Abstract
Background
Navigated total knee arthroplasty (TKA) improves implant and limb alignment but outliers continue to exist. This study aimed to determine the technical and surgical causes of outliers.
Methods
This retrospective cohort study included 208 patients who had undergone navigated TKA. Limb and implant alignment indices were measured on post-operative CT scans: mechanical femoro-tibial angle (MFTA); coronal femoral angle (CFA); coronal tibial angle (CTA); sagittal femoral angle (SFA); and sagittal tibial angle (STA). Values outside 0°±3° for MFTA and SFA, 90°±3° for CFA, CTA and STA were considered outliers. Intra-operative navigation data and CT scans were evaluated to categorize the causes of sagittal and coronal plane outliers into hip centre error; ankle centre error; heterogeneous tibial cement mantle; malalignment accepted by surgeon; suboptimal knee balance; and no obvious explanation.
Results
Of the 1040 measurements (five per TKA), the overall incidence of outliers was 10.4% (n = 108). Femoral component outliers (CFA + SFA, n = 51) were all attributable to hip centre error. Tibial component outliers (CTA + STA, n = 43) were attributable to ankle centre error (n = 6), heterogeneous cement mantle (n = 20), malalignment accepted by the surgeon (n = 6) and no obvious cause (n = 11). MFTA outliers were attributable to hip centre error (n = 4) or suboptimal knee balance (n = 10).
Conclusions
Surgeon related errors can be minimized by a meticulous operative technique. These results indicate scope for additional technical improvement, especially in hip centre acquisition, which may further reduce the incidence of outliers.
Keywords: Outliers, Computer navigation, Total knee arthroplasty, Hip knee ankle angle, Hip centre error
1. Introduction
The use of computer navigation during total knee arthroplasty (TKA) has been shown to improve implant and limb alignment.1, 2, 3, 4 Despite this, outliers continue to exist after navigated TKA.5,6 Many authors have reported about predictive factors like severe preoperative varus, preoperative flexion contracture, and femoral bowing that may increase the risk of malalignment after navigated TKA.5, 6, 7 However, little is known about technical or surgical factors that may result in outliers after navigated TKA. Understanding these factors may help further reduce outlier incidence. Hence, our aim was to determine the causes of outliers after computer navigated TKA by evaluating intra-operative navigation data and post-operative computed tomography (CT) scans.
2. Materials and methods
This retrospective cohort study was approved by the hospital clinical governance department. Patients were selected from a cohort of 220 patients, operated over a period of 21 months who had participated in a previous prospective trial that included a post-operative CT scan.8 The original trial consisted of patients undergoing navigated unilateral TKA for arthritic changes affecting more than one compartment of the knee irrespective of aetiology, using the OrthoPilot® KneeSuite TKA with either Classic (v4.3 or v4.4) or Smart software modules (BBraun Aesculap, Tuttlingen, Germany) and a Columbus® cruciate-retaining (CR) knee implant (BBraun Aesculap, Tuttlingen, Germany). The OrthoPilot® is an image free passive optical navigation system. Inclusion in this study required a navigated Columbus® CR implant, a complete intra-operative navigation record and a high-quality CT scan. Of the original 220 patients, two had a non-navigated implant, three had no CT scan (no follow up), five had a poor quality CT, one did not have a computer file and one was incorrectly recruited despite having a BMI >40 which was an exclusion criteria for the previous trial. Thus, 208 patients were included in this study. Two hundred and two patients in the study had osteoarthritis (OA), five had rheumatoid arthritis (RA) and one had seronegative inflammatory arthritis. There were 102 (49%) female and 106 (51%) male patients, mean age was 67.7 years [standard deviation (SD): 8.8, range: 40 to 91], mean BMI was 31 (SD: 4.1, range: 21.5 to 40) and mean radiographic preoperative alignment was 3.6° varus (SD: 5°, range: 17° varus to 15° valgus). None of these patients had advanced ipsilateral hip or ankle arthritis, malunited ipsilateral femoral or tibial fractures, osteotomies around the ipsilateral hip, knee, or ankle or an extra-articular deformity not amenable to correction with a TKA. All surgeries were performed by three highly experienced arthroplasty surgeons who routinely used computer navigation for all their TKAs or senior trainees under their direct supervision (6 TKAs only). All patients were operated using a standard medial parapatellar approach except two where a lateral parapatellar approach was used because of a large uncorrectable valgus deformity. All surgeries were performed with a tourniquet which was released at the end of the procedure. The femoral and tibial transmitters were attached to the respective bones using a single 4.5 mm screw with bicortical fixation. The infrared camera/receiver was stationed between 1.8 and 2.0 m distance from the transmitters. Measured resection technique was used for all the cases. The registration process was completed as per the manufacturer's recommendations. This system used kinematic method for recording hip and knee