Abstract
Partial-thickness rotator cuff tears are among the most common challenges faced by orthopaedic surgeons today. The ability to adequately manage these injuries depends on identifying their full extent during arthroscopic evaluation. There are many ways to fully visualize these tears, including arm positioning and gentle debridement. The purpose of this article is to highlight several tips and techniques to enable full visualization of partial-thickness rotator cuff tears to determine appropriate treatment.
Partial-thickness rotator cuff tears are a frequent challenge faced by the orthopaedic surgeon. They are a cause of significant pain for the patient and can cause long-term disability when not adequately treated.1 It is well known that adequate visualization is imperative to successfully treat these injuries. The depth and extent of the tear is a key factor in formulating a surgical management plan.2 A classification system (Table 1) previously developed by Ellman3 is beneficial in determining this treatment plan, once the tear has been adequately visualized. The key challenge, however, is in ensuring accurate arthroscopic identification of these tears.
Table 1.
Ellman Classification System for the Assessment of Partial-Thickness Rotator Cuff Tears
| Grade 1 | Partial tear <3 mm deep |
| Grade 2 | Partial tear 3 to 6 mm deep and depth not exceeding one-half of the tendon thickness |
| Grade 3 | Partial tear >6 mm deep |
It is difficult to quantify the frequency with which partial-thickness rotator cuff tears are missed, but they can undoubtedly be a challenge to diagnose. Physical examination and imaging studies are less reliable for detection of partial-thickness rotator cuff tears than full-thickness tears. Imaging studies have been shown to have as low as 63% to 75% accuracy for diagnosing partial-thickness tears.4 In addition, standard physical examination findings are incapable of determining the extent of partial-thickness tears. This combination of diagnostic shortcomings leaves arthroscopy as the gold standard for diagnosing and evaluating the extent of these tears.
Previous studies have discussed a systematic approach for diagnosing subscapularis tears and the importance of addressing these surgically.5 Patient positioning, portal placement, and arm manipulation are discussed in constructing a diagnostic strategy for arthroscopic evaluation of subscapularis tears. Such an approach can be expanded on to assist when approaching partial-thickness cuff tears of all cuff tissues. The purpose of this article is to outline several tips and tricks that can be used to help ensure adequate visualization and identification of partial-thickness rotator cuff tears.
Surgical Technique
All shoulder arthroscopy begins with thorough intra-articular evaluation. Key diagnostic findings can only be seen while the camera is in the joint space. These findings are easily missed if the intra-articular portion of the case is not given full attention.
Optimum positioning of the shoulder is an essential first step when intra-articular arthroscopy is initiated. Gentle traction of the shoulder combined with internal and external rotation of the humerus can deliver the rotator cuff footprint to enable visualization of the entire rotator cuff footprint. The ideal position of the shoulder for visualization of the cuff footprint is the “30-30 position,” produced via ∼30° of forward flexion with 30° of abduction of the shoulder and gentle traction (Fig 1). This position opens the space underneath the superior capsule and allows full visualization of the greater tuberosity footprint (Figs 2 and 3, Video). This is useful for the visualization of subscapularis, supraspinatus, and infraspinatus tears. It is also important to note that reproducing this position with the camera in the subacromial space is particularly useful for creating space in the subacromial bursa and promotes better visualization of the rotator cuff footprint while performing bursectomy. Internal and external rotation may expose the bellows sign, which is indicative of intrasubstance tearing within the rotator cuff and may be seen as ballooning of the attached capsular tissues on the rotator cuff (Video, Fig 4).
Fig 1.
Shown is the application of the 30-30 position, produced through 30° abduction, 30° forward flexion, and gentle traction. Arthroscopic subacromial view of the right shoulder is shown, for patient positioning reference.
Fig 2.
Shown is the greater tuberosity articular side footprint visualized with the arm in the 30-30 position, of the right shoulder in a beach chair position, illustrating the benefits to visualization of specific patient positioning methods.
Fig 3.
