Abstract
The purpose of this study is to assess the role of bioskills in orthopaedic and neurosurgical resident education. A survey of the utilization and perceived efficacy of bioskills was submitted to Lumbar Spine Research Society (LSRS) members. 36/104 surgeons responded, including 25 orthopaedic, 7 neurosurgical, and 4 integrated respondents. 63% of orthopaedic and 83% of neurosurgery faculty, reported using bioskills. When asked if completion of bioskills modules would encourage advancing trainees’ participation (1–10 scale, 10 greatly increase), neurosurgical faculty reported 4.00 versus orthopaedics 6.43. Although orthopaedic faculty perceive greater efficacy of bioskills, the clinical impact of this difference remains uncertain.
Keywords: Spine surgery, Bioskills, Resident education, Fellow education, Medical curricula
1. Introduction
The role of simulation training methods continues to increase in resident education, especially in surgical specialties where there is little margin for novice error. Bioskills laboratories provide residents a simulated setting to learn and develop complex surgical skills through practice and repetition.1,2 Comparing the efficacy of bioskills and training modules across multiple medical disciplines, McGaghie and colleagues compiled a meta-analysis of 14 papers, including 6 randomized control trials, finding an overall benefit to simulation-based education.3 These labs aim to bridge the gap between novice and expert without potential risk of patient morbidity or increased operating times.4 The restrictions on resident work-hours have further increased the necessity of training opportunities outside the operative room.
While the concept of bioskills training has been adopted by many general surgery programs, the implementation has been delayed in orthopaedic and neurosurgical programs. In looking at neurosurgical and orthopaedic spine training, Dvorak et al. found a significant difference in levels of confidence between specialties; additionally they found the strongest predictor of resident confidence to be the amount of spine surgical exposure.5 Spine training makes up a considerably larger portion of neurosurgery residency, than orthopaedic residency. Orthopaedic programs may, therefore, need additional education platforms for their trainees while neurosurgical programs may need these platforms to accelerate or refine surgical training.
The role and efficacy of bioskills has yet to be determined on improving psychomotor skills among trainees. A variety of small studies with limited sample sizes investigated the use of bioskills modules, but these have failed to demonstrate statistical significance.6, 7, 8, 9 The studies demonstrate increased confidence in participants but no significant objective data regarding technical skills. On the other hand, a number of select studies have been more extensively powered and able to draw statistically significant results that demonstrate improvement in both skill and learning retention.10,11 The increasing role of bioskill laboratories within orthopaedic resident training is reflected well by both program directors and residents expressing strong agreement in surgical skill improvement.12
Bioskills labs serve as viable education tools in residency education, but little is known about their current usage in resident education. The goal of this project was to gain a better understanding of how current orthopaedic and neurosurgery residency programs utilize bioskills simulations within their educational curriculum.
2. Methods
2.1. Survey development, subjects, and administration
An online survey was distributed (SurveyMonkey.com, LLC, Palo Alto, CA, USA) in 2015 to the Lumbar Spine Research Society (LSRS), inviting responses from spine surgeons who educate resident or fellows. Survey results from respondents who were not involved in teaching residents or fellows were excluded from the analysis. Questions were designed to understand the utilization and perceived efficacy of current use of bioskills laboratories, value of modules and opinions of current simulators. The self-administered survey consisted of 24 items.
2.2. Data analysis
Results of the survey were retrieved and analyzed by the authors. Responses to items were presented as counts, percentages and means. Student t-tests were used to compare means of continuous variables, with statistical significance assigned to p-values less than 0.05. Analysis of variance (ANOVA) was performed for analyses consisting of 3 or more groups. Fisher's exact tests were performed when appropriate for analysis of response distributions. This study was reviewed by our institutional review board and deemed to be exempt.
3. Results
3.1. Respondent and institutional demographics
A total of 36 responses collected (104 surveys sent, 35% response rate) from the online survey underwent statistical analysis. The majority of responders (69.4%, 25 responses) considered their primary departmental affiliation to be orthopaedic surgery. 19.4% (7) of responders were neurosurgeons and 11.1% (4) of responders were part of an integrated program. 94.3% of responders were affiliated with a spine surgery department that educated both residents and fellows. 70.8% of respondents were directly involved in the design of their program's educational curriculum. The distribution of resident spine case volume reported was significantly different by departmental affiliation (orthopaedic versus neurosurgery) (p < 0.0001). Neurosurgical responders estimated over 200 spine cases per resident, while orthopaedic responders estimated 41 to 80 cases.
