Abstract
This is a technique guide for open anterior capsule reconstruction in unstable native hips due to Ehlers–Danlos syndrome. Ehlers–Danlos syndrome is a connective tissue disease that predisposes an individual to hypermobility of their soft tissues and recurrent subluxations and dislocations of their joints. This may lead to constant instability, guarding of the hip, and subsequent arthritic changes and poor quality of life. We demonstrate anterior capsule reconstruction of the hip using an Achilles tendon allograft performed through a direct anterior approach to the hip (Heuter's approach). This technique guide outlines in detail the surgical steps required to accomplish this reconstructive procedure. Furthermore, a narrated surgical video is provided that clearly depicts the anticipated result of the increased constrained provided to the hip from the anterior capsule reconstruction using an Achilles tendon allograft.
Ehlers–Danlos Syndrome (EDS) affects collagen synthesis, resulting in pathologic connective tissue and joint hypermobility that clinically present as joint subluxations and dislocations.1 Recurrent instability of the hip limits the quality of life of patients due to constant apprehension and chronic pain, and it may predispose them to early joint degeneration.2 Conservative management is the initial treatment; however, in refractory cases, surgical intervention should be considered. Arthroscopic and open capsular plication techniques can be attempted; however, the native pathologic connective tissue increases risk of recurrence. Previously described by our institution, an open caspsuloligamentous reconstruction technique using Achilles tendon allograft has been successful for post-hip arthroscopy instability.3
We present a surgical technique demonstrating an open anterior capsule reconstruction using an Achilles tendon allograft for native hip instability in EDS. We used an allograft to ensure normal collagen is used, as diseased connective tissue of EDS can subsequently stretch and instability can recur. This technique is unique as it is performed on a native hip and shows how the Achilles tendon allograft is fashioned to adopt the dynamic and static stabilizing features of the native iliofemoral ligament. Furthermore, this may be useful for hip arthroscopy surgeons, as it demonstrates a stabilization procedure for the hip that can be used in refractory instability cases post-hip arthroscopy.
The indication for this reconstructive procedure is native hip instability that has failed nonoperative treatment. A trial of activity modification, hip bracing, and gait aids is strongly recommended. The preoperative workup includes a functional history, hip examination focusing on instability, standard hip radiographs, and a magnetic resonance (MR) arthrogram. The MR arthrogram inflates the capsule and helps depict complete defects in the capsule, or patulous capsules, and is recommended over a nonarthrogram study.
Surgical Technique
Room Setup
The room is set up with a flat top radiolucent table to allow for easy intraoperative fluoroscopic images, if needed. A graft table is required for graft preparation.
Specialized Equipment
A direct anterior approach retractor set (Stryker, Kalamazoo, MI) is used to facilitate the capsular exposure (Figs 1 and 2). The reconstruction is performed with an Achilles tendon allograft with the calcaneous tuberosity still attached (Fig 3). Suture anchor choice includes a 5.5-mm suture anchor (CrossFT; ConMed, Utica, NY), which is triple loaded with #2 HiFi sutures and is a biocomposite product. In areas of dense cortical bone such as the lesser trochanter (LT), a 5-mm titanium self-drilling triple-loaded anchor (ThRevo; ConMed) with #2 HiFi sutures can be used. HiFi suture (ConMed) is a high-strength braided nonabsorbable suture. The remaining equipment includes standard orthopedic surgery instrumentation.
Fig 1.
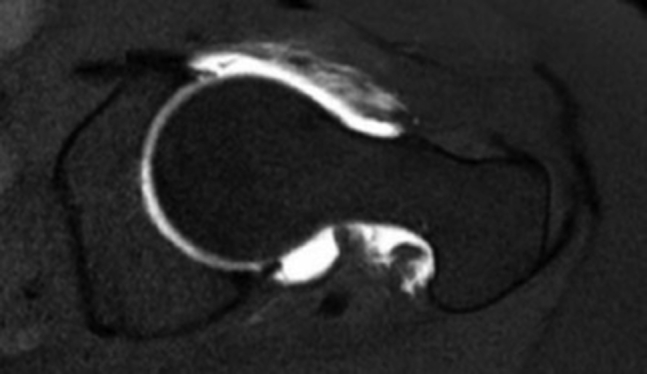
Axial-cut magnetic resonance (MR) arthrogram of the left hip demonstrating a patulous capsule and deficient iliofemoral ligament anteriorly. The anterior capsule is heterogeneous in nature and not a homogenous black band as seen on a normal MR imaging study.
