft is amputated with radiofrequency (Fig 6C and Video 1).
Postoperative Rehabilitation
The patient is placed in a brace (Donjoy X-Act ROM Hip Brace; Donjoy, Carlsbad, CA) for 6 weeks. Use of crutches is encouraged for 6 weeks, with weightbearing restriction of up to 20 pounds foot-flat weightbearing. Under physiotherapist supervision, active range-of-motion exercise is initiated during the first 48 hours with continuous passive motion, static bicycle, or both. Formal physical therapy protocol is begun after the first 6 weeks.
Discussion
The purpose of this technique is to restore hip labrum functionality by preserving viable native circumferential labral fibers by structural augmentation (Fig 7). In the pursuit of a more minimally invasive procedure, this technique opts for an anterior tibialis tendon allograft to avoid potential donor-side morbidity.11 To improve graft fixation and to achieve a more reproducible and faster technique, modern knotless anchor technology is used. Our current indications and contraindications are presented in Table 1.
Fig 7.
(A) Before and (B) after intraoperative images of the labral augmentation using anterior tibialis tendon allograft and the pull-through technique. Viewed from the anterolateral portal with the 70° arthroscope in a right hip, supine position. A, acetabulum; C, capsule; FH, femoral head; G, anterior tibialis allograft; L, irreparable labral tear with intact inner circumferential fibers.
Labral reconstruction is currently the technique of choice for treating irreparable tears, which require complete excision of native labral fibers. Favorable short-term and mid-term outcomes have been reported for labral reconstructions.5, 12, 13, 14, 15 As with reconstruction, augmentation seeks to reestablish the labrum's sealing mechanism, which is critical for appropriate biomechanical function of the hip joint6, 16 (Fig 6D and Video 1).
Philippon et al.7 reported their outcomes comparing labral augmentation versus reconstruction. Thirty-three labral augmentation patients were matched 1:2 with patients undergoing labral reconstruction.7 The authors found that, in their hands, higher clinical outcomes were observed in patients who had previous hip procedures and underwent labral augmentation versus labral reconstruction surgery. Similar revision rates and conversion to total hip arthroplasty were seen in both groups. However, the augmentation technique used by Locks et al.9 is notably different from that presented here. In their article, (1) an autograft needs to be harvested, (2) knots need to be tied, and (3) the labral defect must be measured.9 Labral defect measurement has been suggested by others for labral augmentation techniques,17 but we believe that forgoing this step relieves the risk of graft-defect mismatch and provides for a more expedited procedure (Table 2). Pearls and pitfalls of this procedure are reported in (Table 3).
Table 3.
Arthroscopic Labral Augmentation Pearls and Pitfalls
| Pearls |
| Minimal to no acetabular trimming |
| Use of knotless anchors technology to decrease surgical time |
| Preservation of the capsule for further capsular plication |
| Use of “hard bone” drill to minimize the risk of anchor locking mechanism failure during suture shuttling |
| Pitfalls |
| Minimal experience in advanced arthroscopy techniques may result in a non-reproducible procedure |
| Losing track of the order of sutures and anchors |
| Forgetting to apply gentle tension in the graft during the fixation can result in a bulky augmentation |
Hip arthroscopy with labral augmentation is a feasible alternative for the management of certain types of irreparable labral tears (Fig 7). Nevertheless, we acknowledge the demanding nature of this arthroscopic procedure and recognize the risks. Extravasation is a common concern for arthroscopic procedures. The surgeon must also factor in other previously reported potential complications inherent to hip arthroscopy (Table 4).
Table 4.
