Abstract
In large or massive rotator cuff tears, successful repairs are difficult and complication rates are high, because the torn tendon is contracted and the superior capsule is disrupted. Recent studies have shown that superior capsule reconstruction (SCR) in massive irreparable rotator cuff tears results in better clinical scores and preserves stable glenohumeral stability without significant complications. In this article, we propose a simple, efficient SCR technique to reinforce the repair of large or massive rotator cuff tears. For this technique, the long head of the biceps tendon is used as a local autograft for the SCR, therefore eliminating comorbidities related to graft harvesting. The proximal part of the long head of the biceps tendon is transposed posteriorly and fixed onto the footprint as the SCR, which not only can maintain the stability of the glenohumeral joint, but also can preserve the vascular supply to help healing.
In patients with large or massive rotator cuff tears (RCTs), the superior capsule is disrupted. It is a vital structure that maintains the stability and the biomechanical congruence of the superior glenohumeral joint.1 Surgical intervention of large or massive RCTs without superior capsule reconstruction (SCR) results in low healing rates and puts patients at significant risk of complications such as glenohumeral instability and subacromial impingements.2 Studies have shown that SCR in massive irreparable RCTs results in better clinical scores and significant short-term improvements without significant complications.3, 4 Since the introduction of rotator cuff repairs with SCR, different methods of reconstruction have been done by either biologic augmentations or autografts; however, these techniques have obtained mixed results.5, 6 In this study, we propose an SCR technique that can restore glenohumeral stability by using the long head of the biceps tendon (LHBT), which provides closer anatomic attachments to the original superior capsule without sacrificing other autografts. The preliminary results with this technique showed satisfactory clinical outcomes and improved clinical scores (Video).
Surgical Technique
Preoperative Evaluation and Indications
Before their operations, all patients received thorough physical examinations and clinical evaluations to determine the severity of their RCT. All patients with positive physical examination findings of rotator cuff injuries were surveyed using radiographs (anteroposterior and outlet view) and magnetic resonance imaging. After the imaging studies, patients with the following findings were enrolled for this technique: (1) complete tear of anterosuperior region of the rotator cuff; (2) lesion of the subscapularis smaller than Lafosse type II; (3) presence of the LHBT without anterior dislocation; and (4) fatty change in the torn rotator cuff no worse than Goutallier type II.7, 8
Patients with the following conditions were excluded: (1) severe osteoarthritis of the glenohumeral joint or deformity of the humeral head; (2) deltoid muscle atrophy or axillary nerve injury; or (3) passive range of both flexion and abduction motion of <90°. In clinical situations, diagnostic arthroscopy is the last step to confirm that a patient's injuries match previous examinations. During diagnostic arthroscopy, the quality of the LHBT, including the presence of an intra-articular tear and the severity of the SLAP lesion, were assessed to determine whether the patient was suitable for this technique.
Anesthesia and Patient Positioning
Once sedated using general anesthesia, the patient is placed in the beach chair position with the shoulder in 30° abduction and the elbow in 90° flexion. Then, the crucial landmarks of the shoulder and port insertion points are carefully palpated and marked. The shoulder is prepared and draped using strict sterile techniques.
Diagnostic Arthroscopy
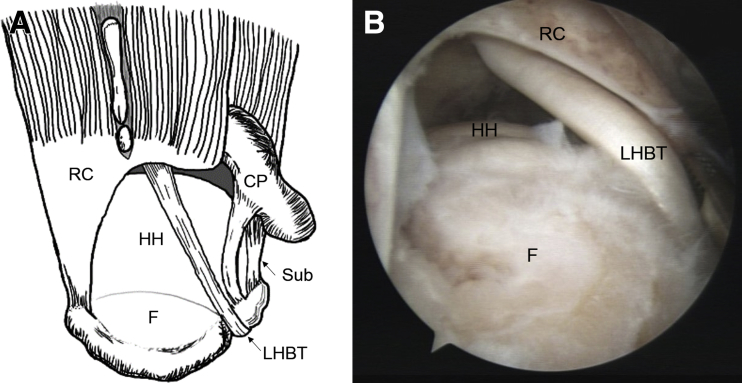
Diagnostic arthroscopy is done using a 30° arthroscopic lens to survey the pattern of subscapularis tear, quality of the LHBT, and condition of the glenohumeral joint. The standard posterior portal (2 cm inferior, 1 cm medial to acromial posterior corner) is placed as the view portal, and the anterior portal is placed as the working portal. We assess the tear pattern of the subscapularis and check for any SLAP or intraarticular biceps lesions using a probe. Patients are deemed unsuitable for this technique if SLAP lesions are worse than type II or there is an intra-articular tear of >30%. After we confirm the LHBT to be acceptable, we shift the arthroscopy to the subacromial space (Fig 1).