centres. Ankle centre was recorded using anatomic and kinematic method with the Classic module and anatomic method only with the Smart module of the software. The system has built in redundancy to check the accuracy of kinematically determined knee centre in the form of calculating the proximal tibial centre (first degree) and the distal femoral centre (second degree). The proximal tibial centre is the centre of the anterior edge of the anterior cruciate ligament footprint at its tibial attachment. The distal femoral centre is determined twice. First, it is computed as a centre of a circle formed using three points: the anterior femoral cortex point, medial posterior femoral condylar point and lateral femoral posterior condylar point. Second, as a centre of a projected sphere based on four most prominent points of the distal femur: one each from medial and lateral distal femoral condyles and one each from medial and lateral posterior femoral condyles. These four points are acquired in a single step using a femoral alignment block (in contact with distal condyles) with orthogonally placed Y shaped footplate (in contact with posterior condyles) positioned such that the assembly is perpendicular to the sagittal femoral mechanical axis. In the Classic module, the kinematic method provides redundancy to verify the accuracy of the anatomic ankle centre. All surgeons prepared the tibia first. The aim was to perform a tibial cut perpendicular to the mechanical tibial axis in the coronal plane with a posterior slope between 0° and 2° and an effective resection of 10 mm of bone from the least affected tibial condyle. The depth of tibial resection was occasionally tailored to the case, especially in the presence of valgus deformity, knee hyperextension, condylar bone loss, etc. This was followed by femoral preparation. The aim of the distal femoral cut was to effectively resect 9 mm of bone from the least affected femoral condyle such that it was perpendicular to the femoral mechanical axes in the coronal and sagittal planes. Femoral rotation (FR) was set such that it was aligned with the surgical transepicondylar axis (TEA) with at least 3° external rotation to the posterior condylar axis (PCA). This position was verified against Whiteside's line. All of the above three landmarks were taken into consideration while setting FR. This was followed by completion of the anteroposterior femoral resection. Appropriate soft tissue releases were performed whenever required in order to balance the knee joint and restore the lower limb alignment.
Tibial rotation (TR) was the only part of the surgery not navigated. It was set using the ‘floating tibial trial’ technique where the tibial baseplate trial was allowed to assume a functional position relative to the femoral component through the range of motion. This position was then secondarily verified in relation to the medial third of the tibial tubercle. In cases where the floating trial was not optimally oriented with respect to the medial third of the tibial tubercle, the surgeon manipulated the tibial tray to adjust it properly.
A cruciate retaining-deep dished (DD) insert which has a built-in 3° posterior slope was used in all the cases. None of the patients underwent patella resurfacing. Patelloplasty and peripheral patellar denervation using electrocautery were performed in all cases.
If the executed tibial and distal femoral cuts were within 1mm/1° of the planned cut, they were considered as acceptable. All the surgeons accepted a final coronal alignment of 180° ± 3° and a balanced knee within ±2°.
The navigation system routinely recorded all intra-operative data. All patients had a CT scan performed at six weeks post-operatively. The Imperial knee protocol that scans the entire femoral head, 10 cm on either side of the knee joint line and 2–3 cm on either side of the tibiotalar joint was used.9 The following indices of limb and implant alignment on the CT images were measured: mechanical femoro-tibial angle (MFTA); coronal femoral angle (CFA); coronal tibial angle (CTA); sagittal femoral angle (SFA); and sagittal tibial angle (STA), as described previously.8 A value outside of 0°±3° for MFTA and SFA and 90°±3° for CFA, CTA, and STA was considered an outlier. All measurements were made by an experienced musculoskeletal radiologist (BRKS) who did not participate in patient care. All measurements were performed on CarestreamVue, v11.4.1.1011 (Carestream Health, Hemel Hempstead, United Kingdom) picture archiving and communications system (PACS). This system has an accuracy of up to 1/100 of a degree and 1/100 of a mm for angular and linear measurements respectively. For the purpose of reporting results, the angular measurements were rounded to the nearest degree. The multiplanar reconstruction (MPR) function of PACS was used to ensure accurate determination of component alignment in the coronal and sagittal planes which eliminates any resultant error from residual knee joint deformity at the time of imaging. We did not measure FR on postoperative CT scans because assessment of the causes of FR outliers requires determination of accuracy of registration of landmarks like femoral epicondyles and PCA during surgery which is difficult post-operatively. We did not measure TR as it was set intra-operatively without using computer navigation.
