Abstract
Abductor tendon tears are one of the common causes of recalcitrant laterally based hip pain and dysfunction. In most cases, abductor tendon tears are associated with chronic nontraumatic tearing of the gluteus medius tendon. Restoring abductor function of the hip by primary repair of the gluteus medius tendon has been reported to have good and excellent outcomes. However, primary repair might not be as effective for chronic detachment of the gluteus medius tendon with a wide separation from the femoral footprint or severe tendon loss. The lack of tendinous foot for repair and the intrinsically degenerative condition of the tendon may create high tension at the repair site thereby predisposing to surgical failure. We believe that the use of soft-tissue allograft from the Achilles tendon or human dermal allograft may help strengthen the surgical site. We describe a superior gluteal reconstruction technique that is suitable for cases with abductor tendon tear with severe tendon loss.
Abductor tendon tears have been described as the “rotator cuff tear of the hip” and increasingly are being recognized as one of the causes of greater trochanteric pain syndrome (GTPS).1 Abductor tendon pathology is more commonly reported in 40- to 60-year-old women.2 Symptoms include lateral hip pain, local tenderness, and abductor weakness that is unresponsive to nonsurgical management. Three clinical presentations have been described. The most common presentation is a chronic nontraumatic tear of the anterior fibers of the gluteus medius tendon, which is seen in this patient. The other presentations are (1) abductor tendon tears that are found coincidentally in femoral neck fractures or osteoarthritis of the hip and (2) abductor tendon avulsion following total hip arthroplasty performed through an anterolateral or transgluteal approach.2
The severity of the abductor tendon tear can be variable.2, 3 The severity may range from a small undersurface tear with minimum muscular atrophy to a massive tear with profound retraction and muscle atrophy. Several treatment options have been proposed for the treatment of the abductor tendon tear based on the size, degree of tendon retraction, and muscle atrophy. Good-to-excellent functional results have been described for primary repair with open or endoscopic techniques for partial- or full-thickness tears with minimal muscle atrophy.4, 5, 6, 7, 8, 9, 10, 11 Gluteus maximus muscle transfer also has been used for abductor tendon tears with advanced muscle atrophy, and this technique also has been done occasionally with the addition of the tensor fascia lata.12, 13 Technical descriptions for repair of abductor tendon tear with severe tendon loss is lacking. The purpose of this report is to describe a superior gluteal reconstruction for abductor tendon tears with severe tendon loss and atrophy.
Surgical Technique
For this procedure, patients are placed in a lateral decubitus position with a slight hip abduction and knee flexion. All bony prominences are padded and a pneumatic compression device is placed on the healthy leg. The operating side is draped with sterile technique that allows free mobilization of the limb. The greater trochanter is identified. A direct lateral approach is used with skin incision centered over the greater trochanter approximately 6 to 8 cm in length (Fig 1). An interval is developed between subcutaneous tissue and the underlying iliotibial (IT) band. The IT band is split longitudinally in line with its fibers to allow entry into the peritrochanteric space. Once in the peritrochanteric space, a trochanteric bursectomy is performed. Vastus ridge and lateral facet of the greater trochanter are then identified, with the hip rotated internally and externally to evaluate the gluteus medius and gluteus minimus insertion sites, respectively.
Fig 1.
Illustration of a right hip in the supine position demonstrating an outline of skin incision for direct lateral approach (red dotted line). The skin incision is located over the center of the greater trochanter (black dotted line). The skin incision length is approximately 6 to 8 cm.
The torn aspect of the gluteus medius and minimus tendon is then identified (Video 1, Fig 2). The devitalized tissue at the tendon edge is debrided while preserving the tendon as much as possible due to short length of the residual tendon. If the tendon is retracted, adequate mobilization of the tendon is important to create a tension-free repair environment. Blunt dissection of scar tissue can be performed between the gluteus medius and the gluteus maximus muscles, as well as between the tensor fascia lata, and the gluteus minimus to mobilize the tendons. The superior gluteal neurovascular bundle should be avoided by doing the superior dissection at least 3 cm from the tip of the greater trochanter. The gluteus minimus muscle is then elevated from the anterior aspect of the capsule and ilium. The remaining soft tissue remnants on the footprint can then be removed using a rongeur to establish a bony contact surface. A 5.5-mm round burr is used to perform decortication at the footprint to form a bleeding cancellous surface. It should be noted that the gluteus medius tendon has 2 distinct insertion sites on the greater trochanter. The posterior part of the gluteus medius inserts onto the superior–posterior facet and the central portion and all of the anterior portion inserts onto the lateral facet. The gluteus minimus inserts via its long head onto a distinct facet medial to the insertion of the gluteus medius and via a reflection onto the capsule.14 Repair techniques seek to replicate this anatomy.
