Abstract
Background
This study assesses the outcome of hemi epiphysiodesis with a 2-holed reconstruction plate using the tension band principle in angular deformities of the knee and variables influencing the outcome.
Methods
Prospective study from 2012 to 2016 included 23 children with coronal deformities of the knee joint. IMD, ICD, BMI, mLDFA, mMPTA, mTFA, Mechanical axis deviation, Perpendicular mechanical axis ratio, and screw angle measured. Correction and rate of correction compared with BMI, age, etiology, PMAR and MAD, deformity, a segment of bone and the screw angle.
Results
Total 65 segments operated in 23 children with 40 knees. Out of the total 65, 36 plates were kept in distal femur physis and 29 in the proximal tibial physis. Thirteen knees had genu varum and 27 had genu valgum. The mean age at the time of surgery was 11.25 months. The mean follow-up of 36 months and the average time for correction was 18.64 months. 77.5% correction achieved with ROC maximum in the initial 6 months. ROC in TFA per year were 7.80(femur), 50(tibia), and 120(femur with tibia). Complications included broken implant, screw back out, screw irritation and rebound phenomenon.
Conclusions
2-holed reconstruction plate gives similar correction to that of the 8-plate within a comparable period without additional complications. It has the advantage of being cost effective and readily available. Age, BMI, type of deformity, amount of initial deformity, do not play a significant role in the outcome of correction. Screw placement may have a role in the final correction of the deformity.
Level of evidence
Level 3.
Keywords: Angular deformity, Genuvalgum, Genuvarum, Hemiepiphysiodesis, Rebound phenomenon
1. Introduction
Hemiepiphysiodesis is useful for pathological angular deformity correction across the knee joint. Temporary methods include stapling, transphyseal screw and tension band plate.1, 2, 3 The use of temporary over a permanent epiphysiodesis has the advantage of being a reversible and untimed procedure thus has the added benefit of applying to younger children with more significant growth potential. Tension band plate works on the tension band principle causing dynamic correction using an extra physeal fulcrum. The tension band plate spares the physis and periosteum, offering perhaps the best solution available for angular deformity to date. No diagnosis or age constitutes a contraindication for guided growth except physiological deformity. It is reversible and well tolerated by children of all ages. Furthermore, the related cost, prolonged hospitalization, delayed weight bearing, and potential complications are less for guided growth using the tension band technique compared to osteotomy. However in developing countries the cost of implant is a main determining factor in surgery. The most popular Orthofix eight-plate® is costly and unaffordable for few patients, especially in bilateral deformities. The reconstruction (recon) plate that we use is available for 1/20th the price of Orthofix eight plate®. If a low cost screw plate construct gives similar outcome like that of a specifically marketed implant, this can be used more globally by avoiding the cost factor. The purpose of this study is to evaluate the clinical and radiological outcome of temporary epiphysiodesis with a 2-holed reconstruction plate using the tension band principle in angular deformities of the knee in children in our hospital. In addition, we assess the rate of deformity correction following Hemi epiphysiodesis using 2- hole reconstruction plate, the complications and the variables influencing the outcome in children with angular deformity.
2. Materials and methods
A prospective study conducted from 2012 to 2016 at a tertiary care center in South India. Forty knees in 23 children with angular deformity of the knee treated with Hemi epiphysiodesis using a 2-holed reconstruction plate from 2012 to 2013 were prospectively followed. Institutional ethical committee clearance for the study and informed patient consents were obtained for the survey. Physiologic varus and valgus deformity and children with an angular deformity for which corrective osteotomy was done in the same limb before the study were excluded. Intermalleolar distance (IMD) for genu valgum, intercondylar distance (ICD) for genu varum and Body mass index (BMI) was assessed clinically. Mechanical lateral distal femoral angle (mLDFA), mechanical medial proximal tibial angle (mMPTA), mechanical tibiofemoral angle (mTFA), Mechanical axis deviation (MAD), Perpendicular mechanical axis ratio (PMAR) and placement of screw (screw angle) in long-standing radiographs were measured preoperatively and during follow-up visits.4,5 Radiographic measurements were made on preoperative and postoperative long standing anteroposterior lower-extremity radiographs (long leg view). Care was taken to ensure that patella is facing forwards when radiographs are taken to avoid error in measurement.