The coronal and sagittal plane outliers (MFTA, CFA, CTA, SFA and STA) were assessed further using navigation and CT data to determine their most likely cause by the senior author who also was one of the operating surgeons (FP). Based on the assessment, we were able to categorize the cause behind an outlier into one of the following:
-
a)
hip centre error- When a perpendicular through the centre of the distal articular surface of the prosthetic femur in the coronal or sagittal plane was not within an 18 mm diameter (9 mm radius) circle centred around the true hip centre (determined on CT) in any plane (Fig. 1). The 18 mm diameter value was chosen as it is the built-in redundancy value used by the computer navigation system to verify the hip centre acquired intra-operatively.
-
b)
ankle centre error- When a perpendicular through the centre of the proximal articular surface of the prosthetic tibia in the coronal or sagittal plane was not within an 18 mm diameter (9 mm radius) circle centred around the true ankle centre (determined on CT) in any plane (Fig. 2). Similar to the above, the 18 mm diameter value was chosen as it is the built in redundancy value used by the computer navigation system to verify the ankle centre acquired intra-operatively.
-
c)
error due to heterogeneous tibial cement mantle- When the angle between the undersurface of the tibial baseplate and the cement-bone junction was >2° in either coronal or sagittal planes (Fig. 3)
-
d)
malalignment accepted by the surgeon- Following bone cuts, the surgeon had accepted malalignment as evident from navigation data.
-
e)
suboptimal knee balance- When the angle between the tangents drawn to the distal femoral and proximal tibial surface was >2° in the coronal plane (Fig. 4)
-
f)
no obvious explanation- When all the above causes were ruled out.
Fig. 1.
Hip centre error: YZ is a perpendicular to the distal articular surface of the prosthetic femur (XX′) through its centre (Y). The proximal projection of YZ is beyond the limits of a circle with a 9 mm radius around the true hip centre (HC) in the transverse plane.
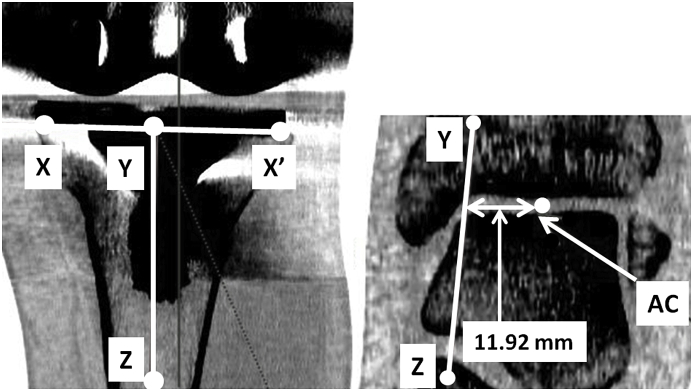
Fig. 2.
Ankle centre error: YZ is a perpendicular to the tibial baseplate (XX′) through its centre (Y). The distal projection of YZ is beyond the limits of a circle with a 9 mm radius around the true ankle centre (AC) in the coronal plane.
Fig. 3.

The angle between the tangents through the undersurface of the tibial baseplate and the bone-cement junction is > 2° (4.12°) suggestive of a heterogeneous tibial cement mantle.
Fig. 4.

The angle subtended between the tangents through the distal femoral and proximal tibial surface in the coronal plane is > 2° (3.22°) suggestive of suboptimal knee balance.
An outlier was categorized into hip (a) or ankle (b) centre error only after c-e were ruled out. Hip and ankle centre errors were ascertained using MPR function of PACS.
All descriptive data are expressed as mean, SD, and range. Proportions are expressed as percentages.
