Abstract
Purpose
Sweetened beverage consumption is associated with type 2 diabetes (T2D) and LADA. We investigated to what extent this association is mediated by BMI and whether it is modified by genotypes of HLA, TCF7L2 rs7903146, or FTO rs9939609.
Methods
Swedish case–control data including incident cases of LADA (n = 386) and T2D (n = 1253) with matched population-based controls (n = 1545) was used. We estimated adjusted ORs of diabetes (95% CI) in relation to sweetened beverage intake (per daily 200 mL serving) and genotypes. The impact of BMI was estimated using causal mediation methodology. Associations with HOMA-IR and HOMA-B were explored through linear regression.
Results
Sweetened beverage intake was associated with increased risk of LADA (OR 1.15, 95% CI 1.03–1.29) and T2D (OR 1.21, 1.11–1.32). BMI was estimated to mediate 17% (LADA) and 56% (T2D) of the total risk. LADA was associated with risk variants of HLA (3.44, 2.63–4.50) and TCF7L2 (1.27, 1.00–1.61) but not FTO. Only among non-carriers of high-risk HLA genotypes was sweetened beverage intake associated with risk of LADA (OR 1.32, 1.06–1.56) and HOMA-IR (beta = 0.162, p = 0.0047). T2D was associated with TCF7L2 and FTO but not HLA, and the risk conferred by sweetened beverages appeared modified by FTO (OR 1.45, 95% CI 1.21–1.73 in non-carriers).
Conclusions
Our findings suggest that sweetened beverages are associated with LADA and T2D partly through mediation by excess weight, but possibly also through other mechanisms including adverse effects on insulin sensitivity. These effects seem more pronounced in individuals without genetic susceptibility.
Electronic supplementary material
The online version of this article (10.1007/s00394-019-01893-x) contains supplementary material, which is available to authorized users.
Keywords: Autoimmune diabetes, Latent autoimmune diabetes in adults, T2D, Sweetened beverage, Genotype, BMI
Introduction
Sweetened beverage consumption has been associated with increased risk of type 2 diabetes (T2D) [1] and childhood type 1 diabetes (T1D) [2]. In a recent study based on Swedish data, we showed that sweetened beverage consumption may also increase the risk of latent autoimmune diabetes in adults (LADA) [3]. One proposed mechanism for its association with diabetes is that high consumption of sweetened beverages may lead to excess energy intake resulting in increased BMI [4], which in turn is a strong risk factor not only for T2D [5], but also for autoimmune diabetes [6, 7]. However, high BMI does not seem to fully explain the associations [1, 3]; there may also be direct effects on glucose metabolism including increased insulin resistance [8] and induced beta cell apoptosis [9].
Genetic susceptibility may modify the association between sweetened beverage intake and autoimmune diabetes. Findings in children suggest that consumption confers an elevated risk only among carriers of high-risk human leucocyte antigen (HLA) genotypes [2], which is the strongest genetic determinant of T1D [10]. LADA is a hybrid form of diabetes associated with HLA but also with transcription factor 7-like 2 (TCF7L2) [11], which confers the strongest genetic predisposition to T2D [12]. TCF7L2 is involved in glucose homeostasis through the Wnt signaling pathway [13] and the minor T allele has been associated with impaired insulin secretion [14]. Furthermore, a recent meta-analysis found sweetened beverage intake to be associated with increases in fasting glucose and insulin [15]. Another gene of potential interest is the fat mass and obesity-associated (FTO) gene, which has been associated with overweight [16], possibly through alterations in satiety perception, energy intake [17], and nutrient preferences [18], but also associates with risk of T2D [19]. Sugar-sweetened beverages are likely to promote weight gain [20] and therefore it may be hypothesized that consumption would be more detrimental in terms of diabetes risk among individuals with genetic predisposition to overweight. To the best of our knowledge, only one previous study has investigated the possible interaction between sweetened beverage consumption and genetic susceptibility on the risk of T2D [21]. No evidence of interaction with a genetic risk score was found, but the role of individual genes was not investigated. Whether the association between sweetened beverages and autoimmune diabetes in adults is modified by genetic susceptibility has not been investigated previously.
Our aim was to clarify the influence of sweetened beverage consumption on LADA and T2D risk by investigating whether the association is modified by genotypes of HLA, TCF7L2, or FTO. These genes are suitable candidate genes for potential interaction with sweetened beverage intake due to their relatively strong genetic contribution to diabetes or overweight. We also aimed to explore underlying mechanisms and proportion of the observed association mediated by BMI.
Subjects and methods
Study population and design
This study is based on incident cases of LADA and T2D included in the ESTRID Study (Epidemiological Study of Risk Factors for LADA and Type 2 Diabetes, http://www.ki.se/imm/estrid), a Swedish case–control study ongoing since 2010 that has been described in detail elsewhere [22]. Cases were recruited from ANDIS (All New Diabetics in Scania, http://andis.ludc.med.lu.se), a diabetes registry aiming at including all new cases of diabetes identified and diagnosed by the health care providers within the county of Scania, and classify them based on clinical and genetic characteristics [23]. All incident cases of LADA and a random sample of T2D cases are invited to participate in ESTRID. Participation includes responding to an extensive questionnaire covering a wide range of health and lifestyle factors. The cases respond to the mailed questionnaire soon after diagnosis with 79% response rate. Controls in ESTRID are recruited from the Swedish Population Register through random selection and matched to the cases based on time and geographical region. These controls provide questionnaire data but no blood samples. For that reason, the present study instead uses data for diabetes-free controls from the EIRA Study (Epidemiological Investigation on Rheumatoid Arthritis, http://www.eirasweden.se), an ongoing, population-based case–control study utilizing similar methodology and questionnaire as ESTRID. The controls, randomly selected from the Swedish Population Register, were post-matched to the ESTRID cases by age and sex.