The rate of correction (ROC) was measured at each visit. ROC was obtained by dividing the difference in the correction of angles in degree by the number of months of follow-up. All measurements were done by one observer on two separate occasions (with an interval of 2 weeks) and also by two different observers independently. The children were followed up to maturity/implant removal.
The mechanical axis (MA) was taken as a line drawn from the center of the femoral head to the center of the tibial plafond. Mechanical axis deviation (MAD) was expressed as the distance of the mechanical axis from the center of the knee. To measure this distance, the knee joint was divided into six zones by a modification of the method originally described by Muller and popularized by Mielke and Stevens.6,7 To avoid magnification errors on radiographs, we measured the position of the mechanical axis ratio (PMAR) by dividing perpendicular distance of mechanical axis from the medial-most point of tibial condyle with a width of the tibial plateau.8 The angle subtended by the two screws with each other was taken as screw angle. Angle more than 100 was considered as divergent and any angle less than 100 was taken as parallel insertion of screws.
2.1. Technique of surgery
All patients were operated by the temporary hemi epiphysiodesis using a 2-holed reconstruction plate by the tension band principle. We followed a modified method to which has been originally described by Stevens.3 The patient was laid supine on a radiolucent operating table, under general anesthesia. Tourniquet control was used in all cases. Fluoroscopy was used to visualize the growth plate on the frontal and sagittal plane. Then a 2 cm long incision, centered on the physis, was made. The dissection was carried through the fascia, between muscles and the leash of epiphyseal vessels was visualized. The periosteum was undisturbed. We did not pass a guide wire into the physis. With fluoroscopic control, the 2-holed reconstruction plate was held spanning the physis using a forceps, and the guide wires were introduced: the epiphyseal guide wire was inserted first, followed by the metaphyseal guide wire. 4 mm cannulated self-tapping fully/partially threaded screws were used to fix the plate. The screws were parallel or divergent but never convergent, and care was taken that they never entered the physis or the joint surface. The plate was centered in the sagittal plane, to avoid an iatrogenic recurvatum deformity (Fig. 1). We used stainless steel recon plates made by a local Indian company. These recon plates are less prominent and thinner than the pelvic recon plates of some of the mainstream manufacturers. The centre to centre distance between the two screw holes in our plate is 14 mm. It has length of 25 mm, breadth of 10 mm and the thickness of the plate is 1.2 mm. It allows for a screw angulation of maximum 360. The screw length used commonly varies from 20 mm to 30 mm.
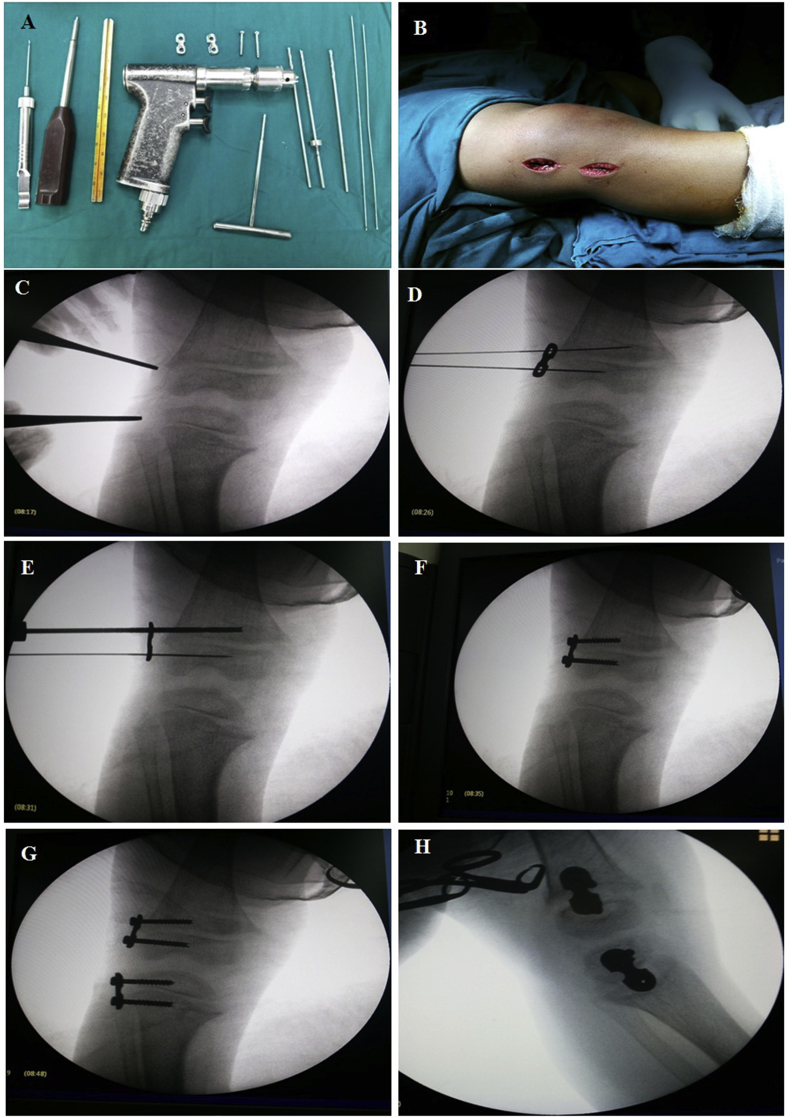
Fig. 1.