Fig 2.

Stryker direct anterior approach retractor set. From left to right: Standard Cobra, Wide Cobra, Standard Homan, and Curved Homan.
Fig 3.

Stryker retractors. Cobras are blunt (left), and Homans are sharp (right).
Patient Position, Preparation, and Draping
The patient is placed supine on a radiolucent flat top operative table. A dynamic examination of the hip is undertaken preoperatively to allow for a postoperative clinical comparison (Video 1). A bump is placed under the ipsilateral hip to allow extension for easier surgical exposure. All pressure points are padded. The operative leg, foot, groin, and as proximal as the umbilicus is prepped in standard fashion. The operative leg is then draped free to allow for intraoperative hip mobilization.
Approach: Superficial Dissection
We use a direct anterior approach (Hueter's approach) to the hip to provide the capsule exposure and working space. The anterior superior iliac spine is palpated and determines the location of the skin incision (Fig 4). The straight leg is internally rotated, which accentuates the tensor fascia lata (TFL) muscle belly. The incision is based over the TFL muscle belly. The incision can be extended proximally for exposure (Fig 4). The superficial fascia of TFL is identified and cleaned to aid with closure. The superficial fascia of the TFL is divided in line with the skin incision, taking care to protect the lateral femoral cutaneous nerve (LFCN), which lies medial to the fascial incision (Fig 5).
Fig 4.

Type of graft used. Achilles tendon allograft with the calcaneal tuberosity still attached. It originally comes with a large bone block and a single tendinous structure. The bone block is fashioned to a width and length of 2 cm each and a depth of 0.8 cm. The single tendinous structure is split longitudinally 50% of its length into 2 strands starting at the free end (non-bony end) to replicate the iliofemoral ligament (allowing for a Y-configuration). The figures depicting the surgical procedure are in a supine position, on a left hip. Proximal, distal, medial, and lateral are the top, bottom, left, and right of the image, respectively.
Fig 5.
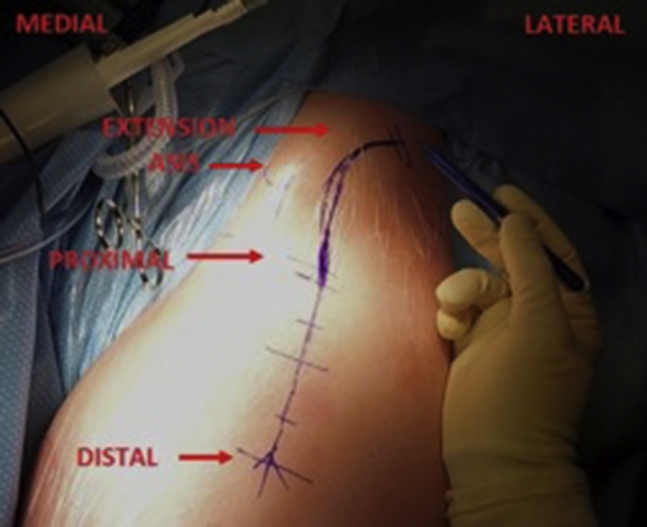
Surgical step 1. Location of the skin incision is 2 finger breadths lateral and 2 finger breadths distal to the anterior superior iliac spine. The tensor fascia lata muscle belly is accentuated with internal rotation of the leg, and the skin incision is centrally based on the muscle belly. Proximal extension above the flexor crease is marked out, which can help with exposure of the anterior inferior iliac spine (AIIS) and the gluteal pillar on the outer table of the pelvis where the graft will be docked. The figures depicting the surgical procedure are in a supine position, on a left hip. Proximal, distal, medial, and lateral are the top, bottom, left, and right of the image, respectively.