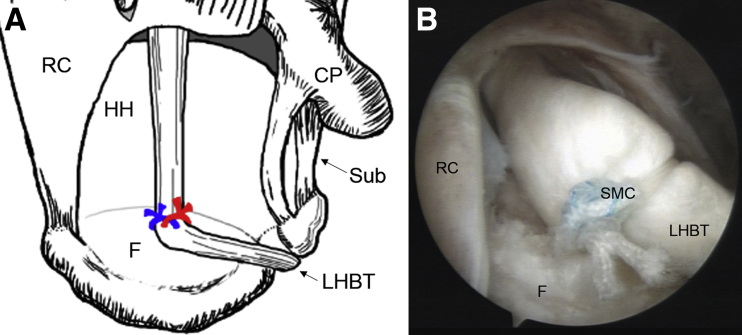
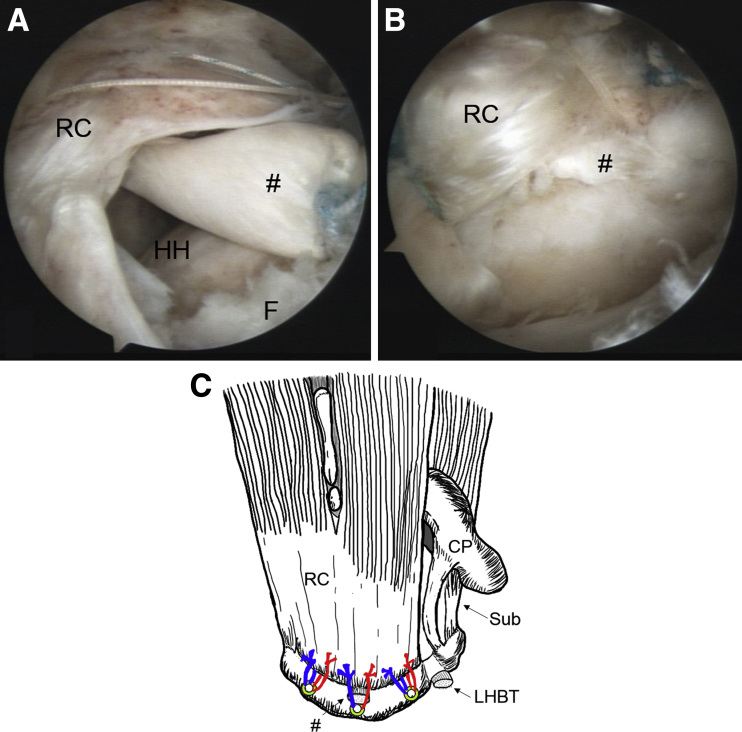
Fig 1.
Diagnostic arthroscopy, standard posterior portal. The patient with right shoulder rotator cuff tear was placed in the beach chair position. The ideal cases for this procedure were complete anterosuperior region tear of the rotator cuff with acceptable LHBT quality (intra-articular LHBT tear <30% and no worse than type II SLAP lesion). Subacromial bursectomy was done as clearly as possible, and the footprint was prepared carefully to expose the cancellous bone bed. The view portal was changed from the standard posterior portal to the posterolateral portal (∼1.0 to 1.5 cm anterior to the posterior corner of the acromial region, just lateral to the acromion). CP, coracoid process; F, footprint of rotator cuff; HH, humeral head; LHBT, long head of the biceps tendon; RC, rotator cuff; Sub, subscapularis.