Eligible for the present study were all patients (n = 386 LADA, n = 1253 T2D) included in ESTRID until July 2017, and controls collected in EIRA 2005–2014 (n = 1545), aged ≥ 35 years and with complete information on lifestyle covariates and at least one of the three genetic factors. This study was approved by the Regional Ethical Review Board in Stockholm and all participants provided informed consent.
Sweetened beverage and covariates
Habitual diet, as an average during the preceding year, was assessed using a validated [24–26] food-frequency questionnaire (FFQ). The FFQs were almost identical for ESTRID and EIRA and designed to cover usual diet. Patients with diabetes were specifically instructed to report their diet as it used to be prior to diagnosis. Sweetened beverages were assessed as the total intake of soft drinks/sodas, diluted syrups and nectars, but not 100% fruit juices. Consumption was reported as number of daily or weekly 200 mL servings. Validation of FFQ-reported sweetened beverage intake against four 1-week diet records in a subsample of 129 women showed a correlation of 0.6 (Wolk, unpublished results).
The ESTRID and EIRA questionnaires included identical questions on covariates. Self-reported height and weight were used to calculate BMI as weight in kilograms divided by the squared height in meters. Highest attained education was categorized as primary school, upper secondary school, or university. Leisure time physical activity during the preceding year (prior to diagnosis for cases) was reported as one of four response options ranging from sedentary to regularly active. Smoking habits of individuals were categorized as never smoker, former, or current smoker. Alcohol intake was estimated from the FFQ and categorized into none, 0.01–4.9 g/day, 5–14.9 g/day, and ≥ 15 g/day.
Diabetes classification
Age at diagnosis, glutamic acid decarboxylase autoantibodies (GADA), and fasting C-peptide were used to determine diabetes subtype. Details of the serological assay methods have been described elsewhere [23]. GADA was measured with an enzyme linked immunosorbent assay (ELISA) with 84% sensitivity and 98% specificity at 10.7 IU/mL cut-off level [27]. Values above 250 IU/mL were censored at 250 IU/mL. Concentration of C-peptide was measured using Cobas e601 analyzer (Roche Diagnostics, Mannheim, Germany) or IMMULITE 2000 (Siemens Healthcare Diagnostics Product Ldt., Llanberis, UK). LADA was defined as age ≥ 35 years, GADA ≥ 10 IU/mL, and C-peptide ≥ 0.2 nmol/L (IMMULITE) or ≥ 0.3 nmol/L (Cobas e 601). Cases were classified as having T2D if age ≥ 35 years, GADA < 10 IU/mL, and C-peptide ≥ 0.60 nmol/L (IMMULITE) or ≥ 0.72 nmol/L (Cobas e 601). Homeostatic model assessment of insulin resistance (HOMA-IR) and beta cell function (HOMA-B) were calculated based on fasting plasma glucose and C-peptide [28].
Genetic analyses
Blood samples for genotyping of patients were analyzed at the Clinical Research Center in Malmö, Sweden, using iPlex Gold Technology (Sequenom, San Diego, CA, USA). Missing genotypes were imputed for a subset using Infinium CoreExome v1.1 (Illumina, San Diego, CA, USA), based on the Haplotype Reference Consortium (http://www.haplotype-reference-consortium.org/; version r1.1 2016) reference panel. Controls were genotyped based on GWAS data generated through an Illumina Global Screening array or an Infinium Illumina 300K immunochip custom array (Illumina, San Diego, CA, USA). Genetic data used in the present study include three single nucleotide polymorphisms (SNPs) within the HLA gene region (rs3104413, rs2854275, rs9273363), one SNP within the TCF7L2 gene (rs7903146), and one SNP within the FTO gene (rs9939609). HLA genotyping was done according to previously described methodology based on the three SNPs specified above, which have shown an accuracy of 99.3% [29]. Patients and controls were categorized as carriers of high-risk HLA genotypes: DR4-DQ8, DR4/3-DQ8, DR3/4, DR3/3, DR4/4, and DQA1*0501-DQB1*0201, or low/moderate-risk genotypes: DR3/x, DR4/x, DR4-DQ7, DRx/x, where x = neither DR4 nor DR3. This categorization was based on the literature [30, 31] and frequency distributions in our study population. Participants were considered carriers of the risk variants of TCF7L2 rs7903146 and FTO rs9939609 if they had at least one risk allele (i.e., genotypes TT/TC in TCF7L2 rs7903146, and AA/AT in FTO rs9939609).
Statistical analyses
Statistical Analysis Software (SAS) 9.4 (SAS Institute, Cary, NC, USA) was used for statistical analyses. Characteristics for patients and controls were presented as proportions, means, or medians (for skewed data), together with standard deviations (SD; for means) or interquartile range (IQR; for medians). Two-tailed p values were calculated by χ2 (proportions), Student’s t test (means), and Kruskal–Wallis H (medians) tests.