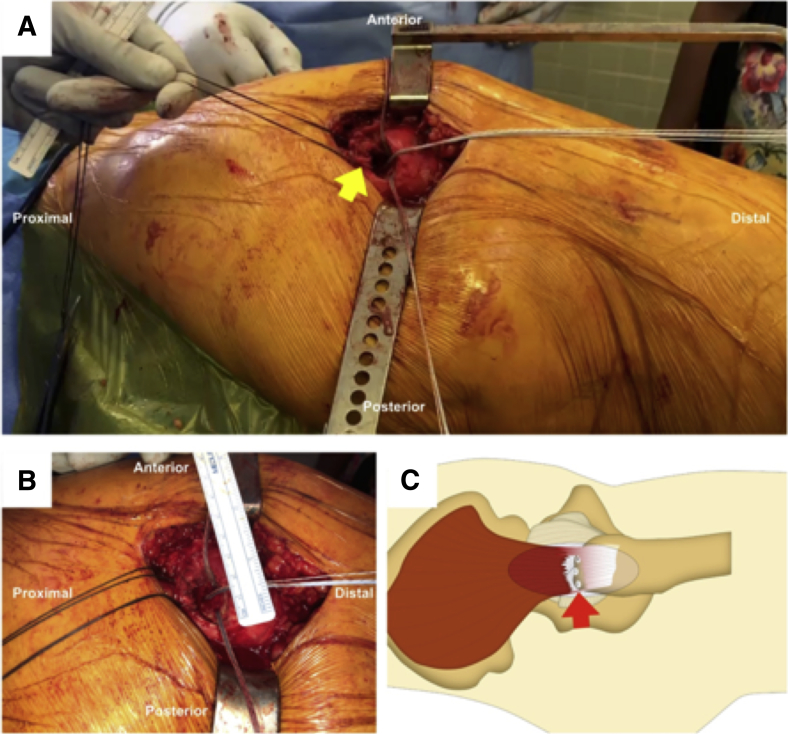
Fig 2.
(A) Image of a right hip of a patient positioned in the lateral decubitus position of the right hip demonstrating the avulsed section of the gluteus medius tendon (yellow arrow). (B) Image of the same right hip with the size of the full-thickness tear being measured. (C) Illustration of a right hip in the supine position demonstrating the location of the tendon defect at the musculotendinous junction (red arrow).
For the repair in the technique demonstrated in Video 1, a double row fixation with 4.5-mm biocomposite suture anchors containing double-loaded No. 2 ultrahigh molecular weight polyethylene braided sutures (BioComposite Corkscrew; Arthrex, Naples, FL) are used (Video 1). The suture anchors are placed in the lateral facet and superoposterior facet near the medial border of the footprint (Video 1, Fig 3). The number of the suture anchors depends on the size of the tear. To reinforce the repair, a fresh-frozen Achilles tendon allograft or acellular human dermal allograft (GRAFTJACKET; Wright Medical Technology, Arlington, TN) supplement of 2- to 3.3-mm thickness and 5 × 5-cm size is used (Fig 4).
Fig 3.
(A) Image of a right hip of a patient positioned in the lateral decubitus position demonstrating the large full-thickness avulsion of the right gluteus medius tendon (yellow arrow) proximal to the lateral facet of the greater trochanter (GT). The 4.5-mm biocomposite suture anchors (BioComposite Corkscrew; Arthrex) containing double-loaded No. 2 ultrahigh molecular weight polyethylene braided sutures are placed in the lateral facet and superoposterior facet near the medial border of the footprint (white dotted line). (B) Image of the same right hip demonstrating a small remaining defect (yellow arrows) between the tendon edge and the footprint after the application of traction sutures.
Fig 4.
Image of a fresh-frozen Achilles tendon allograft that is used for augmentation and close the interval between the avulsed tendon edge and the footprint. It is important to ensure that the graft is larger than the size of the defect. In this particular graft, size is approximately 5 × 5 cm, which is larger than defect measuring 2.5 × 2 cm.
