Abstract
Purpose:
Complications of diabetes mellitus (DM) are a public health problem globally. DM management entails medication and self-management. Peer support groups (PSGs) can improve self-management and promote healthy behavior. The objectives of this study were to design, establish, and evaluate two PSG models for people who had been screened for diabetic retinopathy to assess self-reported lifestyle changes, satisfaction with meetings and barriers to attendance.
Methods:
Peer groups were established using a pre-tested facilitator's guide in 11 locations in 3 states. Group members were oriented on diabetes management and lifestyle changes to improve control. Attendees' experiences were ascertained through semi-structured interviews and self-report. Data were analyzed using MS Excel 2017.
Results:
Eleven PSGs were established in 3 states, in 10 community health centers and one eye hospital. 53 sessions were held and 195 people attended on 740 occasions. Lifestyle changes most frequently reported between first and second visits were taking medication regularly and dietary modification. Attendance declined in the eye hospital group. 83% of CHCs members were satisfied or very satisfied compared with 37% of eye hospital (EH) members. The barriers included distance and lack of family support.
Conclusion:
PSGs held in CHCs were more sustainable than those in an eye hospital, and group members were more satisfied and more likely to report positive lifestyle changes. Findings were self-reported and hence a major limitation for the study. Further studies should focus on obtaining objective measures of control of diabetes and risk factors for diabetic retinopathy from members attending peer support groups in CHCs.
Keywords: Diabetes mellitus, diabetic retinopathy, health systems, India, peer support, uptake
Approximately 75 million Indians are known to be living with diabetes mellitus (DM) and an almost equal number are undiagnosed.[1] DM can have micro- and macrovascular complications and evidence shows that good control of hyperglycemia and other risk factors reduce the incidence of these complications, including diabetic retinopathy (DR). DM management also includes self-management,[2] which has been described as “The tasks individuals must undertake to live with one or more chronic conditions. These tasks include having the confidence to deal with medical management, role management and emotional management of their conditions”.[3]
Peer support groups (PSGs), which have the potential to provide “support from a person who has experiential knowledge of a specific behavior or stressor and similar characteristics as the target population”,[4] can have positive outcomes in chronic conditions by improving self-management.[5] They can vary in several aspects: involve groups or one-to-one interactions; be based in clinics, hospital or in the community, and use health workers or laypersons as facilitators.[4] Heterogeneous membership in relation to characteristics such as education, duration of disease, and degree of control is encouraged, as this promotes peer-learning.
Studies indicate that PSGs can lead to a 0.76% reduction in glycosylated hemoglobin (HbA1C) levels among people with diabetes (PwDM),[4] increase the proportion of people with good control from 28% to 39% and PSGs with health worker participation show positive outcomes.[4] The World Health Organization advocates PSGs for PwDM in conjunction with appropriate medical management.[4] Many countries, including India, have used PSGs and have achieved positive results,[6,7,8] including reduced HbA1C levels and greater utilization of health care facilities. The factors limiting PSGs' success include the location and timing of sessions and lack of instructions about diabetes by experts.
Due to this, potential PSGs were pilot tested within a pilot DR project in India.[9] The objectives were to design and deliver different models of PSGs in rural India, to ascertain which model led to positive behavior change and to explore barriers to scaling up. This was an exploratory, descriptive study to identify factors associated with the establishment and sustainability (i.e., more than three sessions held) of PSGs at three sites in India.
Methods
Mixed methods were used. A PSG facilitator guide was developed, and PSGs were established in community health centers (CHC) or in a partner eye hospital. The study lasted 9 months with PSGs meetings over 7 months. Quantitative and qualitative data were collected throughout and were analyzed using MS Excel 2017.
The study was conducted in three districts in three states (Surat district, Gujarat; Tumkur district, Karnataka; Wardha district, Maharashtra) between August 2018 and May 2019.
A team drafted the facilitator guide after reviewing the literature and capturing experiences of researchers in India via calls and e-mails. The guide included a range of topics [Table 1].[10,11] The draft was pre-tested at a location with PSG experience and changes were made based on feedback.
Table 1.