3. Results
A total of 1040 alignment indices were measured in the 208 TKAs (five per TKA). The overall incidence of outliers was 10.4% (n = 108). All indices showed outliers with the highest being for STA and CFA (17% and 16% respectively) and the lowest for CTA (4%) (Table 1). 118 TKAs had all five alignments within range (56.7%), 73 TKAs had one index that was an outlier (35.1%), 16 (7.7%) had two and 1 (0.5%) had three. The most prevalent causative factor for coronal and sagittal plane outliers (n = 108) was hip centre error (51%) and the least being ankle centre error and accepted malalignment (both 5.5%) (Table 2). Femoral component outliers (CFA and SFA; n = 51) were all attributable to hip centre error (Table 2). Tibial component outliers (CTA and STA; n = 43) were attributable to ankle centre error (n = 6), heterogeneous cement mantle (n = 20), malalignment accepted by the surgeon (n = 6) and no obvious cause (n = 11) (Table 2). MFTA outliers were attributable to hip centre error (n = 4) or suboptimal knee balance (n = 10) (Table 2).
Table 1.
Measured alignment indices from CT scans.
| Index | Mean ± SD (range) | No. of outliers (%) |
|---|---|---|
| Mechanical femoro-tibial angle (MFTA) | −0.4° ± 1.9° (−7.0°–6.0°) | 14 (7%) |
| Coronal femoral angle (CFA) | 91.6° ± 1.9° (82.0°–97.0°) | 33 (16%) |
| Coronal tibial angle (CTA) | 89.0° ± 1.4° (80.0°–92.0°) | 8 (4%) |
| Sagittal femoral angle (SFA) | 0.9° ± 1.9° (−5.0°–8.0°) | 18 (9%) |
| Sagittal tibial angle (STA) | 88.2° ± 1.6° (85.0°–92.0°) | 35 (17%) |
*SD: standard deviation; MFTA-negative values indicate varus and positive values indicate valgus alignment; CFA and CTA-acute angles denote varus alignment and obtuse angles denote valgus alignment of the respective prosthetic components; SFA-positive values denote flexion and negative values denote extension; STA-acute angles denote posterior slope and obtuse angles denote anterior slope.
Table 2.
Causative factors for sagittal and coronal plane outliers in order of incidence.
| No. | Causative factor | Number of cases (≈%) |
|---|---|---|
| 1 | Hip centre error | 55 (51%) |
| 2 | Heterogeneous cement mantle | 20 (18.5%) |
| 3 | No obvious cause | 11 (10%) |
| 4 | Suboptimal knee balance | 10 (9.5%) |
| 5 | Ankle centre error | 6 (5.5%) |
| 6 | Malalignment accepted by the surgeon | 6 (5.5%) |
| Total | 108 (100%) |
4. Discussion
The rationale behind the use of computer navigation during TKA is to improve implant and limb alignment and to minimize the incidence of outliers. However, outliers continue to exist after navigated TKA with a reported incidence between 7% and 20.4% for coronal lower limb alignment.5, 6, 7,10,11 Although clinical predictors for outliers like severe varus deformity and femoral bowing have been reported,5,6 there is no literature on technical or surgical factors responsible for outliers after navigated TKA. Hip centre error was responsible for a little over half of the outliers (51%) in our study. Inaccurate acquisition of the hip centre (and ankle centre) may either be due to the surgeon or the computer navigation system. An inaccurate hip centre can affect CFA, SFA, and MFTA. The navigation system registers the functional hip centre kinematically and could differ from the anatomic hip centre determined on CT scan. Other authors have found that different methods of identifying hip centres give varying results; the kinematic and fluoroscopically determined hip centre differed by up to 5 mm12; and between kinematic and geometric hip centre by up to 14 mm.13 This most likely explains error in hip centre registration as a common cause for outliers after navigated TKA as determined on post-operative CT images. Kinematic hip centre determination involves performing a hip circumduction manoeuvre. Originally, computer navigation systems recorded the hip centre using an iliac tracker and a femoral tracker so that any movement of the pelvis during circumduction could be accounted for.14,15 However, an additional iliac tracker adds to surgical trauma and it is difficult to incorporate it in the sterile surgical field. A cadaveric study demonstrated that there was no statistically significant difference in location of hip centre with or without an iliac tracker.16 Contemporary navigation systems record kinematic hip centre without an iliac tracker. This involves performing a circumduction manoeuvre by moving the femur against a stable pelvis. During this process it is assumed that the spatial location of the pelvis is relation to the infra red navigation camera is fixed. Movement of the pelvis while performing this manoeuvre can result in error in hip centre determination. A common situation where this can happen is when the side support used during TKA is not unfastened and pushed out of the way to allow an unrestricted circumduction manoeuvre. In this case the thigh may push against the unyielding side support causing the pelvis to be moved, thus resulting in an error. This is especially likely in obese patients with large sized thighs. It is now our routine practice to unfasten the side support and push it out of the way in order to allow unrestricted hip circumduction. The side support is repositioned after the hip centre is acquired. There is sufficient slack in the drapes to allow doing this without compromising the sterility of the operating field. Furthermore, no one