Approach: Deep Dissection
The TFL muscle is dissected bluntly off the medial fascia. Retractor placement includes a wide Cobra (Stryker) at the lateral femoral neck, a standard Homan (Stryker) inferolateral to the greater trochanter, and a broad right-angle is used to retract the medial tissue. The ascending branch of the lateral femoral circumflex artery is now visualized and cauterized. The deep investing fascial layer of the TFL is divided. The precapsular fat pad of the hip is visualized and removed. The capsule is exposed with the help of the standard Cobra on the medial femoral neck and the curved Homan over the pelvic brim elevating the iliocapsularis, rectus femoris, and iliopsoas (Fig 6). It is crucial to keep the curved Homan perpendicular to the inguinal ligament to prevent a femoral nerve palsy. Scar tissue on the anterior capsule is anticipated in patients with recurrent dislocations, and development of the appropriate planes with a Cobb elevator is helpful. This completes the anterior capsule exposure. The dissection is carried along the outer table of the pelvis, elevating the TFL off bone (Fig 7). The 3 main anchor points for the allograft are now visualized; outer table of pelvis adjacent to the anterior inferior iliac spine (origin for the graft), adjacent to the lesser trochanter (medial limb of the graft), and the anterior prominence of the greater trochanter crest (lateral limb of the graft).
Fig 6.
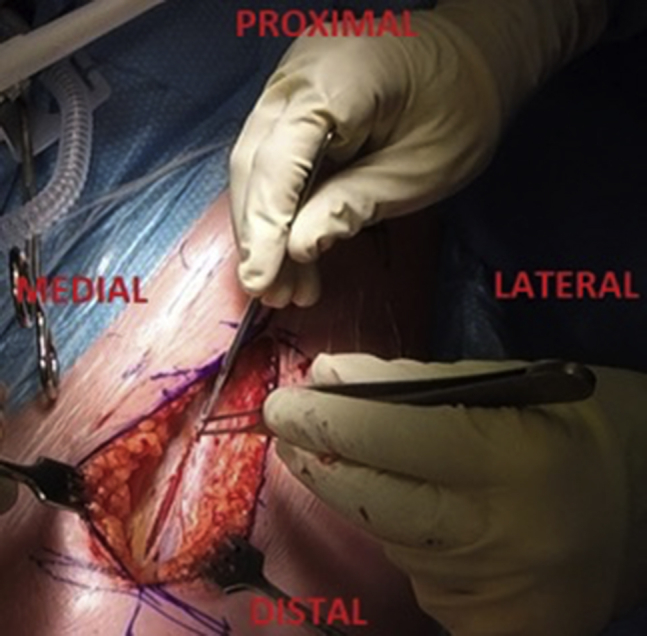
Surgical step 2. Incision of the tensor fascia lata (TFL) superficial fascia is in line with the skin incision. The Hueter's approach through the TFL fascia helps to protect the lateral femoral cutaneous nerve as it lies medial to the superficial fascial incision. The figures depicting the surgical procedure are in a supine position, on a left hip. Proximal, distal, medial, and lateral are the top, bottom, left, and right of the image, respectively.
Fig 7.

Surgical step 3. Stryker direct anterior approach retractor placement to exposure the anterior hip capsule includes the wide Cobra at the lateral femoral neck, the standard Cobra at the medial femoral neck, and the curved Homan over the pelvic brim. The curved Homan needs to stay perpendicular to the inguinal ligament to prevent a femoral nerve palsy. The figures depicting the surgical procedure are in a supine position, on a left hip. Proximal, distal, medial, and lateral are the top, bottom, left, and right of the image, respectively.
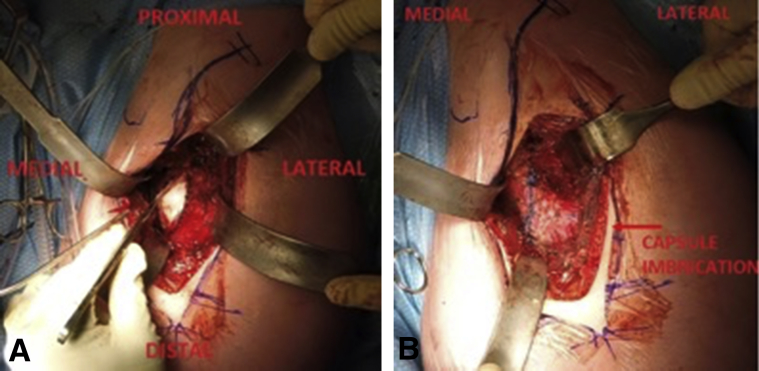
Capsule Imbrication
A new No. 15 scalpel is used to perform a capsule cut running from superolateral to inferomedial, avoiding the cartilage of the femoral head (Fig 8). The capsule is then imbricated in a pants over vest technique using a #1 Vicryl stitch (Fig 8).