A; Surgical instruments, B; Surgical incision, C; indentification of the physis using fluoroscopy, D; Passing guide wire and placement of the plate spanning the physis, E; Drilling for screw placement, F; after fixation of both screws, G; After both femur and tibia hemiepihysiodesis, H; Lateral view showing central placement of the screw.
Since the first postoperative day, movement and weight-bearing were encouraged as per pain tolerance, and patients were discharged by second or third day after surgery. Patients were called for follow up at regular intervals of 3 months each and clinical and radiological assessment was done.
Outcome (correction) of the procedure was categorized as fully corrected, partially corrected and not corrected. Knees in which the MA reverted back to normal and reached the center of the knee was taken as a full correction. The knee in which the MA showed a shift from a farther MA zone to a nearer zone but did not achieve full correction was considered as partially corrected. When there was no change in the MA zone before surgery and at the end of study/skeletal maturity was regarded as not corrected. The outcome of surgery and ROC was compared with variables like BMI, age at the time of surgery, etiology (nature of physis), PMAR and MAD before surgery, type of deformity, the segment of bone on which surgery was done and the screw angle. Once the correction was achieved, we waited till the next adjacent follow-up visit (after three months) for implant removal for all children to avoid rebound phenomenon. The end of the study was described as skeletal maturity or a bony procedure done for the correction of the deformity.
3. Results
All evaluation measures were found reproducible with intraobserver and interobserver agreements (Interclass correlation coefficient >0.90 for all parameters)(p < 0.001). There were 23 children with 40 affected knees, 12 boys, and 11 girls. Out of the 40 involved knees, 21 were the right side, and 19 were left knee. The total number of segments (femur/tibia) operated was 65. Out of the total 65, 36 plates were in the distal femur physis and 29 in the proximal tibial physis. 13 knees had genu varum, and 27 had genu valgum (Table 1). 13 knees had normal physis of distal femur and tibia, and the rest 27 had sick (abnormal) physis of distal femur and tibia. The mean age at the time of surgery was 11.25 months and the average follow-up period was 36 months. The average time taken for correction was 18.64 months. Mean body mass index (BMI) of the children were 19.54 ± 4.92 kg/m2. Intermalleolar and intercondylar distance improved from the preoperative median values of 11 cm and 10 cm respectively to 9 cm and 5 cm at final follow-up.
Table 1.
Mean preoperative angles in varus and valgus deformity of the knee.
| Angle | Preop |
Preop |
|---|---|---|
| G. Varum(Mean ± SD) (in degree) |
G.Valgum(Mean ± SD) (in degree) |
|
| mLDFA | 98.39 ± 6.69 | 82.95 ± 5.11 |
| mMPTA | 80.05 ± 5.96 | 94.01 ± 6.24 |
| mTFA | 21.18 ± 9.62 | 12.73 ± 6.46 |
mLDFA, mMPTA, and mTFA showed a more rapid rate of correction in the early period (3 months and 6 months) compared to the one year, and the final follow-up rate of corrections (Table 2). The rate of correction of MPTA had a statistically significant correlation with the segment where surgery was done (p-value 0.037)(Table 2). No statistically significant difference was observed between the rate of corrections of angles in genu varum and genu valgum (p > 0.05) (Table 2). There was no statistical significance between the rate of corrections in a healthy and sick physis in our study. However, the knees with sick physis had a better rate of correction in all angles compared to normal physis including correction of PMAR. The mTFA had a far superior rate of correction in case of sick physis (1.13) compared to the normal physis (0.56) (Table 2). [pvalue of TFA with type of the physis = 0.065].