Risks and Limitations
| Risks |
| Abdominal extravasation |
| Abdominal compartmental syndrome |
| Tight compartmental syndrome |
| Increased risk of neurologic lesion |
| Limitations |
| Trained surgical team/staff |
| Availability of allografts |
| Challenging procedure |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.C.L. reports grants and non-financial support from Arthrex, non-financial support from Iroko, non-financial support from Medwest, non-financial support from Smith & Nephew, grants and non-financial support from Stryker, non-financial support from Vericel, non-financial support from Zimmer Biomet, outside the submitted work. B.G.D. reports grants and other from American Orthopedic Foundation, during the conduct of the study; personal fees from Adventist Hinsdale Hospital, personal fees and non-financial support from Amplitude, grants, personal fees and non-financial support from Arthrex, personal fees and non-financial support from DJO Global, grants from Kaufman Foundation, grants, personal fees and non-financial support from Medacta, grants, personal fees, non-financial support and other from Pacira Pharmaceuticals, grants, personal fees, non-financial support and other from Stryker, grants from Breg, personal fees from Orthomerica, grants, personal fees, non-financial support and other from Mako Surgical Corp, grants and non-financial support from Medwest Associates, grants from ATI Physical Therapy, grants, personal fees and non-financial support from St. Alexius Medical Center, grants from Ossur, outside the submitted work; In addition, Dr. Domb has a patent 8920497 - Method and instrumentation for acetabular labrum reconstruction with royalties paid to Arthrex, a patent 8708941 - Adjustable multi-component hip orthosis with royalties paid to Orthomerica and DJO Global, and a patent 9737292 - Knotless suture anchors and methods of tissue repair with royalties paid to Arthrex and Dr. Domb is the Medical Director of Hip Preservation at St. Alexius Medical Center, a board member for the American Hip Institute Research Foundation, AANA Learning Center Committee, the Journal of Hip Preservation Surgery, the Journal of Arthroscopy; has had ownership interests in the American Hip Institute, Hinsdale Orthopedic Associates, Hinsdale Orthopedic Imaging, SCD#3, North Shore Surgical Suites, and Munster Specialty Surgery Center. R.W. reports Dr. Walker reports non-financial support from Encore Medical, non-financial support from Globus Medical, non-financial support from Acumed LLC, non-financial support from Depuy Synthes Sales, non-financial support from Medical Device Business Services, non-financial support from Johnson and Johnson International, non-financial support from Smith & Nephew, non-financial support from DJO, non-financial support from Covidien Caribbean, non-financial support from Biomarin Pharmaceutical, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The video presents a labral augmentation using an anterior tibialis allograft and the pull-through technique to treat a labral tear in a patient's right hip with a hypoplastic labrum. With the patient in the supine position under traction, the joint is accessed from the anterolateral portal and visualized using a 70° arthroscope. After completing the diagnostic arthroscopy, the inner circumferential labral fibers are found to be intact. The rim is prepared using a 5.5-mm burr from the distal anterolateral accessory (DALA) portal. From the mid-anterior portal, a drill hole is created for the most medial point of fixation for the 2.9 mm PushLock anchor. From the DALA portal, the knotless SutureTak anchors are placed sequentially from medial to lateral. A 6- to 7-mm single-stranded anterior tibialis tendon allograft is used for labral augmentation. The graft is passed from the mid-anterior portal to the posterolateral portal using the pull-through maneuver. The PushLock anchor is inserted at the most medial position of the defect, and the graft is retrieved back into the joint and fixated. Medial to lateral fixation with the remaining Knotless SutureTak anchors along the acetabular rim is performed. The excess graft is amputated with a radiofrequency device. The final portion of the video reveals the augmented labrum restoring the suction seal of the joint.
References
- 1.Ferguson S.J., Bryant J.T., Ganz R., Ito K. The acetabular labrum seal: A poroelastic finite element model. Clin Biomech Bristol Avon. 2000;15:463–468. doi: 10.1016/s0268-0033(99)00099-6. [DOI] [PubMed] [Google Scholar]
- 2.Bsat S., Frei H., Beaulé P.E. The acetabular labrum: A review of its function. Bone Jt J. 2016;98-B(6):730–735. doi: 10.1302/0301-620X.98B6.37099. [DOI] [PubMed] [Google Scholar]
- 3.Philippon M.J., Nepple J.J., Campbell K.J. The hip fluid seal—Part I: The effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22:722–729. doi: 10.1007/s00167-014-2874-z. [DOI] [PubMed] [Google Scholar]