should touch the computer-camera system at this stage as even the slightest movement can result in an inaccurate hip centre acquisition. We also employ another check to rule out hip centre registration error during surgery.16 We determine the coronal distal femoral articular angle (DFAA) on preoperative lower limb alignment (hip-knee-ankle) radiographs that are routinely obtained for all our cases. This is the angle subtended by a tangent through the distal femoral articular surface with the femoral mechanical axis in the coronal plane. We would suspect an error in hip centre registration if there is a discrepancy of >3⁰ between radiographic coronal DFAA and that displayed by computer navigation. We are aware that radiographic DFAA does not take into account differential cartilage wear between the femoral condyles unlike the DFAA determined using navigation. Keeping this in mind, if there is a strong suspicion of error, we register the hip centre again. A stiff hip due to any aetiology that precludes an unrestricted hip circumduction is another plausible cause of hip centre error. None of the patients in our cohort had advanced ipsilateral hip arthritis and a resultant stiff hip. Also, it is our standard practice to replace an arthritic hip before the knee in cases with co-existing hip and knee arthritis. The accuracy of hip centre determination also depends upon the algorithm used by the computer system. The algorithm used by this system has been reported to be accurate and precise.16 Stindel et al. reported an algorithm that was found to be robust to noise, compensated for pelvic motion, and could be used in cases with restricted hip motion.17 And finally, cumulative errors are potentially occurring within the system during the acquisition process due to several factors like tracker orientation, rate of data collection, camera refreshment rate (60 Hz) and computer-camera communication which are difficult to identify. It is suggested that surgeons exercise the utmost caution while acquiring hip centre during surgery in order to avoid the commonest cause of outliers in this study.
The second commonest cause of outliers in this study was a heterogeneous tibial cement mantle (18.5%). Cementation and impaction of implants can introduce considerable errors in alignment despite accurate resection planes.18 Catani et al. recommend checking the final alignment before the cement sets.18 Howie et al. recommend concentrating on the implantation process in order to improve alignment and reduce outliers.19 Lower limb alignment can be changed by a small magnitude by applying appropriate force (varus/valgus or flexion/extension) before the cement sets. Alignment of individual components can also be verified using a tracked plate-probe and altered to a small extent before the cement sets. However, there is a risk of scratching the implant with the tracked plate-probe and hence we do not use it in our practice. The best way to avoid errors due to a heterogeneous cement mantle is by ensuring a meticulous cementation and implantation technique. One may consider implanting femoral and tibial components separately with different batches of cement which may give enough working time with the cement to ensure optimum component implantation.
Error in ankle centre registration was responsible for about 5.5% outliers in this study. The navigation system used in this study determines the anatomic ankle centre by first establishing a primary axis across the centres of the medial and lateral malleoli that are obtained by palpation. This is followed by palpating the anterior ankle joint centre along the central tibial axis. Intersection of a perpendicular through the anterior ankle joint point with the primary axis provides the ankle centre. Establishing ankle centre using the centres of medial and lateral malleoli has been reported to be accurate and precise (4.5 ± 4.1 mm lateral error; 2.7 ± 4.5 mm posterior error).20 However, determination of the malleoli or the anterior ankle joint point can be difficult in obese patients and patients with lower limb oedema which may exaggerate the error significantly enough to result in an outlier. We routinely confirm the placement of the tibial cutting block prior to its resection using a drop rod in order to verify that there was no major error in ankle centre registration. The kinematic method of ankle centre registration provided redundancy to the anatomically acquired one in the Classic module of the navigation software used in this study. This redundancy mechanism was not a part of the Smart module of the software. However, the sagittal and coronal tibial component positions and the MFTA which are all linked to the accuracy of ankle centre acquisition were reported to be similar between the Classic and Smart modules of this navigation system.8
Suboptimal knee balance was responsible for 9.5% of outliers in this study as observed on CT. As CT images depict the lower limb under non-weight bearing conditions, it is not possible to infer about knee balance under weight-bearing conditions. Weight-bearing may correct or exaggerate the suboptimal knee balance. Intra-operative knee balance is dependent on the surgeon's assessment and can vary between surgeons. In addition, intra-operative data is obtained from an anaesthetized lower limb with open soft tissues and an inflated tourniquet.
