INTRODUCTION
Anxiety disorders are the most prevalent psychiatric disorders worldwide, with a lifetime prevalence of up to 33%.[1] They often run a chronic course and are highly comorbid with other anxiety and mood disorders. Anxiety disorders are associated with immense healthcare costs and huge burden. Despite the availability of evidence-based interventions, they are often underrecognized and undertreated. The major anxiety disorders in the current classificatory system include panic disorder (PD), generalized anxiety disorder (GAD), specific phobia, and social anxiety disorder (SAD). Obsessive–compulsive disorder (OCD) has been nosologically separated from anxiety disorders and classified under the section of obsessive–compulsive and related disorders (OCRDs) in the DSM-5[2] and ICD-11.[3] Commonly described disorders in this category include OCD, body dysmorphic disorder (BDD), body-focused repetitive behaviors (BFRBs, i.e., trichotillomania and skin-picking disorder), and hoarding disorder.
Both pharmacological and psychological interventions are effective in treating anxiety disorders and OCRDs. Clinical practice guidelines often recommend cognitive-behavioral therapy (CBT) as a first-line treatment for both anxiety disorders and OCRDs. In the following sections, we discuss scientifically tested CBT models, their evidence base, and treatment recommendations for individual disorders. Treatment recommendations are graded based on the Strength of Recommendation Taxonomy system, with three levels of recommendation, based on the quality, quantity, and consistency of evidence [Table 1].[4]
Table 1.
Grading of recommendation based on Strength of Recommendation Taxonomy
| Strength of recommendation | Definition | Examples |
|---|---|---|
| A | Consistent and good-quality patient-oriented evidence | Meta-analysis of RCTs with consistent findings or high quality individual RCT |
| B | Inconsistent or limited-quality patient-oriented evidence | Systematic review/meta-analysis of lower quality clinical trials or studies with inconsistent findings/lower quality |
| C | Consensus-based evidence | Extrapolations from bench research, disease-oriented evidence, usual practice, opinion, case series |
RCT – Randomized controlled trials
PANIC DISORDER
PD is often a chronic illness with waxing and waning course characterized by recurrent and unexpected panic attacks. The panic attacks are usually associated with anticipatory anxiety/worry of having another panic attack or consequences of the attack and maladaptive behaviors such as avoidance, safety behaviors, and changes in daily routine. Patients often develop agoraphobia in response to panic attacks. Lifetime prevalence of PD ranges between 1.6% and 5.2%, and it is about two times more common in women than in men.[1] PD is often comorbid with other psychiatric disorders, particularly anxiety, mood, and substance use disorders.
Assessment
Patients with PD often focus on physical symptoms and attribute their symptoms to medical causes. Ruling out medical causes of panic attacks is an important aspect of assessment. Proper diagnosis and assessment of severity of the panic and comorbid disorders play an important role in planning therapy. Comorbidity generally adds to the severity of symptoms, functional impairment, and economic costs and is associated with slower rate of response. For example, the presence of severe depression may interfere with the therapy for PD. Therefore, it is important to assess for comorbid conditions and treat them.
Commonly used instruments to diagnose and assess panic attacks are shown in Table 2. Behavioral analysis of the problem is an important aspect of assessment that would provide information on predisposing, precipitating, and perpetuating biopsychosocial and lifestyle factors. Some of the major points gathered by behavioral analysis are shown in Table 3. Comprehensive assessment would aid in identifying the targets of therapy and choosing therapeutic components and appropriate assessment methods to monitor outcome. Having a collaborative therapeutic relationship is crucial for obtaining adequate information, enhancing motivation, and ensuring participation in therapy.
Table 2.
Instruments for assessing panic disorder
| Name of the scale | Purpose |
|---|---|
| Physical sensation self-monitoring scale[5] | Assesses for intensity and anxiety regarding physical sensations to provide information on interoceptive triggers |
| Severity Measure for Panic Disorder-Adult[6] | Severity of panic disorder |
| Panic disorder severity scale[7] | 7 items on 5-point scale (0-4) to assess severity of panic disorder |
| Panic and agoraphobia scale[8] | Severity of panic disorder and agoraphobia |
| Weekly Panic Log[9] | Provides contextual information about panic attacks, their symptom expression, anxious appraisal, reappraisal capacity and coping resources |
| Agoraphobic cognitions questionnaire[10] | Measures the frequency of thoughts about catastrophic consequences of anxiety and panic |
| Body sensations questionnaire[10] | Assesses fear associated with physical symptoms of arousal |
| Anxiety sensitivity index[11] | Measures symptoms of anxious arousal |
| Mobility inventory[12] | Measures avoidance of typical agoraphobic situations |
| PAI[13] | Consists of three separate scales for assessing the cognitive appraisal patterns of panic sufferers (anticipated panic, panic consequences and panic coping) |
PAI – Panic appraisal inventory
Table 3.
Behavioral Analysis of panic disorder
| 1. Nature, intensity, frequency, and duration of the symptoms |
| 2. The situations/triggers for the symptoms, internal (e.g., tightness of chest, difficulty in breathing, nausea, increased heart rate, feeling tense/restless, dizziness, feeling unreal) and external (e.g., being at home alone, crowds, elevators, shopping malls, crossing bridges, theatres, public transport) |
| 3. Feared consequences of the symptoms (e.g., fear of death, heart attack, and “going crazy” or losing control) |
| 4. The factors that maintain the symptoms, i.e., avoidance, safety behaviors, accommodation and reinforcement of symptoms by family members |
| 5. History of mental health and physical health problems in self and family, any adverse experiences in the family |
| 6. Socio-cultural factors, relationships, support systems, and expectations of the patient and family members regarding treatment |
| 7. Attempts made by the individual to overcome the problem. Awareness regarding the problem and psychological interventions |
Formulating a treatment plan
Formulating the treatment plan would be based on the targets identified during assessment, which is communicated to the patient. Formulation often includes presenting a model of panic and factors maintaining the disorder, as well as the treatments available. The formulation should also include education about comorbid symptoms if present. The formulations are delivered according to the need, receptivity, and understanding of the patient. Presenting a formulation gives confidence to the patients that their symptoms can be understood, explained, and treated.
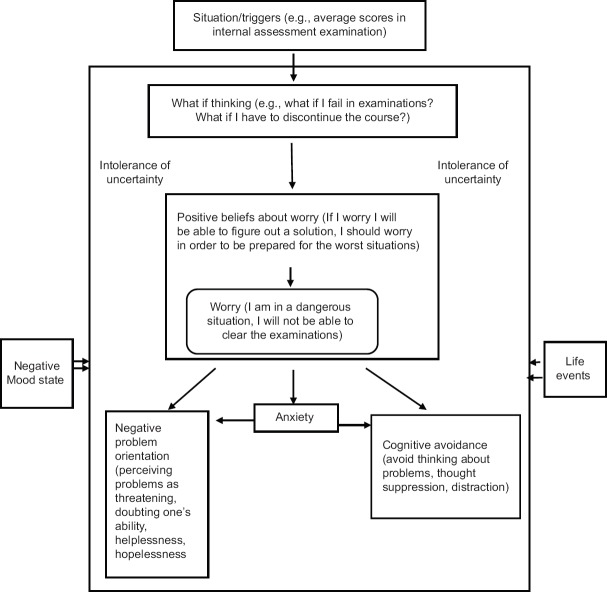
The typical CBT model is based on the catastrophic misinterpretation of interoceptive stimuli. The model emphasizes a vicious cycle of catastrophic misinterpretation of normal bodily sensations, resulting in anxiety symptoms (arousal symptoms), interpretation of anxiety symptoms as indicators of impending dangerous consequences which further worsens the problem, and consequent avoidance and safety behaviors leading to maintenance of fear and anticipatory anxiety [Figure 1].[14] The standard components of individual CBT are summarized in Table 4.[15,16] The steps involved in administering CBT are shown in Figure 2.
Figure 1.
Cognitive model of panic disorder
Table 4.
Components of cognitive behavioral therapy for panic disorder
| Components | Description |
|---|---|
| Educating the patient about panic disorder (psychoeducation) | Educate about symptoms of anxiety and panic disorder, “flight or fight” response and corresponding physiological responses, causes, and maintaining factors (role of avoidance and safety behaviors) Share the clinical case formulation, available treatments, outcome and rationale for CBT Educate the family members and facilitate support |
| Interoceptive exposure (symptom induction) and threat schema activation | Hyperventilation (to induce breathlessness), spin around or staring at a spot continuously (to induce dizzy or faint feeling), run on spot (racing heart), etc. |
| Cognitive restructuring of catastrophic misinterpretation | Addressing catastrophic cognitions, exaggerated threat perception, overestimation of negative consequences of panic and generating alternative benign explanations for symptoms |
| In vivo graded exposure to feared stimuli (particularly in agoraphobia) | Aids in habituation and disconfirmation of feared consequences Reduces avoidance and safety behaviors (presence of companion, carrying eatables, medicines, known location with availability of hospital, toilet, etc.) Therapist uses exposure to challenge catastrophic cognitions |
| Relapse prevention | Prepare the patient for occasional and at times unexpected panic symptoms/attacks and teach what to do if symptoms return Encourage patient to develop realistic expectations of treatment outcome and reduce “fear of fear” Gradually decrease the frequency of therapy sessions and schedule booster sessions |
CBT – Cognitive behavioral therapy
Figure 2.
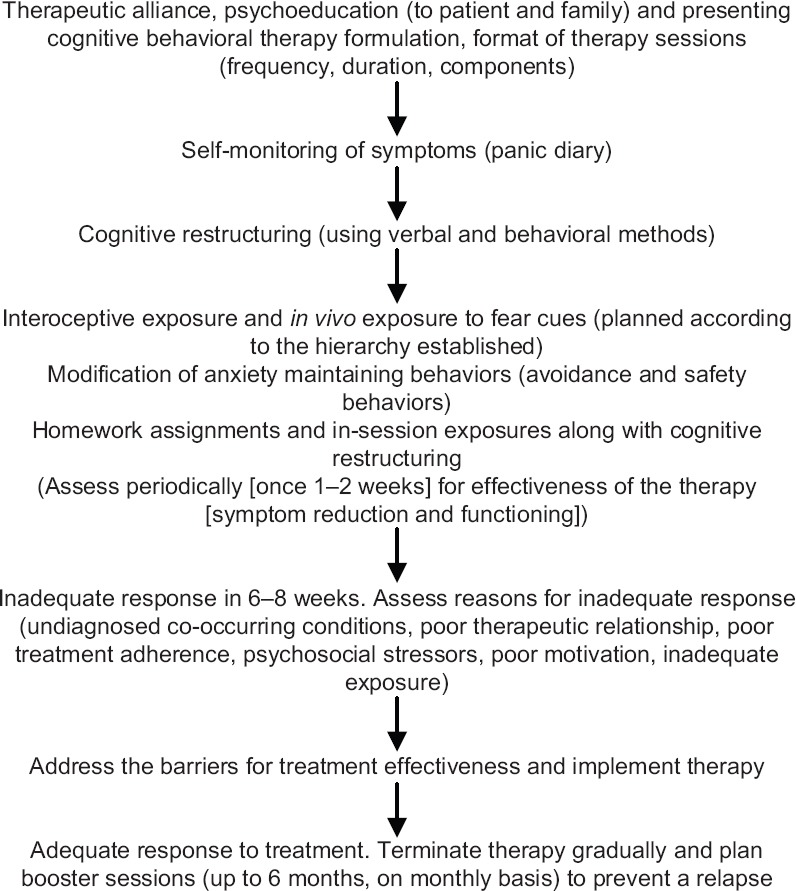
Steps in cognitive behavioral therapy for panic disorder
Choice of treatment settings
Therapy for PD is largely carried out on an outpatient basis. However, in certain situations (e.g., presence of comorbid severe depression/other anxiety disorders/substance abuse or dependence, failed outpatient therapy, and inability to implement therapy on an outpatient basis because of severity of illness), in-patient therapy may be offered.
