Abstract
Diabetes mellitus (DM) is of increasing public health importance in India. The magnitude has been increasing over the past three decades. DM is associated with major microvascular complications among which diabetic retinopathy (DR) is emerging as one of the leading causes of visual impairment in low and middle income countries. Two-thirds of the Indian population resides in rural areas where access to modern medicine is limited mostly to the public health system. Operational guidelines are critical in delivering program components effectively. They provide the template to benchmark service delivery and help in improving quality of care. A pilot initiative to reduce visual impairment in people with diabetes was supported by an international nongovernmental funding organization over a 5-year period in India. This initiative facilitated the development of operational guidelines for DR. The guidelines were developed through consensus and primarily addressed the public health system in India.
Keywords: Diabetes, diabetic retinopathy, India, operational guidelines, visual impairment
Diabetes mellitus (DM) is of public health concern in India with an increasing magnitude over the past three decades.[1] In India, among the 20 + population, there were an estimated 65 million people with DM in 2016.[1] Assuming 15%–20% of these individuals have any diabetic retinopathy (DR) and 5%–7% have vision-threatening DR, 3.25–4.55 million people are at risk of visual loss or have already lost vision from DR. This Equals to 2240–3136 people aged 20 years and above in a district of 1 million.[2]
A major initiative to pilot interventions to reduce the prevalence of DR in India was supported by the Queen Elizabeth Diamond Jubilee Trust (The Trust), UK. One of the outputs of this initiative was the development of technical and operational guidelines for the control of visual loss from DR in India.
Operational guidelines document the processes and systems in implementing a program effectively while technical guidelines highlight the clinical management using an evidence-based approach. Operational guidelines support quality assurance frameworks and improve the effectiveness and efficiency of service delivery at different levels of the health system. They establish an accountability matrix by specifying what can be done at different levels and who would be responsible for managing services at all levels of the health system. Therefore, the purpose of such guidelines is to enable all personnel working in the public health system to deliver the full range of services possible.
As part of the National Health Mission and Ayushman Bharat initiatives, a number of operational guidelines for different health conditions have been developed. Operational guidelines for the prevention, screening, and control of common noncommunicable diseases (including diabetes) have been prepared.[3] However, no such guidelines were developed on DR. Therefore, such a document to facilitate the delivery of diabetic and eye care services to prevent visual loss in DR was recently developed.[4] The primary audience for the guidelines were those responsible for delivering diabetic and eye care services and for those responsible for planning and implementing such programs using the public health system.
Methods
The operational guidelines were developed using the Delphi technique.[5] This method helps to synthesize expert opinion when evidence is not available. Clinical practice guidelines are routinely evidence-based but program guidelines/operational guidelines are mostly developed using expert consensus. Sometimes a hybrid approach is followed where clinical evidence wherever available is supplemented with expert advice. Such an approach has been effectively used for pragmatic guidelines for special situations like fasting during Ramadan for people with diabetes.[6]
Expert groups were facilitated by a core guideline writing group which reviewed available evidence and sought expert advice on the drafting of the final recommendations.
Summarized guidelines
The detailed guidelines briefly describe the following: the magnitude and risk factors for diabetes and DR, integrating the DR screening and management program into the existing public health system, prevention of visual impairment in DR, suggested screening protocol and competencies required, and monitoring and program management.[4] The guidelines emphasize that the aim of an integrated DR screening and management program is that the prevention, detection, and management of DR should become an integral component of the existing public health system. The guidelines draw upon the experience gained from implementing the pilot DR screening and management program in India across 10 districts spread across 10 States (one district in each of the targeted States), which was supported by The Trust (2013–2019).[7]
The guidelines stress the importance of synergy between the two public-funded programs: the National Program for the Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) and the National Program for Control of Blindness and Visual Impairment (NPCB and VI). They also highlight the work of the nongovernmental organizations (NGOs) and the need to leverage their presence and support. The NPCDCS was launched in 2010 with the objective to prevent and control common noncommunicable diseases (NCDs) through behavior and lifestyle changes, and to provide early diagnosis and management of common NCDs.[8] Diabetes is an important component of the NPCDCS program. The activities of the NPCDCS program are incorporated at all levels of the health system: states, districts, community health centers (CHCs), primary health centers (PHCs), and health and wellness centers (HWCs)/sub health centers (SHCs).