For six outliers, the operating surgeon had accepted residual malalignment during surgery as understood from the navigation data. All six pertain to STA i.e. tibial slope. A posterior slope of 4° was accepted in 4 cases and 5° in 2 cases. As the tibial insert has a built-in posterior slope of 3°, this resulted in an effective posterior slope of 7° and 8° respectively which is not excessive as such. In retrospect, it is not possible to state specifically as to why the surgeon accepted these malalignment. It is likely that the surgeons deemed it appropriate to accept excessive posterior slope in order to achieve the final target of a balanced knee with acceptable lower limb alignment. All the participating surgeons are high volume arthroplasty surgeons with a large experience of performing navigated TKAs with this system prior to this study (FP > 1000, JB > 500, DA >300 navigated TKAs). Moreover, this represents only 0.6% (6/1040) of all the alignment values assessed so only affects a small number of cases.
There was no obvious cause for 11 outliers (10%). We suspect these may be due to errors from the computer system, tracking-camera system, or unstable trackers. Clarke et al.21 reported an error range of 2.3 mm for distance measurements with one commercially available camera system. Other possible sources of error include blood stained reflectors on the trackers, obstruction in the line of sight between camera and the trackers, excessively bright ambient light, projection angle of the camera on the trackers or a camera positioned outside the recommended 1.8 m–2.0 m distance from the trackers.22
This study has a number of limitations. Errors due to inaccurate acquisition of knee centre cannot be discerned from post-operative CT images as the peri-articular knee anatomy is altered following TKA. It is possible that errors in the intra-operative determination of mechanical femoral and tibial axes were actually due to an incorrect knee centre acquisition rather than an incorrect hip or ankle centre acquisition respectively. However, this possibility is very low due to the built-in redundancy in the system to verify the kinematically acquired knee centre using proximal tibial and distal femoral knee centres. Also presence of a flexion deformity at the time of CT scan may affect the measurement of MFTA (but not CFA/SFA or CTA/STA due to the use of the MPR function of PACS which limits errors in bony alignment). However, we do not expect any significant flexion deformity at 6 weeks after surgery and believe that any resulting error would be small as such. Medio-lateral positioning of the femoral and tibial prosthetic components can affect the position of the respective perpendiculars drawn through the centre of the distal femoral or proximal tibial surfaces, thus affecting the assessment of hip and ankle centre errors respectively. This however, is unlikely to have any significant effect as we have used a wide acceptable range of 18 mm due to reasons stated earlier. This cohort included patients operated using two different software modules- Classic (n = 105) and Smart (n = 103) of the OrthoPilot® KneeSuite TKA system. However, implant and limb alignment indices and the incidence of outliers have been reported to be similar between these two modules.8 Lastly, we did not determine intra and inter-observer variability for the indices measured on CT scans. However, previous studies have reported excellent intra and inter-observer reliability for measurement of indices on CT after TKA.23,24 Although not strictly a limitation, this study only pertains to one navigation system. Generalization of these findings must be done with caution as all navigation systems are not equivalent.25 Accuracy may be system dependant due to inherent differences in hardware, algorithms and software.
Our study also has its strengths. Most studies reporting on outliers after navigated TKA are based on standing long leg radiographs which are not completely free from error due to limb rotation or flexion deformity.26 Moreover, these radiographs are under weight-bearing condition unlike supine CT scans; and muscle tone and gravity may alter lower limb alignment.27 In this regard, conditions during supine CT scans are closer to intra-operative conditions recorded by the navigation system than standing long leg radiographs.