Fig 8.
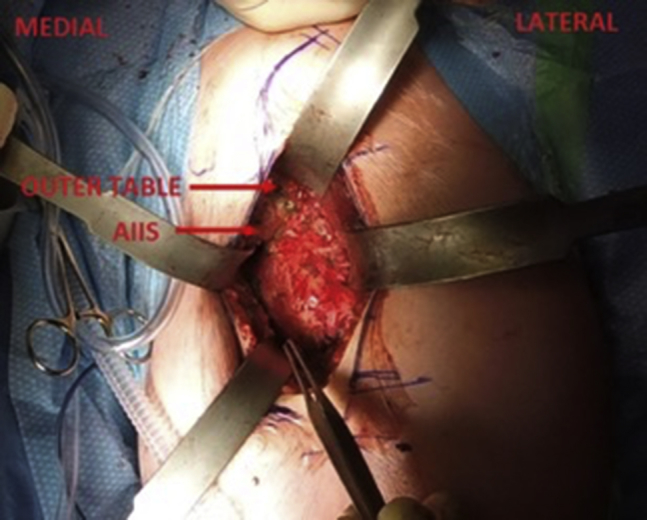
Surgical step 4. Exposure of the anterior inferior iliac spine (AIIS) and outer table of the pelvis. Just adjacent to the AIIS is where the docking site of the graft is prepared. This 2-cm × 2-cm area is decorticated with an oscillating saw until bleeding bone is visualized. The figures depicting the surgical procedure are in a supine position, on a left hip. Proximal, distal, medial, and lateral are the top, bottom, left, and right of the image, respectively.
Graft Preparation
The Achilles tendon allograft is prepared by drilling six 2.5-mm holes in the bone block to allow for horizontal mattress suture passage. The tendinous portion of the graft is divided into 2 equal width longitudinal limbs encompassing 50% of the overall length of the tendon, creating a Y-configuration (Fig 4).
Graft Deployment
The docking sites for the graft were chosen to mimic the native iliofemoral ligament.4 The proximal docking area is located on the outer table of the pelvis just adjacent to the anterior inferior iliac spine abutting the anterolateral acetablulum.4 This 2 × 2-cm area is decorticated using an oscillating saw. A 5.5-mm suture anchor (CrossFT; ConMed) is then deployed in the decorticated docking site in a distally based direction to allow for better pullout strength, a theory borrowed from the shoulder deadman's angle (Fig 9). Each limb of suture in the triple loaded anchor is passed through the bone block to allow tying over the bone block in a horizontal mattress fashion (Fig 10). The allograft limbs are now spun 180° to create the corkscrew phenomenon and reciprocal tightening of the iliofemoral ligament. The medial limb is deployed at the anteroinferior femur just anterior to the LT,4 and finally the lateral limb to the anterior prominence of the greater trochanter crest4 in the same horizontal mattress fashion (Fig 11). Occasionally, a ConMed ThRevo anchor, which is a 5-mm titanium self-drilling anchor, is required for the medial limb deployment as the cortical bone in this location can be very thick. We tension the allograft in 45° of hip flexion and 15° of internal rotation to allow for appropriate tension of the graft. Finally, each limb is oversewn to the capsule using #1 Vicryl stitch to augment the fixation (Fig 12).
Fig 9.
Surgical step 5. The capsule imbrication is an augmentation to the procedure. A superolateral to inferomedial cut in the capsule is made with a new No. 15 scalpel and the femoral head is exposed (left). When performing the capsulotomy, heavy pickups are used to lift the capsule off the surface of the femoral head to avoid iatrogenic damage to the underlying cartilage. The capsule is imbricated with a pants over vest technique using #1 Vicryl suture (right). The figures depicting the surgical procedure are in a supine position, on a left hip. Proximal, distal, medial, and lateral are the top, bottom, left, and right of the image, respectively.