Facilitator guide topics
| Purpose of peer support group meetings: Introduction and benefits |
| Planning peer group meeting: location, participant selection, topic selection, guidelines for facilitators and tasks before, during and after meeting |
| Interaction session: preparation and logistics. Group dynamics and training aids for facilitators |
| Dos and don’ts of sessions |
| Content for facilitators for peer group meetings: Introduction to diabetes, diabetic retinopathy, diet modification, sample sessions, role-play |
A research team worked with three-partner nongovernment eye hospitals to establish PSGs and identify peer facilitators who could motivate other group members to attend, or re-attend if they had defaulted. PSGs were established in eye hospitals (EHs) or CHCs. Group members were selected if they had been screened for DR, and no new members joined the groups later. Identifying and motivating PwDM to attend meetings was undertaken by NGO staff for PSGs in the EH, and by NGO staff, and ASHA workers for CHC PSGs. The lead researcher, who also has DM, conducted the initial meetings in each location. At each meeting, one topic was discussed, which had been selected by members or the NGO partner and lead researcher. Initially, the PSGs were held at monthly intervals. Later, PSGs at CHCs were held every 2 months because a specialist could not be available to address monthly meetings.
To assess lifestyle changes that would improve self-management of diabetes a semi-structured, open-ended questionnaire was developed. Data were collected on sociodemographic data, lifestyle variables, visits to health facilities, and satisfaction with PSG [Table 2]. For the latter a Likert score (1–5) was used where 5 was “extremely satisfied” and 1 was “extremely unsatisfied.” For understanding lifestyle changes and barriers, open-ended questions were employed, the responses analyzed, and themes identified. To track the change in lifestyle variables at every meeting, members were asked to self-report lifestyle changes in how regularly they took their medication, their diet and daily exercise, and the number of hospital visits to obtain medication since the previous meeting. The questionnaire, which was translated into the local language and adapted and finalized after feedback from the NGO partners, was administered by a trained investigator. Lifestyle data were only included in the analysis for members who had attended for more than one session. As numbers declined over time, findings at baseline were compared longitudinally with findings at the second visit.
Table 2.
Overview of the data collected during the study
| Variable | Baseline | At every subsequent attendance |
|---|---|---|
| Socio-demographic data | Documented | NA |
| Medication taking pattern | Documented | Self-reported change in medication |
| Diet | Documented | Self-reported change in diet |
| Lifestyle | Documented | Self-reported change in lifestyle |
| Health care facility visits | Documented | Visits made since previous attendance |
| Satisfaction | Not applicable | Scored at the end of every session attended |
| Barriers in attending the session | Not applicable | Self-reported |
| How sessions could be improved | Not applicable | Self-reported |
Ethical approval was obtained from the Indian Institute of Public Health, Hyderabad. Verbal informed consent was obtained from all PSG members at the first meeting by the NGO partners in the local languages.
Results
Eleven PSGs were established, in 1 EH and in 10 CHCs. 53 of the 100 planned sessions took place [Table 3]. Only three PSG meetings were held in the EH and 50 were held in the CHCs (mean 9.6, range 9–11). 195 people attended the first sessions. Females predominated (621, 83.9%) and 75.6% were > 60 years of age [Table 4]. Members attending the EH PSG traveled an average of 45 km, which took 3 h; those attending CHC PSGs traveled an average of 25 km, which took 1 h.
Table 3.