Conditional logistic regression was used to estimate odds ratios (OR) and 95% confidence intervals (CI) for the association between sweetened beverage consumption or genotype, and risk of LADA or T2D. Sweetened beverage consumption was analyzed in four categories and per one 200 mL daily serving increment in intake. Stratified analysis of the association between sweetened beverage intake and diabetes risk was done across genotypes of HLA (high or low/moderate risk), TCF7L2 rs7903146 (TT/CT or CC) and FTO rs9939609 (AA/AT or TT). We also examined the presence of interaction, defined as departure from additivity of effects, between high sweetened beverage consumption (> 2 servings/day) and risk genotype by calculating attributable proportion due to interaction (AP). A significant positive interaction is indicated when AP > 0 and the confidence interval does not include 0 [32]. The change in loge transformed HOMA-IR and HOMA-B, expressed as the regression coefficient, associated with one daily serving increase in sweetened beverages was assessed using linear regression.
All analyses were conditioned on age and sex (post-matching variables). Model 1 was adjusted for education, physical activity, smoking, and alcohol intake. Model 2 was also adjusted for BMI which was considered a mediator. Results from model 1 will be discussed in the text unless otherwise specified. Adjustment for dietary factors (red/processed meat, fatty fish, vegetables, fruit, sweet/salty snacks, and coffee) had little impact on the observed associations and were not included in the final models presented in this paper.
Using the approach suggested by VanderWeele [33], we assessed the mediating effect of BMI by estimating the natural direct and indirect effects, and proportion mediated, by means of the freely available SAS macro [34]. The method is designed to handle case–control data but does not account for the matched study design. This means that the estimates reflect the proportion of association mediated in our material, but hampers generalizability to the underlying population.
Sensitivity analysis included restricting analysis to controls from the years overlapping with the cases (i.e., 2010–2014), restricting the analysis to patients who filled out the questionnaire within 3 months of diagnosis, and restricting analysis to women only.
Results
In comparison with T2D patients, LADA patients were younger, more often female, higher educated, more physically active, and had lower BMI (Table 1). The controls were leaner than the patients and the proportion of men was lower due to the fact that they originate from a matched study on rheumatoid arthritis, which predominantly affects women. This discrepancy in sex distribution is handled by post-matching. Patients with LADA were more often on insulin treatment and had worse beta cell function but lower degree of insulin resistance. Sweetened beverage intake did not differ between LADA and T2D patients (p = 0.9666), but was higher among cases compared to controls (0.59 vs. 0.28 servings/day, p < 0.0001).
Table 1.
Characteristics of study participants
| Control | LADA | T2D | pa | |
|---|---|---|---|---|
| No. of individuals | 1545 | 386 | 1253 | |
| Men, % | 26.5 | 52.6 | 60.4 | 0.0064 |
| Age (years), mean (SD) | 57.6 (9.8) | 58.6 (12.4) | 63.2 (10.3) | < 0.0001 |
| BMI (kg/m2), mean (SD) | 25.4 (4.1) | 27.9 (5.3) | 31.1 (5.3) | < 0.0001 |
| Sweetened beverage intake (serv/d), mean (SD) | 0.28 (0.84) | 0.59 (1.31) | 0.59 (1.58) | 0.9666 |
| High education level, % university | 36.6 | 28.2 | 20.4 | 0.0013 |
| Low leisure time physical activity, % | 10.9 | 17.4 | 23.3 | 0.0135 |
| Current smoker, % | 18.6 | 22.3 | 20.0 | 0.3393 |
| Low alcohol intake (< 5 g/day), % | 10.5 (12.8) | 10.6 (19.8) | 13.6 (42.4) | 0.8066 |
| High-risk HLA, % | 31.6 | 61.2 | 31.4 | < 0.0001 |
| TT/TC in TCF7L2 rs7903146, % | 46.2 | 52.1 | 52.7 | 0.8225 |
| AA/AT in FTO rs9939609, % | 64.2 | 65.8 | 67.5 | 0.5561 |
| With insulin treatment, % | – | 47.0 | 5.6 | < 0.0001 |
| GADA (IU/mL), median (IQR) | – | 240 (29–250) | – | – |
| HOMA-B, median (IQR) | – | 32.8 (13.1–65.2) | 68.1 (42.4–93.7) | < 0.0001 |
| HOMA-IR, median (IQR) | – | 2.70 (1.80–4.40) | 3.60 (2.70–4.80) | 0.0014 |
ap for the difference between LADA and type 2 diabetes
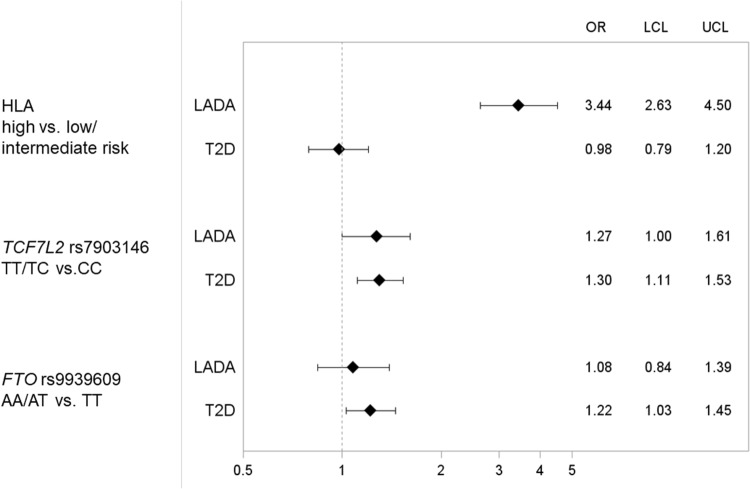
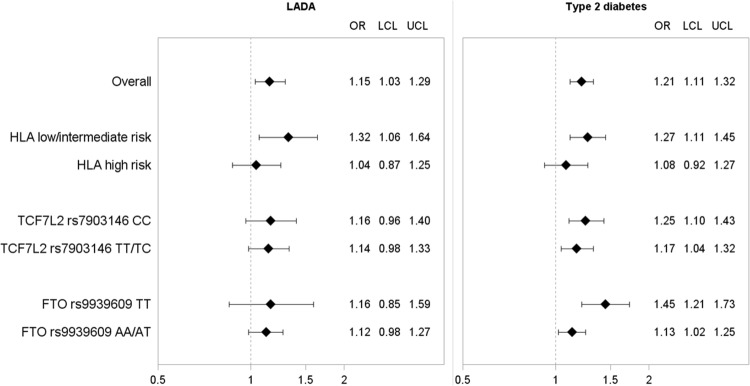