Table 2.
Rate of correction of angles and PMAR with respect to various parameters for comparison.
| Parameter for Comparison | Rate of Correction (degree per month) |
||||
|---|---|---|---|---|---|
| mLDFA | mMPTA | mTFA | PMAR | ||
| Time (Mean) | 3 months | 0.34 | 0.59 | 0.72 | 0.04 |
| 6 months | 0.73 | 0.33 | 1.25 | 0.07 | |
| 1 year | 0.50 | 0.20 | 0.60 | 0.03 | |
| Final follow up | 0.61 | 0.30 | 0.81 | 0.04 | |
| Segment of bone operated (IQR) (Median) |
Femur | 0.65 (0.50,1.21) | 0.04 (0.00,0.30) | 0.65 (0.34,1.27) | 0.03 (0.02,0.065) |
| Tibia | 0.12 * | 0.52 * | 0.65 * | ||
| Both femur and tibia | 0.61 (0.21,0.84) | 0.33 (0.09,0.66) | 0.98 (0.49,1.32) | 0.05 (0.03,0.07) | |
| Type of Deformity and Nature of Physis (IQR) (Median) |
Genu Varum N = 13 |
0.61 (0.21,0.95) | 0.33 (0.30,0.73) | 1.20 (0.66,1.32) | 0.05 (0.03,0.08) |
| Genu Valgum N = 27 |
0.61 (0.21,0.87) | 0.13 (0.00,0.52) | 0.58 (0.40,1.28) | 0.04 (0.02,0.08) | |
| Normal Physis N = 13 |
0.50 (0.01,0.85) | 0.30 (0.04,0.71) | 0.56 (0.15,1.15) | 0.02 (0.01,0.08) | |
| Sick Physis N = 27 |
0.62 (0.47,1.05) | 0.32 (0.00,0.52) | 1.13 (0.70,1.320 | 0.05 (0.03,0.07) | |
* Single case where only tibial segment alone was operated.
Mean BMI were 18.8, 17.5, 22.2 kg/m2 in the corrected, partially corrected and not corrected groups respectively.(p = 0.572). Mean age at the time of surgery in full corrected, partially corrected and not corrected patients were 10.99, 12.87 and 11.16 years respectively.(p = 0.327).