Efficacy of cognitive behavioral therapy in panic disorder
CBT is the first-line psychological treatment for PD.[17,18] There is well-replicated evidence for short- and long-term effectiveness of CBT.[19] Strength of recommendation for various psychological interventions for PD is shown in Table 5. A recent component network meta-analysis reviewed 72 studies to disentangle the effects of components of CBT and reported that cognitive restructuring, interoceptive exposure, and face-to-face setting were associated with better efficacy and acceptability, while muscle relaxation, breathing retraining, in vivo exposure, and virtual reality exposure (VRE) were associated with lower efficacy.[19] Pharmacological interventions, antidepressants in particular, and CBT appear to be equally efficacious in the treatment of PD.[20] A long-term follow-up study of PD patients treated with CBT reported a relapse rate of 23% over 2–14 years of follow-up period.[21]
Table 5.
Recommendations for psychological interventions in panic disorder
| Therapy | Strength of recommendation |
|---|---|
| Individual face-to-face CBT with exposure (interoceptive exposure and graded in vivo exposure) | A |
| CBT + antidepressants | A |
| Group therapy | B |
| Self-help* CBT (therapist-guided) | B |
| Internet based therapy (self-guided) | B |
| Psychodynamic therapy | B |
| Supportive therapy | B |
| Third-wave therapies | B |
*Internet based and bibliotherapy. CBT – Cognitive behavioral therapy
Delivery of cognitive behavioral therapy
Individual face-to-face mode of CBT is found to be most effective.[19] The number of sessions generally range between 10 and 15 weekly sessions; however, briefer intervention with 6–7 sessions is also shown to be effective.[22] Minimal therapist contact interventions such as bibliotherapy, internet-based CBT, and self-exposure have been studied and found to be more effective than waitlist or relaxation controls. However, unsupervised self-help is found to be less effective than therapist-administered treatments. There is a need to examine cost-effectiveness and acceptability of these interventions.
When to stop treatment
Acute treatment is stopped after addressing the symptoms causing distress, i.e., the target symptoms identified in collaboration with the patient, which may happen over 10–15 weeks. The decision on discontinuation/spacing of the sessions (weekly to fortnightly or monthly) is taken jointly. The patients are prepared for the termination in advance (at the beginning when therapy plan is proposed as well as a few sessions before termination). Patients are prepared for detecting the early warning signs and application of the techniques learned in the therapy. They are also prepared to handle the factors that may trigger panic. It has been found that supplemental CBT, offered at the time of medication withdrawal, has lowered relapse rates in some people. Psychological therapies are found to have a long duration of effect followed by pharmacological therapy and self-help.[19]
Guidance for maintenance and follow-up
Most often, booster sessions carried out over few months would maintain the gains. A randomized controlled trial (RCT) indicated that maintenance CBT carried out monthly over 9 months after acute treatment maintained the gains up to 21 months and had significantly lowered the relapse rate (5.2%) compared to those who did not get maintenance CBT (18.4% relapsed).[23] In some people, continuing booster sessions only during relapse would help. In people where there are multiple psychosocial stressors that contribute to the maintenance of PD, psychological therapies have to be adapted to the mode of maintenance therapy (similar to chronic illness). Augmentation of CBT with mindfulness, acceptance and commitment therapy (ACT), or supportive therapy according to the necessity as assessed by a clinician also might be helpful. However, there is a need to examine the effect of augmentation of therapies in treatment-refractory cases.
GENERALIZED ANXIETY DISORDER
Patients with GAD worry excessively over everyday things and experience excessive anxiety. They find it difficult to control the worry and often experience symptoms, such as restlessness, easy fatigue, concentration difficulties, irritability, muscular tension, and sleep problems. The content of worry would include things within their control as well as which are not under one's control (e.g., illness, future, and community issues) going wrong in a catastrophic way. They involve in behaviors to reduce the worry such as reassurance-seeking, avoidance of events, and mentally preparing for events.
Lifetime prevalence of GAD ranges between 3% and 6%; it is around two times more common in women than in men.[1] GAD has a chronic course with exacerbations during stressful life events. It is associated with significant dysfunction and results in reduced quality of life and economic costs. Less than one-third of the patients seek help and mostly from primary care physicians, often for physical symptoms or for depression. GAD is highly comorbid with other anxiety and mood disorders; in addition, the risk of medical conditions is also elevated.
Assessment
It is important to ascertain the nature and content of worry. Commonly used measures of GAD are given in Table 6. The assessment aims to ascertain the diagnosis of GAD and comorbid (anxiety/mood) disorders and exclude medical conditions with similar presentations (endocrine, cardiopulmonary, and neurological conditions). Behavioral analysis is crucial to understand the individual and environmental factors, contributing to the maintenance of symptoms as well as those that alleviate and aggravate the symptoms [Table 7]. Establishing a good therapeutic relationship and facilitating motivation for therapy are important. It is also crucial to understand the patient's goals and expectation of therapy.
Table 6.
Instruments for assessing generalized anxiety disorder
| Scale | Description |
|---|---|
| Penn state worry questionnaire-ultrabrief version[24] | A 3-item measure of worry severity |
| GAD-7[25] | It is a 7-item screening tool for assessing severity in clinical practice and research |
| GAD Severity Scale[26] | 6-item scale to assess the severity of GAD symptoms |
GAD – Generalized anxiety disorder
Table 7.
Behavioral analysis for generalized anxiety disorder
| 1. Nature (content of worry, somatic symptoms), intensity, frequency, and duration of the symptoms. Any deficits that contribute to worry (e.g., problem-solving skills, communication skills, assertiveness) |
| 2. The situations/triggers for the symptoms, internal (e.g., ill health, worries, symptoms of anxiety) and external (e.g., ill health of family/others, witnessing loss, stressful events in one’s life or other’s life, work demands, changes in personal/family/occupational domains) |
| 3. Feared consequences of the symptoms (e.g., fear of losing control over thoughts, developing mental illness/physical illness – blood pressure and other health problems) |
| 4. The factors that maintain the symptoms, i.e., avoidance, reassurance seeking, safety behaviors, beliefs about need for control and intolerance of uncertainty, accommodation by family members |
| 5. History of mental health and physical health problems in self and family, life events, ongoing stressors, personality traits of anxiety/worry proneness |
| 6. Sociocultural factors (family environment, modeling of anxiety/worry, life style, beliefs about worrying) relationships, support systems, and expectations of the patient and family members regarding treatment |
| 7. Attempts made by the individual to overcome the problem. Awareness of the patient and significant others regarding the problem and psychological interventions |
Formulating a treatment plan
Various cognitive models have tried to explain GAD for avoidance model of worry and GAD, intolerance of uncertainty model, metacognitive model, emotion dysregulation model, and acceptance-based model.[27] The common concepts across various models include cognitive avoidance (experiential avoidance), positive and negative beliefs about worry, poor understanding of emotions and maladaptive coping with emotions (worrying), and poor problem orientation and problem-solving. The individual formulations are tailored according to the presentation of symptoms in a patient.[27]
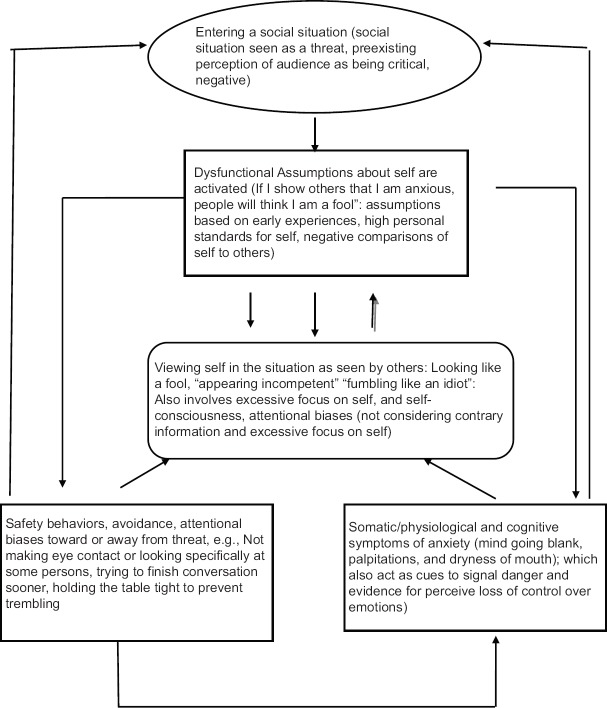
Therapy should be planned based on the baseline assessment, expectations, and preferences of the patient and feasibility. The distress and dysfunction have to be addressed first by working on regularizing the daily activities. CBT programs typically address the physical, cognitive, and behavioral symptoms of GAD. Cognitive model (intolerance of uncertainty model) of GAD is shown in Figure 3.[28] The essential components of CBT are given in Table 8.[5,29,30] Steps involved in the delivery of CBT are shown in Figure 4.
Figure 3.
Cognitive model (intolerance of uncertainty model) of generalized anxiety disorder
Table 8.