LADA was associated with HLA and TCF7L2 rs7903146 but not FTO rs9939609 (Fig. 1). Sweetened beverage intake was also associated with LADA: Each daily 200 mL serving increment corresponded to an OR of 1.15 (Fig. 2 and Supplementary Table 1). There was no evidence of interaction between sweetened beverages and any of the genotypes as indicated by AP, which means that the risk variants did not enhance the effect of sweetened beverage intake on diabetes risk (Supplementary Table 2). Instead, stratification by HLA genotype suggested that an increased risk of LADA in relation to sweetened beverage consumption was present primarily in carriers of low/intermediate risk genotypes. Further adjustment for BMI slightly attenuated the results (Supplementary Table 2). Neither TCF7L2 rs7903146 nor FTO rs9939609 genotype seemed to modify the association between sweetened beverage intake and risk of LADA (Fig. 2 and Supplementary Table 3).
Fig. 1.
OR with 95% CI of incident LADA and type 2 diabetes in relation to genotypes of HLA, TCF7L2, and FTO. The model is adjusted for age and sex. Distribution of patients and controls with each genotype was as follows: LADA HLA low/intermediate risk n = 149, high risk n = 235; T2D HLA low/intermediate risk n = 851, high risk n = 389; controls HLA low/intermediate risk n = 601, high risk n = 278; LADA TCF7L2 CC n = 184, TT/TC n = 200; T2D TCF7L2 CC n = 587, TT/TC n = 655; controls TCF7L2 CC n = 823, TT/TC n = 707; LADA FTO TT n = 124, AA/AT n = 239; T2D FTO TT n = 392, AA/AT n = 814; controls FTO TT n = 548, AA/AT n = 983
Fig. 2.
OR with 95% CI of incident LADA and type 2 diabetes per one daily serving of sweetened beverages by genotypes of HLA, TCF7L2, and FTO. The model is adjusted for age, sex, education, physical activity, smoking, and alcohol intake
T2D was positively associated with genotypes of TCF7L2 rs7903146 and FTO 9939609 but not HLA (Fig. 1). Sweetened beverage consumption was associated with 21% increased risk of T2D per one daily 200 mL serving increment (Fig. 2 and Supplementary Table 1). Similar to LADA, AP did not indicate any interaction between sweetened beverage intake and any of the genetic risk variants on the risk of T2D (Supplementary Table 2). Moreover, stratification by genotype showed no effect modification by TCF7L2 (Fig. 2). However, the association between sweetened beverages and T2D was more pronounced in non-carriers of the risk variants of FTO, with minor influence of further BMI adjustment (Supplementary Table 1), and HLA (Fig. 2).
Insulin sensitivity increased by each daily serving of sweetened beverages in T2D patients (HOMA-IR beta = 0.035, p = 0.0007) (Supplementary Table 3). For LADA, such a relationship was apparent only among non-carriers of high-risk HLA genotypes (beta = 0.162, p = 0.0047). Additional adjustment for BMI had minor impact for both T2D and LADA. No changes in beta cell function related to sweetened beverage consumption were observed (Supplementary Table 3).
Categorical assessment of sweetened beverages suggested that consumption of more than two daily servings conferred an increased risk of both LADA (OR 2.04, 95% CI 1.11–3.77) and T2D (OR 3.34, 95% CI 2.11–5.28) compared to non-consumers (Supplementary Table 1). We subsequently used a mediation analysis approach and found BMI to mediate 17% of the association with LADA and 56% of the association with T2D among high consumers (Table 2). The natural direct effect of sweetened beverages on diabetes risk was estimated as a twofold increase in odds of both LADA and T2D.
Table 2.
Estimates of direct effect and effect mediated through BMI of the association between sweetened beverage intake and LADA and T2D
| > 2 serv/d vs. less | LADA | Type 2 diabetes |
|---|---|---|
| OR (95% CI)a | OR (95% CI)a | |
| Total effect | 2.21 (1.22–3.99) | 3.37 (1.78–6.35) |
| Natural direct effect | 2.01 (1.07–3.76) | 2.05 (1.22–3.43) |
| Natural indirect effect | 1.10 (0.90–1.34) | 1.64 (1.10–2.45) |
| Proportion mediated through BMI | 17% | 56% |
aModel adjusted for age, sex, education, physical activity, smoking, and alcohol intake
The associations between LADA and T2D and one serving/day increase in sweetened beverage intake remained in the sensitivity analyses; restriction of controls from the years overlapping with the patients (i.e., 2010–2014) resulted in OR 1.18 (95% CI 1.00–1.38) for LADA and 1.28 (95% CI 1.12–1.47) for T2D, and restriction to patients who had responded to the questionnaire within 3 months of diagnosis showed OR 1.31 (95% CI 1.08–1.60) and OR 1.22 (95% CI 1.08–1.37) for LADA and T2D, respectively. OR from the analysis restricted to women, assessing the potential impact of the skewed sex distribution between patients and controls, was 1.20 (95% CI 1.02–1.41) for LADA and 1.37 (95% CI 1.20–1.56) for T2D per one daily serving.