Subacromial Space Arthroscopy
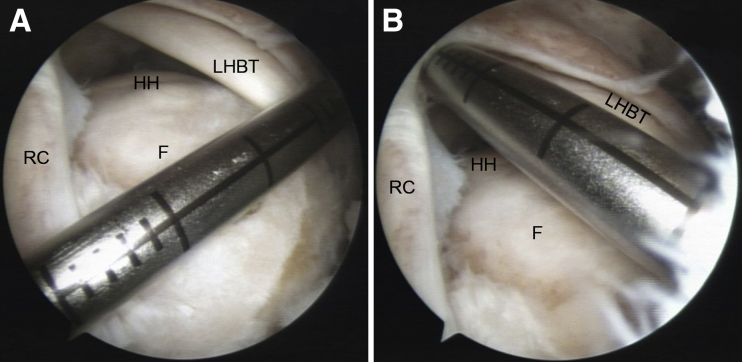
In the subacromial space, the working portal is changed to the lateral portal. A bursectomy is done as clearly as possible using a shaver (3.5-mm Cuda; ConMed), and acromioplasty is done using a burr (4.0-mm Oval Burr; ConMed) if an acromial spur is present. Then, the view portal is changed to the posterolateral portal (∼1.0 to 1.5 cm anterior to the posterior corner of the acromial region, just lateral to the acromion). The tear size of the RCT in the anteroposterior and medial-lateral aspect are measured with a laser-marked device (Fig 2). The adhesive RCT is released superiorly and inferiorly with a shaver and electrocautery device (Saphyre II 90°; Smith & Nephew), and the footprint is prepared carefully by using a shaver or bone cutter to expose the cancellous bone bed while preserving sufficient integrity for anchor placement. Finally, if poor mobility of the LHBT is found, the upper part of the transverse ligament or adhesion is released with an electrocautery device to ensure successful transposition of the LHBT to the middle footprint.
Fig 2.
Measurement of the right torn rotator cuff in the posterior lateral portal. The torn rotator cuff was released superiorly and inferiorly, and the shattered edge was debrided. We used a laser-marked device to measure the tear size in the anteroposterior and medial-lateral aspect. F, footprint of rotator cuff; HH, humeral head, LHBT, long head of the biceps tendon; RC, rotator cuff.
Posterior Transposition of the LHBT as Superior Capsule Repair
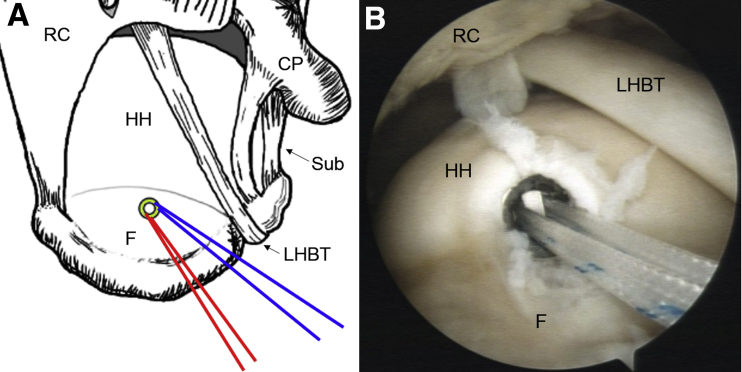
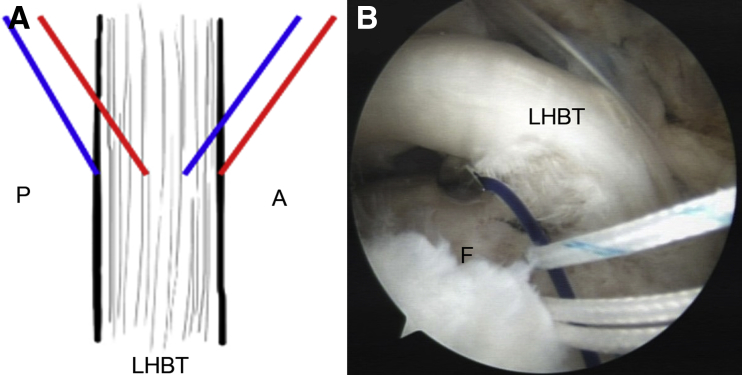
During posterior LHBT transposition, the shoulder is placed in 30° abduction and 10° flexion and the elbow in 90° flexion. A double-loaded suture anchor (5.0-mm TwinFix Ti Suture Anchor; Smith & Nephew) is inserted at the medial (mediolateral aspect) and middle (anteroposterior aspect) footprint (Fig 3). The double-loaded suture anchor has 2 sutures represented by blue and red colored lines in the animated figures. One end of the blue line is passed through the anterior third portion of the LHBT, and the other end is left in the posterior side. One end of the red line is then passed through the posterior third portion of the LHBT, and the other end is put in the anterior side (Fig 4). After that, the posteriorly transposed LHBT is fixed onto the footprint by the double-loaded sutures with Samsung Medical Center (SMC) knots individually (Fig 5). Before the tenotomy, we preserve ∼1 to 1.5 cm of the LHBT distal to the fixation, so the stump can be later sandwiched between the rotator cuff and footprint (Fig 6). If the patient is young or active, a subpectoral tenodesis is performed.