Comparison of baseline and follow-up scores and level of satisfaction among people with diabetes attending peer group meetings in an eye hospital and community health centers in three states
| Peer groups | Eye hospitals | Community health centers | Total | ||||
|---|---|---|---|---|---|---|---|
| Number of groups (N) | 1 | 10 | 11 | ||||
| Meetings planned (N) | 9 | 90 | 100 | ||||
| Meetings held (N) | 3 (33%) | 50 (56%) | 53 (53%) | ||||
| Members (N) | 32 | 163 | 195 | ||||
| Attendances | 56 | 684 | 740 | ||||
| Time period of meetings | 3 months | 7 months | |||||
| Health-workers involved | NGO workers | ASHA/NGO workers | |||||
| Lifestyle factors* | Baseline n=23 | After n=23 | % Change | Baseline n=100 | After n=100 | % Change | |
| Take medicines on time | 2 (9%) | 3 (13%) | 4% | 21 (21%) | 45 (45%) | 24% | |
| Modified diet | 1 (4%) | 2 (9%) | 5% | 10 (10%) | 26 (26%) | 16% | |
| Daily walking | 19 (83%) | 23 (100%) | 19% | 5 (5%) | 10 (10%) | 5% | |
| Regular follow up | 15 (65%) | 16 (70%) | 5% | 1 (1%) | 4 (4%) | 3% | |
| Level of satisfaction** | n=32 | % | n=143 | % | All (n=175) | ||
| Extremely satisfied | 9 | 28% | 90 | 63% | 99 (57%) | ||
| Satisfied | 3 | 9% | 38 | 27% | 41 (23%) | ||
| Neutral | 2 | 6% | 9 | 6% | 11 6%) | ||
| Dissatisfied | 7 | 22% | 6 | 4% | 13 (7%) | ||
| Extremely dissatisfied | 11 | 35% | 0 | 0% | 11 (6%) | ||
*At 2nd visit compared with the first visit, *At last visit, or first visit if only attended once
Table 4.
Age and sex distribution of the peer group members
| Age group (years) | Male | Female | Total | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| 40-50 years | 13 | 10.9% | 65 | 10.5% | 78 | 10.5% |
| 51-60 years | 16 | 13.4% | 86 | 13.8% | 102 | 13.8% |
| 61-70 years | 71 | 59.7% | 373 | 60.1% | 444 | 60.0% |
| ≥71 years | 19 | 16.0% | 97 | 15.6% | 116 | 15.7% |
| Total | 119 | 100% | 621 | 100% | 740 | 100% |
| Mean age | 60.9 years (SD±11.6) | 59.5 years (SD±10.8) | ||||
Members attended on a total of 740 occasions with wide variation in the number per site and per meeting [Fig. 1], which declined over time from an average of 32 to 5.3. Two PSGs ended before the 4th meeting, one at each location. The average attendance at PSGs with more than 1 session was 16/session and 67% of members attended more than one session.
Figure 1.
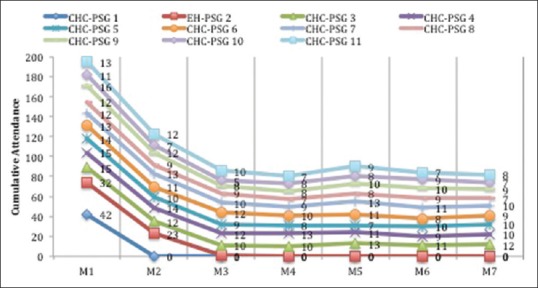
Cumulative attendance at peer support group (PSG) meetings over the study period, by the site. M = Month of peer group meeting, CHC-PSG = Community health center peer support group, EH-PSG = Eye hospital peer support group
People attending CHC PSGs reported greater positive lifestyle changes than EH PSG members [Table 3], particularly in taking their diabetes medication more regularly (24% increase) and more frequent daily exercise (15% increase). Those attending CHC meetings were also more satisfied, with 80% reporting that they were satisfied or extremely satisfied [Table 3] compared with 37% in those attending the EH PSG. Barriers to attendance included distance, and a lack of household decision-makers to support changes such as diet modification or regular exercise, especially among older rural women.
Discussion
In this study, CHC PSGs were more sustainable than EH PSGs, which may reflect the lower recruitment and greater distances members had to travel to attend the EH.[12] CHC PSGs members were also more satisfied and likely to report positive lifestyle changes, particularly in taking their medication more regularly. These changes are consistent with other studies.[6] However, with only one EH PSG the sample was too small to draw definitive conclusions. The PSGs in CHCs used ASHAs who are likely to know their communities and may have contributed to the higher recruitment and sustained attendance. Elderly rural women found it more difficult to attend and make lifestyle changes, which likely reflect social and cultural factors limiting their autonomy.
A limitation is that only verbal information on the member's educational status was obtained, and outcomes were self-reported. Further studies should investigate whether reported lifestyle changes translate into better control of hyperglycemia and other risk factors using objective measures. The period of time individuals need the support of a peer group and whether they can ultimately be self-sustaining are factors which affect whether PSGs are scalable.