Discussion
Consumption of sweetened beverages is high worldwide and an important contributor to overweight [20] and also associated with diabetes risk [1]. Our findings indicate that sweetened beverage intake, in addition to its effect on overweight, may have a direct effect on the risk of both T2D and LADA and that this effect may be exerted through insulin resistance. Genetic risk variants did not seem to enhance the effect of sweetened beverage intake on diabetes risk, which concurs with the conclusions of a recent T2D study using a genetic risk score [21]. In contrast, consumption seemed to be a stronger risk factor among those with low genetic susceptibility for diabetes; in LADA, the highest risk conferred by sweetened beverages was seen in non-carriers of HLA risk genotypes whereas for T2D, the highest risk was seen among those not carrying the risk genotype of FTO. It is, however, important to note that the confidence intervals are overlapping and these findings thus need to be interpreted with caution.
In LADA, sweetened beverage intake was positively associated with insulin resistance only among those with low/intermediate-risk HLA genotypes. The pathogenesis of LADA is known to include both autoimmunity and insulin resistance, and the latter may be a promotor of less importance among individuals who are already at increased risk due to genetically induced autoimmunity. Our findings for LADA contradict previous findings for T1D in children, where sugar-sweetened beverage intake was positively associated with the progression from islet autoimmunity to clinical onset of diabetes only among high-risk HLA individuals [2]. There may be important differences in the pathophysiology between LADA and childhood T1D that could explain this discrepancy. Although the potential role of insulin resistance on T1D development has been brought to attention through the ‘accelerator hypothesis’ [35], it is likely to play a less pronounced role for childhood T1D [36] than for autoimmune diabetes with adult onset [37]. It has been proposed that a high sugar intake may be toxic to the beta cells leading to apoptosis [9] and that these detrimental effects may be exacerbated when autoantibodies are already present [38]. However, our findings did not indicate any changes in beta cell function. Of note, it has been reported that low/moderate-risk HLA genotypes have become more common among newly diagnosed T1D patients over the past decades, suggesting increased importance of environmental factors in the development of autoimmune diabetes [39]. We can also confirm that LADA is associated with TC7FL2 [11], but not with FTO which is in contrast with a previous report [40]. Neither TCF7L2 nor FTO seem to modify the association between sweetened beverages and risk of LADA.
To the best of our knowledge, this is the first study investigating whether the association between sweetened beverages and T2D is modified by TCF7L2 and FTO. Our hypothesis was that the detrimental effect would be amplified in those with genetic susceptibility. Contrary to our hypothesis, there were no indications of synergistic effects; a positive association with sweetened beverage intake was observed across genotypes of both TCF7L2 and FTO. In fact, the strongest association was found among those homozygous for the non-risk allele of FTO. One could speculate that carriers of the non-risk genotype of FTO have lower probability of becoming overweight and can therefore consume higher amounts of sweetened beverages without subsequent weight gain. If indeed sweetened beverages have detrimental effects on insulin resistance beyond what is mediated through BMI, this may explain our observed findings. In similarity with LADA, we found the association between sweetened beverages and T2D to be stronger in non-carriers of high-risk HLA genotypes. Importantly however, HLA genotype per se was not associated with T2D incidence, which is in concordance with the literature [41]. In this context, it is noteworthy that although GADA is the most frequent antibody found in LADA patients, 10% of patients are positive for other autoantibodies such as insulinoma-associated antigen-2 (IA-2A) or zinc transporter 8 (ZnT8A) [42]. Hence, it is possible that some of the patients classified as T2D, especially among carriers of HLA risk genotypes, are misclassified LADA patients and this could contribute to similarities in the results regarding the association with sweetened beverage intake. These findings should indeed be interpreted with caution; confirmations are clearly warranted.
Findings from the mediation analysis indicated that the direct effect of sweetened beverages on diabetes risk is of similar magnitude for LADA and T2D. This speaks in favor of a common underlying mechanism of equal importance. Beyond the direct effect, sweetened beverages seem to have an effect that is mediated through BMI which is more pronounced for T2D than for LADA. This is in line with a recent study indicating that overweight is a stronger risk factor for T2D than LADA [7]. Sweetened beverages were associated with insulin resistance also after adjustment for BMI, which suggests that it may be part of the observed direct effect. These findings confirm previous studies of both BMI as a mediator [1] and of insulin resistance as a possible driving force behind the observed associations [8].