The graft is placed over the tendon defect and greater trochanter. The sutures are passed using a free needle through the proximal part of the tendon and the overlying graft in horizontal mattress fashion (Video 1, Fig 5). Before knot tying, the hip is placed in 20° of abduction, neutral to slightly internal rotation using a Mayo stand. After knot tying, the tendon edge is approximated to the medial edge of the footprint. Combination with the graft is performed, which helps reinforce the repair strength and prevent suture pullout. The free ends of the sutures are then placed through a self-punching PEEK (polyetheretherketone) knotless anchor (SwiveLock suture anchor; Arthrex) approximately 2 to 3 cm distal and lateral to the medial-row anchors (Video 1, Fig 6). This double-row repair allowed broad area for graft compression to the osseous bed (Video 1, Fig 7). After this is completed, the integrity of the repair is confirmed, and the IT band is closed.
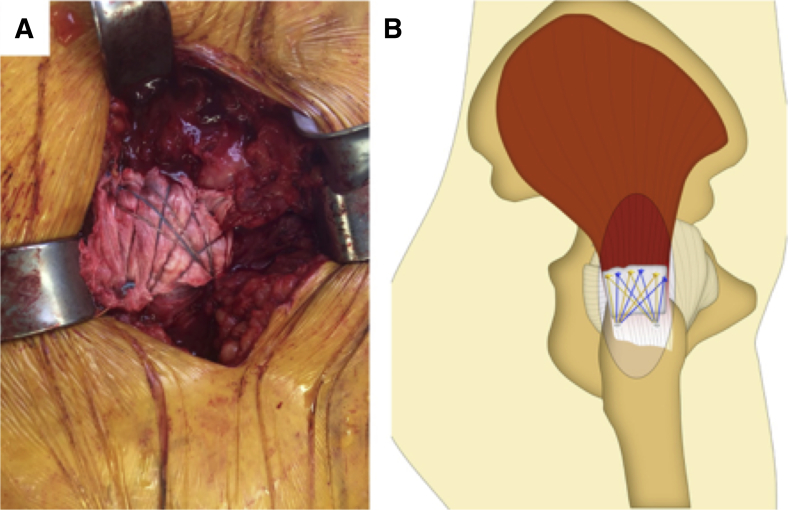
Fig 5.
The image (A) and illustration (B) of a right hip of a patient positioned in the lateral decubitus position demonstrating an Achilles tendon allograft (yellow arrow) placed over the tendon defect and the greater trochanter. The sutures are passed using free needle through the proximal tendon and the overlying graft in horizontal mattress fashion.
Fig 6.
The images of a right-sided hip of a patient positioned in the lateral decubitus position demonstrating 2 lateral row anchors being placed using free ends of the sutures placed through a self-punching PEEK knotless anchor (SwiveLock suture anchor; Arthrex) approximately 2 to 3 cm distal and lateral to the medial-row anchors. The first anchor is shown in (A) and the second anchor is shown in (B).
Fig 7.
The image (A) and illustration (B) of right hip of a patient positioned in the lateral decubitus position demonstrating the final view of the double-row suture repair with superior gluteal reconstruction using Achilles tendon allograft. This allows for broad area graft compression to the osseous bed and complete closure of the defect.
Postoperatively, the patient is instructed to use a continuous passive motion device set at 30° to 70° of flexion, which is increased by 5° increments until 0° to 90° is achieved 2 weeks after surgery. Partial weight bearing is continued with 20-lb flat-foot for 8 weeks, and no active abduction or passive adduction. Weight bearing as tolerated is allowed by 9 weeks and full weight bearing without assistive devices by 12 weeks.
Discussion
GTPS is becoming a more recognized cause of lateral hip pain, particularly in middle-aged women. These patients usually present with lateral hip pain and weakness with abduction that worsens in the lateral decubitus position and movements such as walking.2 Abductor tendon tear is one of the causes of GTPS associated with abductor weakness.