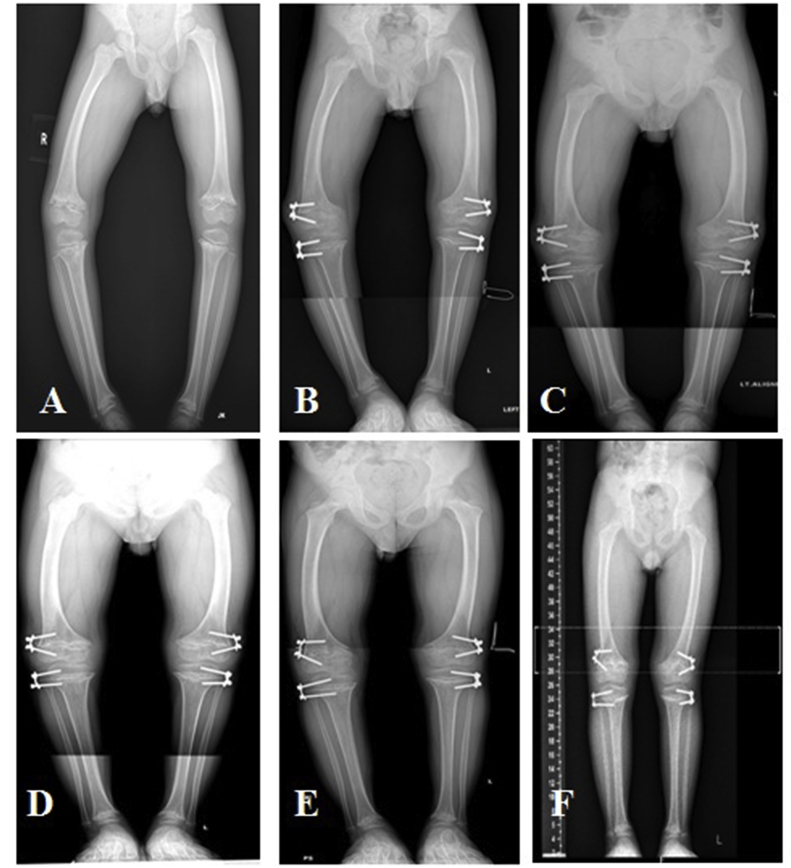
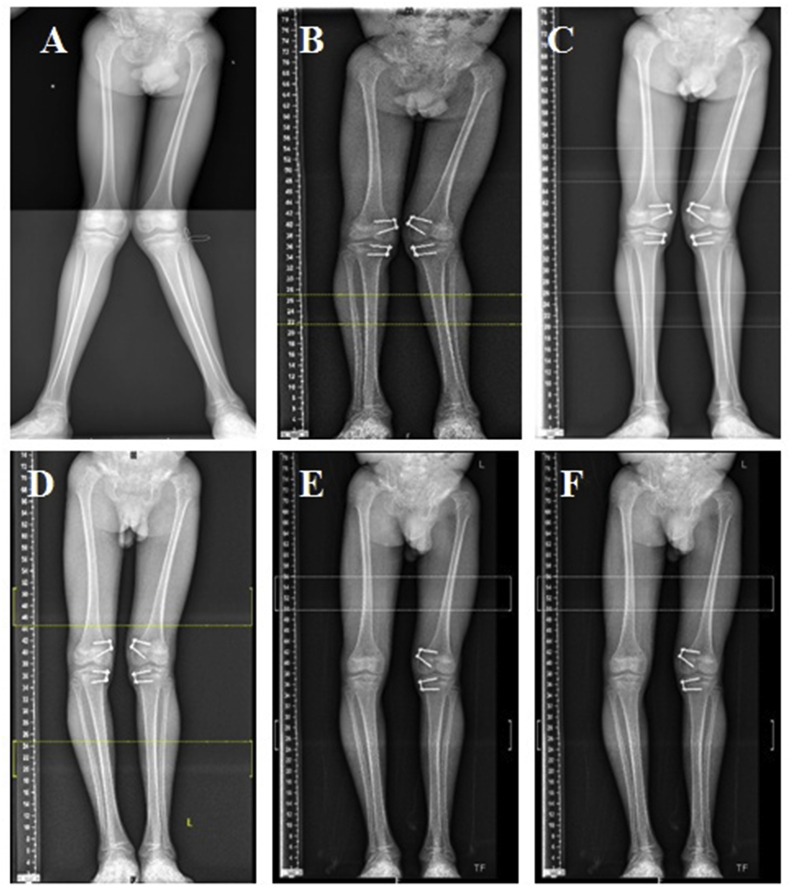
8 of the 13 varus knees got corrected (61.5%), and 23 of the 27 valgus knees got corrected (85.2%)(Table 3)(p = 0.421)(Fig. 2, Fig. 3). Out of the 9 knees in 7 children which were not corrected, 5 had genu varum, and 4 had genu valgum. Six out of the total seven children were girls. Three children had idiopathic genu valgum; three children had Hypophosphatemic rickets, another girl had Ellis Van Creveld syndrome.
Table 3.
Evaluation of surgical outcome and complications with respect to deformity and nature of physis.
| Number of Knees (N) (%) | Genu Varum(%) (N) | Genu Valgum(%)(N) | Normal Physis (%) | Sick Physis (%) | ||
| Outcome | Full Correction | 75% (30) | 61.50% (8) | 81.5% (22) | 76.9% | 74.1% |
| Partial Correction | 2.5% (1) | 0.00% (0) | 3.7% (1) | 0% | 2.5% | |
| No Correction | 22.5% (9) | 38.5% (5) | 14.8% (4) | 23.1% | 22.5% | |
| Total Correction | 77.5% (31) | 61.50% (13) | 85.2% (27) | 76.9% | 76.60% | |
| Complications (N) | Broken Implant | 0 | 1 | |||
| Screw Backout | 1 | 3 | ||||
| Rebound Phenomenon | 0 | 2 | ||||
| Difficult Implant Removal | 1 | 0 | ||||
| Screw Irritation | 0 | 1 | ||||
| Overcorrection | 0 | 2 | ||||
| Total | 2 (18.2%) | 9 (81.8%) | ||||
Fig. 2.