The main strengths of our study are the population-based design and large number of incident LADA and T2D patients. We also have detailed dietary data from an extensively validated FFQ [24–26] as well as comprehensive information on important confounding factors. An important limitation is the retrospective nature of the collected data, which may lead to recall bias. However, the sensitivity analysis restricted to patients with the shortest diabetes duration indicates minor impact of such error. Furthermore, if patients have limited their sweetened beverage intake after diagnosis and reported accordingly, it would lead to underestimated ORs. In this context, it is important to note that our observed association between sweetened beverage intake and risk of T2D is in concordance with previous reports from prospective studies [1]. The controls were collected within a somewhat different context and time period and had a larger proportion of women than the cases. Sensitivity analysis indicated that this had minor influence on the results. Furthermore, the observed associations between sweetened beverage intake and diabetes correspond well to our previous findings based on the internal ESTRID controls with similar sex distribution and recruitment period [3]. Likewise, the association we observe for TCF7L2, and lack of association with HLA genotype, in relation to T2D risk is in line with previous findings [11]. Another important question is whether the sweetened beverage consumption of the controls reflects that of the population that generated the cases. In support hereof, we find that their mean consumption was quite similar to that of the general population according to the latest national survey by National Food Agency Sweden (in 2010, http://www.slv.se), slightly higher in male controls (0.47 vs. 0.42 servings/day) and slightly lower in female controls (0.21 vs. 0.28 servings/day). Importantly, mean consumption among the patients was higher than both the intake reported by controls and the reported average in the national survey. We could not distinguish between sugar-sweetened and artificially sweetened beverage, however, our previous findings indicate that the diabetes risk is increased irrespective of beverage type [3]. Neither was it possible to adjust for total energy intake and family history of diabetes, which are two potentially confounding factors, due to data availability. However, in our earlier publication using the same cases but controls collected within the ESTRID study [3], we found sweetened beverage intake to be positively associated with both LADA and T2D also after adjustment for these factors. Height and weight was self-reported for both cases and controls, which may lead to inaccurate BMI data. However, for the cases this shows high correlation with BMI based on clinical measurements from time of diagnosis (r = 0.92). Despite this, the use of BMI as a proxy for body fat is a crude measure [43]. Consequently, it is possible that we have underestimated the proportion of association mediated by BMI. Still, crude assessment of body fat mass is unlikely to explain the different results regarding mediation that we observed for LADA compared to T2D. The mediation analysis assumes a causal effect of sweetened beverages on both BMI and diabetes risk, which we are unable to prove.
In conclusion, these results indicate that high intakes of sweetened beverages increase the risk of both LADA and T2D, and that the effect is not amplified by genetic susceptibility conferred by genotypes of HLA, FTO or TCF7L2. The potential influence of sweetened beverages on diabetes risk seems to include effects on overweight as well as direct effects on insulin sensitivity. Thus, reducing sweetened beverage intake on the population level is likely to result in health gains both in terms of overweight and diabetes incidence.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
JEL contributed to the study objectives, data analysis, interpretation of results, and writing of the manuscript. SC researched data (ESTRID), contributed to the study objectives, interpretation of results, and reviewed and revised the manuscript. TA contributed to data analysis, interpretation of results, and reviewing and revising of the manuscript. LG, EA, MD (ANDIS) and LA (EIRA) contributed to collection of data. AW, LG, EA, MD, LA, and TT contributed to interpretation of results, and reviewing and revising of the manuscript. All authors have read and approved the final version of the manuscript. JEL had access to all data and takes responsibility for the integrity of the data, and accuracy of data analysis and study report.
Funding
This study, including the ESTRID data collection, was supported by research grants from Martin Rind Foundation, the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, AFA Insurance, the Swedish Diabetes Association, and the Novo Nordisk Foundation. ANDIS was supported by the Swedish Research Council (including ALF funding for clinical research in medicine) and European Research Council Advanced Researcher grant (GA 269045) to LG. The EIRA study was supported by grants from Swedish Medical Research Council, the Swedish Research Council for Health, Working Life and Welfare, the Swedish Rheumatic Foundation, the AFA Insurance Company, and Stockholm County Council.
Compliance with ethical standards
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
This study was approved by the Regional Ethical Review Board in Stockholm. All included participants provided informed consent prior to study inclusion.
References