Shown within the subacromial space is a partial bursal-sided tear, independent of the previously revealed articular partial tear, as viewed in a beach chair position, from the lateral portal with the right arm in the 30-30 position.
Fig 4.
The paired images, from the posterior portal with the right shoulder in the beach chair position, show the dynamic exposure of a bellows sign at the subscapularis insertion when the humeral head is manually rotated, allowing for identification of an intratendinous tear.
Intra-articular findings are often subtle when looking for partial-thickness tears. These may be visualized as small lesions in the capsule attached to the rotator cuff. A simple slit through the capsule may be a sign of a significant partial-thickness cuff tear (Fig 5). This is where the application of selective debridement is essential to localize and determine tear thickness. Placement of the shaver (Dyonics Powermax; Smith & Nephew) with light suction in these areas often can expose significant partial-thickness tears of the rotator cuff (Fig 6). After debridement, placement of a spinal needle and localizing suture (frequently PDS; Ethicon) allows for easy identification of the tear while in the subacromial space (Video, (Fig 7). This is a key step, as determining thickness of the tear depends on precise localization of the corresponding articular-sided lesion.
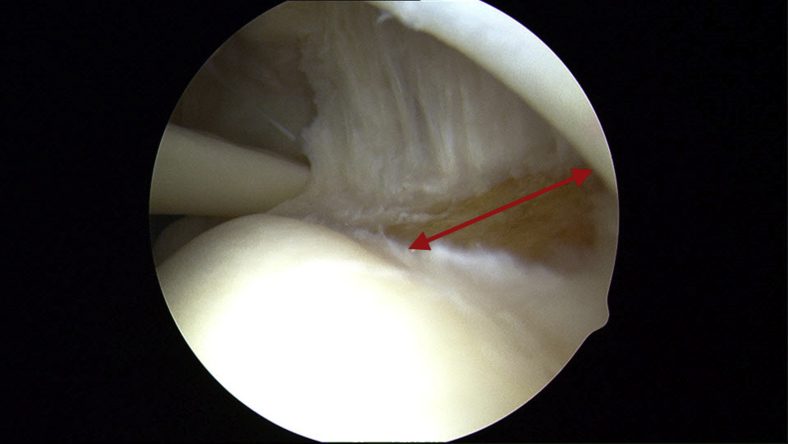
Fig 5.
A subtle superior capsule slit within the supraspinatus tendon, viewed from the posterior portal for a right shoulder in the beach chair position, provides evidence of an underlying articular sided and/or intratendinous tear.
Fig 6.
Superior capsule slit debridement exposes a near full-thickness bursal-sided tear of the rotator cuff for a right shoulder viewed from the posterior portal.
Fig 7.
Placement of the spinal needle through the articular-sided tear allows for a convenient suture marker technique to visualize the tendon tear on the bursal surface of a right shoulder viewed from the posterior portal.
While in the subacromial space, the first and most essential step in identification of partial-thickness tears involves a thorough subacromial bursectomy. Adequate visualization of the entire rotator cuff footprint through removal of the subacromial bursa is key to identifying partial-thickness bursal-sided tears. Again, the 30-30 position is helpful to open the subacromial space and deliver the rotator cuff footprint to the field of view.
It is key to avoid tunnel vision in the subacromial space after identifying partial-thickness articular sided tears. It is not uncommon to identify a partial-thickness tear on the bursal side at a distinctly different location from the articular-sided tear (Fig 8). Internal and external rotation of the glenohumeral joint while in the subacromial space is also tremendously useful and can bring the entire footprint into focus. If desired, an intra-articular depth gauge may be used after adequate bursectomy to determine the depth of tear involvement.6 Another common technique to determine an approximate tear depth is through use of a known shaver diameter as a ruler (most commonly 3.5 vs 4.5 mm).
Fig 8.
A partial-thickness, supraspinatus tear located on the articular surface, in a left shoulder. The marking suture technique is used to guide inspection of the adjacent bursal surface, revealing no pathology. Viewing is from the posterior portal within the subacromial space.