Fig 10.
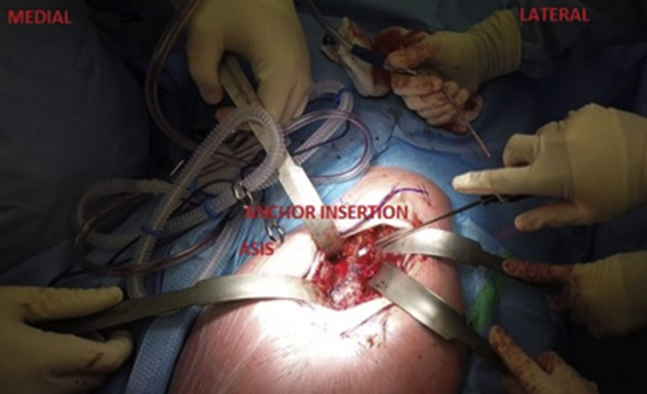
Surgical step 6. Proximal anchor insertion is done at a 45° distal angle at the docking site, just adjacent and lateral to the anterior inferior iliac spine (AIIS). The 45° distal angle of anchor insertion helps with pullout strength. A triple-loaded anchor is used. The figures depicting the surgical procedure are in a supine position, on a left hip. Proximal, distal, medial, and lateral are the top, bottom, left, and right of the image, respectively.
Fig 11.
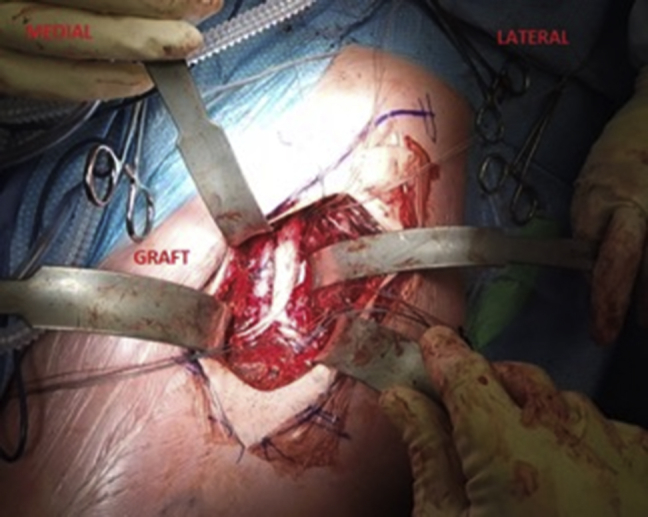
Surgical step 8. The Achilles tendon allograft shown fixed in place by use of proximal, medial, and lateral triple-loaded suture anchors. The Y-limbs are spun 180° to allow for the corkscrew effect and reciprocal tightening of the iliofemoral ligament. The medial suture anchor is positioned just anterior to the lesser trochanter, and the lateral suture anchor is positioned on the anterior prominence of the greater trochanter crest. The limbs are tensioned in flexion and internal rotation of the hip. The wound is then irrigated, and closed in layers starting with the tensor fascia lata fascia, subcutaneous layer, and finally skin. The figures depicting the surgical procedure are in a supine position, on a left hip. Proximal, distal, medial, and lateral are the top, bottom, left, and right of the image, respectively.
Fig 12.