The etiology of the chronic nontraumatic tears of the anterior fibers of the gluteus medius tendon appears to be secondary to a degenerative process similar to rotator cuff tears of the shoulder.3 Most tears begin in the central fibers of the gluteus medius tendon insertion and typically progress in both posterior and inferior directions, to involve the superior fibers and anterior fibers of the gluteus medius/long head of the gluteus minimus, respectively.2
In case of large gluteus medius tear with severely compromised tendon without muscle atrophy, primary repair remains a challenge due to chronic nature of these tears and subsequently limited tendon excursion for repair. Fehm et al.15 performed 7 abductor reconstructions with an Achilles tendon allograft with a calcaneal bone block attached to the greater trochanter in patients with abductor muscle deficiency secondary to avulsion of the greater trochanter or the abductor insertion after total hip replacement. The authors reported improvement of pain, abductor muscle strength, decreased limp, and improvement in function at 2 years' follow-up. Rao et al.16 performed transosseous repair of gluteus medius and minimus insertions augmented by a GRAFTJACKET allograft acellular human dermal matrix in 12 patients. They attached the torn tendon to the greater trochanter through intra-osseous tunnels using a Krackow core stitch and augment the repair with allograft acellular human dermal matrix to cover the bare area of greater trochanter with continuous No. 1 Vicryl absorbable suture. They reported significant improvement in pain, gait along with abductor strength, and Harris hip scores.16
There are several techniques for the repair of abductor avulsions. In the case of partial or full-thickness tears, open repair and endoscopic techniques have been well described with good outcomes.4, 5, 6, 7, 8, 9, 10, 11 This Technical Note details our technique for endoscopic repair of proximal hamstring avulsion injuries. Table 1 outlines the advantages and disadvantages of our technique and Table 2 lists salient pearls and pitfalls. There are a number of advantages to an open repair of abductor avulsions, including the ability to perform a repair of a complete avulsion particularly in the case of tendon atrophy. The degenerative condition of the tendons at the time of repair may be a predisposing factor for re-tears regardless of the surgical approach.10 Performing this open approach is also a less technically demanding procedure when compared with an endoscopic repair. As such, the long learning curve of this technique can be not as prohibitive as endoscopic approaches, leading to lower operative times and decreased risk to surrounding neurovascular structures when performed by a more novice surgeon.
Table 1.
Advantages and Disadvantages of the Superior Gluteal Reconstruction
| Advantages | Disadvantages |
|---|---|
| Lack of fluid extravasation associated with endoscopic procedures | More-invasive technique with fewer smaller surgical incisions |
| Shorter surgical time compared with endoscopic procedures | Increased blood loss |
| Steep learning curve and high technical skill required | Injury to neurovascular structures |
| Ideal for tendon and muscular atrophy | Increased risk of infection |
Table 2.
Pearls and Pitfalls of Superior Gluteal Reconstruction
| Pearls | Pitfalls |
|---|---|
|
|
There are also disadvantages to an open approach that must be considered. The re-tear rate has been reported as 6% to 31% in open repair.10, 11, 17, 18 There is still a considerable risk to damage of surrounding neurovascular tissues and an inherent increased risk of infection when compared with endoscopic approaches.
In this technique, we incorporate the graft into the repair construction using a double-row repair. We believe that this technique provides better mechanical properties by increasing the immediate structural strength to prevent suture pullout. Moreover, this technique enables better area of graft compression to the bone, which may help increase healing rate. Acellular human dermal allograft has shown to improve healing rates and outcomes in large rotator cuff tears in a safe and effective manner in multiple studies.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.J.N. reports non-financial support from Allosource, other from American Journal of Orthopedics, other from American Orthopaedic Society for Sports Medicine, non-financial support from Arthrex, other from Arthroscopy Association of North America, non-financial support from Athletico, non-financial support from DJ Orthopaedics, non-financial support from Linvatec, non-financial support from Miomed, personal fees from Ossur, non-financial support from Smith & Nephew, personal fees and non-financial support from Springer, and non-financial support from Stryker, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Right lateral decubitus, right side, open approach. This video demonstrates our approach to repair of abductor tendon tear with severe tendon loss using a superior gluteal reconstruction technique. In this technique, we use an acellular human dermal allograft and incorporate it into the repair construction using a double-row repair, providing better mechanical properties by increasing the immediate structural strength to prevent suture pullout. This technique also enables better area of graft compression to the bone which may help increase healing rate.
