Abstract
The purpose of this study was to identify the vessels feeding the FPL to reduce the FPL tendon ruptures related to VLP surgery. The dissections identified the FPL, radial artery (RA) and anterior interosseous artery (AIA). The mean number of branches of the RA and AIA to the FPL was 2.0 and 4.0, respectively. The distance from volar prominence of the radius to the most distal branch of the RA and AIA was 43 mm and 57 mm, respectively. The most distal branch would be frequently injured during VLP surgery because of its proximity to the surgical field.
Keywords: Volar locking plates, Flexor pollicis longus, Feeding vessels, Radial artery, Anterior interosseous artery
Abbreviations: DRFs, distal radius fractures; VLPs, volar locking plates; FPL, flexor pollicis longus; FCR, flexor carpi radialis; RA, radial artery; PQ, pronator quadratus; FDS, flexor digitorum superficialis; FDP II, flexor digitorum profundus II; AIA, anterior interosseous artery
1. Introduction
Due to the increasing population of elderly patients with osteoporosis, the number of patients with distal radius fractures (DRFs) is increasing, which has become a health problem in our country.1,2 Volar locking plates (VLPs) have been widely used for patients with unstable DRF; however, there are many reports about flexor pollicis longus (FPL) rupture due to the implant irritation after VLP surgery.3, 4, 5
Normal blood circulation is an important factor for keeping the tendons healthy. The durability of tendons depends on several factors, such as blood supply, presence of rheumatoid arthritis 6, and steroid use.7 However, there are only a few reports on the role of feeding vessels in flexor pollicis longus (FPL) tendons.8,9 FPL tendons have three circulation systems. First, the vinculum system provides blood supply at the digital area. Second, the synovium system via the median nerve artery provides blood supply at the level of the distal radius. Lastly, the circulation from the FPL muscle in the forearm also supplies blood to the FPL tendon.10, 11, 12, 13, 14, 15
The VLP surgical approach involves an incision in the flexor carpi radialis (FCR) tendon. After dividing the FCR tendon and the radial artery (RA), the FPL is retracted at the ulnar side and then the volar surface of the radius is exposed. Most surgeons detach the pronator quadratus (PQ) from the radial border to place the volar plate on the fracture site. Blood flow to the FPL tendon can be decreased due to scar formation and damage to the feeding vessels and the synovium after VPL surgery. This study aimed to investigate the blood supply to the FPL and identify the FPL feeding vessels to reduce FPL tendon ruptures related to VPL surgery.
2. Material and methods
A total of 14 unpaired human cadaveric right upper limbs, (8 male and 6 female specimens; age range, 65–99 years), with no severe macroscopic degenerative or traumatic changes, were used in this study.
All specimens were fixed with 10% formalin and were preserved in 50% alcohol for 6 months. These cadavers were donated to our institute for education and research purposes, and this study was approved by the ethics committee of Iwate Medical University (No.H28-90).
Cadaver preparation began by removing the skin and soft subcutaneous tissue on the forearm to expose the flexor muscle group. The FPL and flexor digitorum superficialis (FDS) were exposed when the FCR was removed. The FDS arose from the radial border, and a part of its origin was attached to the FPL. After removal of the FDS, the FPL originated from the radial border of the radius to the interosseous membrane, joining the flexor digitorum profundusII (FDP II) in the middle of the forearm (Fig. 1). Between the FDP II and FPL, the anterior interosseous artery (AIA) ran on the interosseous membrane, accompanied by the anterior interosseous nerve (Fig. 1). The AIA ran with branches supplying the FPL and went into the PQ from the proximal edge (Fig. 1). In the middle of the forearm, the RA ran along the ulnar side of the brachioradialis muscle. The RA descended on the radial side of FPL and extended to the wrist, also supplying the FPL (Fig. 2). The FPL muscle was supplied by branches from the AIA on the ulnar side and from the RA on the radial side.
Fig. 1.
Frontal view of the right forearm, showing the anterior interosseous artery. Black stars indicate branches from the anterior interosseous artery.
The white arrow indicates the anterior interosseous nerve. The black arrow indicates the anterior interosseous artery. FDPⅡ: flexor digitorum profundusⅡ; PQ: pronator quadratus; FPL: flexor pollicis longus.
Fig. 2.
Frontal view of the right forearm, showing the radial artery.
Black stars indicate branches from the radial artery. FDP Ⅱ: flexor digitorum profundus Ⅱ; RA: radial artery.