Components of cognitive behavioral therapy for generalized anxiety disorder
| Psychoeducation | About GAD: Its symptoms, course and treatment options |
| Educate on nature of worry and cognitive perspective of worry, help distinguish productive from unproductive worry | |
| Self-help reading material on treatment may also be used, if feasible | |
| Cognitive restructuring | Challenge unhelpful thinking such as overestimation of likelihood of harm/something bad happening, intolerance of uncertainty, beliefs on benefits of worry and worry about worrying (beliefs about negative effects of worry) |
| Help shift attention away from worry | |
| Challenge underestimation of one’s ability to cope with the problems | |
| Behavioral strategies | Behavioral avoidance is addressed through graded exposure to activities and situations and minimizing reassurance seeking or over preparing/planning (worry exposure) |
| Worry induction and decatastrophizing (within session and home-work assignments) | |
| Teach problem solving skills for solvable practical problems and social skills training | |
| Self-monitoring would help keep track of the worry across the situations | |
| Arousal reduction and mindfulness strategies (optional) | Physical symptoms of anxiety are addressed through progressive muscle relaxation and breathing retraining. Mindfulness meditation and acceptance exercises also are used to reduce focus on symptoms need for control and experiential avoidance |
GAD – Generalized anxiety disorder
Figure 4.
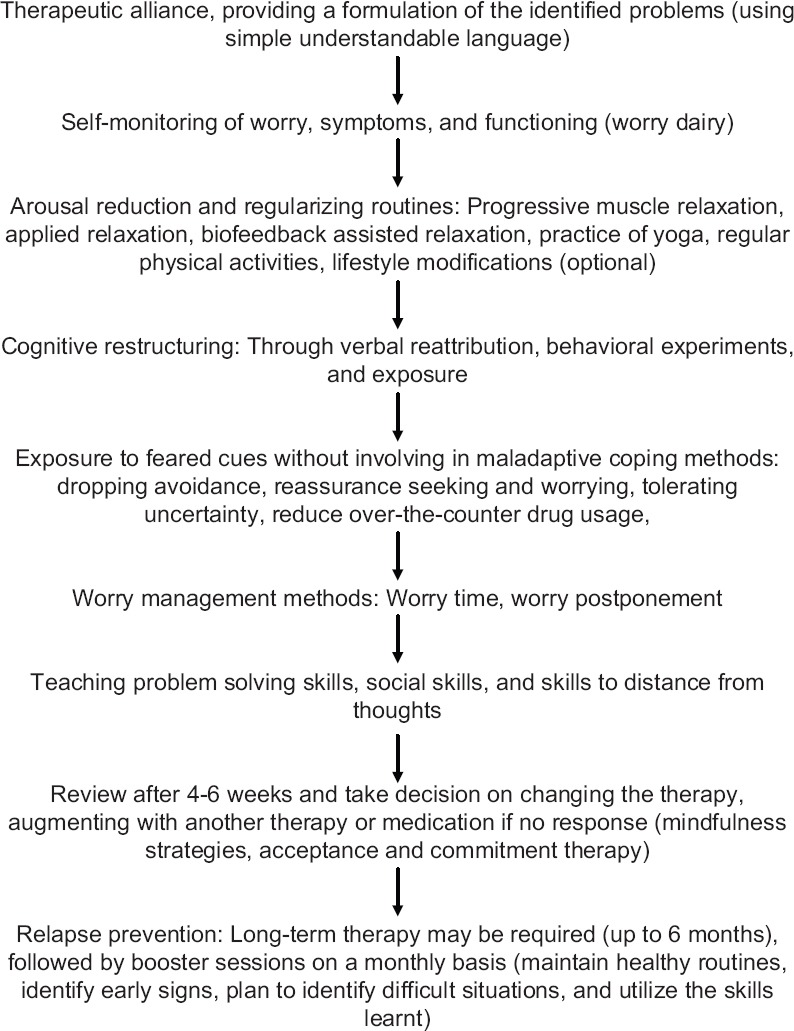
Steps in delivery of cognitive behavioral therapy for generalized anxiety disorder
Choice of treatment setting
CBT for GAD is typically delivered on an outpatient basis. However, in-patient treatment may be considered in the presence of comorbid severe anxiety, OCD, substance abuse, personality disorder, depressive disorders, or self-harm behaviors.
Efficacy of cognitive behavioral therapy for generalized anxiety disorder
CBT is found to be more efficacious than waitlist control condition in treating GAD, but its superiority over other psychotherapies is not established because of paucity of comparative studies.[31] CBT may be helpful for treating comorbid depression, with gains being maintained at 6 and 12 months of follow-up.[31] There is some evidence that CBT may be more effective than applied relaxation.[31] Although both individual and group CBT are equally effective, individual therapy is associated with a larger effect size, earlier improvement in symptoms, and higher adherence. Therapy formats with eight or fewer sessions are also found to be effective; however, more number of sessions may be required when addressing worry and depression.[32] Mindfulness is found to have similar effects compared to CBT and behavior therapies.[33] A meta-analysis has shown that digital/internet-based CBT is superior to waitlist and placebo control while being comparable to face-to-face and group CBT.[34] Transdiagnostic therapies designed to be applicable across various emotional disorders have been found to be helpful, especially in those with comorbid conditions. Comparative efficacy of this intervention vis-a-vis disorder-specific therapy is yet to be evaluated rigorously.[35]
There are a number variants of CBT that have been examined using RCTs with and without replication: applied relaxation, cognitive therapy, mindfulness and acceptance-based interventions, metacognitive therapy (MCT), intolerance of uncertainty therapy, cognitive bias modification, emotion regulation therapy, yoga-enhanced CBT, exercise therapy, and short-term psychodynamic psychotherapy. There is a need for further studies to replicate their effectiveness as well as comparative effectiveness to CBT. Strength of recommendation for various psychological interventions for GAD is shown in Table 9.
Table 9.
Recommendations for psychological interventions in generalized anxiety disorder
| Therapy | Strength of recommendation |
|---|---|
| Individual CBT | A |
| Group CBT | B |
| CBT + pharmacotherapy | B |
| Applied relaxation | B |
| Internet based therapies | B |
| Transdiagnostic therapies | B |
| Third wave therapies | B |
| Psychodynamic psychotherapy | B |
CBT – Cognitive behavioral therapy
When to stop treatment
The number of sessions required for improvement may vary depending on the severity of GAD and response to therapy. Although the optimal duration of therapy is not determined, people with GAD may require more number of sessions, spread over a year. Initial 12–15 sessions may be spaced closely (weekly) followed by more spaced sessions (once a month). Treatment can be terminated either when the targets are achieved or when there is plateauing of response.
Guidance for maintenance and follow-up
There are no agreed upon guidelines for maintenance and follow-up of psychotherapy in GAD. Therapy is generally long term and may require regular follow-up up to 1 year. Open appointments to help handling stressful situations that trigger beliefs of uncertainty/need for control/positive beliefs of worrying would help in coping with stressful situations and reducing severity of symptoms.
SPECIFIC PHOBIA
Phobia is defined as an excessive, irrational fear toward an object or situation that cannot be explained or reasoned away and is beyond voluntary control. A person actively avoids the stimulus or endures it with extreme distress. There is significant impairment in the individual's functioning due to fear. Specific phobic stimuli include animals (spiders, insects, and dogs), natural environment (storms, thunder, and heights), situations (elevators and airplanes), and blood injury phobia (needles and invasive procedures). About 75% have more than one phobia.[2]
Specific phobia is the most prevalent anxiety disorder, with a lifetime prevalence between 8.3%–13.8%.[1] Similar to other anxiety disorders, it has a female: male prevalence ratio of around 2:1.[1] Treatment seeking and utilization in specific phobias are delayed or limited and many do not seek mental health consultations.
Assessment
In addition to a detailed clinical interview, assessment for CBT for specific phobia must include functional analysis of cues, extent of avoidance, safety behaviors, accommodation by others, nature of arousal symptoms, negative automatic thoughts associated with it, and degree of impairment. If there is more than one phobic stimulus, this information is obtained separately for each of them. The functional analysis will also document information on early learning experiences that are likely contributors to the acquisition of the phobia. A fear hierarchy, with an ascending order of the triggering cues, along with subjective units of distress is constructed for the purpose of exposure therapy.
Self-report of fears
The Fear Questionnaire by Mathews and Marks[36] is a self-report measure of fear and avoidance of various stimuli, including blood, traveling alone, social situations, and going to a dentist. Items are marked on both avoidance and distress experienced. Several other measures are available that tap specific fears (spider, dental, and blood injury) and may be used in addition to functional analysis.
Formulating a treatment plan
CBT for specific phobias is based on the learning theories that explain acquisition and maintenance of phobias using the two-factor model, where fear is acquired through classical conditioning (anxiety/aversive experience associated with the stimuli) and maintained through instrumental conditioning (avoidance). Acquisition of fears via modeling (vicarious) and informational learning (social messages) is emphasized by social learning theory. Cognitive models of phobia stress on the role of threat appraisal in the development of specific phobias. Based on these learning and cognitive theories, psychological treatments of specific phobias focus on exposure to phobic stimuli, habituation, and extinction of fear response and reappraisal of threat.
Exposure therapies
Exposure is the treatment of choice in the management of specific phobias and refers to deliberate presentation of the feared stimulus for a prolonged period of time, without engaging in distraction, avoidance, or any other safety behaviors, until the stimuli no longer evoke fear or the fear is significantly reduced. Habituation (to the fear response) and extinction are two key mechanisms by which exposure works.
Exposure can be delivered through several ways. The most effective way is that of in vivo exposure or direct exposure to feared stimuli, followed by imaginal exposure in which the patient is asked to imagine the feared stimuli, and in vitro or virtual reality-based exposure.
Virtual reality exposure
VRE is a technology-based exposure in which the person is exposed to the feared stimulus using a simulated environment within the controlled setting and is immersive and interactive in nature, therefore closest to real-life exposure. VRE has demonstrated efficacy in specific phobias (fear of flying, interactions, and large open spaces), with large-to-moderate effect sizes and maintenance of gains over follow-up.[37]
Despite its demonstrated efficacy, one of the major challenges in exposure therapy is the high attrition rate and refusal to participate in exposure due to intolerance of anxiety. Brief inadequate exposures result in insufficient exposure to feared stimuli, or if safety behaviors or subtle avoidance during exposure result in enhancement of fear response, through incubation.
Modeling is a therapeutic approach based on vicarious learning. Modeling can be achieved by directly modeling the behavior by a role model (e.g., therapist in the session) or through video modeling (e.g., a successful medical procedure). Modeling here is used to promote or facilitate approach behaviors toward the feared object.
Systematic desensitization (SD) is a therapeutic approach is based on the principle of reciprocal inhibition. SD comprises three steps of training in deep muscle relaxation, constructing a fear hierarchy, and presenting the anxiety cues, by juxtaposing them with the experience of relaxation such that relaxation inhibits the anxiety.