- 1.Imamura F, O’Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, Forouhi NG. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ. 2015;351:h3576. doi: 10.1136/bmj.h3576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lamb MM, Frederiksen B, Seifert JA, Kroehl M, Rewers M, Norris JM. Sugar intake is associated with progression from islet autoimmunity to type 1 diabetes: the Diabetes Autoimmunity Study in the Young. Diabetologia. 2015;58:2027–2034. doi: 10.1007/s00125-015-3657-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Löfvenborg JE, Andersson T, Carlsson PO, Dorkhan M, Groop L, Martinell M, Tuomi T, Wolk A, Carlsson S. Sweetened beverage intake and risk of latent autoimmune diabetes in adults (LADA) and type 2 diabetes. Eur J Endocrinol. 2016;175:605–614. doi: 10.1530/EJE-16-0376. [DOI] [PubMed] [Google Scholar]
- 4.Malik VS, Hu FB. Sweeteners and risk of obesity and type 2 diabetes: the role of sugar-sweetened beverages. Curr Diab Rep. 2012;12:195–203. doi: 10.1007/s11892-012-0259-6. [DOI] [PubMed] [Google Scholar]
- 5.Abdullah A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract. 2010;89:309–319. doi: 10.1016/j.diabres.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 6.Censin JC, Nowak C, Cooper N, Bergsten P, Todd JA, Fall T. Childhood adiposity and risk of type 1 diabetes: a mendelian randomization study. PLoS Med. 2017;14:e1002362. doi: 10.1371/journal.pmed.1002362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hjort R, Ahlqvist E, Carlsson PO, Grill V, Martinell M, Rasouli B, Rosengren A, Tuomi T, Åsvold BO, Carlsson S. Overweight, obesity and the risk of LADA: results from a Swedish case–control study and the Norwegian HUNT Study. Diabetologia. 2018;61:1333–1343. doi: 10.1007/s00125-018-4596-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ma J, Jacques PF, Meigs JB, Fox GT, Smith CE, Hruby A, Saltzman E, McKeown NM. Sugar-sweetened beverage but not diet soda consumption is positively associated with progression of insulin resistance and prediabetes. J Nutr. 2016;146:2544–2550. doi: 10.3945/jn.116.234047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang Z, Li J, Yang L, Chen R, Yang R, Zhang H, Cai D, Chen H. The cytotoxic role of intermittent high glucose on apoptosis and cell viability in pancreatic beta cells. J Diabetes Res. 2014;2014:712781. doi: 10.1155/2014/712781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pociot F, Lernmark Å. Genetic risk factors for type 1 diabetes. Lancet. 2016;387:2331–2339. doi: 10.1016/S0140-6736(16)30582-7. [DOI] [PubMed] [Google Scholar]
- 11.Cervin C, Lyssenko V, Bakhtadze E, Lindholm E, Nilsson P, Tuomi T, Cilio CM, Groop L. Genetic similarities between latent autoimmune diabetes in adults, type 1 diabetes, and type 2 diabetes. Diabetes. 2008;57:1433–1437. doi: 10.2337/db07-0299. [DOI] [PubMed] [Google Scholar]
- 12.Helgason A, Pálsson S, Thorleifsson G, Grant SF, Emilsson V, Gunnarsdottir S, Adeyemo A, Chen Y, Chen G, Reynisdottir I, et al. Refining the impact of TCF7L2 gene variants on type 2 diabetes and adaptive evolution. Nat Genet. 2007;39:218–225. doi: 10.1038/ng1960. [DOI] [PubMed] [Google Scholar]
- 13.Jin T. Current understanding on role of the Wnt signaling pathway effector TCF7L2 in glucose homeostasis. Endocr Rev. 2016;37:254–277. doi: 10.1210/er.2015-1146. [DOI] [PubMed] [Google Scholar]
- 14.Florez JC, Jablonski KA, Bayley N, Pollin TI, Shuldiner AR, Knowler WC, Nathan DM, Altshuler; Diabetes Prevention Program Research Group TCF7L2 polymorphisms and progression to diabetes in the diabetes prevention program. N Engl J Med. 2006;355:241–250. doi: 10.1056/NEJMoa062418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McKeown NM, Dashti HS, Ma J, Haslam DE, Kiefte-de Jong JC, Smith CE, Tanaka T, Graff M, Lemaitre RN, Rybin D, et al. Sugar-sweetened beverage intake associations with fasting glucose and insulin concentrations are not modified by selected genetic variants in a ChREBP-FGF21 pathway: a meta-analysis. Diabetologia. 2018;61:317–330. doi: 10.1007/s00125-017-4475-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM, Perry JR, Elliott KS, Lango H, Rayner NW, et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science. 2007;316:889–894. doi: 10.1126/science.1141634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Melhorn SJ, Askren MK, Chung WK, Kratz M, Bosch TA, Tyagi V, Webb MF, De Leon MRB, Grabowski TJ, Leibel RL, et al. FTO genotype impacts food intake and corticolimbic activation. Am J Clin Nutr. 2018;107:145–154. doi: 10.1093/ajcn/nqx029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Loos RJ, Yeo GS. The bigger picture of FTO: the first GWAS-identified obesity gene. Nat Rev Endocrinol. 2014;10:51–61. doi: 10.1038/nrendo.2013.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hertel JK, Johansson S, Sonestedt E, Jonsson A, Lie RT, Platou CG, Nilsson PM, Rukh G, Midthjell K, Hveem K, et al. FTO, type 2 diabetes, and weight gain throughout adult life: a meta-analysis of 41,504 subjects from the Scandinavian HUNT, MDC, and MPP studies. Diabetes. 2011;60:1637–1644. doi: 10.2337/db10-1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98:1084–1102. doi: 10.3945/ajcn.113.058362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ericson U, Hindy G, Drake I, Schulz CA, Brunkwall L, Hellstrand S, Almgren P, Orho-Melander M. Dietary and genetic risk scores and incidence of type 2 diabetes. Genes Nutrition. 2018;13:13. doi: 10.1186/s12263-018-0599-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Löfvenborg JE, Andersson T, Carlsson PO, Dorkhan M, Groop L, Martinell M, Rasouli B, Storm P, Tuomi T, Carlsson S. Coffee consumption and the risk of latent autoimmune diabetes in adults–results from a Swedish case–control study. Diabet Med. 2014;31:799–805. doi: 10.1111/dme.12469. [DOI] [PubMed] [Google Scholar]