3.2. Skill proficiency of trainees
The distribution of proficiency timing by departmental affiliation was similar for many skills (Fig. 1). Level of training proficiency for multiple surgical tasks, such as use of burr for decompression, dural repairs, and closure of spinal wounds demonstrated significant differences between responders stratified by departmental affiliations. Specifically, the estimated year to become proficient with using the burr for decompression was significantly different between responders of different departmental affiliations (Fisher's exact p = 0.0058). Orthopaedic responders identified proficiency at a mean of PGY 5.11 years ±1.29, which was longer than integrated responders, 4.33 years ±0.47, and neurosurgical responders, 3.17 years ±0.90. Additionally, the estimated year to become proficient with repairing dural tears was significantly different between responders of different departmental affiliations (Fisher's exact p = 0.0003). Orthopaedic responders identified proficiency of repairing dural tears at a mean of PGY 5.76 years ±0.55, which was longer than neurosurgical responders, 5.00 years ±1.73, and integrated responders, 4.67 years ±0.47.
Fig. 1.
Average experience level that respondents believed correlated with surgical skill set.
3.3. Exposure of bioskills curriculum
Among responders, 68% reported the implementation of a bioskills curriculum at their institution with cadavers serving as the most common simulation (94.1%) followed by sawbone models (82.4%) (Fig. 2). Respondents stated cadavers were used most commonly on either an annual (41.2%) or quarterly (35.3%) basis. The majority (73.1%) of responders reported trainees utilizing industry sponsored courses for bioskills training. 35% of respondents preferred that bioskills modules be maintained at their current level, while 61% of respondents preferred that the time spent performing modules be increased. Based on a 10-point Likert scale, the two largest barriers to implementing bioskills in a spine surgery educational curriculum are financial constraints (mean = 6.52) and faculty time constraints (mean = 6.48). Forty percent indicated their program had a budget from $1000 to $10,000; 50% stated current funding was sufficient while 40% stating need for additional funding. Both external industry related funding and departmental funding the most commonly cited contributors toward funding bioskills training session.
Fig. 2.
Reported use of simulators in bioskills curricula.
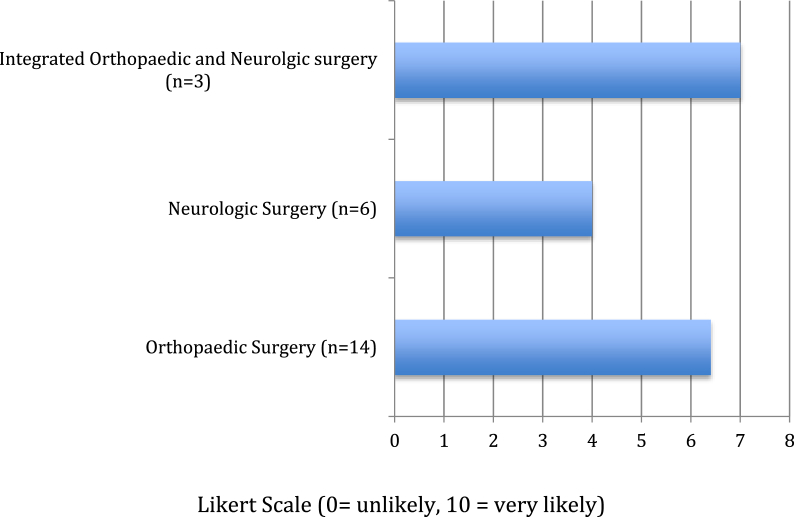
On a scale of 1, indicating “No significant change in OR participation,” to 10, indicating “Very likely to increase OR participation,” responders reported an average of 5.87 score, suggesting that successful demonstration of skills during a bioskills session would encourage them to advance a trainee's level of participation in the OR (Fig. 3). Using a similar scale (1-no significance and 10- critical importance), the mean response was 5.45 regarding the importance of bioskills modules to training of residents/fellows. Respondents reported the most beneficial aspect, based on a 10-point Likert scale, was the ability for trainees to gain familiarity and experience with the use of instruments. Regarding opinions about incorporation of psychomotor skills within bioskills training, the greatest support (based on a 10-point Likert scale) was for trainees to learn how to practice open placement of pedicle screws.
Fig. 3.
Surgeon responses* to question: Would satisfactory completion of a formal bioskills lab with successful demonstration of tested skills encourage you to advance residents and/or fellows participation in the OR?.
3.4. Preparedness for practice
On a scale from 1 (poor preparation) to 10 (very well prepared), the mean response was 8.68 regarding a fellow's level of preparedness (from their educator's perspective) upon completion of his fellowship. ANOVA demonstrated difference between preparedness score based on training (p < 0.0001) with significant differences between Orthopaedic residents and Neurosurgery residents as well as Orthopaedic residents and integrated programs. Mean Orthopaedic, Neurosurgery, and Integrated scores were 2.67 ± 0.4, 6.33 ± 0.8, and 8.17 ± 0.6, respectively. Significant differences were found for preparedness for independent practice based on case volume (p < 0.0001) with significant differences between those who had over 200 (mean score 8.42 ± 0.5) and 0–40 (mean score 3 ± 1.0, p = 0.0018), 41–80 (mean score 2.78 ± 0.5, p < 0.0001), and 81 to 120 (mean score 3.33 ± 1.0, p = 0.0008).