While exposure therapy is the treatment of choice for specific phobias, cognitive therapy addresses threat appraisal, in addition to safety behaviors and avoidance. Cognitive therapy in specific phobia is more effective than waitlist control and no treatment controls and may be more indicated when maintaining factors are related to cognitions and safety behaviors than merely the fear response.[38] However, few studies employ cognitive restructuring alone to allow for comparisons between treatments.
Treatment of blood injury phobia
Blood injury phobia is a distinct focal phobia that is characterized by a vasovagal response that results in fainting (syncope), and there is a drop in blood pressure rather than anxiety. Persons with blood injury phobia may additionally have significant avoidance of hospitals and other associated cues such as needles and blood. While exposure is effective in treating avoidance response to generalized cues, applied tension (AT), a technique that raises blood pressure, is recommended when working on exposure to specific cues related to the phobia.[39] AT, a five-session behavioral coping technique, has two components: learning a tension technique and applying it in specific situations. Treatment begins with providing the patient a rationale for AT based on the diphasic response of initial increase in blood pressure and subsequent drop, resulting in fainting. Patient is instructed to note down early cues of this response. Following this, the tension method is introduced, whereby patient is asked to tense, gross muscle groups across arms, chest, and legs, until the patient feels a sense of warmth in the face. In the next three sessions, the patient is exposed gradually to pictures of injury and blood and then to actual settings, such as blood donation and minor surgeries, during which the patient is instructed to apply the tension technique.
Choice of treatment setting
Most patients are treated on an outpatient basis and remain functional in most areas of life.
Efficacy of cognitive behavioral therapy in specific phobia
Review of psychological treatments for specific phobias indicates largest and consistent evidence for exposure therapies. While all modalities of exposure are effective compared to other treatment components, in vivo exposure is superior compared to imaginal and in vitro exposure. Exposure therapies also outperform treatments that do not include exposure as a component, such as applied relaxation with no exposure, only cognitive restructuring, AT. With respect to factors moderating effect size and outcome, type of phobia is not a significant factor; however, the number of treatment sessions was a significant moderator, with multi-session treatments performing better than single-session treatments.[40] Strength of recommendation for various techniques targeting specific phobia is shown in Table 10.
Table 10.
Recommendations for psychological interventions for specific phobia
| Therapy | Strength of recommendation |
|---|---|
| Exposure therapy | A |
| In vivo exposure | A |
| Imaginal exposure | A |
| In vitro exposure | A |
| Systematic desensitization | B |
| Applied tension* | B |
| Cognitive restructuring | B |
*For blood/injury phobia
SOCIAL ANXIETY DISORDER
SAD is a common anxiety disorder, with a lifetime prevalence varying from 3% to 13%.[1] It has an onset in early-to-middle adolescence and is more prevalent among women.[1] SAD is characterized by marked and persistent fear of social (meeting people, attending a social gathering) or performance (public speaking) situations, with fear of being embarrassed, scrutinized, or negatively evaluated. Social situations are avoided or endured with distress. Other clinical features of SAD include experience of physiological arousal (e.g., fear of blushing, sweating, and palpitations) and negative cognitions (e.g., social and/or cognitive catastrophes, such as losing control over emotions and going blank). SAD is marked by functional impairment and is more than normal shyness, although people with SAD may report being shy individuals. SAD is characterized by high degree of psychiatric comorbidity. The most common comorbid conditions include major depressive disorder, other anxiety disorders, substance use disorders, and personality disorders and notably anxious avoidant personality disorder.[41]
Assessment
The most widely used measures in SAD are shown in Table 11. A detailed clinical history and a cognitive behavioral or functional analysis [Table 12] are essential steps in the assessment for therapy. Assessment is aimed at identifying nature of fears, extent of avoidance, fears of negative evaluation, severity of social anxiety, and impairment in functioning and comorbid conditions.
Table 11.
Instruments for assessing social anxiety disorder
| Name of the scale | Purpose |
|---|---|
| Liebowitz Social Anxiety Scale[42] | A 24-item, clinician rated measure of fear and avoidance in social and performance situations |
| BFNE[43] | A 12-item measure of the fear of negative evaluation, a cognitive component in SAD |
| SIAS[44] | This 19-item measure assesses cognitive, affective, or behavioral reaction to a social interaction in dyads or groups |
| SPIN[45] | Screening tool which assesses fear, avoidance, physiological arousal related to social phobia |
| SPRS[46] | Outcome measure consisting of five rating scales assessing key components of the Clark and Wells’ (1995) model[47] of social phobia - distress, avoidance, self-consciousness, frequency of safety-seeking behaviors, and negative beliefs |
SPRS – Social Phobia Rating Scale; SPIN – Social Phobia Inventory; SIAS – Social Interaction and Anxiety Scale; BFNE – Brief Fear of Negative Evaluation scale; SAD – Social anxiety disorder
Table 12.
Behavioral analysis for social anxiety disorder
| 1. The antecedents/situations/triggers of social anxiety (social interactions, performance situations like public speaking, being center of attention, attending social functions, small/large group interactions, introducing self in a group); intensity and magnitude of anxiety, associated anxiety symptoms. These are elicited using specific, recent incidents of social anxiety |
| 2. Specific cognitions (negative automatic thoughts, dysfunctional assumptions, cognitive errors such as mind reading, selective abstraction), anticipated anxiety and outcomes (self-focused attention, fears of going blank, social catastrophes like a making a fool of oneself, losing control over anxiety symptoms, others noticing one’s anxiety) |
| 3. Maintaining factors such as use of safety behaviors (holding a spoon tight to avoid trembling of hands, covering one’s face to avoid attention, excessive rehearsal before a presentation), avoidance (not making eye contact, avoiding meetings, refusing promotions), perfectionistic beliefs regarding self-presentation and social behaviors |
| 4. Early learning experiences (including parenting styles, exposure to anxiety experiences, anxious temperament, sensitivity to criticism, role models (or absence of appropriate role models), social skill deficits, critical events such a bullying, illness or other factors that impact self-image |
| 5. Sociocultural factors, social relationships, support systems, and expectations of the patient and family members regarding role functions and demands |
Formulating a treatment plan
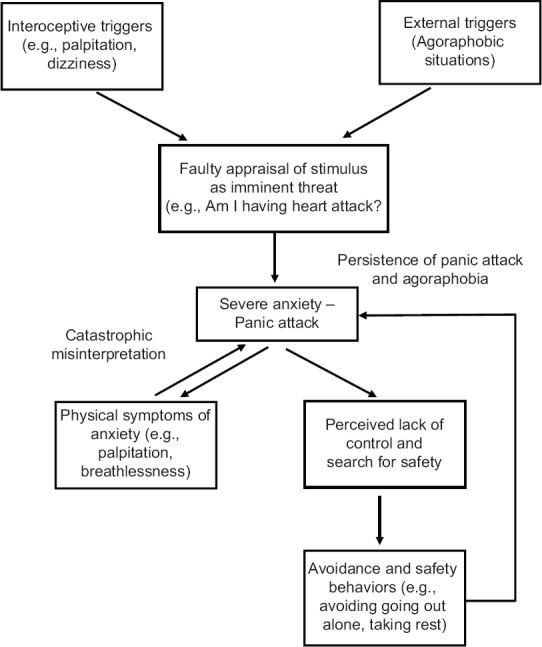
Cognitive models of social anxiety focus on self-focused attention and resultant heightened self-consciousness and self-processing biases,[47] mental representation of self as seen by others and attentional biases to threats in social situations,[48] and metacognitive processes[49] underlying social anxiety. Typical model and the steps involved in administering CBT for SAD are shown in Figures 5[47,48] and 6, respectively.
Figure 5.
Cognitive model of social anxiety disorder
Figure 6.
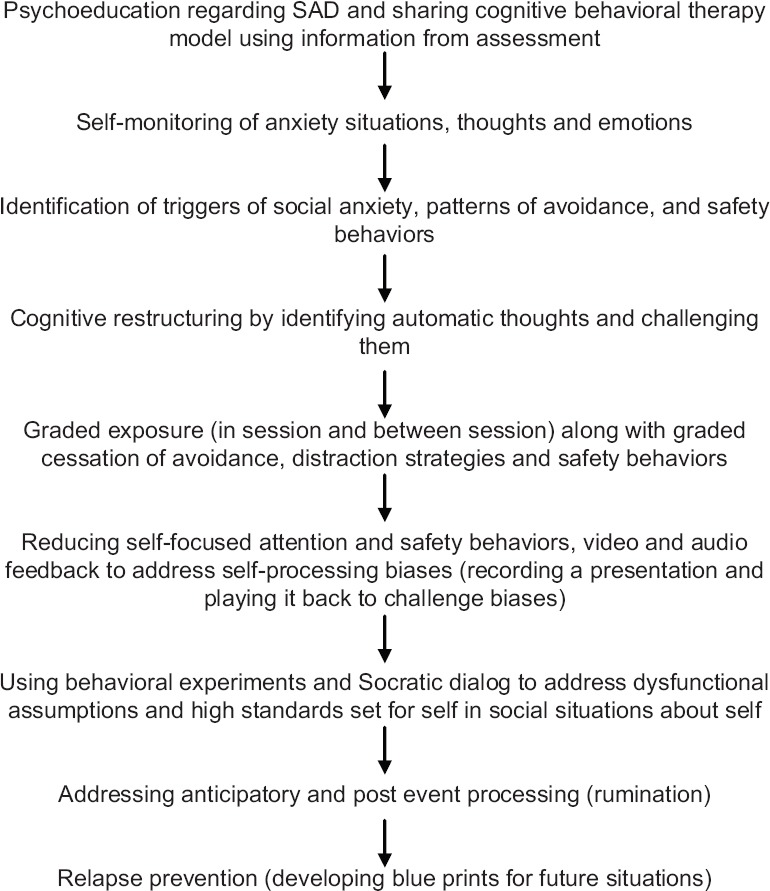
Steps of cognitive behavioral therapy for social anxiety disorder
CBT for social anxiety is typically conducted over 14–16 sessions (weekly, over 3–4 months). The essential components of the program are shown in Table 13. Patients may also be encouraged to use workbooks to maximize gains in therapy.[50] Systematic and repeated practice of skills is essential and the key to better outcomes across all approaches within CBT.
Table 13.