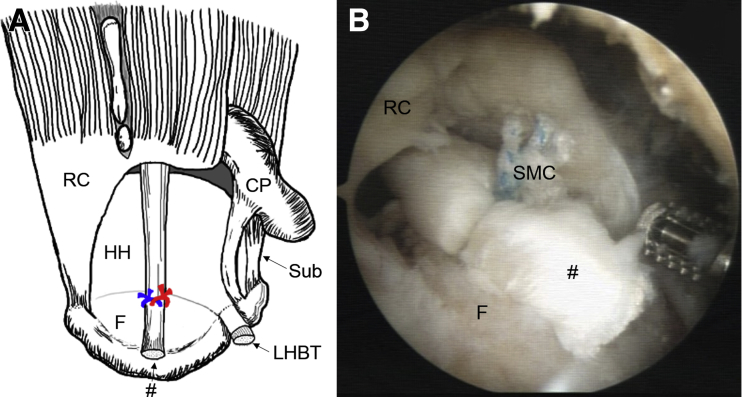
Fig 3.
Preparation for posterior transposition of the right LHBT in the posterior lateral portal. A double-loaded suture anchor was inserted at the center of anteroposterior aspect of the footprint and medial part of the medial-lateral aspect of the footprint (close to the junction of humeral cartilage). CP, coracoid process; F, footprint of rotator cuff; HH, humeral head; LHBT, long head of the biceps tendon; RC, rotator cuff; Sub, subscapularis.
Fig 4.
Preparation for fixation of the posteriorly transposed right LHBT in the posterior lateral portal. The shoulder was placed in 30° abduction and 10° flexion and the elbow in 90° flexion. If poor mobility of the LHBT was found, the upper part of the transverse ligament or adhesion was released to ensure successful posterior transposition of the LHBT to the middle footprint. The double-loaded suture anchor had 2 sutures, represented by blue and red colored lines in the animated figures. Each line passes the anterior and posterior third of the LHBT individually. A, anterior to the LHBT; F, footprint of rotator cuff; LHBT, long head of the biceps tendon; P, posterior to the LHBT.
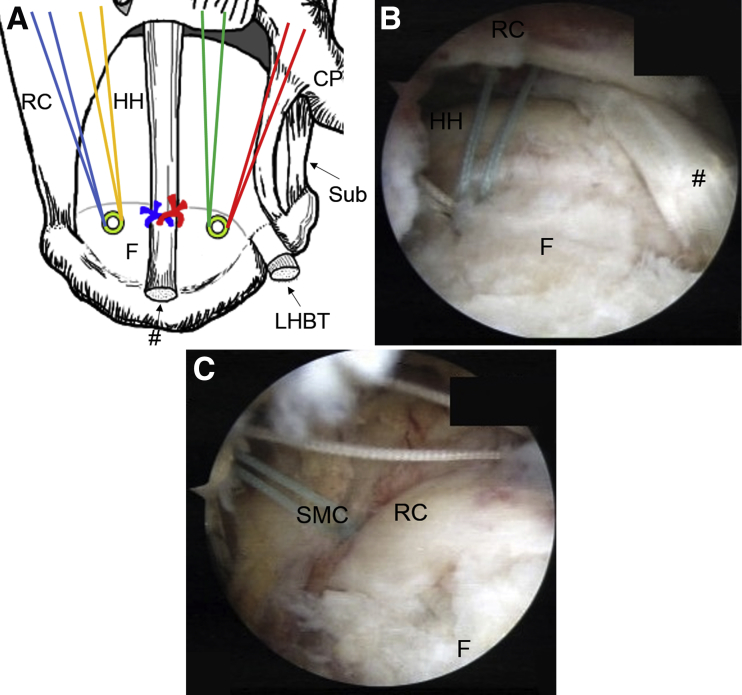
Fig 5.
Fixation of the posteriorly transposed right LHBT in the posterior lateral portal. The posteriorly transposed LHBT was fixed onto the footprint by the double-loaded sutures individually with SMC knots. CP, coracoid process; F, footprint of rotator cuff; HH, humeral head; LHBT, long head of the biceps tendon; RC, rotator cuff; SMC, Samsung Medical Center knot; Sub, subscapularis.
Fig 6.
Tenotomy of the right distal LHBT in the posterior lateral portal. We tenotomized the LHBT and preserved the stump of the LHBT ∼1 to 1.5 cm distal to the fixation. The stump will be sandwiched between the rotator cuff and footprint. #, posteriorly transposed LHBT; CP, coracoid process; F, footprint of rotator cuff; HH, humeral head; LHBT, long head of the biceps tendon; RC, rotator cuff; SMC, Samsung Medical Center knot; Sub, subscapularis.