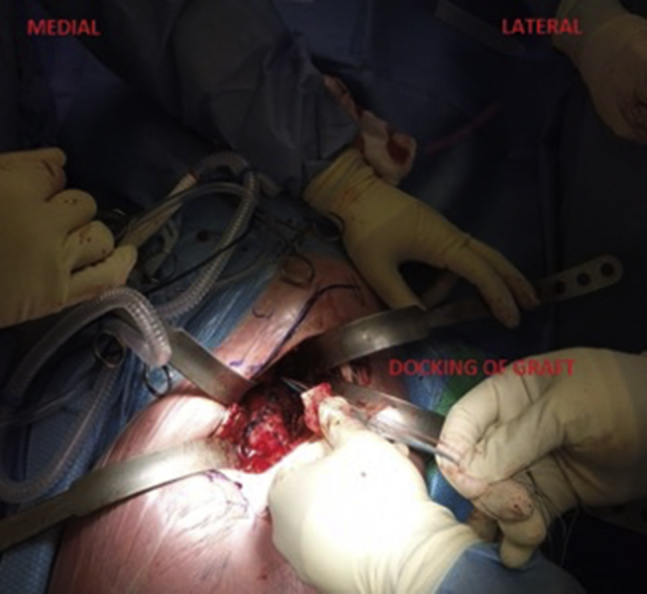
Surgical step 7. The bone block attachment of the Achilles tendon allograft is docked by passing all 6 strands of the triple loaded anchor to allow for horizontal mattress suture fixation over a bone bridge. The figures depicting the surgical procedure are in a supine position, on a left hip. Proximal, distal, medial, and lateral are the top, bottom, left, and right of the image, respectively.
Testing
The graft undergoes clinical testing with range of motion, and the corkscrew phenomenon with reciprocal tightening of the reconstructed iliofemoral ligament is observed (Video 1).
Closure
The wound is irrigated with normal saline to prevent infection and heterotopic ossification formation. We use 3 g of tranexamic acid topically to allow for added hemostasis. Pericapsular local anesthetic is infiltrated for postoperative pain control. The superficial fascia of the TFL is closed in a running fashion with intermittent locking stitches, paying close attention to not capture the LFCN. The wound is then closed as per the surgeon's preference.
Postoperative Examination and Postoperative Rehabilitation
The hip is taken through the same examination as done preoperatively to evaluate and compare the stability of the hip (Video 1). The patient remains touch weight bearing for 6 weeks. Progressive physiotherapy is then started for range of motion. Strengthening begins at 12 weeks.
Discussion
The presentation of native hip instability is rare; however, it can occur in patients with connective tissue disorders. In 2015, Larson et al.5 reported outcomes on 16 patients with EDS-hypermobility type who underwent hip arthroscopy for femoroacetabular impingement and capsular laxity with capsular plication. After a mean follow-up of 45 months, there were significant improvements in all outcome measures, with 1 patient requiring revision arthroscopy for recurrent pain and subjective instability. In the present case, the authors felt that a capsular plication alone would be insufficient, given the recurrent history of symptomatic instability and evidence on MR imaging (MRI) of an attenuated anterior hip capsule. Furthermore, we believe there are limits to arthroscopic management in patients with global capsular insufficiency, especially those with collagen disorders. The use of native collagen for capsular plication in patients with EDS is at greater risk of recurrence. We advocate allograft reconstruction using an open direct anterior technique to reduce the risk of recurrence.
Risks to an open anterior capsule reconstruction of the hip should be mentioned (Table 1). Risks can be divided into immediate and late risks. Due to the open and invasive characteristics of this approach, immediate risks include nerve (lateral femoral cutaneous nerve, femoral nerve), artery and blood loss (ascending branch of the lateral circumflex femoral artery), infection (open nature of the procedure), iatrogenic cartilage injury (during the capsulotomy), scar formation (superficial and deep), and postoperative pain management. Late risks are recurrence of instability, and theoretical overconstraint of the hip leading to early arthritis, akin to the historic procedure of shoulder capsulorrhaphy leading to shoulder arthropathy.
Table 1.
Advantages and Disadvantages for Open Anterior Capsule Reconstruction of the Hip Using an Achilles Tendon Allograft
| Advantages | Disadvantages |
|---|---|
|
|
This technique allows for a step-by-step guide in anterior capsule reconstruction using an Achilles tendon allograft with a calcaneal bone block in situ. The bone block is helpful, as it provides bone on bone healing at the proximal docking site. The Achilles tendon allograft is sturdy, and can be split distally into a Y-configuration to replicate the iliofemoral ligament.
We like to use biocomposite suture anchors to allow for postoperative MRI if necessary. Using metal suture anchors will result in a large metal artifact on MRI and limit the quality and interpretation of the images. However, metal suture anchors can be useful in dense cortical bone areas such as the medial limb anchor site anterior to the LT (Table 2).