Components of cognitive behavioral therapy for social anxiety disorder
| Components | Description |
|---|---|
| Psychoeducation | Educating client regarding factors contributing to social anxiety, role of safety behaviors, avoidance, and attentional biases in SAD, sharing the CBT model using information from assessment |
| Self-monitoring of anxiety | Self-monitoring of social and performance situations that trigger anxiety, cognitions and emotions associated with them and safety behaviors adopted |
| Cognitive restructuring (for self-processing biases, cognitive errors and beliefs) | Identifying automatic thoughts, cognitive errors, such as mind reading, fortune telling, modifying dysfunctional assumptions and fear of negative evaluation using Socratic dialogue, verbal challenging strategies (e.g., keeping a positive data log, maintain a social balance sheet to gather evidence for and against assumptions). Using behavioral experiments, based on the PETS model[46] to challenge specific predictions in social situations |
| Reducing self-focused attention and safety behaviors | Understanding self-focused attention, in maintaining social anxiety. Specific assumptions regarding safety behaviors, self-focused attention are tested using video and audio exercises, tasks for shifting of attention to external cues such as objects, sounds (to reduce self-focused attention) |
| Graded exposure | In session (controlled exposures) and between-session exposure tasks to reduce avoidance, provide opportunities to experience and face anxiety, while dropping safety behaviors |
| Addressing anticipatory and postevent processing (rumination) | Using self-monitoring, postevent processing is identified and avoiding rumination is recommended |
| Relapse prevention | Continued exposure in real life situations. Making a blue print for plans after end of active treatment. Anticipating and dealing with high-risk situations are discussed |
CBT – Cognitive behavioral therapy; SAD – Social anxiety disorder; PETS – Prepare-Expose-Test-Summarize
Exposure
Exposure is an essential component of CBT. It involves graded exposure to socially feared situations without any escape or avoidance (including distraction and safety behaviors). Exposure can be in vivo or in imagination and would be largely dependent on the nature of the feared stimuli and opportunities for exposure. Although exposure is a critical element in the treatment of phobias, there are some challenges posed in the use of exposure in SAD. These include (a) being able to ensure graduated and repeatable tasks as social situations may be variable and somewhat unpredictable in outcomes; (b) prolonging exposure time as social situations may be naturally brief; (c) ensuring that adequate time is spent in exposure, due to cognitive processes such as self-focused attention; and (d) dealing with the cognitive aspects of social phobia, such as cognitive errors.[51] These difficulties are overcome using in-session exposures, behavioral experiments, and role-plays, which provide opportunities to ensure consistency across exposure tasks.
Cognitive restructuring
Cognitive restructuring is achieved through both verbal and behavioral methods. As part of the process of cognitive restructuring, individuals are taught to (1) identify negative thoughts that occur before, during, or after anxiety-provoking situations using self-monitoring; (2) evaluate the accuracy of their thoughts using information from Socratic questioning and/or through behavioral experiments that are aimed at testing predictions (e.g., “I will stammer so much that the shop-keeper will not understand me”); and (3) generate rational alternative thoughts based on the information acquired through and rate the conviction in these rational alternatives. Cognitive restructuring techniques and exposure are interlinked in that exposure tasks and behavioral experiments can be used to challenge dysfunctional beliefs. Modification of dysfunctional beliefs can also be attempted using other verbal methods, such as asking patient to drop excessive rules for one's social behavior, keeping a log of positive experiences that counter their predictions, recording evidence from the external situation that contradicts their biases, and facilitating perspective-taking.[47,48]
Applied relaxation
Excessive physiological arousal is common in SAD and may interfere with expression of social skills and enhance self-processing biases. Some patients also report panic attacks. The role of relaxation in social anxiety has been discussed with varying viewpoints, with some models excluding relaxation altogether.[47,48] Applied relaxation involves training the client through various stages of relaxation from progressive muscle relaxation to rapid relaxation, with the aim of producing the relaxation response in a short time, to be used in different social situations (applied) at the earliest experience of anxiety. It is a portable form of relaxation and involves elements of exposure in the final phase of application. It is meant to serve as a coping mechanism. The client should be aware of this and should not use relaxation as a safety behavior. Although it was initially used extensively in PD, later studies have demonstrated its role in SAD as well.
Social skills training
Majority of persons with SAD may have performance deficits due to anxiety, rather than actual skills deficits. The need to address social skills has been linked to social competence and functioning in persons with SAD. Assertiveness skills training addresses specific interpersonal skills such as making and refusing requests, expressing negative and positive feelings, negotiating, and bargaining. Social skills training (SST) involves a significant component of exposure to social situations as part of the training and contributes to the reduction in anxiety. The common techniques used for SST include modeling, role-play, behavioral rehearsal, reinforcement, feedback, and homework practice.
Choice of treatment settings
Most treatment-seeking persons with social anxiety are treated in outpatient settings since they are often employed or engaged in other activities despite their anxiety. In-patient setting may be considered only when patient has other comorbid conditions, such as severe depression.
Efficacy of cognitive behavioral therapy in social anxiety disorder
Among the various interventions, individual CBT appears to have the largest effect size for the treatment of SAD.[52] The most frequently examined components of CBT for SAD include exposure therapies, cognitive restructuring (with and without exposure), applied relaxation, and SST. Exposure alone or in combination with cognitive restructuring has demonstrated the greatest effect sizes among the various components of CBT, and other components when incorporated with exposure result in significant changes in symptoms. Studies examining SST and its efficacy in SAD indicate that little evidence for SST alone in SAD.[53] However, social skills, in combination with exposure, are reported to yield larger effect sizes than exposure alone.[54] The recommendations for psychological intervention components of CBT are shown in Table 14.
Table 14.
Recommendations for psychological interventions for social anxiety disorder
| Therapy | Grading of evidence |
|---|---|
| Exposure alone | A |
| Cognitive restructuring alone | A |
| Cognitive restructuring + exposure (CBT) | A |
| CBGT | A |
| CBT + pharmacotherapy (antidepressants) | A |
| Internet-based CBT (with minimal therapist guidance via email/SMS) | A |
| VRE | A |
| Applied relaxation with exposure | B |
| Mindfulness based interventions (acceptance and commitment and mindfulness based stress reduction***) | B |
| Interpersonal therapy for social anxiety*** | B |
| Social skills training alone | C |
| Applied relaxation alone | C |
| MCT | C |
| Brief CBT (<10 sessions) | C |
| Short-term psychodynamic psychotherapy*** | C |
| Supportive psychotherapy | C |
***Treatment components are similar to CBT (included modified exposure, cognitive restructuring, and distancing). CBGT – Cognitive behavioral group therapy; MCT – Metacognitive therapy; VRE – Virtual reality exposure; CBT – Cognitive behavioral therapy
Third-wave behavior therapies and other psychological approaches for social anxiety disorder
There is limited but emerging evidence for newer therapeutic approaches, within CBT such as ACT and mindfulness-based interventions, as well as for manualized psychodynamic psychotherapy and interpersonal therapy. Therapeutic components in each of these approaches have been modified for social anxiety. These also incorporate strategies similar to self-exposure, restructuring of beliefs regarding self and skills training. Hence, it may be difficult to ascertain exact mechanisms that result in improvement with these therapies.
Variants in delivery and format of cognitive behavioral therapy
Attempts to deliver CBT in varying formats have been reported. These include cognitive behavioral group therapy (CBGT), brief CBT and internet-delivered CBT (ICBT), and VRE therapy (VRET).
Rapee and Heimberg's cognitive behavioral group therapy (CBGT) model has been examined widely.[48] Reviews comparing individual CBT with group CBT report that both are equally effective in reducing levels of social anxiety. There is a paucity of evidence for the efficacy of brief CBT; however, preliminary evidence suggests that this may be a promising approach.[55]
Internet-delivered cognitive behavioral therapy
In a review of over 21 studies, of both guided and unguided ICBT for SAD, substantial reductions in social anxiety were noted, with larger within-group effect sizes and long-term gains from 3 months to 5 years.[56] However, ICBT may not be equally beneficial in all patients with SAD and careful screening of patients is important. It must be noted that control groups have been largely waitlist groups. A systematic review comparing ICBT with face-to-face therapy found that the two modes of CBT delivery were equally effective for SAD.[57]
Virtual reality for social anxiety disorder
Virtual reality is an emerging CBT component for SAD. It offers opportunities for exposure to interactions and other situations, under simulated conditions. Generalization from virtual reality to actual social situations may be a challenge when in vivo exposure and homework are not planned. Studies on virtual reality for social anxiety additionally indicate that VRET alone is not as effective as compared to individual in vivo exposure therapy or virtual reality that combines actual social interactions. A meta-analysis of technology-based interventions for SAD, including VRET, ICBT, and cognitive bias modification, indicated that both ICBT and VRET show promise in reducing symptoms of SAD and that ICBT had an advantage over active control conditions.[58]
Other therapeutic approaches and third-wave therapies
MCT[59] employs strategies such as detached mindfulness, attentional control training, and metacognitive Socratic dialog in addition to classic CBT. Evidence for its efficacy and superiority over traditional CBT is limited. It may be helpful in addressing metacognitions.[60]
When to stop treatment
Termination of active sessions in CBT is determined by the reduction in symptoms, rated on measures of anxiety, avoidance.[61] Active sessions may be terminated when the patient reports improvement on both self-report and clinician-assessed measures. It is recommended that at the start of the therapy, the therapist and patient collaboratively discuss the goals of therapy and expected realistic outcomes. Unlike in other anxiety disorders, complete extinction of anxiety is unlikely in SAD. This is particularly true when patients have generalized social anxiety and/or AAPD.
Guidance for maintenance and follow-up
Relapse prevention is an essential component of CBT for SAD. Due to the nature of SAD, continued practice of exposure is recommended. Maintenance of gains is determined by how prepared the patient is to deal with future situations of anxiety. Hence, during the phase of termination, the patient and therapist discuss and prepare a blueprint of what to expect after termination of active sessions and the importance of reduced avoidance. Booster sessions may be planned collaboratively to enhance consolidation and continued learning for specific skills. Studies on CBT suggest maintenance of gains in social anxiety up to a year following therapy.
OBSESSIVE–COMPULSIVE DISORDER
OCD is a disabling psychiatric disorder characterized by the presence of obsessions and compulsions. Obsessions are repetitive intrusive and often unwanted thoughts, images, or urges, which are associated with anxiety or distress. Patients with OCD perform repetitive and often ritualistic behaviors and/or mental acts to decrease the anxiety/distress associated with obsessions. The current classificatory systems recognize that insight of patients regarding the irrationality or excessiveness of their symptoms may vary from good to poor to delusional.