Rotator Cuff Repair
Rotator cuff repair is performed with either a double-row suture bridge technique or a single-row technique. For the double-row suture bridge technique, 2 double-loaded metal suture anchors (5.0-mm TwinFix Ti Suture Anchor), separated by the posteriorly transposed LHBT, are used as the medial row (Fig 7). The torn rotator cuff is passed by sutures using horizontal mattress methods with a suture-passing device (TruePass Suture Passer, Self-Capture; Smith & Nephew) or a suture hook preloaded with No. 0 PDS II (Ethicon). The free ends of the passed sutures are tied individually with SMC knots. Finally, all passed sutures are crossed and secured with 2 PopLoks (4.5 mm; ConMed) as the lateral row (Fig 8). For the single-row suture technique, a double-loaded suture anchor is placed on the lateral side of the previously transposed LHBT. The sutures are passed through the stump of the transposed LHBT and then through the torn rotator cuff. The other 2 or more double-loaded metal suture anchors, also separated by the transposed LHBT, are used to repair the rotator cuff using a single-row technique (Fig 9). Regardless of which method is used for rotator cuff repair, the LHBT stump is sandwiched between the rotator cuff and the footprint (Table 1).
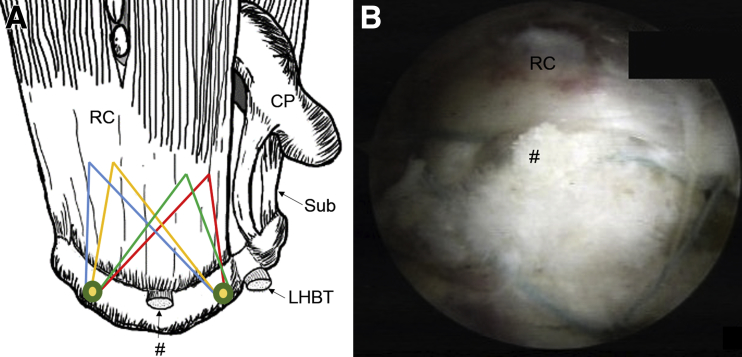
Fig 7.
The right shoulder rotator cuff repaired by the double-row suture bridge technique in the posterior lateral portal. (A) Two double-loaded suture anchors were inserted onto the anterior and posterior sides of the posteriorly transposed LHBT as the medial row for suture bridge. (B) All sutures were passed through the torn rotator cuff. (C) The free ends of the passed sutures were tied individually with SMC knots. #, posteriorly transposed LHBT; CP, coracoid process; F, footprint of rotator cuff; HH, humeral head; LHBT, long head of the biceps tendon; RC, rotator cuff; SMC, Samsung Medical Center knot; Sub, subscapularis.
Fig 8.
Final construct of the double-row suture bridge technique for rotator cuff repair with posteriorly transposed LHBT as SCR. All passed sutures were crossed and secured with 2 PopLok (4.5 mm; ConMed) as the lateral row. The stump of the posteriorly transposed LHBT was secured and sandwiched by the repaired rotator cuff and footprint. #, posteriorly transposed LHBT; CP, coracoid process; LHBT, long head of the biceps tendon; RC, rotator cuff; SCR, superior capsule reconstruction; Sub, subscapularis.
Fig 9.
Finial construct of the single-row suture technique for right shoulder rotator cuff repair with posteriorly transposed LHBT as SCR. (A) A double-loaded suture anchor was placed on the lateral side of the transposed LHBT. The sutures were passed through the stump of the posteriorly transposed LHBT and then passed through the torn rotator cuff. Two or more double-loaded suture anchors separated by the transposed LHBT were used to repair the rotator cuff by single-row technique. (B,C) The stump of the posteriorly transposed LHBT was secured and sandwiched by repaired rotator cuff and footprint. #, posteriorly transposed LHBT; CP, coracoid process; F, footprint of rotator cuff; HH, humeral head; LHBT, long head of the biceps tendon; RC, rotator cuff; Sub, subscapularis.
Table 1.