The National Program for Control of Blindness and Visual Impairment (NPCB and VI) was launched in 1976 as a 100% centrally sponsored scheme with the goal of reducing the prevalence of blindness to 0.3% by 2020.[9]
The guidelines also opine that a new opportunity for integration has opened up with the Ayushman Bharat initiative and this can afford avenues for better synergy from the village level onwards.
The estimated annual workload for systematic screening for DM/DR was computed [Table 1]. It was observed that the number of persons with VTDR manageable at the district hospital level was approximately 630 per million population.
Table 1.
Estimated workload at different levels of the public health system
| Levels of care | Population | People at risk of DM (≥30 years) | People with diabetes | PwDM with DR | PwDM with VTDR |
|---|---|---|---|---|---|
| Assumptions | 45% | 8% | 25% | 7% | |
| Health and Wellness Centers/Subcenters | 5000 | 2250 | 180 | 45 | 3 |
| Primary Health Center | 30,000 | 13,500 | 1080 | 270 | 19 |
| Community Health Center | 120,000 | 54,000 | 4320 | 1080 | 76 |
| District Health Center/District Hospital | 1,000,000 | 450,000 | 36,000 | 9000 | 630 |
| Action Needed | Screening for diabetes | Screening for DR | Screen Failure: Refer for Diagnosis | Treatment and follow-Up |
DM: Diabetes Mellitus; DR: Diabetic Retinopathy; PwDM: People with Diabetes Mellitus; VTDR: Vision Threatening Diabetic Retinopathy
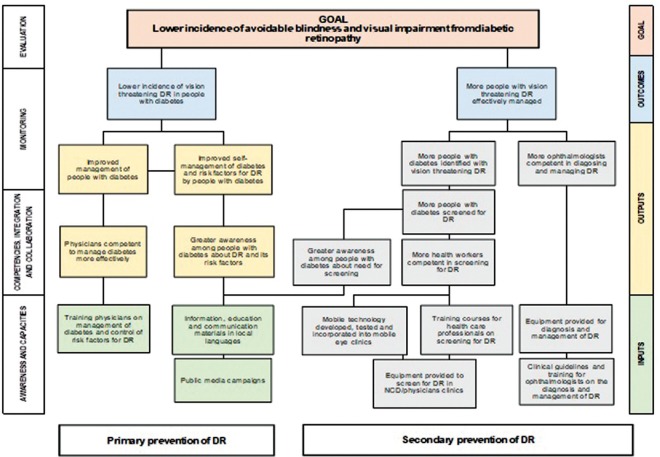
A theory of change was used to identify different strategies to achieve the objective of a DR program [Fig. 1]. Theories of Change define and describe all the interconnected elements needed to bring about the long-term goal of a program using a causal pathway. The long-term goal is defined first, and working back from this, inputs and interventions, activities and processes are described in a logical manner.
Figure 1.
Theory of change: different strategies to achieve the objective of an integrated DR screening and management program
Personnel required to implement the strategies at different levels of prevention for the control of visual loss in diabetes were identified [Table 2]. The services that can be provided at different levels of the public health system have also been listed [Table 3].
Table 2.