OCD has a lifetime prevalence of 1%–3%.[62] Untreated OCD often runs a chronic waxing and waning course. OCD is often comorbid with other conditions such as mood, anxiety, and personality disorders, as well as childhood-onset neuropsychiatric conditions such as tic disorders and attention-deficit hyperactivity disorder. Further, obsessive–compulsive spectrum conditions such as BDD and hoarding disorder are often underrecognized comorbidities. Serotonin reuptake inhibitors and/or CBT are the first-line treatments for OCD.[63]
Assessment
After establishing a diagnosis of OCD, a detailed evaluation of clinical profile is necessary before initiating therapy. It is essential to identify psychiatric comorbidities including mood, anxiety, and personality disorders, which might require separate attention and also help the therapist readjust the course of therapy accordingly. It would be helpful to assess various facets of illness, including severity, nature of obsessions/compulsions, extent of avoidance, and family accommodation. Assessment of underlying constructs such as obsessive beliefs, sensory phenomena, and disgust sensitivity may help readjust therapy in certain circumstances. Structured instruments for assessing OCD are summarized in Table 15. Behavioral analysis of symptoms [Table 16] aids in understanding the symptoms from a behavioral perspective and thus aids in planning therapy.
Table 15.
Instruments for assessing obsessive-compulsive disorder
| Instrument | Description |
|---|---|
| Y-BOCS[64] | The Y-BOCS symptom checklist assesses for current, past and principal symptoms of OCD-helps identify targets of therapy The Y-BOCS severity scale is considered the gold standard for assessing severity of OCD. It is helpful in monitoring of symptoms - has expert consensus defined cut-offs for diagnosis, severity, treatment response[65] |
| OCI-R[66] | 18-item self-report measure used for assessing severity across dimensions |
| MOCI[67] | 30-item self-report scale with dichotomous responses used for screening and severity |
| FOCI[68] | Self-report questionnaire- with 2 parts for screening and severity rating |
| Leyton obsessional inventory [69] | 69-item self-report questionnaire for assessing obsessional symptoms and traits |
| DY-BOCS[70] | Assesses for severity across various symptom dimensions |
| Dimensional Obsessive-Compulsive scale[71] | 20-item self-report scale to assess severity of symptoms along 4 dimensions |
| Scales to assess insight in OCD | |
| YBOCS, Item 11[64] | Single item - rates insight between 0-4 |
| BABS[72] | 7-item clinician-administered scale to assess the degree of conviction and insight into beliefs |
| OVIS[73] | 11-item clinician-administered scale to assess severity of overvalued ideation |
| Assessment of related constructs | |
| FAS[74] | 13-item clinician-administered scale to screen and monitor family accommodation |
| OBQ[75] | 44-item self-report to assess beliefs underlying development and maintenance of OCD |
| MCQ-30[76] | Self-report questionnaire which assesses beliefs about thinking |
| DPSS[77] | 16-item scale for assessing the tendency and emotional impact of disgust |
| University of São Paulo Sensory Phenomena Scale[78] | Self-report scale which includes checklist and assessment of severity for sensory phenomena in OCD subjects |
OCD – Obsessive-compulsive disorder; Y-BOCS – Yale-Brown Obsessive-Compulsive Scale; OCI-R – Obsessive-compulsive inventory-revised; MOCI – Maudsley Obsessive-compulsive inventory; FOCI – Florida Obsessive-Compulsive Inventory; DY-BOCS – Dimensional Yale-Brown Obsessive-Compulsive Scale; BABS – Brown Assessment of Beliefs Scale; OVIS – Overvalued ideas Scale; FAS – Family Accommodation Scale; OBQ – Obsessive-beliefs questionnaire; MCQ-30 – Metacognitions questionnaire – 30; DPSS – Disgust propensity and sensitivity scale
Table 16.
Behavioural analysis of obsessive-compulsive disorder
| 1. Specific antecedents that trigger anxiety/distress, which include both external (e.g., washrooms) and internal triggers (e.g., thoughts, images). It is important to elaborate on the specific and idiosyncratic nature of cues to plan exposure-based therapy. Build a hierarchy of the triggers based on subjective units of distress scale (0-100) |
| 2. Feared consequence of the triggers (e.g., contracting illness, something terrible happening to family members) - would aid in planning exposure tasks, preventing subtle avoidance and plan cognitive restructuring |
| 3. Elaborate understanding of rituals (compulsions) including overt compulsions, mental compulsions, and compulsions by proxy. The sequence and function of each ritual have to be elicited |
| 4. Avoidance/other safety behaviors (e.g., not using public toilets, avoiding work/cooking), which passively prevent habituation and maintain symptoms |
| 5. Family accommodation of symptoms (e.g., performing patient’s work such as arranging clothes, cooking, helping patient avoid triggers, compulsions by proxy), which has to be decreased gradually as part of exposure tasks |
| 6. Insight into obsessions and motivation for change has to be addressed before planning exposure-based strategies. |
| 7. Personality traits, which may maintain symptoms (e.g., distress tolerance, harm avoidance, perfectionism) |
| 8. Socio-cultural factors - cultural beliefs (e.g., about cleanliness), support system, expectation of patient and family members |
Formulating a treatment plan
Before starting CBT, it is important to discuss an individualized CBT model for OCD, therapeutic techniques involved, expected frequency/number/duration of sessions, need to tolerate anxiety as a part of treatment, need for homework compliance, and involvement of family members, if required.
Different CBT models have been proposed for OCD. The earlier two-stage behavioral model, based on learning theory, explains the acquisition of obsessive fears through classical conditioning, while avoidance/compulsions maintain the fears through operant conditioning. More recent cognitive models explain obsessions as normal cognitive intrusions, which are misinterpreted as threatening by patients with OCD due to certain underlying beliefs. These obsessive beliefs, such as exaggerated threat perception, inflated responsibility, need for perfection/certainty, thought-action fusion, and over-importance of thoughts and need to control thoughts, may be secondary to individualistic factors such as early life experiences, personality traits, and critical life incidents.
The cornerstone of OCD therapy has been exposure and response prevention (ERP), which involves graded exposure to the obsession triggers while preventing compulsive rituals and avoidance until the anxiety gradually wanes off. The principle behind ERP is the extinction of conditioned fear response through habituation and disconfirmation of underlying beliefs/assumptions. ERP also helps patients gain self-efficacy through mastery of fears without having to rely on avoidance or compulsions. Recent models emphasize on inhibitory learning paradigm.[79] Purely cognitive interventions without behavioral techniques are also sometimes employed. The CBT model for OCD is depicted in Figure 7. The components of CBT for OCD are summarized in Table 17. Steps involved in CBT are shown in Figure 8.
Figure 7.
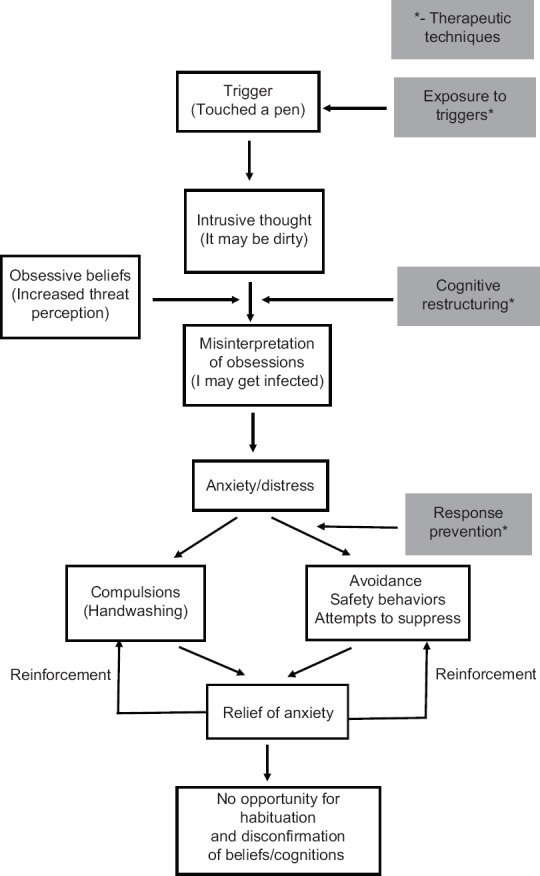
Cognitive behavioral therapy model for obsessive–compulsive disorder
Table 17.
Components for cognitive behavioral therapy for obsessivecompulsive disorder
| Step | Components |
|---|---|
| Psychoeducation | About OCD (symptoms, course, and treatment) |
| Principles of CBT for OCD | |
| Rationale behind ERP (concept of habituation and fear extinction and how compulsions, avoidance, and safety behaviors maintain obsessions and prevent fear extinction and disconfirmation of beliefs) | |
| Expected frequency/number/duration of sessions | |
| Need to tolerate anxiety as part of treatment | |
| Importance of between session exposures | |
| Involvement of family members | |
| Therapeutic formulation | Personalized formulation of therapy based on symptoms and individual cognitive distortions/beliefs |
| Collaborative understanding of formulation | |
| Exposure and Response prevention | Build a hierarchy of obsessional triggers based on subjective units of distress (0-100) |
| Graded exposure from the least to the most anxiety provoking stimulus and graded response prevention | |
| Practice exposure till reduction or cessation of anxiety/fear | |
| Homework ERP exercises | |
| Cognitive restructuring | Elicit faulty appraisals and cognitive distortions |
| Gather evidence for and against beliefs and explore alternative benign explanations | |
| Challenge the assumptions employing Socratic questioning and behavioral experiments | |
| Handling obsessive thoughts/ruminations | Being a “neutral spectator” by observing thoughts without interpreting, controlling and resisting thoughts |
| Relapse prevention | Explain need for continued exposure |
| Periodic booster sessions, as required | |
| Education regarding possibility of future relapse, early warning symptoms and signs of subtle avoidance |
CBT – Cognitive behavioral therapy; OCD – Obsessive-compulsive disorder; ERP – Exposure and response prevention
Figure 8.