Finally, there are a few special considerations for subscapularis tears. First to consider in these scenarios is biceps management. Again, positioning of the shoulder is essential for clear identification of the subscapularis. Leaving the arm at the side is helpful, and performing a posterior “lever push” of the arm with internal rotation as described by Denard and Burkhart4 can help deliver the lesser tuberosity into view and detect otherwise hidden partial undersurface subscapularis tears (Video, Fig 9).
Fig 9.
Internal rotation with posterior translation of the humerus to expose the lesser tuberosity footprint (posterior lever push technique) is a helpful manipulation for exposure and identification of subscapularis tendon insertion tears, as seen via a posterior portal in this left shoulder, positioned in a beach chair position.
If there is difficulty fully visualizing the tear from the back, use of a 70° scope may also be considered. Other techniques include an accessory anterolateral viewing portal to obtain a top-down view of the footprint. It is also well known that biceps subluxation often coincides with tears of the subscapularis. This often interferes with complete visualization of the lesser tuberosity footprint, as well as with adequate treatment of the tear. Careful consideration should be given toward early release of the biceps to adequately visualize and treat these tears.
In addition to biceps pathology, dense rotator interval tissue frequently impedes access to treat these tears effectively. Thorough debridement of the rotator interval tissue often allows for full visualization of the anterior surface of the subscapularis, as well as a working space for suture management during repair. Subscapularis tears historically have been difficult to fully and clearly identify. Identification of the “comma tissue” is often essential to localize and approximate the appropriate reduction of the subscapularis.5, 7, 8 The comma tissue consists of the superior glenohumeral ligament and coracohumeral ligament tissue that make up the medial sling of the biceps. This may be detached from the humerus at the upper border of the subscapularis footprint but remains attached to the subscapularis. This robust tissue is an excellent means for reducing a torn subscapularis back to its anatomic location on the lesser tuberosity.
Conclusions
A plethora of literature is available discussing the treatment of partial-thickness rotator cuff tears. Among the key tenets of treatment is adequate visualization of these tears. Although there is significant discussion about the treatment, there is very limited discussion of methods of improving visualization or identifying these tears intra-operatively. Identification of subscapularis tears alone has been published,5 but few publications comprehensively identify techniques for partial-thickness supraspinatus and infraspinatus tears. This article details the many tips and tricks that can be used, and the advantages and disadvantages are summarized in Table 2.
Table 2.
Advantages and Disadvantages of the Demonstrated Techniques for Discovery, Exposure, and Repair of Partial-Thickness Rotator Tendon Tears
| Advantages | Disadvantages |
|---|---|
| Minimally invasive | Aggressive debridement and suction use can cause iatrogenic injury to the tissue |
| Standard arthroscopic setup and familiar portals | |
| Special equipment not required | The features indicating possible partial-thickness tears can be subtle and easily missed without considerable experience |
| Low-risk techniques to improve visualization |
The key pearls to these techniques emphasize the position of the arm to enhance visualization. This is a benign technique that can tremendously improve identification of partial-thickness rotator cuff tears. The 30-30 position and the posterior lever pull with internal rotation4 are simple and effective tools for this purpose. A summary of pearls and pitfalls of these techniques is listed in Table 3.
Table 3.