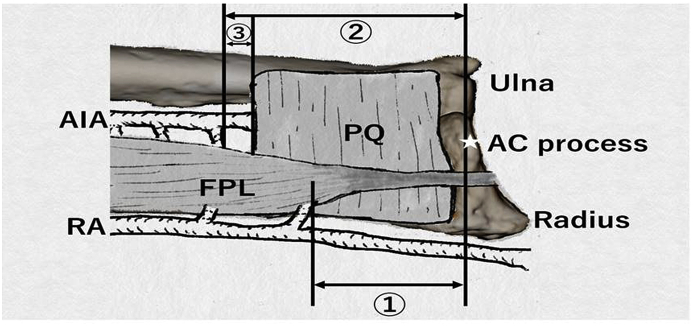
The number of branches was recorded. The most volarly prominence on the distal radius (AC process), the proximal edge of the PQ, the most distal branch of the AIA, and the most distal branch of the RA were marked, and their lengths were measured (Fig. 3).
Fig. 3.
Schematic diagram depicting each distance.
① indicates the distance from AC process to the most distal branch of the RA. ② indicates the distance from AC process to the most distal branch of the AIA. ③ indicates the distance between the proximal edge of the PQ and the most distal branch of the AIA.
The white star indicates the AC process.
3. Results
Blood supply to the FPL was from the branches of the AIA and RA (Fig. 3) (Table 1). The mean number of branches of the RA and AIA was 2.0 (0–4) and 4.0 (2–7), respectively (Fig. 3) (Table 1). The mean distance from AC process to the most distal branch of the RA and AIA was 43.0 (24–85) and 57.0 (38–72) mm, respectively (Fig. 3). The mean distance between the proximal edge of the PQ and the most distal branch of the AIA is 14.2 mm (4–26 mm) (Fig. 3).
Table 1.
Anatomical findings.
| Case | Age | Sex | Number of branches |
Distance from AC process to the most distal branch (mm) |
Distance between the PQ and the most distal branch of the AIA (mm) | ||
|---|---|---|---|---|---|---|---|
| RA | AIA | RA | AIA | ||||
| 1 | 89 | M | 1 | 2 | 35 | 50 | 15 |
| 2 | 75 | F | 1 | 3 | 85 | 55 | 10 |
| 3 | 67 | M | 3 | 5 | 35 | 55 | 10 |
| 4 | 72 | F | 2 | 4 | 58 | 60 | 20 |
| 5 | 84 | M | 3 | 5 | 40 | 52 | 12 |
| 6 | 79 | M | 1 | 3 | 63 | 71 | 20 |
| 7 | 83 | F | 1 | 2 | 54 | 52 | 15 |
| 8 | 85 | M | 2 | 5 | 48 | 52 | 5 |
| 9 | 74 | F | 2 | 4 | 24 | 38 | 4 |
| 10 | 64 | M | 2 | 7 | 24 | 66 | 22 |
| 11 | 89 | M | 0 | 5 | 0 | 58 | 5 |
| 12 | 80 | F | 3 | 4 | 24 | 72 | 25 |
| 13 | 70 | M | 4 | 4 | 35 | 68 | 26 |
| 14 | 86 | F | 1 | 3 | 35 | 49 | 10 |
| mean | 78.4 | 2.0 | 4.0 | 43.0 | 57.0 | 14.2 | |
4. Discussion
There are several reports about the blood supply to the FPL. In the digital area, the FPL tendon is supplied by the vinculum, which is the specialized mesotendineum of the synovial sheath that provides the vascular supply to the tendon in the synovial space.10, 11, 12, 13,15 Vessels from the vinculum enter the dorsum of the flexor pollicis longus and run in a longitudinal direction proximally and distally.10, 11, 12,15
Revol et al.14 reported the blood supply of the FPL in a fresh cadaver. According to the report, the FPL was supplied mainly by branches from the AIA, and the RA was a secondary feeding vessel. Although there were only a few cases reported, the FPL was also supplied by branches of the ulnar artery. Our study revealed that the AIA supplied more branches to the FPL compared to the RA. These findings are generally in agreement with previous reports. The FPL tendon is only supplied by the median nerve artery via the synovium and slight blood circulation from the muscle at the level of the distal radius.12 Therefore, the FPL is considered to be fragile in this area, which is also the location of VLP placement.
In this study, the mean distance from AC process to the most distal branch of the RA and AIA was 43.0 and 57.0 mm, respectively. We speculated that these branches are found in the surgical field, especially the branch of the RA, because the length of commercial VLPs is about 50–60 mm. The most distal branch of the RA may become damaged, because the FPL needs to be continuously retracted towards the ulnar side during surgery. The most distal branch of the AIA was found near the proximal edge of the PQ. Preservation of this vessel is recommended to prevent further deterioration of blood flow to the FPL. Careful detachment of the PQ is necessary, and blind operations may increase the risk of injury to this vessel. Surgeons must know these anatomical features to avoid internal bleeding and the development of hematomas, which leads to hand edema.