5. Conclusions
This study has identified potential causes of outliers after navigated TKA which can be broadly grouped into surgeon related and systemic. Errors due to inaccurate acquisition of landmarks, improper prosthetic cementation and suboptimal knee balance can be attributed to the surgeon and these can be minimized by a meticulous surgical technique. Systemic errors may arise from the computer, tracking system or camera device. Over the last decade, there have been substantial improvements in computer navigation systems. However, there appears to be scope for additional improvement, especially in the process of hip centre acquisition which may further reduce the incidence of outliers after navigated TKA.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
The authors thank Mr. Joseph Baines, Dr. Benjamin R. K. Smith, Dr. Mohammed Almustafa and the Radiology Department, particularly Elizabeth Philip and Fozia Zaheer, who all contributed to the original study that generated the data used in this retrospective analysis. The authors also thank Angela H. Deakin for her assistance with the study and preparation of the manuscript.
References
- 1.Moskal J.T., Capps S.G., Mann J.W., Scanelli J.A. Navigated versus conventional total knee arthroplasty. J Knee Surg. 2014;27(3):235–248. doi: 10.1055/s-0033-1360659. [DOI] [PubMed] [Google Scholar]
- 2.Hetaimish B.M., Khan M.M., Simunovic N., Al-Harbi H.H., Bhandari M., Zalzal P.K. Meta-analysis of navigation vs conventional total knee arthroplasty. J Arthroplast. 2012;27(6):1177–1182. doi: 10.1016/j.arth.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 3.Fu Y., Wang M., Liu Y., Fu Q. Alignment outcomes in navigated total knee arthroplasty: a meta-analysis. Knee Surg Sport Traumatol Arthrosc. 2012 Jun;20(6):1075–1082. doi: 10.1007/s00167-011-1695-6. [DOI] [PubMed] [Google Scholar]
- 4.Mason J.B., Fehring T.K., Estok R., Banel D., Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplast. 2007;22(8):1097–1106. doi: 10.1016/j.arth.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 5.Chowdhry M., Bamne A.B., Na Y.G., Kang Y.G., Kim T.K. Prevalence and predictors of post-operative coronal alignment outliers and their association with the functional outcomes in navigated total knee arthroplasty. J Arthroplast. 2014;29(12):2357–2362. doi: 10.1016/j.arth.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 6.Mullaji A.B., Shetty G.M., Lingaraju A.P., Bhayde S. Which factors increase risk of malalignment of the hip-knee-ankle axis in TKA? Clin Orthop Relat Res. 2013;471(1):134–141. doi: 10.1007/s11999-012-2520-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miyasaka T., Kurosaka D., Saito M., Omori T., Ikeda R., Marumo K. Accuracy of computed tomography based navigation assisted total knee arthroplasty: outlier analysis. J Arthroplast. 2017;32(1):47–52. doi: 10.1016/j.arth.2016.05.069. [DOI] [PubMed] [Google Scholar]
- 8.Sciberras N.C., Almustafa M., Smith B.R.K., Allen D.J., Picard F., Deakin A.H. A randomized controlled trial to compare component placement in navigated total knee arthroplasty using original and streamlined registration processes. Arthroplast Today. 2016;3(2):111–117. doi: 10.1016/j.artd.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henckel J., Richards R., Lozhkin K. Very low-dose computed tomography for planning and outcome measurement in knee replacement. The imperial knee protocol. J Bone Joint Surg Br Vol. 2006;88(11):1513–1518. doi: 10.1302/0301-620X.88B11.17986. [DOI] [PubMed] [Google Scholar]
- 10.MacDessi S.J., Jang B., Harris I.A., Wheatley E., Bryant C., Chen D.B. A comparison of alignment using patient specific guides, computer navigation and conventional instrumentation in total knee arthroplasty. The Knee. 2014;21(2):406–409. doi: 10.1016/j.knee.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Stockl B., Nogler M., Rosiek R., Fischer M., Krismer M., Kessler O. Navigation improves accuracy of rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2004;426:180–186. doi: 10.1097/01.blo.0000136835.40566.d9. [DOI] [PubMed] [Google Scholar]