Pearls and Pitfalls Associated with the Demonstrated Techniques for Discovery, Exposure, and Repair of Partial-Thickness Rotator Tendon Tears
| Pearls | Pitfalls |
|---|---|
| Manipulation of shoulder position dramatically improves visualization | Biceps management crucial for subscapularis tears and release often required |
| Selective debridement can expose previously hidden bursal- and articular-sided tears | Aggressive debridement and overuse of suction can cause iatrogenic tendon injury |
| Partial tear localization with spinal needle can help identify tear on bursal side | Tunnel vision in the subacromial space can cause one to miss a bursal-sided tear in a separate location from previously seen articular-sided tear |
Selective debridement is also a key component of tear identification. When certain telltale signs are present, careful use of an arthroscopic shaver will yield dramatic improvement in the ability to identify and define tears that would be missed otherwise. The bellows sign is a feature that can localize significant intratendinous tearing.9 Injection of saline into a region of suspicious rotator cuff tendon on the bursal side will bubble out and not resist flow of saline. It has been shown that given time, most tears of the rotator cuff will increase in size, leading to increased complexity of a subsequent repair.10
It is essential to take care during shaver debridement and continue to respect the tissue during this portion of the procedure. Overly aggressive debridement or nonjudicious use of suction can lead to iatrogenic injury. Shaver selection also plays a significant role in injury prevention, as larger incisor-type shavers can be particularly aggressive when used on normal tissue and can lead to significant iatrogenic tearing. Very light use of suction is usually more than adequate for the diseased tendon to declare itself.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: L.D.F. reports consulting income, Smith & Nephew; research and educational support, Arthrex, Mitek, Smith and Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Video examples utilize right and left shoulders, positioned in the beach chair position, and viewed from the articular and bursal aspects. Useful arthroscopic techniques for the diagnosis and treatment of partial-thickness rotator cuff tears. Key anatomic features that indicate the possible presence of partial tears, selective debridement techniques for improved visualization, and patient extremity positioning/manipulation are addressed. Methods for tear localization and treatment are also shown.
References
- 1.Strauss E.J., Salata M.J., Kercher J. The arthroscopic management of partial-thickness rotator cuff tears: A systematic review of the literature. Arthroscopy. 2011;27:568–580. doi: 10.1016/j.arthro.2010.09.019. [DOI] [PubMed] [Google Scholar]
- 2.Matava M.J., Purcell D.B., Rudzki J.R. Partial-thickness rotator cuff tears. Am J Sports Med. 2005;33 doi: 10.1177/0363546505280213. 1417-1417. [DOI] [PubMed] [Google Scholar]
- 3.Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res. 1990:64–74. [PubMed] [Google Scholar]
- 4.Teefey S.A., Rubin D.A., Middleton W.D., Hildebolt C.F., Leibold R.A., Yamaguchi K. Detection and quantification of rotator cuff tears: Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86:708–716. [PubMed] [Google Scholar]
- 5.Denard P.J., Burkhart S.S. Arthroscopic recognition and repair of the torn subscapularis tendon. Arthrosc Tech. 2013;2:373–379. doi: 10.1016/j.eats.2013.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carroll M.J., More K.D., Sohmer S. The use of an intra-articular depth guide in the measurement of partial thickness rotator cuff tears. Adv Orthop. 2013;2013:959305. doi: 10.1155/2013/959305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lo I.K., Burkhart S.S. The comma sign: An arthroscopic guide to the torn subscapularis tendon. Arthroscopy. 2003;19:334–337. doi: 10.1053/jars.2003.50080. [DOI] [PubMed] [Google Scholar]
- 8.Adams C.R., Brady P.C., Koo S.S. A systematic approach for diagnosing subscapularis tendon tears with preoperative magnetic resonance imaging scans. Arthroscopy. 2012;28:1592–1600. doi: 10.1016/j.arthro.2012.04.142. [DOI] [PubMed] [Google Scholar]
- 9.Lo I.K., Gonzolez D.M., Burkhart S.S. The bubble sign: An arthroscopic indicator of an intratendinous rotator cuff tear. Arthroscopy. 2002;18:1029–1033. doi: 10.1053/jars.2002.36486. [DOI] [PubMed] [Google Scholar]
- 10.Yamaguchi K. Natural history of asymptomatic rotator cuff tears: A longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10:199–203. doi: 10.1067/mse.2001.113086. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video examples utilize right and left shoulders, positioned in the beach chair position, and viewed from the articular and bursal aspects. Useful arthroscopic techniques for the diagnosis and treatment of partial-thickness rotator cuff tears. Key anatomic features that indicate the possible presence of partial tears, selective debridement techniques for improved visualization, and patient extremity positioning/manipulation are addressed. Methods for tear localization and treatment are also shown.