Long leg radiographs in a case of bilateral genu varum. A; preoperative severe genu varum, B; 3 months post-operative, C; 6 months follow-up, D; 9 months follow-up, E; 15 months follow-up, G; 24 months follow-up with full correction.
Fig. 3.
Long leg radiographs in a case of bilateral genu valgum. A; Before surgery, B; 3 months follow-up, C; 6 months follow-up, D; 9 months follow-up, E; 15 months follow-up, F; 24 months follow-up.
Full correction and overall correction was comparable for normal and for sick physis (Table 3). (p = 0.421).
Divergent screws produced full corrections in 86% and parallel screws produced full correction only in 50%,(p = 0.031). There was no statistically significant association between PMAR and MAD before surgery and after surgery in the outcome (p = 0.486 and p = 0.891 respectively). There was no correlation between age at the time of surgery and mean time taken for correction (p = 0.831).
Three patients who had overcorrection were all due to missing of follow-up visits. The majority of the complications were observed in patients who had a sick physis (81.8%) as shown in Table 3.
4. Discussion
Reproduction of zones of mechanical axis, MAD, LDFA, MPTA, and TFA in this study had excellent intra and inter-observer reliability regardless of the experience of the observer. All the measurements were equal to or greater than 0.90, similar to that of the previous studies.9, 10, 11
A retrospective multicentric study by Danino et al. on 967 physes calculated ROC of 0.77°/month for the femur and 0.79°/month for the tibia.12 In our study, we achieved correction in 77.5% of children with a mean time of correction of 18 months which is comparable to the studies by Ballal et al. (16months) and Weinmann et al. (14 months).13,14 Ballal et al. had a ROC per year of 8.40(femur), 60(tibia), and 14.40 (femur with tibia).13 We have achieved a ROC in TFA per year of 7.80(femur), 50(tibia), and 120(femur with tibia). Weinmann has reported a rate of correction of 100/year. Kumar et al. reported a ROC of 1.40/month in the TFA using eight plate.15 We have observed that ROC in the early period (3 and 6 months follow-up) is more compared to 9 months, one year and end of the study. This was also reported by Weinmann et al. in their study. We found that fastest ROC was achieved when the distal femoral and proximal tibial physis were treated concurrently. There was no restriction on mobilization and weight bearing after surgery for our children and encourage as per pain tolerance. The measurement of ROC allows the surgeon to estimate the overall time and provide parents with relevant information.
In our study most of the patients were adolescents. This is similar to the study by Stevens et al. and Ballal et al.3,13 In the study by Danino et al., they observed that patients with more than three years of growth remaining at the time of surgery had a statistically significant chance of correction.12 BMI, age at the time of surgery, degree of angulation before surgery had no statistically significant influence on outcome in our study. The type of deformity did not play a significant role in final correction in our patients. Both PMAR and MAD are important parameters to assess during follow-up visits, and PMAR will minimize magnification errors of the radiograph. There is split opinion regarding the direction of screw placement across the physis. We observed a statistically significant difference between parallel and divergent placement of screw in the outcome of correction. Divergent screws produced full corrections in 86% and parallel screws produced full correction only in 50%.
It was believed that sick physis did not tolerate direct surgical manipulation and could lead to physeal closure. Contemporary studies suggest that this is not the case.16 Even a sick physis is not a contraindication for guided growth. As per Stevens, part of that “sickness” is because of gravity, eccentric loading, and ligamentous laxity compounded by shear and torsional forces.17 We observed that sick physis had an equal amount of correction compared to the normal physis and even a better percentage of ROC of all the angles than a normal physis even though there was no statistical significance. It may be either due to more number of knees with sick physis in our study or probably that a pathological physis is more malleable to changes and growth modulation. But, it has also been proven that many conditions like Blount's disease and Hypophosphatemic rickets can be extremely resistant to growth modulation, and tension band plate in such cases has been mostly recommended to prevent the progression of the deformity than the actual correction of it. Peter M Stevens and Joshua B Klatt support early intervention via guided growth to restore and preserve neutral axis in pathological physis.17 It was observed that ROC of mTFA was highest when hemiepiphysiodesis of both femur and tibia was combined and least when tibia alone was done.