- 12.Victor J., Hoste D. Image-based computer-assisted total knee arthroplasty leads to lower variability in coronal alignment. Clin Orthop Relat Res. 2004;428:131–139. doi: 10.1097/01.blo.0000147710.69612.76. [DOI] [PubMed] [Google Scholar]
- 13.Speirs A.D., Benoit D.L., Beaulieu M.L., Lamontagne M., Beaule P. The accuracy of the use of functional hip motions on localization of the center of the hip. HSS J. 2012;8(3):192–197. doi: 10.1007/s11420-012-9296-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Delp S.L., Stulberg S.D., Davies B., Picard F., Leitner F. Computer assisted knee replacement. Clin Orthop Relat Res. 1998;354:49–56. doi: 10.1097/00003086-199809000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Stulberg S.D., Picard F., Saragaglia D. Computer assisted total knee arthroplasty. Oper Tech Orthop. 2000;10(1):25–39. [Google Scholar]
- 16.Picard F., Leitner F., Gregori A., Martin P. A cadaveric study to assess the accuracy of computer-assisted surgery in locating the hip center during total knee arthroplasty. J Arthroplast. 2007;22(4):590–595. doi: 10.1016/j.arth.2006.04.027. [DOI] [PubMed] [Google Scholar]
- 17.Stindel E., Gil D., Briard J.L., Merloz P., Dubrana F., Lefevre C. Detection of the center of the hip joint in computer-assisted surgery: an evaluation study of the Surgetics algorithm. Comput Aided Surg. 2005;10(3):133–139. doi: 10.3109/10929080500229975. [DOI] [PubMed] [Google Scholar]
- 18.Catani F., Biasca N., Ensini A. Alignment deviation between bone resection and final implant positioning in computer-navigated total knee arthroplasty. J Bone Joint Surg Am Vol. 2008;90(4):765–771. doi: 10.2106/JBJS.G.00293. [DOI] [PubMed] [Google Scholar]
- 19.Howie D.F., Love G.J., Deakin A.H., Kinninmonth A.W. Intra-operative deviation in limb alignment occurring at implantation in total knee arthroplasty. The Knee. 2015;22(1):47–50. doi: 10.1016/j.knee.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 20.Siston R.A., Daub A.C., Giori N.J., Goodman S.B., Delp S.L. Evaluation of methods that locate the center of the ankle for computer-assisted total knee arthroplasty. Clin Orthop Relat Res. 2005;439:129–135. doi: 10.1097/01.blo.0000170873.88306.56. [DOI] [PubMed] [Google Scholar]
- 21.Clarke J.V., Deakin A.H., Nicol A.C., Picard F. Measuring the positional accuracy of computer assisted surgical tracking systems. Comput Aided Surg. 2010;15(1-3):13–18. doi: 10.3109/10929081003775774. [DOI] [PubMed] [Google Scholar]
- 22.Bae D.K., Song S.J. Computer assisted navigation in knee arthroplasty. Clin Orthop Surg. 2011;3(4):259–267. doi: 10.4055/cios.2011.3.4.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chao T.W., Geraghty L., Dimitriou P., Talbot S. Averaging rotational landmarks during total knee arthroplasty reduces component malrotation caused by femoral asymmetry. J Orthop Surg Res. 2017;12(1):74. doi: 10.1186/s13018-017-0575-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mizu-uchi H., Matsuda S., Miura H., Okazaki K., Akasaki Y., Iwamoto Y. The evaluation of post-operative alignment in total knee replacement using a CT-based navigation system. J Bone Joint Surg Br Vol. 2008;90:1025–1031. doi: 10.1302/0301-620X.90B8.20265. [DOI] [PubMed] [Google Scholar]
- 25.Carli A., Aoude A., Reuven A., Matache B., Antoniou J., Zukor D. Inconsistencies between navigation data and radiographs in total knee arthroplasty are system-dependent and affect coronal alignment. Can J Surg. 2014;57(5):305–313. doi: 10.1503/cjs.031313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holme T.J., Henckel J., Hartshorn K., Cobb J.P., Hart A.J. Computed tomography scanogram compared to long leg radiograph for determining axial knee alignment. Acta Orthop. 2015;86(4):440–443. doi: 10.3109/17453674.2014.1003488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Livshetz I., Brin Y.S., Holcroft C., Antoniou J., Zukor D.J. Deviations between intra-operative navigation data and post-operative weight-bearing x-rays. Comput Aided Surg. 2010;15(1-3):56–62. doi: 10.3109/10929088.2010.480884. [DOI] [PubMed] [Google Scholar]