Proposed strategies at different levels of prevention
| Levels of Prevention | Health care personnel responsible for implementation of strategies |
|---|---|
| Primordial Prevention | |
| Education about diabetes and its complications, and the benefits of a healthy lifestyle | Community health workers |
| Mobilize people at risk for diabetes to attend diabetes screening camps | ASHAs |
| Primary Prevention | |
| Screen for diabetes and confirm the diagnosis | ANMs |
| Good control of blood glucose, and hypertension and dyslipidemia, if present | Physicians at all levels |
| Promote lifestyle changes to improve control of the above | Physicians, counsellors, peer support groups |
| Secondary Prevention | |
| Referral for retinal screening/retinal examination by an ophthalmologist | NCD staff and physicians at all levels |
| Integrated visual acuity measurement and retinal screening for DR in vision centers/NCD clinics in CHCs and district hospitals; in physicians and endocrinologists clinics using nonmydriatic digital fundus camera | Screening can be undertaken by the following, if competent after training: ophthalmic officers/assistants or equivalent, NCD nurses, other healthcare professionals |
| Grading images, with referral of those with signs of mild or more severe DR, or who fail screening for other reasons (e.g., poor image quality; reduced visual acuity). Annual screening for those with no or minimal DR | Ophthalmologists/diabetic eye screeners trained in image grading |
| Manage vision threatening DR, with regular follow-up | Trained ophthalmologists |
| Tertiary Prevention | |
| Treat DME associated with loss of vision | Trained ophthalmologists |
| Manage advanced DR, if indicated, at the discretion of the ophthalmologist | Retina specialists in centers of excellence |
| Rehabilitation for those with irreversible loss of vision | Rehabilitation workers |
ASHA: Accredited Social Health Activist; ANM: Auxiliary Nurse Midwife; DR: Diabetic Retinopathy; NCD: Noncommunicable Diseases; DME: Diabetic Macular Edema
Table 3.
Activities that can be undertaken at different public health facilities
| Activities | PHC/CHC/HWCs | Diabetes centers/clinics (NCD clinics) | Vision center | Secondary center | Tertiary center |
|---|---|---|---|---|---|
| Diabetes screening | |||||
| History | + | + | + | + | + |
| Blood test | + | + | + | + | + |
| DR screening | |||||
| Visual acuity measurement | + | + | + | + | + |
| Dilated eye examination: direct ophthalmoscopy or slit-lamp biomicroscopy | + | + | + | ||
| Fundus photography | +/- | + | +/- | + | + |
| Distribution of IEC material | + | + | + | + | + |
| Counseling and referral to secondary/tertiary eye care centers | + | + | + | + | + |
PHC: Primary Health Center; CHC: Community Health Center; HWC: Health and Wellness Center; NCD: Noncommunicable Diseases; DR: Diabetic Retinopathy; IEC: Information, Education and Communication
The principal purpose of screening for DR is to detect retinopathy that warrants a more detailed examination by an ophthalmologist followed by treatment if required. During screening, other eye conditions associated with diabetes, such as cataract and retinal vein occlusions, may be detected. Visual acuity measurement is very important in people with DM and should be done during each visit to diabetic and eye care facilities. Anyone with reduced vision in one or both eyes (vision of less than 6/12) should be referred, even if no DR is detected on screening. This is because they may have diabetic macular edema (DME), which cannot always be detected during screening.
Any healthcare professional suitably trained can screen for DR: ophthalmic officers/assistants/optometrists, (noncommunicable disease) NCD nurses, physicians, and trained technicians. All those involved in the screening for DR (diabetic eye screeners) need to undergo appropriate training in the use of nonmydriatric digital fundus camera and storage and grading of images with documentation of the findings. Fundus imaging will be the mainstay for screening in the foreseeable near future. Pupil dilation should not be practiced if no eye care personnel are available and in such situations the nonmydriatic images may need to be read remotely. If the images are read remotely, adequate internet bandwidth should be available to transmit the images. It is imperative that the results of screening are communicated to all patients screened in a timely fashion.
Counseling patients before treatment is critical to ensure patients understand what the treatment entails, the possible complications, the need for close follow-up after treatment, and the need for a very long follow-up of patients treated for DR and DME. Information, education, and communication (IEC) materials that are in simple language, preferably in the local vernacular need to be provided.
Tracking people with DM needing retinal examination is an essential component for success of a DR screening and management program. Tracking helps identify if the persons with DM referred have access to the screening and treatment services. Tracking should be bi-directional: forward tracking of people with DM requiring screening for diabetes/DR, with backward feedback to those screened/managed for DR. Backward tracking is necessary to check compliance with medical advice, such as keeping follow-up schedules, taking medications, etc.