4. Discussion
The role of bioskills laboratories has become increasingly significant within medical education, however its efficacy within resident training is unknown. Our study captures current utilization of spine bioskills curricula within orthopaedic and neurosurgery residency training demonstrating significant differences between subspecialties and perceived efficacy of bioskills modules. Additionally, this study confirms that budget and faculty time constraints are potential barriers to implementation in surgical training.
The majority (12/18) of orthopaedic faculty reported residents completing fewer than 80 spine cases compared to all neurosurgical faculty reporting over 200 spine cases. Our study re-demonstrates this disparity in current literature regarding resident spine case volumes between specialties.13 Competency for various spine surgical skills trended toward earlier level of training expectations for neurosurgery compared with orthopaedic surgery. It is yet to be determined if a direct correlation exists between spine case volume and competency in earlier years of training; however, this trend at the very least demonstrates an association.
Utilization of bioskills modules among programs varied with neurosurgery respondents reporting 83.3% and orthopaedic surgery respondents reporting 62.5%. Interestingly in addition to the case volume discrepancy, we found a similar difference in utilization of bioskills laboratories, further highlighting difference of spine exposure in and out of the operating room between specialties. When asked if satisfactory completion of bioskills modules would encourage advancing trainees participation (1-no significance, 10-very greatly increase), total responses yield a weighted average of 5.87. When stratified by responses by department, orthopaedic surgery (n = 14) was 6.43 and neurosurgery (n = 6) was 4.00 (P value 0.0139). The results show greater utility of bioskills curriculum within orthopaedic training compared to neurosurgery; however, successful completion of bioskills and intraoperative competency were not compared, making it difficult to draw direct conclusions between bioskills efficacy and operative competency. Outcomes of the survey demonstrated that neurosurgery tends to expect earlier performance of clinical skills than does orthopaedic surgery. The impact of higher utilization of bioskills laboratories and difference in case volumes could potentially provide insight into early competency of neurosurgery programs; however, this is not addressed within this project.
Our survey demonstrated that 68% of respondents reported using bioskills education, with cadaveric and sawbones as the most common simulations, 94% and 82%, respectively. Interestingly 96% of respondents recommended increasing their program's time spent on bioskills curriculum, which re-demonstrates the growing trend of incorporating a bioskills curriculum into resident education.3,14,15 Orthopaedic faculty's response of improved competency with use of bioskills makes incorporation significantly beneficial for orthopaedic residents. When asked to report readiness for spine practice after residency (1–10), orthopaedics was 3.14 whereas neurosurgery was 8.17. Lack of readiness for practice was found correlate with case volume in this study, which is found in current literature demonstrating orthopaedic surgery residents averaging less than one-half of the spine procedures performed by neurosurgery residents.13 Importantly, however, orthopaedic spine fellowship training provides an additional case volume (approximately 300–500 procedures) exposure equal to or extending that of neurosurgery residents.13
This study is limited by the subjective nature of survey questions, which are predicated on faculty opinions rather than objective evidence. The nature of this survey does not provide direct correlations between utilization of bioskills and competency; however, it does afford possible associations. An additional limitation is the small cohort of respondents, a more complete analysis could be provided if spine faculty within other spine organizations were surveyed.
Although bioskills simulations provide an environment to further develop surgical skills, they are unable to replicate the skills obtained from repetitive live operative experiences. In creating transparency in the manner in which programs train resident outside the operating room, this survey data is useful in providing information for programs interested in further developing bioskills curricula. Orthopaeadic surgery programs will need to further address the spine case volume discrepancies and the manner in which bioskill labs can substitute for operative experience.
5. Conclusion
The results of our survey, along with current trends in resident training, have demonstrated that bioskills laboratories are a widely utilized resource in surgical education advancing surgical skills and techniques. While orthopaedic surgery faculty seem to perceive greater efficacy of bioskills laboratories on developing readily transferable surgical skills than their neurosurgical colleagues, this may be partially influenced by variability in orthopaedic surgery versus neurosurgical program training experiences. Furthermore, the data gathered from this research will guide further internal projects focused on creating high fidelity, low cost bio skills curriculum, using feedback from programs as to what they value for education and integrating it into future project designs.
Declaration of competing interestCOI
The authors report no external funding source for this study. The authors declare no conflict of interest.
Contributor Information
Michael H. McCarthy, Email: michaelhallmccarthy@gmail.com.
Barrett S. Boody, Email: barrett.s.boody@gmail.com.
Peter R. Swiatek, Email: peter.swiatek@northwestern.edu.