We have experienced rebound growth in 2 children, many months after achieving full correction and implant removal. Rebound growth remains enigmatic and difficult to predict but easy to manage and does not preclude a successful outcome. Rebound phenomenon in younger children can be tackled by repeat hemiepiphysiodesis. In our children, we intentionally tried to remove the implant three months after the MA has come to neutral to prevent the rebound phenomenon. This method is also practiced by Meilke et al.7
We have used the principle of tension band plating for guided growth using a 2-holed reconstruction plate instead of the costly 8-plate. Hossein Aslani et al., in 2013 had done a similar study using 2-holed 3.5 mm reconstruction plate and 4 mm non-cannulated cancellous screws/non-cannulated cortical screws for temporary hemiepiphysiodesis around the knee.18 They achieved 86% complete correction in their patients which is higher than the correction that we achieved with our children. Normal physis were more in their study (30) compared to 13 in our study. The mean age at the time of surgery was less in their study than ours. The complications rate were comparable to our study however screw breakage and failure was more in their study (10%). The reconstruction plate that we have used is thinner than the regular pelvic reconstruction plates.
In our study, 82% (9 out of 11) of the complications were observed in children with pathological physis. This was also reported by Weinmann et al. in their study.14 Rather than a physeal shutdown, failure of the implant has been reported to be a significant problem in patients with pathological physes. A good correction was achieved in those in whom the metal work did not fail but predictors for failure has not been identified. In our study screw back out was the most common complication. This was also the commonest complication in study by Kulkarni et al.19 We had one case of breakage of screw, however we did not have any broken plate. Rebound phenomenon was observed in two children, one had a repeat Hemi epiphysiodesis for the rebound growth, and the other child required an osteotomy, since she had almost reached skeletal maturity. Both our children who had overcorrection had missed multiple follow-up visits and this stresses the need for regular monitoring after hemi-epiphysiodesis.
Out of the 9 knees in 7 children which were not corrected, 5 had genu varum, and 4 had genu valgum. Six out of the total seven children were girls. Three children had normal physis and four children had sick physis. Three children had idiopathic genu valgum; three children had Hypophosphatemic rickets, another girl had Ellis Van Creveld syndrome. The idiopathic cases were close to maturity and achieved skeletal maturity before the correction was achieved. The deformities in Hypophosphatemic rickets and Ellis Van Creveld Syndrome are extremely resistant to correction. They also have more implant failure and re surgeries. These conditions need hemi epiphysiodesis at a younger age which will help in decreasing the severity of deformity along with correction of the deformity.
The limitations of this study are the limited number of cases and diverse etiology for the deformity. The average age of the study group is also on the higher side which would have affected the final outcome in some of our patients. Further studies using the standard screw plate constructs in a larger and younger population are recommended.
In summary, low cost custom made reconstruction plate implant gives equal results to traditional tension band plate. The cheap, custom made plate can be used to correct angular deformity. The technique and similar plate can be used in any developing county. No special implant is required or ordered for the correction. The low profile reconstruction plate is different from traditional tension band plate; hence the technique of the reconstruction plate is different (no Keith needle is required), surgical time is short and the technique is effective as tension band plate.
The 2-holed reconstruction plate is significantly less expensive than the 8-plate but has comparable outcome, time for correction and complications. 2-holed reconstruction plate is better suited to Indian population where cost of surgery is an important deciding factor in choosing the form of treatment.
Funding
There is no funding source.
Ethical approval
We received the ethics committee review board approval from our institution before the initiation of this study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Disclosure
None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work.
Funding
None declared.
Declaration of competing interest
The authors declare that they have no conflict of interest.