Table 2.
Pearls and Pitfalls for Open Anterior Capsule Reconstruction of the Hip Using an Achilles Tendon Allograft
| Pearls | Pitfalls |
|---|---|
|
|
DAA, direct anterior approach; LT, lesser trochanter; TFL, tensor fascia lata.
Hip instability cases invariably have had repetitive subluxations and resultant tissue trauma to the hip. Impressionable scar tissue forms anterior to the capsule, and the reflected head of rectus femoris as well as the iliocapsularis are significantly adhered at this location. Care must be taken to elevate these tissues completely to obtain the proper tissue plane and allow adequate exposure.
Many capsuloligamentous reconstruction techniques have been previously described to address symptomatic instability in both native and non-native hip joints.6, 7, 8, 9 However, the technique in this paper is unique in that using a direct anterior approach to a native hip, the anatomic configuration of the iliofemoral ligament is replicated with an Achilles tendon bone block allograft to turn the original insufficient capsule into a now enhanced reconstructed iliofemoral ligament.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: D.W. is a consultant for Intellijoint. O.R.A. is on the Speakers Bureau for ConMed. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical video on the step-by-step technique for anterior capsule reconstruction using an Achilles tendon allograft performed through a direct anterior approach to a left hip.
References
- 1.Castori M. Ehlers-Danlos syndrome, hypermobility type: An underdiagnosed hereditary connective tissue disorder with mucocutaneous, articular, and systemic manifestations. ISRN Dermatol. 2012;2012:751768. doi: 10.5402/2012/751768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reinstein E., Pariani M., Lachman R.S., Nemec S., Rimoin D.L. Early-onset osteoarthritis in Ehlers-Danlos syndrome type VIII. Am J Med Genet A. 2012;158A:938–941. doi: 10.1002/ajmg.a.35261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yeung M., Khan M., Williams D., Ayeni O.R. Anterior hip capsuloligamentous reconstruction with Achilles allograft following gross hip instability post-arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2017;25:3–8. doi: 10.1007/s00167-016-4258-z. [DOI] [PubMed] [Google Scholar]
- 4.Telleria J.J.M., Lindsey D.P., Giori N.J., Safran M.R. A quantitative assessment of the insertional footprints of the hip joint capsular ligaments and their spanning fibers for reconstruction. Clin Anat. 2014;27:489–497. doi: 10.1002/ca.22272. [DOI] [PubMed] [Google Scholar]
- 5.Larson C.M., Stone R.M., Grossi E.F., Giveans M.R., Cornelsen G.D. Ehlers-Danlos syndrome: Arthroscopic management for extreme soft-tissue hip instability. Arthroscopy. 2015;31:2287–2294. doi: 10.1016/j.arthro.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Chahla J., Dean C.S., Soares E., Mook W.R., Philippon M.J. Hip capsular reconstruction using dermal allograft. Arthrosc Tech. 2016;5:e365–e369. doi: 10.1016/j.eats.2016.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fujishiro T., Nishikawa T., Takikawa S., Saegusa Y., Yoshiya S., Kurosaka M. Reconstruction of the iliofemoral ligament with an artificial ligament for recurrent anterior dislocation of total hip arthroplasty. J Arthroplasty. 2003;18:524–527. doi: 10.1016/s0883-5403(03)00073-1. [DOI] [PubMed] [Google Scholar]
- 8.Trindade C.A.C., Sawyer G.A., Fukui K., Briggs K.K., Philippon M.J. Arthroscopic capsule reconstruction in the hip using iliotibial band allograft. Arthrosc Tech. 2015;4:e71–e74. doi: 10.1016/j.eats.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perets I., Hartigan D.E., Walsh J.P., Chaharbakhshi E., Close M.R., Domb B.G. Arthroscopic capsular reconstruction of the hip with acellular dermal extracellular matrix: Surgical technique. Arthrosc Tech. 2016;5:e1001–e1005. doi: 10.1016/j.eats.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical video on the step-by-step technique for anterior capsule reconstruction using an Achilles tendon allograft performed through a direct anterior approach to a left hip.