Pearls and Pitfalls of Critical Surgical Steps
| Surgical Step | Pitfalls | Pearls |
|---|---|---|
| Assessment of the glenohumeral joint | A patient with GH joint OA worse than expected should be excluded. | In patients with severe GH joint OA, in addition to an RCT repair, the source of the OA must be treated to achieve a satisfactory outcome. |
| RCT repair will not relieve pain or improve stability if the main cause of pain and instability is a labral tear. | Labral examination should be done to check if a Bankart lesion or posterior labral tear is present, after which repairs should be done. | |
| Assessment of the LHBT | Poor mobility of the LHBT due to insufficient release from adhesive tissue or transverse ligament | LHBT tears should be checked carefully for proper release of adhesion. |
| Fixation of the LHBT | LHBT injury caused by repeated passes of suture wires through the anterior third and posterior third of the LHBT | Suture wires should be passed through the LHBT only when the correct position is confirmed to avoid LHBT injury. |
| Insertion of medial anchors | Improper position of the anchor may cause anchor pullout, iatrogenic fractures, or improper repair of torn rotator cuff. | Both medial anchors should be evenly spaced to ensure sufficient coverage of the footprint of the RC after passing suture wires through the RCT. |
| Passing suture wires from medial anchors through the RCT | Progressive RCT is caused by repeated attempts or poor choice of passing area. | Passing the suture wires evenly through the plain of an RCT may reduce the chance of extra tears because the pulling force can be evenly dispersed into each wire. |
| Cross tie the medial suture wires with lateral row PopLok | Poor planning of the PopLok will cause incomplete coverage of the footprint and a dog-ear formation. | Settling the lateral row of the suture bridge on top of the transposed LHBT can reinforce the LHBT fixation. |
GH, glenohumeral joint; LHBT, long head of the biceps tendon; OA, osteoarthritis; RC, rotator cuff; RCT, rotator cuff tear.
Postoperative Care
After the operation, the shoulder is immobilized with an abductor brace for 4 weeks. During this time, only active motion of the hand and wrist is allowed. After 4 weeks, passive motion of the shoulder and elbow is allowed. Active motion of the shoulder is allowed at month 3 after the operation, and at month 6, the patient may participate in sports requiring overhead motion.
Discussion
The importance of the superior capsule in glenohumeral stabilization has been clearly stated. SCR in a massive RCT is crucial to prevent upward translation and maintain a constant restraint on the glenohumeral joint.1, 4, 9 Our technique effectively uses the bicep tendon as an autograft without donor site morbidity. The biceps tendon can be easily transposed from the intra-articular space without much of a challenge, and the process does not require extra incisions for extra portals. Furthermore, tenotomy of the distal bicep tendon may relieve shoulder pain caused by biceps tendon issues that coexist with the RCT, and postoperative pain from the bicep tendon can also be avoided.10, 11
Sufficient nutrient and vascular supplies are important for tenocyte growth and healing of the torn tendon. Besides the blood supply from the bone bed of the footprint, in this technique, the transposed LHBT provides extra supplies of nutrient and blood for healing of RCT.12, 13 Biomechanically, this technique acts as a superior capsule to provide a constant superior constraint and maintain a stable glenohumeral fulcrum. The biomechanical study by El-Shaar et al.14 of SCR with an LHBT autograft has been proven to be equivalent and potentially even stronger than SCR with a tensor fascia lata autograft for the prevention of superior humeral migration. The biceps transposed into the greater tuberosity relieves the upward tension of the shoulder, providing a tensionless repair of the RCT and thus preventing possible subacromial impingement syndrome in patients with superior migration (Table 2).
Table 2.
Advantages and Disadvantages of SCR by Posteriorly Transposed LHBT
| Advantages |
| 1. This technique can be performed in reparable or irreparable RCTs. |
| 2. The LHBT is a local autograft; the patient will not have donor site morbidity. |
| 3. All procedures are done on the same shoulder, thus reducing operation time and risk of infection. |
| 4. Preserved vascular supply of the transposed LHBT may improve healing progression of the RCT repair. |
| 5. There is no extra cost for an allograft or artificial graft. |
| 6. There is minimal use of suture anchor, for lower cost. |
| Disadvantages |
| 1. Popeye-sign deformity or biceps cramping pain caused by tenotomy of the LHBT is possible. |
| 2. This technique is not available to patients with poor-quality LHBTs. |
| 3. This technique is not available for larger subscapularis tears. |
LHBT, long head of biceps tendon; RCT, rotator cuff tear; SCR, superior capsule reconstruction.
Upon reviewing techniques related to rotator cuff repair with SCR, we found 2 published techniques that also yielded improved outcomes. The first technique was published by Boutsiadis et al.15 As in our technique, proximal LHBTs were transposed posteriorly, and tenotomy was done distally. Boutsiadis et al.’s technique was limited to irreparable RCTs, whereas our technique can be used for large to massive RCTs. In Boutsiadis et al.’s work, the LHBT was transposed to cover the anterior footprint and was repaired side-to-side with the residual rotator cuff.15 In our technique, the posteriorly transposed LHBT was sandwiched between the repaired rotator cuff and the footprint, and the LHBT was not fixed anterior to the repaired rotator cuff.