Brett D. Rosenthal, Email: brettdavidrosenthal@gmail.com.
Jason Savage, Email: savagej2@ccf.org.
Wellington K. Hsu, Email: Wkhsu@yahoo.com.
Alpesh A. Patel, Email: alpesh.patel1@nm.org.
References
- 1.Sanfey H.A., Dunnington G.L. Basic surgical skills testing for junior residents: current views of general surgery program directors. J Am Coll Surg. 2011;212:406–412. doi: 10.1016/j.jamcollsurg.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 2.Ahmed K., Miskovic D., Darzi A., Athanasiou T., Hanna G.B. Observational tools for assessment of procedural skills: a systematic review. Am J Surg. 2011;202:469–480 e6. doi: 10.1016/j.amjsurg.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 3.McGaghie W.C., Issenberg S.B., Barsuk J.H., Wayne D.B. A critical review of simulation-based mastery learning with translational outcomes. Med Educ. 2014;48:375–385. doi: 10.1111/medu.12391. [DOI] [PubMed] [Google Scholar]
- 4.Bann S., Davis I.M., Moorthy K. The reliability of multiple objective measures of surgery and the role of human performance. Am J Surg. 2005;189:747–752. doi: 10.1016/j.amjsurg.2005.03.020. [DOI] [PubMed] [Google Scholar]
- 5.Dvorak M.F., Collins J.B., Murnaghan L. Confidence in spine training among senior neurosurgical and orthopedic residents. Spine (Phila Pa 1976) 2006;31:831–837. doi: 10.1097/01.brs.0000207238.48446.ce. [DOI] [PubMed] [Google Scholar]
- 6.Chitale R., Ghobrial G.M., Lobel D., Harrop J. Simulated lumbar minimally invasive surgery educational model with didactic and technical components. Neurosurgery. 2013;73(Suppl 1):107–110. doi: 10.1227/NEU.0000000000000091. [DOI] [PubMed] [Google Scholar]
- 7.Ghobrial G.M., Anderson P.A., Chitale R., Campbell P.G., Lobel D.A., Harrop J. Simulated spinal cerebrospinal fluid leak repair: an educational model with didactic and technical components. Neurosurgery. 2013;73(Suppl 1):111–115. doi: 10.1227/NEU.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 8.Harrop J., Rezai A.R., Hoh D.J., Ghobrial G.M., Sharan A. Neurosurgical training with a novel cervical spine simulator: posterior foraminotomy and laminectomy. Neurosurgery. 2013;73(Suppl 1):94–99. doi: 10.1227/NEU.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 9.Ray W.Z., Ganju A., Harrop J.S., Hoh D.J. Developing an anterior cervical diskectomy and fusion simulator for neurosurgical resident training. Neurosurgery. 2013;73(Suppl 1):100–106. doi: 10.1227/NEU.0000000000000088. [DOI] [PubMed] [Google Scholar]
- 10.Gottschalk M.B., Yoon S.T., Park D.K., Rhee J.M., Mitchell P.M. Surgical training using three-dimensional simulation in placement of cervical lateral mass screws: a blinded randomized control trial. Spine J. 2015;15:168–175. doi: 10.1016/j.spinee.2014.08.444. [DOI] [PubMed] [Google Scholar]
- 11.Luciano C.J., Banerjee P.P., Bellotte B. Learning retention of thoracic pedicle screw placement using a high-resolution augmented reality simulator with haptic feedback. Neurosurgery. 2011;69 doi: 10.1227/NEU.0b013e31821954ed. ons14-o19; discussion ons9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karam M.D., Pedowitz R.A., Natividad H., Murray J., Marsh J.L. Current and future use of surgical skills training laboratories in orthopaedic resident education: a national survey. J Bone Joint Surg Am. 2013;95:e4. doi: 10.2106/JBJS.L.00177. [DOI] [PubMed] [Google Scholar]
- 13.Daniels A.H., Ames C.P., Smith J.S., Hart R.A. Variability in spine surgery procedures performed during orthopaedic and neurological surgery residency training: an analysis of ACGME case log data. J Bone Joint Surg Am. 2014;96:e196. doi: 10.2106/JBJS.M.01562. [DOI] [PubMed] [Google Scholar]
- 14.Kneebone R. Simulation in surgical training: educational issues and practical implications. Med Educ. 2003;37:267–277. doi: 10.1046/j.1365-2923.2003.01440.x. [DOI] [PubMed] [Google Scholar]
- 15.Nousiainen M.T., McQueen S.A., Ferguson P. Simulation for teaching orthopaedic residents in a competency-based curriculum: do the benefits justify the increased costs? Clin Orthop Relat Res. 2016;474:935–944. doi: 10.1007/s11999-015-4512-6. [DOI] [PMC free article] [PubMed] [Google Scholar]