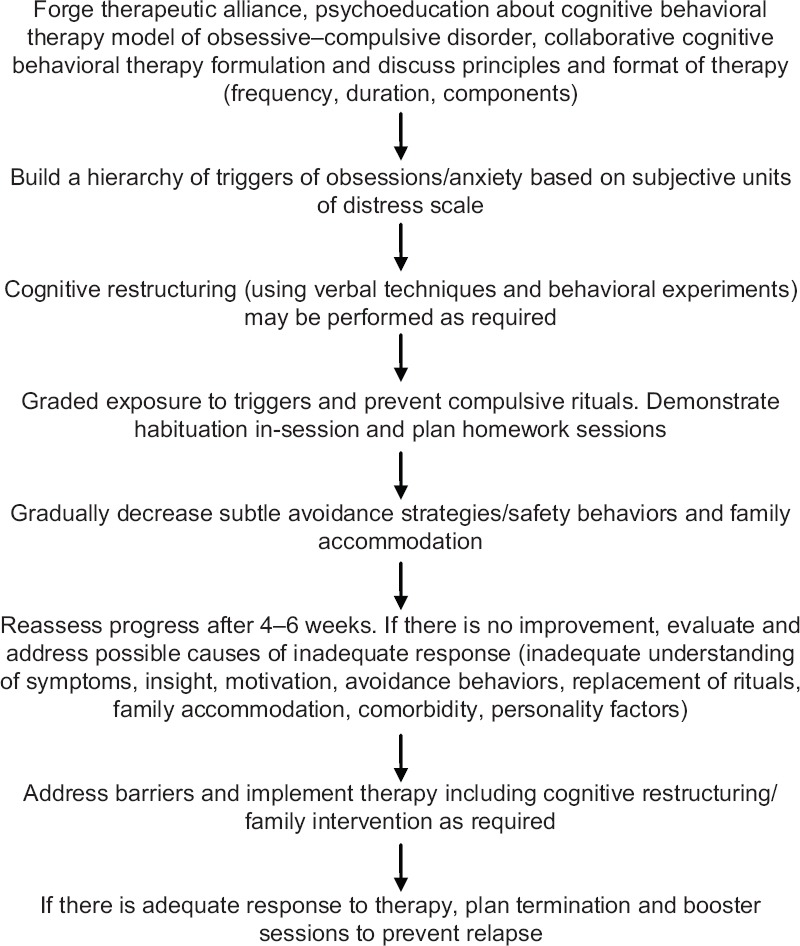
Steps involved in cognitive behavioral therapy for obsessive–compulsive disorder
Therapy should be planned based on a personalized formulation constructed around the symptoms and identified cognitive distortions/beliefs. A collaborative understanding of the formulation with the patient is essential before starting intervention.
Choice of treatment settings
CBT for OCD is generally provided on an outpatient basis as individual therapy. Typical CBT package is delivered over 2–3 months of 2–3 sessions a week for around 15–20 sessions.
Access to trained therapists and time constraints are major barriers in the Indian setting. Recent developments such as ICBT or computer-delivered CBT decrease direct therapist contact, and the therapy can be delivered in the home atmosphere. The principles of CBT are similar to that of office-based CBT, but the major part of the intervention is done by logging to a website and administering online self-help material. Periodic therapist contact (online or telephonic) may be necessary to improve outcomes and prevent dropouts in internet-based therapy.[80] Notwithstanding promising results from uncontrolled trials, there is limited evidence in the form of well-controlled trials. Moreover, this mode of intervention has not been evaluated in the Indian setting.
Intensive residential treatment (IRT) is a form of in-patient treatment for OCD, which is generally provided for severe and treatment-resistant patients, who do not respond to outpatient treatment. It is a multidimensional treatment that involves elements of medication management, intensive behavioral therapy, milieu support, and sometimes group therapy. The CBT sessions are more intensive with close supervision of ERP by a multidisciplinary team of trained therapists. Exposure tasks are facilitated by addressing therapeutic milieu and family accommodation.
Efficacy of cognitive behavioral therapy in obsessive–compulsive disorder
CBT involving ERP has been consistently shown to be efficacious in the treatment of OCD.[81] All treatment guidelines, including Indian guidelines, recommend CBT as a first-line treatment for OCD.[63] When therapists are available, CBT/ERP may be attempted as monotherapy in mild-to-moderately severe OCD. Severely ill patients may require a combination of CBT and an Selective Serotonin Reuptake Inhibitor (SSRI). CBT is the first-line augmenting strategy for partial/nonresponders to SSRIs.[82]
A recent meta-analysis did not find significant difference in efficacy between individual and group therapy.[83] However, group therapy unlike individual CBT has not been evaluated in large well-controlled studies.
With regard to IRT, uncontrolled studies from different centers have shown improvement in 50%–70% of predominantly treatment-resistant samples. A meta-analysis of 19 IRT studies involving 2306 participants found a mean reduction of 10.7 (9.8–11.5) points in Yale-Brown Obsessive–Compulsive Scale (Y-BOCS), with a large effect size of 1.87.[84] There is evidence to suggest that the improvement may persist up to 6 months postdischarge.[85,86] However, difficulty in obtaining suitable controls precludes gathering higher level of evidence for this intervention.
A recent innovation is the Bergen 4-day concentrated exposure treatment, which involves concentrated exposure-based therapy over a 4-day period for groups consisting of 3–6 patients, by the same number of therapists. The therapy is described as “individual treatment delivered in a group setting” and is found to be highly efficacious in uncontrolled studies.[87]
Family interventions targeting family accommodation and aimed at improving family functioning have been found to be helpful in reducing symptoms of OCD.[88] Thus, family involvement in therapy has to be encouraged, especially in those with high family accommodation.
Inference-based approach to therapy is more or less a cognitive model. It presumes that obsessive doubts arise from inferences about reality made based on an internal narrative, which is remote from empirically available sensory information. This leads to an incorrect interpretation of a distant possibility as reality, while compulsions result from acting as if the possibility is true. Therapy targets insight through reality reorientation by staying in touch with sensory information. Two controlled trials have shown efficacy comparable to CBT.[89] There is a need for larger trials, especially in those with poor insight.
Third-wave therapies such as ACT and mindfulness-based cognitive therapy are yet to be tested in controlled trials. Stress management, relaxation training, and psychodynamic therapies have scant evidence as standalone treatments for OCD. The role of pharmacological augmenters of CBT, such as d-cycloserine, is yet to be established.
The treatment recommendations for psychological interventions for OCD are summarized in Table 18.
Table 18.
Recommendations for cognitive behavioral therapy for obsessive-compulsive disorder
| Therapy | Strength of recommendation |
|---|---|
| CBT | A |
| Behavior therapy (exposure and response prevention) | A |
| CBT/BT formats | |
| Outpatient individual therapy | A |
| Outpatient group therapy | A |
| Intensive residential treatment | B |
| Internet-based CBT | B |
| Bergen’s 4-day concentrated CBT | B |
| Mindfulness-based CBT | C |
| Acceptance and commitment therapy | C |
| Stress management and relaxation training | C |
| Thought stopping | C |
| Dynamic psychotherapy | C |
CBT – Cognitive behavioral therapy
When to stop treatment
The decision for termination of therapy should be made based on the progress in relation to collaboratively arrived goals at the initiation of therapy. It is important to periodically monitor symptoms for the improvement and plateauing of response. While evidence suggests that full remission at the end of treatment predicts long-term outcomes,[90] it might be a utopian goal in many patients with OCD. Therapy may be terminated based on a realistic goal, when most of the planned targets are achieved, with plans for booster sessions as required. Preparation for termination of therapy should be done in advance, addressing issues such as need for continued exposure, homework tasks, stress management, relapse prevention, and optimizing functional outcomes.
Guidance for maintenance and follow-up
Although there is evidence to suggest that relapse rates are less following CBT as compared to medication discontinuation, posttherapy relapse occurs in at least 20% of patients. Factors such as lower initial severity of illness, remission at the end of treatment, absence of comorbidities, more intensive CBT, and better homework compliance predict long-term success.[91] A plan for relapse prevention plan is imperative before termination. Most CBT trials have included patients on medications. The long-term outcome of these patients without medications is not clear. Thus, medications may have to be continued over long term to prevent relapses, especially when CBT is provided as an augmentation treatment. Relapse prevention programs have been found helpful.[92] Relapse prevention programs include psychoeducation, self-exposure, stress/anxiety management, and lifestyle modification. Booster sessions with telephonic/direct contact may be planned with gradually tapering during follow-up.
BODY DYSMORPHIC DISORDER
BDD is a disabling psychiatric condition characterized by exaggerated and persistent preoccupation with perceived defects or flaws in one's appearance.[2]
BDD is currently listed under OCRDs Chapter of DSM-5[2] and the ICD-11.[3] Patients with BDD perform repetitive behaviors such as repeated mirror-gazing, exaggerated grooming behaviors, reassurance-seeking, or cognitive acts in response to appearance preoccupations. DSM-5 has an insight specifier, which helps clinicians to identify patients with BDD with poor insight, without having them assigned to a diagnosis of delusional disorder. DSM-5 also has a specifier for muscle dysmorphia. Major depressive disorder, SAD, and substance use disorders are common comorbid conditions in BDD. Suicide risk is high in BDD. The prevalence rates of BDD among both adult and adolescent populations is around 2%, and it is more common among females.[93]
Assessment
The BDD version of the YBOCS (BDD-YBOCS) is considered the gold standard measure of BDD symptom severity, and this instrument has been used as the principal outcome measure in various clinical trials.[94] The BDD-YBOCS is a 12-item semi-structured, clinician-administered scale, which records BDD symptom severity over the past week. It is sensitive to changes with treatment and has good psychometric properties. The BDD Questionnaire is a brief self-report screening instrument with good psychometric properties.[95]
Formulating a treatment plan
The literature extends the best support for the use of CBT as the primary treatment for BDD.[96] The other evidence-based treatment includes pharmacotherapy with serotonin reuptake inhibitors, as in OCD.[96]
Biological, psychological, and sociocultural factors in the development and persistence of BDD symptoms have been considered and incorporated into the CBT models of BDD.[97,98] These models explain that persons with BDD exhibit selective attention over minor features of appearance, instead of paying attention to a larger picture. They also over-estimate the importance of perceived physical deformities/deficits (ascribing greater value to these flaws). Patients may also misinterpret small flaws as major personal concerns. It is theorized that self-defeating explanations result in the development of negative feelings, which in turn are neutralized with rituals such as repeated mirror-gazing and seeking cosmetic surgery. Further, they avoid social situations to minimize perceived negative evaluation. These behaviors are thought to be negatively reinforced since they result in temporary reduction of anxiety culminating in maladaptive beliefs and poor coping methods. The CBT model for BDD is depicted in Figure 9.
Figure 9.
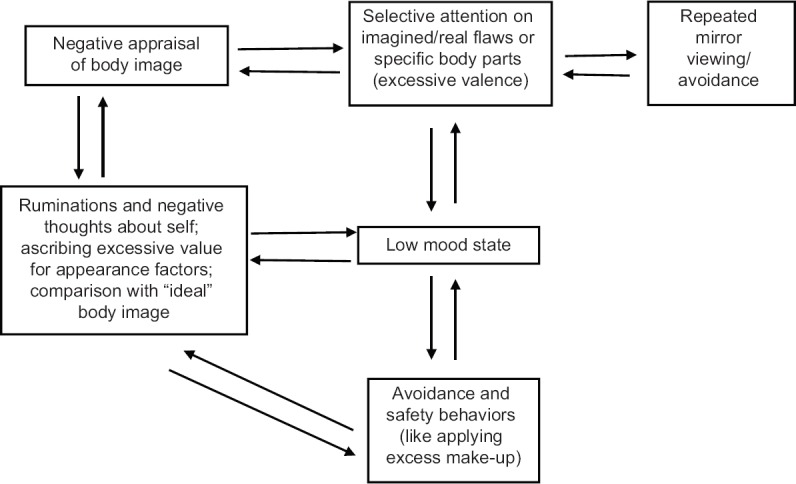
Cognitive behavioral therapy model for body dysmorphic disorder
CBT for BDD starts with detailed assessment of symptoms. This is followed by psychoeducation where explanations for the symptoms are provided with individualized presentation of the CBT model. The subsequent components include cognitive restructuring, exposure, and ritual and relapse prevention. Certain CBT models also include a component of perceptual retraining to address mirror-related behaviors. The components of CBT for BDD are elaborated in Table 19.