References
- 1.Bunker T.D., Esler C.N., Leach W.J. Rotator-cuff tear of the hip. J Bone Joint Surg Br. 1997;79:618–620. doi: 10.1302/0301-620x.79b4.7033. [DOI] [PubMed] [Google Scholar]
- 2.Lachiewicz P.F. Abductor tendon tears of the hip: Evaluation and management. J Am Acad Orthop Surg. 2011;19:385–391. doi: 10.5435/00124635-201107000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Kagan A., 2nd Rotator cuff tears of the hip. Clin Orthop Rel Res. 1999:135–140. [PubMed] [Google Scholar]
- 4.Byrd J.W.T., Jones K.S. Endoscopic repair of hip abductor tears: Outcomes with two-year follow-up. J Hip Preserv Surg. 2017;4:80–84. doi: 10.1093/jhps/hnw047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perets I., Mansor Y., Yuen L.C., Chen A.W., Chaharbakhshi E.O., Domb B.G. Endoscopic gluteus medius repair with concomitant arthroscopy for labral tears: A case series with minimum 5-year outcomes. Arthroscopy. 2017;33:2159–2167. doi: 10.1016/j.arthro.2017.06.032. [DOI] [PubMed] [Google Scholar]
- 6.Thaunat M., Chatellard R., Noel E., Sonnery-Cottet B., Nove-Josserand L. Endoscopic repair of partial-thickness undersurface tears of the gluteus medius tendon. Orthop Traumatol Surg Res. 2013;99:853–857. doi: 10.1016/j.otsr.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Nho S.J., Grzybowski J.S., Bogunovic L. Diagnosis, evaluation, and endoscopic repair of partial articular gluteus tendon avulsion. Arthrosc Tech. 2016;5:e425–e431. doi: 10.1016/j.eats.2016.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chandrasekaran S., Lodhia P., Gui C., Vemula S.P., Martin T.J., Domb B.G. Outcomes of open versus endoscopic repair of abductor muscle tears of the hip: A systematic review. Arthroscopy. 2015;31:2057–2067.e2. doi: 10.1016/j.arthro.2015.03.042. [DOI] [PubMed] [Google Scholar]
- 9.Domb B.G., Nasser R.M., Botser I.B. Partial-thickness tears of the gluteus medius: Rationale and technique for trans-tendinous endoscopic repair. Arthroscopy. 2010;26:1697–1705. doi: 10.1016/j.arthro.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 10.Walsh M.J., Walton J.R., Walsh N.A. Surgical repair of the gluteal tendons: A report of 72 cases. J Arthroplasty. 2011;26:1514–1519. doi: 10.1016/j.arth.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Davies J.F., Stiehl J.B., Davies J.A., Geiger P.B. Surgical treatment of hip abductor tendon tears. J Bone Joint Surg Am. 2013;95:1420–1425. doi: 10.2106/JBJS.L.00709. [DOI] [PubMed] [Google Scholar]
- 12.Whiteside L.A. Surgical technique: Transfer of the anterior portion of the gluteus maximus muscle for abductor deficiency of the hip. Clin Orthop Rel Res. 2012;470:503–510. doi: 10.1007/s11999-011-1975-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whiteside L.A. Surgical technique: Gluteus maximus and tensor fascia lata transfer for primary deficiency of the abductors of the hip. Clin Orthop Rel Res. 2014;472:645–653. doi: 10.1007/s11999-013-3161-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robertson W.J., Gardner M.J., Barker J.U., Boraiah S., Lorich D.G., Kelly B.T. Anatomy and dimensions of the gluteus medius tendon insertion. Arthroscopy. 2008;24:130–136. doi: 10.1016/j.arthro.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 15.Fehm M.N., Huddleston J.I., Burke D.W., Geller J.A., Malchau H. Repair of a deficient abductor mechanism with Achilles tendon allograft after total hip replacement. J Bone Joint Surg Am. 2010;92:2305–2311. doi: 10.2106/JBJS.I.01011. [DOI] [PubMed] [Google Scholar]
- 16.Rao B.M., Kamal T.T., Vafaye J., Taylor L. Surgical repair of hip abductors. A new technique using Graft Jacket allograft acellular human dermal matrix. Int Orthop. 2012;36:2049–2053. doi: 10.1007/s00264-012-1630-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alpaugh K., Chilelli B.J., Xu S., Martin S.D. Outcomes after primary open or endoscopic abductor tendon repair in the hip: A systematic review of the literature. Arthroscopy. 2015;31:530–540. doi: 10.1016/j.arthro.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 18.Davies H., Zhaeentan S., Tavakkolizadeh A., Janes G. Surgical repair of chronic tears of the hip abductor mechanism. Hip Int. 2009;19:372–376. doi: 10.1177/112070000901900412. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Right lateral decubitus, right side, open approach. This video demonstrates our approach to repair of abductor tendon tear with severe tendon loss using a superior gluteal reconstruction technique. In this technique, we use an acellular human dermal allograft and incorporate it into the repair construction using a double-row repair, providing better mechanical properties by increasing the immediate structural strength to prevent suture pullout. This technique also enables better area of graft compression to the bone which may help increase healing rate.