- 23.Ahlqvist E, Storm P, Käräjämäki A, Martinell M, Dorkhan M, Carlsson A, Vikman P, Prasad RB, Aly DM, Almgren P, et al. Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol. 2018;6:361–369. doi: 10.1016/S2213-8587(18)30051-2. [DOI] [PubMed] [Google Scholar]
- 24.Messerer M, Johansson SE, Wolk A. The validity of questionnaire-based micronutrient intake estimates is increased by including dietary supplement use in Swedish men. J Nutr. 2004;134:1800–1805. doi: 10.1093/jn/134.7.1800. [DOI] [PubMed] [Google Scholar]
- 25.Levitan EB, Westgren CW, Liu S, Wolk A. Reproducibility and validity of dietary glycemic index, dietary glycemic load, and total carbohydrate intake in 141 Swedish men. Am J Clin Nutr. 2007;85:548–553. doi: 10.1093/ajcn/85.2.548. [DOI] [PubMed] [Google Scholar]
- 26.Wallin A, Di Giuseppe D, Burgaz A, Håkansson N, Cederholm T, Michaëlsson K, Wolk A. Validity of food frequency questionnaire-based estimates of long-term long-chain n-3 polyunsaturated fatty acid intake. Eur J Nutr. 2014;53:549–555. doi: 10.1007/s00394-013-0563-1. [DOI] [PubMed] [Google Scholar]
- 27.Rahmati K, Lernmark A, Becker C, Foltyn-Zadura A, Larsson K, Ivarsson SA, Törn C. A comparison of serum and EDTA plasma in the measurement of glutamic acid decarboxylase autoantibodies (GADA) and autoantibodies to islet antigen-2 (IA-2A) using the RSR radioimmunoassay (RIA) and enzyme linked immunosorbent assay (ELISA) kits. Clin Lab. 2008;54:227–235. [PubMed] [Google Scholar]
- 28.The Oxford Center for Diabetes. Endocrinology & metabolism. Diabetes trial unit. HOMA calculator. Available from: http://www.dtu.ox.ac.uk/homacalculator/index.php. Accessed June 2013
- 29.Nguyen C, Varney MD, Harrison LC, Morahan G. Definition of high-risk type 1 diabetes HLA-DR and HLA-DQ types using only three single nucleotide polymorphisms. Diabetes. 2013;62:2135–2140. doi: 10.2337/db12-1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hagopian WA, Sanjeevi CB, Kockum I, Landin-Olsson M, Karlsen AE, Sundkvist G, Dahlquist G, Palmer J, Lernmark A. Glutamate decarboxylase-, insulin-, and islet cell-antibodies and HLA typing to detect diabetes in a general population-based study of Swedish children. J Clin Invest. 1995;95:1505–1511. doi: 10.1172/JCI117822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Törn C, Gupta M, Nikitina Zake L, Sanjeevi CB, Landin-Olsson M. Heterozygosity for MICA5.0/MICA5.1 and HLA-DR3-DQ2/DR4-DQ8 are independent genetic risk factors for latent autoimmune diabetes in adults. Hum Immunol. 2003;64:902–909. doi: 10.1016/s0198-8859(03)00158-7. [DOI] [PubMed] [Google Scholar]
- 32.Andersson T, Alfredsson L, Källberg H, Zdravkovic S, Ahlbom A. Calculating measures of biological interaction. Eur J Epidemiol. 2005;20:575–579. doi: 10.1007/s10654-005-7835-x. [DOI] [PubMed] [Google Scholar]
- 33.Valeri L, VanderWeele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18:137–150. doi: 10.1037/a0031034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harvard School of Public Health. Mediation SAS macro program at https://www.hsph.harvard.edu/tyler-vanderweele/tools-and-tutorials/. Accessed 24 May 2018
- 35.Wilkin TJ. The accelerator hypothesis: a review of the evidence for insulin resistance as the basis for type I as well as type II diabetes. Int J Obes. 2009;33:716–726. doi: 10.1038/ijo.2009.97. [DOI] [PubMed] [Google Scholar]
- 36.Siljander HT, Hermann R, Hekkala A, Lähde J, Tanner P, Keskinen P, Ilonen J, Simell O, Veijola R, Knip M. Insulin secretion and sensitivity in the prediction of type 1 diabetes in children with advanced b-cell autoimmunity. Eur J Endocrinol. 2013;169:479–485. doi: 10.1530/EJE-13-0206. [DOI] [PubMed] [Google Scholar]
- 37.Juhl CB, Bradley U, Holst JJ, Leslie RD, Yderstraede KB, Hunter S, Action LADA. Pathophysiology Similar weight-adjusted insulin secretion and insulin sensitivity in short-duration late autoimmune diabetes of adulthood (LADA) and type 2 diabetes: Action LADA 9. Diabet Med. 2014;31:941–945. doi: 10.1111/dme.12434. [DOI] [PubMed] [Google Scholar]
- 38.Björk E, Kämpe O, Karlsson FA, Pipeleers DG, Andersson A, Hellerström C, Eizirik DL. Glucose regulation of the autoantigen GAD65 in human pancreatic islets. J Clin Endocrinol Metab. 1992;75:1574–1576. doi: 10.1210/jcem.75.6.1464667. [DOI] [PubMed] [Google Scholar]
- 39.Fourlanos S, Varney MD, Tait BD, Morahan G, Honeyman MC, Colman PG, Harrison LC. The rising incidence of type 1 diabetes is accounted for by cases with lower-risk human leukocyte antigen genotypes. Diabetes Care. 2008;31:1546–1549. doi: 10.2337/dc08-0239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pettersen E, Skorpen F, Kvaløy K, Midthjell K, Grill V. Genetic heterogeneity in latent autoimmune diabetes is linked to various degrees of autoimmune activity: results from the Nord-Trøndelag. Health Study. 2010;59:302–310. doi: 10.2337/db09-0923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tuomi T, Santoro N, Caprio S, Cai M, Weng J, Groop L. The many faces of diabetes: a disease with increasing heterogeneity. Lancet. 2014;383:1084–1094. doi: 10.1016/S0140-6736(13)62219-9. [DOI] [PubMed] [Google Scholar]
- 42.Hawa MI, Kolb H, Schloot N, Beyan H, Paschou SA, Buzzetti R, et al. Adult-onset autoimmune diabetes in Europe is prevalent with a broad clinical phenotype: action LADA 7. Diabetes Care. 2013;36:908–913. doi: 10.2337/dc12-0931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rothman KJ. BMI-related errors in the measurement of obesity. Int J Obes. 2008;32(Suppl 3):S56–S59. doi: 10.1038/ijo.2008.87. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.