This study had several limitations. First, a comparatively small number of specimens were investigated. Due to normal anatomical variations, a study with a larger sample size is needed. Second, investigation was carried out with formalin-fixed cadavers and without colored latex injections, which may lead to overlooking of thin vessels. Lastly, there is no verification about blood supply to the FPL after VLP surgery.
This study is clinically relevant, because it identifies the feeding vessels to the FPL and related structures at the wrist. This knowledge may assist surgeons in performing VLP surgery with less complications.
5. Conclusion
The blood supply of the FPL was from the branches of the AIA and RA. The most distal branch of the RA would be often damaged during VLP surgery. The most distal branch of the AIA is found near the proximal edge of the PQ and careful detachment of the PQ is recommended to avoid the risk of injury of this vessel.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
None.
References
- 1.Hagino H., Yamamoto K., Ohshiro H., Nakamura T., Kishimoto H., Nose T. Changing incidence of hip, distal radius, and proximal humerus fractures in Tottori Prefecture, Japan. Bone. 1999;24:265–270. doi: 10.1016/s8756-3282(98)00175-6. [DOI] [PubMed] [Google Scholar]
- 2.Yoshimura N., Muraki S., Oka H., Kawaguchi H., Nakamura K., Akune T. Cohort profile: research on Osteoarthritis/Osteoporosis against Disability study. Int J Epidemiol. 2010;39:988–995. doi: 10.1093/ije/dyp276. [DOI] [PubMed] [Google Scholar]
- 3.Limthongthang R., Bachoura A., Jacoby S.M., Osterman A.L. Distal radius volar locking plate design and associated vulnerability of the flexor pollicis longus. J Hand Surg. 2014;39:852–860. doi: 10.1016/j.jhsa.2014.01.038. [DOI] [PubMed] [Google Scholar]
- 4.Imatani J., Akita K., Yamaguchi K., Shimizu H., Kondou H., Ozaki T. An anatomical study of the watershed line on the volar, distal aspect of the radius: implications for plate placement and avoidance of tendon ruptures. J Hand Surg. 2012;37:1550–1554. doi: 10.1016/j.jhsa.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 5.Soong M., Earp B.E., Bishop G., Leung A., Blazar P. Volar locking plate implant prominence and flexor tendon rupture. J Bone Joint Surg Am. 2011;93:328–335. doi: 10.2106/JBJS.J.00193. [DOI] [PubMed] [Google Scholar]
- 6.Ishikawa H. The latest treatment strategy for the rheumatoid hand deformity. J Orthop Sci. 2017;22(4):583–592. doi: 10.1016/j.jos.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 7.Kanayama G., DeLuca J., Meehan W.P., 3rd Ruptured tendons in anabolic-androgenic steroid users: a cross-sectional cohort study. Am J Sports Med. 2015;43:2638–2644. doi: 10.1177/0363546515602010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trevor D. Rupture of the extensor pollicis longus tendon after Colles fracture. J Bone Joint Surg Br. 1950;32-b:370–375. doi: 10.1302/0301-620X.32B3.370. [DOI] [PubMed] [Google Scholar]
- 9.Helal B., Chen S.C., Iwegbu G. Rupture of the extensor pollicis longus tendon in undisplaced Colles' type of fracture. Hand. 1982;14:41–47. doi: 10.1016/s0072-968x(82)80038-7. [DOI] [PubMed] [Google Scholar]
- 10.Lundborg G. The vascularization of the human flexor pollicis longus tendon. Hand. 1979;11:28–33. doi: 10.1016/s0072-968x(79)80005-4. [DOI] [PubMed] [Google Scholar]
- 11.Hergenroeder P.T., Gelberman R.H., Akeson W.H. The vascularity of the flexor pollicis longus tendon. Clin Orthop Relat Res. 1982:298–303. [PubMed] [Google Scholar]
- 12.Azar C.A., Culver J.E., Fleegler E.J. Blood supply of the flexor pollicis longus tendon. J Hand Surg. 1983;8:471–475. doi: 10.1016/s0363-5023(83)80210-x. [DOI] [PubMed] [Google Scholar]
- 13.Armenta E., Fisher J. Anatomy of flexor pollicis longus vinculum system. J Hand Surg. 1984;9:210–212. doi: 10.1016/s0363-5023(84)80143-4. [DOI] [PubMed] [Google Scholar]
- 14.Revol M.P., Lantieri L., Loy S., Guerin-Surville H. Vascular anatomy of the forearm muscles: a study of 50 dissections. Plast Reconstr Surg. 1991;88:1026–1033. doi: 10.1097/00006534-199112000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Zbrodowski A., Gajisin S., Bednarkiewicz M. Mesotendons of the flexor pollicis longus muscle. Acta Anat. 1994;151:131–137. doi: 10.1159/000147654. [DOI] [PubMed] [Google Scholar]