Discussion
The success of a DR program depends on:
Awareness generation among the general population about diabetes and its complications and the need for regular screening for DR and eye disease
Capacity building by providing necessary human resources and equipment in the health facilities to carry out screening and management of VTDR and other eye diseases
Periodic training of the healthcare staff on diabetes screening, DR screening, and management for knowledge enhancement.
The availability of guidelines is a step toward providing quality need-based services. However, the mere availability of guidelines does not result in improved quality as the recommendations have to be enforced. Without an enabling environment which supports regular use of the guidelines, success cannot be guaranteed. A study in the United States observed that there was a disconnect between primary care physician's stated adherence to screening guidelines and actual practice.[10] This has to be guarded against.
Conclusion
This is the first set of guidelines on the screening and management of DR in India which highlights the need, potential, and possible strategies at different levels of the public health system to operationalize an integrated program. This will be a useful supplement to the technical guidelines which showcase the evidence-based clinical interventions that can be implemented for tackling visual loss in diabetes.
Financial support and sponsorship
The Queen Elizabeth Diamond Jubilee Trust, London, UK.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Tandon N, Anjana RM, Mohan V, Kaur T, Afshin A, Ong K, et al. The increasing burden of diabetes and variations among States in India: The Global Burden of diseases Study 1990-2016. Lancet Glob Health. 2018;6:e1352–62. doi: 10.1016/S2214-109X(18)30387-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Indian Institute of Public Health, Hyderabad. Guidelines for the Prevention and Management of Diabetic Retinopathy and Diabetic Eye Disease in India. Version 1. Hyderabad, India: Indian Institute of Public Health, Hyderabad; 2019. pp. 1–91. [Google Scholar]
- 3.National Health Mission. Operational guidelines: Prevention, Screening and Control of Common Non-communicable Diseases: Hypertension, Diabetes and Common Cancers (Oral, Breast, Cervix). National Health Mission. 2018. [Last accessed on 2018 Nov 20]. pp. 1–48. http://nicpr.res.in/images/PDF/guidelines_for_population_level_screening_of_common_NCDs.pdf .
- 4.Indian Institute of Public Health, Hyderabad. Operational Guidelines for the Control of Visual Loss from Diabetic Retinopathy in India, 2019. Hyderabad: Indian Institute of Public Health; 2019. pp. 1–47. [Google Scholar]
- 5.Humphrey-Murto S, Varpio L, Wood TJ, Gonsalves C, Ufhoiz LA, Mascioli K, et al. The use of the Delphi and other consensus group methods in medical education research: A review. Acad Med. 2017;92:1491–8. doi: 10.1097/ACM.0000000000001812. [DOI] [PubMed] [Google Scholar]
- 6.Hassanein M, Al-Arouj M, Hamdy O, Bebakar WMW, Jabbar A, Al-Madani A, et al. Diabetes and Ramadan: Practical guidelines. Diabetes Res Clin Pract. 2017;126:303–16. doi: 10.1016/j.diabres.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 7.Gudlavalleti VS, Shukla R, Batchu T, Malladi BV, Gilbert C. Public health system integration of avoidable blindness screening and management, India. Bull World Health Organ. 2018;96:705–15. doi: 10.2471/BLT.18.212167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Government of India-WHO Collaborative Programme 2008-2009. National Programme for Prevention and Control of Diabetes, Cardiovascular Disease and Stroke: A Manual for Medical Officers. [Last accessed on 2019 May 31]. Available from: http://www.searo.who.int/india/topics/cardiovascular_diseases/NCD_Resources_COMBINED_MANUAL_for_medical_officer.pdf .
- 9.National Programme for Control of Blindness, Ministry of Health and Family Welfare, Government of India. [Last accessed on 2019 Jun 03]. Available from: http://npcb.nic.in/
- 10.Mehta S, Mocarski M, Wisniewski T, Gillespie K, Venkat Narayan KM, Lang K. Primary care physicians' utilization of type 2 diabetes screening guidelines and referrals to behavioral interventions: A survey-linked retrospective study. BMJ Open Diab Res Care. 2017;5:e000406. doi: 10.1136/bmjdrc-2017-000406. [DOI] [PMC free article] [PubMed] [Google Scholar]