- 4.Dwyer M.K., Noble P.C. Evaluating the outcome of hip preserving procedures: Patient function, satisfaction, and impairment. In: McCarthy J.C., Noble P.C., Villar R.N., editors. Hip Joint Restoration: Worldwide Advances in Arthroscopy, Arthroplasty, Osteotomy and Joint Preservation Surgery. Springer New York; New York: 2017. pp. 649–653. [Google Scholar]
- 5.Chandrasekaran S., Darwish N., Close M.R., Lodhia P., Suarez-Ahedo C., Domb B.G. Arthroscopic reconstruction of segmental defects of the hip labrum: Results in 22 patients with mean 2-year follow-up. Arthroscopy. 2017;33:1685–1693. doi: 10.1016/j.arthro.2017.03.015. [DOI] [PubMed] [Google Scholar]
- 6.Domb B.G., Hartigan D.E., Perets I. Decision making for labral treatment in the hip: Repair versus débridement versus reconstruction. J Am Acad Orthop Surg. 2017;25:e53–e62. doi: 10.5435/JAAOS-D-16-00144. [DOI] [PubMed] [Google Scholar]
- 7.Philippon M.J., Bolia I.K., Locks R., Briggs K.K. Labral preservation: Outcomes following labrum augmentation versus labrum reconstruction. Arthroscopy. 2018;34:2604–2611. doi: 10.1016/j.arthro.2018.04.021. [DOI] [PubMed] [Google Scholar]
- 8.Krych A.J. Editorial commentary: Meet your newest tool in the hip labral preservation toolbox: Labral augmentation. Arthroscopy. 2018;34:2612–2613. doi: 10.1016/j.arthro.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 9.Locks R., Chahla J., Frank J.M., Anavian J., Godin J.A., Philippon M.J. Arthroscopic hip labral augmentation technique with iliotibial band graft. Arthrosc Tech. 2017;6:e351–e356. doi: 10.1016/j.eats.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perets I., Hartigan D.E., Chaharbakhshi E.O., Walsh J.P., Close M.R., Domb B.G. Circumferential labral reconstruction using the knotless pull-through technique-surgical technique. Arthrosc Tech. 2017;6:e695–e698. doi: 10.1016/j.eats.2017.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barbour S.A., King W. The safe and effective use of allograft tissue—an update. Am J Sports Med. 2003;31:791–797. doi: 10.1177/03635465030310052801. [DOI] [PubMed] [Google Scholar]
- 12.Boykin R.E., Patterson D., Briggs K.K., Dee A., Philippon M.J. Results of arthroscopic labral reconstruction of the hip in elite athletes. Am J Sports Med. 2013;41:2296–2301. doi: 10.1177/0363546513498058. [DOI] [PubMed] [Google Scholar]
- 13.Geyer M.R., Philippon M.J., Fagrelius T.S., Briggs K.K. Acetabular labral reconstruction with an iliotibial band autograft: Outcome and survivorship analysis at minimum 3-year follow-up. Am J Sports Med. 2013;41:1750–1756. doi: 10.1177/0363546513487311. [DOI] [PubMed] [Google Scholar]
- 14.Scanaliato J.P., Christensen D.L., Salfiti C., Herzog M.M., Wolff A.B. Primary circumferential acetabular labral reconstruction: Achieving outcomes similar to primary labral repair despite more challenging patient characteristics. Am J Sports Med. 2018;46:2079–2088. doi: 10.1177/0363546518775425. [DOI] [PubMed] [Google Scholar]
- 15.Locks R., Chahla J., Bolia I.K., Briggs K.K., Philippon M.J. Outcomes following arthroscopic hip segmental labral reconstruction using autologous capsule tissue or indirect head of the rectus tendon. J Hip Preserv Surg. 2018;5:73–77. doi: 10.1093/jhps/hnx033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.White B.J., Herzog M.M. Labral reconstruction: When to perform and how. Front Surg. 2015;2:27. doi: 10.3389/fsurg.2015.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McConkey M.O., Moreira B., Mei-Dan O. Arthroscopic hip labral reconstruction and augmentation using knotless anchors. Arthrosc Tech. 2015;4(6):e701–e705. doi: 10.1016/j.eats.2015.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The video presents a labral augmentation using an anterior tibialis allograft and the pull-through technique to treat a labral tear in a patient's right hip with a hypoplastic labrum. With the patient in the supine position under traction, the joint is accessed from the anterolateral portal and visualized using a 70° arthroscope. After completing the diagnostic arthroscopy, the inner circumferential labral fibers are found to be intact. The rim is prepared using a 5.5-mm burr from the distal anterolateral accessory (DALA) portal. From the mid-anterior portal, a drill hole is created for the most medial point of fixation for the 2.9 mm PushLock anchor. From the DALA portal, the knotless SutureTak anchors are placed sequentially from medial to lateral. A 6- to 7-mm single-stranded anterior tibialis tendon allograft is used for labral augmentation. The graft is passed from the mid-anterior portal to the posterolateral portal using the pull-through maneuver. The PushLock anchor is inserted at the most medial position of the defect, and the graft is retrieved back into the joint and fixated. Medial to lateral fixation with the remaining Knotless SutureTak anchors along the acetabular rim is performed. The excess graft is amputated with a radiofrequency device. The final portion of the video reveals the augmented labrum restoring the suction seal of the joint.