Another technique was reported by Kim et al.16 Both methods transpose LHBT to the middle of the footprint as SCR for reinforcement of both reparable and irreparable RCTs, also LHBT tenotomy was performed distally. However, there are still some differences between our methods and others in terms of the fixation methods and the order in which the transposed LHBT is managed. For example, Kim et al.16 fixed the transposed LHBT with 2 suture anchors, proximally and distally. In our technique, we also fix the transposed LHBT both proximally and distally, but we use a suture anchor for the proximal fixation. After finishing the rotator cuff repair, the transposed LHBT distal stump is pressed by the repaired rotator cuff. We do not need another suture anchor for distal fixation of the transposed LHBT, and we obtain an effect similar to that of Kim et al.16 The other difference is the LHBT fixation methods. Kim et al.16 use a lasso-loop tie and 2 more wraparound ties for LHBT fixation. However, we fix the LHBT by passing through both the anterior and posterior thirds of the LHBT and then tying both loops individually. Our technique does not induce longitudinal tears of the LHBT and may be easier than lasso-loop methods (Table 3).
Table 3.
Comparison of Techniques
| Item | Our Technique | Kim et al.16 | Boutsiadis et al.15 |
|---|---|---|---|
| Order of critical steps | 1. Insertion of suture anchor for LHBT fixation at the medial and middle part of the footprint | 1. Insertion of suture anchor for LHBT fixation at the lateral and middle part of the footprint | 1. Insertion of suture anchor for LHBT fixation at the lateral and anterior part of the footprint |
| 2. Fixation of LHBT by passing suture wires through both the anterior and posterior third of the LHBT | 2. Fixation of LHBT with a lasso-loop tie and 2 more wraparound ties | 2. Fixation of LHBT with a lasso-loop tie | |
| 3. Tenotomy of LHBT | 3. Insertion of medial anchor for another LHBT medial fixation using the lasso-loop technique | 3. Tenotomy of LHBT | |
| 4. RCT repaired by single-row or suture bridge techniques | 4. Tenotomy of LHBT | 4. Repair of RCT with single-row or suture bridge techniques | |
| 5. RCT repaired by delaminated double row or suture bridge | 5. Side-to-side repair of rotator cuff and transposed LHBT | ||
| LHBT fixation | Medial and lateral | Medial and lateral | Lateral |
| Method of LHBT fixation | Passing through both the anterior and posterior thirds of the LHBT and then tying both loops individually | A lasso-loop tie and 2 more wraparound ties | A lasso-loop tie |
| Longitudinal tear of fixed LHBT | No | No | No |
| Management of distal to fixation of LHBT | Tenotomy or subpectoral tenodesis | Tenotomy | Tenotomy |
| Transposition of LHBT | Sandwiched between the repaired rotator cuff and the footprint | Sandwiched between the repaired rotator cuff and the footprint | Anterior to repaired rotator cuff |
| Configuration of RCT repair | 1. For a reparable tear, suture bridge or single-row techniques depending on the tear size | 1. For delaminated tears, a separate double-row repair or separate bridge repair | 1. Tension-free partial repair RCT and side-to-side margin repair of the rotator cuff with the LHBT |
| 2. For irreparable tear, a partial repair is acceptable | 2. For irreparable tear, a partial repair is acceptable | ||
| 3. Double row for reparable RCT |
LHBT, long head of biceps tendon; RCT, rotator cuff tear.
The disadvantages and limitations of this technique revolve around the quality of the LHBT and the possible complications from tenotomy of the LHBT. The quality of the intra-articular LHBT limits the use of this technique, so patients with complete rupture or partial tears >30% of intra-articular biceps are not suitable candidates. Tenotomy of the LHBT may result in reduced force in elbow flexion and supination, the popeye-sign deformity, and painful cramps in the biceps. However, Hufeland et al.17 concluded in their prospective randomized study that there were no significant differences in terms of elbow flexion and forearm supination force between LHB tenodesis and tenotomy. Their findings additionally showed a nonsignificant trend toward a higher rate of popeye-sign deformities after biceps tenotomy.17 The outcomes of tenotomy and tenodesis are still controversial, and further studies are required. We believe this technique could bring promising clinical outcomes with fewer complications; however, more studies with a larger patient population are required to fully assess the efficacy of this technique.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video shows the operative procedure for arthroscopic rotator cuff repair with posteriorly transposed LHBT as SCR. The video shows the critical steps of the technique, including LHBT transposition, LHBT tenotomy, rotator cuff repair, and the final construct of the double-row suture bridge technique for rotator cuff repair with posteriorly transposed LHBT as SCR. LHBT, long head of the biceps tendon; SCR, superior capsule reconstruction.