References
- 1.Blount W.P., Clarke G.R. Control of bone growth by epiphyseal stapling: preliminary report. J Bone Joint surgery Am. 1949;31:464–478. [PubMed] [Google Scholar]
- 2.Metaizeau J.P., Wong-Chung J., Bertrand H., Pasquier P. Percutaneous epiphysiodesis using transphyseal screws (PETS) J Pediatr Orthop. 1998;18:363–369. [PubMed] [Google Scholar]
- 3.Stevens P.M. Guided growth for angular correction a preliminary series using a tension band plate. J Pediatr Orthop. 2007;27:253–259. doi: 10.1097/BPO.0b013e31803433a1. [DOI] [PubMed] [Google Scholar]
- 4.Paley D. Frontal plane mechanical and anatomic axis planning. In: Paley D., editor. Principles of Deformity Correction. first ed. Springer; Berlin: 2005. pp. 61–97. Corr. 3rd printing. Revised edn. [Google Scholar]
- 5.Paley D., Tetsworth K. Mechanical axis deviation of the lower limbs: preoperative planning of uniapical angular deformities of the tibia or femur. Clin Orthop Relat Res. 1992;280:48–64. [PubMed] [Google Scholar]
- 6.Muller K., Muller-Farber J. Indications, localisation and planning osteotomies about the knee. In: Hierholzer G., Muller K., editors. Corrective Osteotomies of the Lower Extremity after Trauma. Springer-Verlag; Berlin: 1984. pp. 195–223. [Google Scholar]
- 7.Mielke C.H., Stevens P.M. Hemiepiphyseal stapling for knee deformities in children younger than 10 years: a preliminary report. J Pediatr Orthop. 1996;16:423–429. doi: 10.1097/00004694-199607000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Ganjwala D., Shah S., Shah S. Use of external and internal fixation in angular deformity around knee. Results of a retrospective study. Indian J Orthop. 2014;48:495–500. doi: 10.4103/0019-5413.139863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gordon J.E., Chen R.C., Dobbs M.B., Luhmann S.J., Rich M.M., Schoenecker P.L. Interobserver and intraobserver reliability in the evaluation of mechanical axis deviation. J Pediatr Orthop. 2009;29:281–284. doi: 10.1097/BPO.0b013e31819b9188. [DOI] [PubMed] [Google Scholar]
- 10.Gorman T.M., Vanderwerff R., Pond M., MacWilliams B., Santora S.D. Mechanical axis following staple epiphysiodesis for limb length inequality. J Bone Joint Surg Am. 2009;91:2430–2439. doi: 10.2106/JBJS.H.00896. [DOI] [PubMed] [Google Scholar]
- 11.Stevens P.M., Maguire M., Dales M.D., Robins A.J. Physeal stapling for idiopathic genu valgum. J Pediatr Orthop. 1999;19:645–649. [PubMed] [Google Scholar]
- 12.Danino B., Rödl R., Herzenberg J.E. Guided growth: preliminary results of a multinational study of 967 physes in 537 patients. J Child Orthop. 2018;12:91–96. doi: 10.1302/1863-2548.12.170050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ballal M.S., Bruce C.E., Nayagam S. Correcting genu varum and genu valgum in children with guided growth: temporary hemiepiphysiodesis using tension band plates. J Bone Joint Surg Br. 2010;92:273–276. doi: 10.1302/0301-620X.92B2.22937. [DOI] [PubMed] [Google Scholar]
- 14.Wiemann J.M., Tryon C., Szalay E.A. Physeal stapling versus 8-plate hemiepiphysiodesis for guided correction of angular deformity about the knee. J Pediatr Orthop. 2009;29:481–485. doi: 10.1097/BPO.0b013e3181aa24a8. [DOI] [PubMed] [Google Scholar]
- 15.Kumar A., Gaba S., Sud A., Mandlecha P., Goel L., Nayak M. Comparative study between staples and eight plate in the management of coronal plane deformities of the knee in skeletally immature children. J Child Orthop. 2016;10:429–437. doi: 10.1007/s11832-016-0758-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klatt J., Stevens P.M. Guided growth for fixed knee flexion deformity. J Pediatr Orthop. 2008;28:626–631. doi: 10.1097/BPO.0b013e318183d573. [DOI] [PubMed] [Google Scholar]
- 17.Stevens P.M., Klatt J.B. Guided growth for pathological physes radiographic improvement during realignment. J Pediatr Orthop. 2008;28:632–639. doi: 10.1097/BPO.0b013e3181841fda. [DOI] [PubMed] [Google Scholar]
- 18.Aslani H., Panjavy B., Bashy R.H.Z., Tabrizi A., Nazari B. The efficacy and complications of 2-hole 3.5mm reconstruction plates and 4mm noncanulated cancellous screws for temporary hemiepiphysiodesis around the knee. J Pediatr Orthop. 2014;34:462–466. doi: 10.1097/BPO.0000000000000115. [DOI] [PubMed] [Google Scholar]
- 19.Kulkarni Ruta M., Ilyas Rushnaiwala Faizaan M., Kulkarni G.S., Rajiv Negandhi, Kulkarni Milind G., Kulkarni Sunil G. Correction of coronal plane deformities around the knee using a tension band plate in children younger than 10 years. Indian J Orthop. 2015;49:208–218. doi: 10.4103/0019-5413.152484. [DOI] [PMC free article] [PubMed] [Google Scholar]