Conclusion
PSGs held in CHCs were more sustainable than those in an eye hospital, and group members were more satisfied and were more likely to report positive lifestyle changes. This being a study based on self-reported outcomes, future studies should focus on obtaining objective measures of control of diabetes and risk factors for diabetic retinopathy from members attending peer support groups in CHCs.
Financial support and sponsorship
The Queen Elizabeth Diamond Jubilee Trust, London, UK.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
I would like to acknowledge the support and continuous effort of Dr. Krishna Murthy from VIIO, Mr. Vinuth from VIIO, Mr. Vimal Prajapati from Divyajyoti Trust for their dedication towards organizing the PSGs at their respective states. A special mention to all the Postgraduate students (ophthalmology), the interns posted at the ophthalmology department and the fieldwork staff at MGIMS, Sevagram for their dedication and efforts towards the initiation and sustenance of the PSGs in Maharashtra. I would also like to thank Dr. Dinesh, Ophthalmologist, District Hospital, Tumkur for allowing us to conduct the PSG at the district hospital, Tumkur.
References
- 1.International Diabetes Federation. 8th ed. 2017. [Last accessed on 2018 Nov 25]. Available from: https://idf.org/e-library/epidemiology-research/diabetes-atlas.html .
- 2.Heisler M, Choi H, Mase R, Long JA, Reeves PJ. Effectiveness of technologically enhanced peer support in improving glycemic management among predominantly African American, low-income adults with diabetes. Diabetes Educ. 2019;45:260–71. doi: 10.1177/0145721719844547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adams K, Greiner AC, Corrigan JM, editors . Committee on the Crossing the Quality Chasm: Next Steps Toward a New Health Care System The 1st Annual Crossing the Quality Chasm Summit – A Focus on Communities. Washington, DC: The National Academies Press; 2004. [Last accessed on 2019 Oct 05]. Available from: http://wwwnapedu/catalog/11085html . [PubMed] [Google Scholar]
- 4.World Health Organization. Peer Support Programmes in Diabetes. Geneva: 2008. pp. 1–22. [Google Scholar]
- 5.Dennis CL. Peer support within a health care context: A concept analysis. Int J Nurs Stud. 2003;40:321–32. doi: 10.1016/s0020-7489(02)00092-5. [DOI] [PubMed] [Google Scholar]
- 6.Dale JR, Williams SM, Bowyer V. What is the effect of peer support on diabetes outcomes in adults? A systematic review. Diabet Med. 2012;29:1361–77. doi: 10.1111/j.1464-5491.2012.03749.x. [DOI] [PubMed] [Google Scholar]
- 7.Paul G, Keogh K, D'Eath M, Smith SM. Implementing a peer-support intervention for people with type 2 diabetes: A qualitative study. Fam Pract. 2013;30:593–603. doi: 10.1093/fampra/cmt027. [DOI] [PubMed] [Google Scholar]
- 8.Thankappan KR, Sathish T, Tapp RJ, Shaw JE, Lotfaliany M, Wolfe R, et al. A peer-support lifestyle intervention for preventing type 2 diabetes in India: A cluster randomized controlled trial of the Kerala Diabetes Prevention Program. PLoS Med. 2018;15:e1002575. doi: 10.1371/journal.pmed.1002575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gudlavalleti VS, Shukla R, Batchu T, Malladi BVS, Gilbert C. Public health system integration of avoidable blindness screening and management, India. Bull World Health Organ. 2018;96:705–15. doi: 10.2471/BLT.18.212167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Partners for Health. Training of Trainers: A manual for training facilitators in participatory teaching techniques. [Last accessed on 2019 Oct 05]. Available from: https://www.pih.org/practitioner-resource/training-of-trainers .
- 11.OMNI: Toolkit for Conducting Focus Groups. OMNI: 32. [Last accessed on 2019 Oct 05]. Available from: https://www.nyla.org/max/userfiles/Documents/D._Focus_Group_Toolkit.pdf .
- 12.Klug C, Toobert DJ, Fogerty M. Healthy Changes™ for living with diabetes. Diabetes Educ. 2008;34:1053–61. doi: 10.1177/0145721708325886. [DOI] [PMC free article] [PubMed] [Google Scholar]