References
- 1.Adams C.R., DeMartino A.M., Rego G., Denard P.J., Burkhart S.S. The rotator cuff and the superior capsule: Why we need both. Arthroscopy. 2016;32:2628–2637. doi: 10.1016/j.arthro.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 2.Galatz L.M., Ball C.M., Teefey S.A., Middleton W.D., Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J. Bone Joint Surg Am. 2004;86:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Mihata T., McGarry M.H., Pirolo J.M., Kinoshita M., Lee T.Q. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am J Sports Med. 2012;40:2248–2255. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 4.Mihata T., Lee T.Q., Hasegawa A. Superior capsule reconstruction for reinforcement of arthroscopic rotator cuff repair improves cuff integrity. Am J Sports Med. 2019;47:379–388. doi: 10.1177/0363546518816689. [DOI] [PubMed] [Google Scholar]
- 5.Mori D., Funakoshi N., Yamashita F. Arthroscopic surgery of irreparable large or massive rotator cuff tears with low-grade fatty degeneration of the infraspinatus: patch autograft procedure versus partial repair procedure. Arthroscopy. 2013;29:1911–1921. doi: 10.1016/j.arthro.2013.08.032. [DOI] [PubMed] [Google Scholar]
- 6.Anley C.M., Chan S.K., Snow M. Arthroscopic treatment options for irreparable rotator cuff tears of the shoulder. World J Orthop. 2014;5:557–565. doi: 10.5312/wjo.v5.i5.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lafosse L., Jost B., Reiland Y., Audebert S., Toussaint B., Gobezie R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am. 2007;89:1184–1193. doi: 10.2106/JBJS.F.00007. [DOI] [PubMed] [Google Scholar]
- 8.Goutallier D., Postel J.M., Bernageau J., Lavau L., Voisin M.C. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994:78–83. [PubMed] [Google Scholar]
- 9.Mihata T., Lee T.Q., Watanabe C. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 10.Meeks B.D., Meeks N.M., Froehle A.W., Wareing E., Bonner K.F. Patient satisfaction after biceps tenotomy. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117707737. 2325967117707737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCrum C., Alluri R., Batech M., Mirzayan R. Long head of the biceps tenotomy and tenodesis: Does technique, location, or implant influence outcomes and complications? Arthroscopy. 2017;33:e11. [Google Scholar]
- 12.Christoforetti J.J., Krupp R.J., Singleton S.B., Kissenberth M.J., Cook C., Hawkins R.J. Arthroscopic suture bridge transosseus equivalent fixation of rotator cuff tendon preserves intratendinous blood flow at the time of initial fixation. J. Shoulder Elbow Surg. 2012;21:523–530. doi: 10.1016/j.jse.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 13.Cheng N.M., Pan W.R., Vally F., Le Roux C.M., Richardson M.D. The arterial supply of the long head of biceps tendon: Anatomical study with implications for tendon rupture. Clin Anat. 2010;23:683–692. doi: 10.1002/ca.20992. [DOI] [PubMed] [Google Scholar]
- 14.El-Shaar R., Soin S., Nicandri G., Maloney M., Voloshin I. Superior capsular reconstruction with a long head of the biceps tendon autograft: A cadaveric study. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118785365. 2325967118785365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boutsiadis A., Chen S., Jiang C., Lenoir H., Delsol P., Barth J. Long head of the biceps as a suitable available local tissue autograft for superior capsular reconstruction: “The Chinese Way.”. Arthrosc Tech. 2017;6:e1559–e1566. doi: 10.1016/j.eats.2017.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim Y.S., Lee H.J., Park I., Sung G.Y., Kim D.J., Kim J.H. Arthroscopic in situ superior capsular reconstruction using the long head of the biceps tendon. Arthrosc Tech. 2018;7:e97–e103. doi: 10.1016/j.eats.2017.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hufeland M., Wicke S., Verde P.E., Krauspe R., Patzer T. Biceps tenodesis versus tenotomy in isolated LHB lesions: A prospective randomized clinical trial. Arch Orthop Trauma Surg. 2019;139:961–970. doi: 10.1007/s00402-019-03136-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video shows the operative procedure for arthroscopic rotator cuff repair with posteriorly transposed LHBT as SCR. The video shows the critical steps of the technique, including LHBT transposition, LHBT tenotomy, rotator cuff repair, and the final construct of the double-row suture bridge technique for rotator cuff repair with posteriorly transposed LHBT as SCR. LHBT, long head of the biceps tendon; SCR, superior capsule reconstruction.