Table 19.
Components of cognitive behavioral therapy for body dysmorphic disorder
| CBT step | Component |
|---|---|
| Assessment | Assess the points of concern, thoughts, behaviors, and associated impairment |
| Degree of extension into various spheres of life, avoidance behaviors, and the degree of rituals involved | |
| Assessment of insight into symptoms | |
| Examine for comorbidities - depression, social anxiety, suicidal ideations | |
| Patients’ plans for cosmetic remediations such as surgery | |
| Prior medication and CBT history, if any | |
| Motivational assessment | Assessment of motivation levels incorporate techniques from motivational interviewing, particularly for those with poor insight |
| Psychoeducation | Provide psychoeducation of the illness - prevalence, presenting symptoms |
| Discuss the difference between body image and appearance | |
| Personalized model of BDD in tune with the patient’s specific set of symptoms | |
| Cognitive methods | Cognitive strategies -identifying and examining maladaptive/dysfunctional thoughts together with generating alternative adaptive thoughts |
| Identify particular cognitive errors seen with the condition such as “all or none thinking,” and mind-reading | |
| Addressing the core-beliefs such as “I am an inadequate person” and “I am not fit enough to be loved” | |
| Maladaptive core beliefs need to be addressed through cognitive restructuring, behavioral experiments | |
| Learning to widen the components of self-worth by including appearance-unrelated factors such as other positive factors in their personality and skills | |
| Exposure and ritual prevention (Behavioral experiments) | Develop a hierarchy of anxiety-provoking/avoided- situations |
| Monitor the frequency and situations in which rituals occur | |
| Strategies to eliminate rituals or reduce rituals - e.g., resisting urges to check mirror, using less make-up before going out | |
| Exposure exercises like behavioral experiments to examine the validity of negative predictions and thus disconfirming the previous fears over time | |
| Perceptual training | Aims to address distorted body-image perception. It helps patients learn to engage in more adaptive mirror-related behaviors such as not specifically focusing on one particular area, using objective description in place of evaluative language in front of mirror and not entirely avoiding the mirror |
| Relapse prevention | Consolidation of skills and exploring clear future plans |
| Booster sessions may be offered, as required |
CBT – Cognitive behavioral therapy; BDD – Body dysmorphic disorder
Efficacy of cognitive behavioral therapy in body dysmorphic disorder
RCTs in adult participants have demonstrated efficacy of CBT in reducing BDD symptom severity as compared to waitlist controls as well as other nonspecific interventions, such as anxiety management and supportive psychotherapy.[99,100,101] A naturalistic 1–4-year follow-up of participants in an RCT found that the gains made at the end of CBT sessions were sustained in the long term.[102] More recently, internet-based therapist-assisted CBT has also be systematically tested and found to be useful in this condition.[103] There have been no consistent response predictors of response to CBT, but greater motivation, greater expectation from treatment, as well as better insight at the baseline may predict improvement with CBT.[104] Overall, based on the available evidence, CBT has strength of recommendation level A for BDD.
BODY-FOCUSED REPETITIVE BEHAVIORS: TRICHOTILLOMANIA AND SKIN-PICKING DISORDER
Trichotillomania (hair-pulling disorder) is a disorder of repetitive pulling out of one's own hair, while skin-picking disorder is characterized by recurrent picking of one's own skin. These conditions are often subsumed under a common rubric “BFRBs.” DSM-5[2] and ICD-11[3] have included trichotillomania and excoriation (skin-picking) disorder within the OCRDs. Trichotillomania has a prevalence of 1%–3% across studies conducted in different populations.[105] Its prevalence is four times greater among women compared to men. There are no well-conducted prevalence studies for excoriation disorder. However, the limited existing studies report a prevalence estimate of 1%–4% for distressing excoriation conditions.[106] Anxiety disorders and depression are frequent comorbidities.
Scalp is the most common location for hair-pulling in trichotillomania followed by the eyebrows. Hair-pulling may be preceded by various triggers, including sensory (e.g., sensations on the scalp), mood-related (anxiety, boredom, anger), and cognitive (rigidity in thinking/cognitive errors) stimuli. However, some patients report that they are not “aware” of hair-pulling, and this is referred to as “automatic” hair-pulling. About 5%–20% of individuals with trichotillomania engage in trichophagia (ingestion of hair). This may rarely lead to a gastric medical complication called trichobezoar. In excoriation disorder, the sufferers experience repeated and compulsive urges to remove certain alterations in the areas with acne, scars, and scabs.[107] The regions of excoriation may vary. Generally, multiple areas of the body that are easily accessible (face, extensor surface of the arms, and fingers) are targets.
Assessment
A summary of instruments available for the assessment of hair-pulling and skin-picking have been provided by Jones et al.[108] Massachusetts General Hospital Hair Pulling Scale (MGH-HPS) is generally recommended for measuring the severity of hair-pulling disorder.[109] The MGH-HPS is a 7-item self-report scale that measures urge to pull hair, amount of pulling, control over the behavior, and the associated distress over the previous 7 days. The Keuthen Diagnostic Inventory for Skin Picking for DSM-5 has been recommended as a quick tool to measure the severity of skin-picking.[108] Since anxiety disorders, depression, and OCD are commonly seen comorbid with trichotillomania and excoriation disorder, it is important to systematically assess for the presence of these conditions. Functional analysis of the pulling behavior helps to identify antecedent triggers (may be external and/or internal) and consequences (positive or negative reinforcement) following hair-pulling behavior.
Cognitive behavioral therapy for body-focused repetitive behaviors
Although the evidence is relatively limited compared to the other disorders discussed above, CBT is often recommended as a first-line treatment for both trichotillomania and skin-picking disorder. Behavioral techniques are more commonly employed. In particular, habit reversal therapy (HRT) is the most commonly prescribed technique. The components of HRT are elaborated in Table 20.
Table 20.
| Therapy step | Components |
|---|---|
| Psychoeducation | Education about the disorder with explanation related to triggers and mood state associated with hair-pulling |
| Awareness training | Helping to develop awareness of situations that triggers/precedes hair-pulling episodes |
| Stimulus control | Patient is asked to prevent hair-pulling through reduction of the impact of conditioned-cues in the surroundings (e.g., restricting access to hair-pulling instruments) |
| Competing response practice | Encourage practicing motor-response which is incompatible with hair-pulling (e.g., clenching of fists) |
Efficacy of cognitive behavioral therapy in body-focused repetitive behaviors
Multiple RCTs support the efficacy of HRT for trichotillomania, while there are few studies on skin-picking disorder too.[110] HRT has been administered in different frequency formats, ranging from 4 to 20 sessions. Dialectical behavioral augmented CBT[112] and ACT[113] have been tested in single RCTs each. Dialectical approaches may help in augmenting HRT. The components of this approach include mindfulness training where patients are encouraged to experiences the urges/emotions associated as they occur at the moment, inculcating necessary skills for emotion regulation and build distress tolerance. ACT may also be used similarly as a component in the context of HRT, whereby the patient is explained to experience hair-pulling urges and accept those urges without having to act on them.
Similar strategies are suggested for excoriation disorder also.[114] Skin-picking disorder, being a recently recognized diagnostic entity, has been less studied less extensively. HRT has been found to be useful for skin-picking disorder in a limited number of RCTs, while ACT has been tested only in uncontrolled studies. The recommendations for OCRD are summarized in Table 21.
Table 21.
Recommendation for obsessive-compulsive-related disorders
| Therapy | Strength of recommendation |
|---|---|
| Body dysmorphic disorder | |
| Cognitive behavioral therapy | A |
| Trichotillomania | |
| Habit reversal therapy | A |
| Dialectical behavioral therapy | B |
| Acceptance and commitment therapy | B |
| Skin-picking disorder | |
| Habit reversal therapy | B |
| Acceptance and commitment therapy | C |
SUMMARY
CBT is a first-line treatment for most anxiety disorders and obsessive–compulsive-related disorders. It has also been found to be helpful in those with inadequate response to medications. Despite similarity of certain techniques such as exposure and cognitive restructuring, individual disorders have different CBT models, which have been tested and proven to be effective. For some disorders, such as specific phobia and BFRB, primarily behavioral techniques have been found to be helpful. While graded exposure is helpful in the former, habit reversal is recommended for the later. Individual face-to-face therapy has been the most rigorously tested, but group therapy also has been found effective in many conditions. Self-help therapy, such as internet-based therapy, may be helpful, especially when used with intermittent therapist guidance. Exposure using virtual reality, augmentation with mindfulness, and emotional regulation strategies are exciting and emerging strategies for augmenting the effects of CBT.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015;17:327–35. doi: 10.31887/DCNS.2015.17.3/bbandelow. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Publishing. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, D.C: American Psychiatric Publishing; 2013. [Google Scholar]
- 3.Stein DJ, Kogan CS, Atmaca M, Fineberg NA, Fontenelle LF, Grant JE, et al. The classification of obsessive-compulsive and related disorders in the ICD-11. J Affect Disord. 2016;190:663–74. doi: 10.1016/j.jad.2015.10.061. [DOI] [PubMed] [Google Scholar]
- 4.Ebell MH, Siwek J, Weiss BD, Woolf SH, Susman J, Ewigman B, et al. Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature. J Am Board Fam Pract. 2004;17:59–67. doi: 10.3122/jabfm.17.1.59. [DOI] [PubMed] [Google Scholar]
- 5.Clark DA, Beck AT. New York: The Guilford Press; 2011. Cognitive Therapy of Anxiety Disorders: Science and Practice. Updated edition. [Google Scholar]
- 6.Craske M, Wittchen U, Bogels S, Stein M, Andrews G, Lebeu R, et al. Severity Measure for Panic Disorder – Adult. American Psychiatric Association. 2013. [Last accessed on 2019 Aug 29]. Available from: http://tpcjournal.nbcc.org/wp-content/uploads/2014/07/Pages-216-231-Schmit.pdf .
- 7.Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, et al. Multicenter collaborative panic disorder severity scale. Am J Psychiatry. 1997;154:1571–5. doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- 8.Bandelow B, Broocks A, Pekrun G, George A, Meyer T, Pralle L, et al. The use of the Panic and agoraphobia scale (P and A) in a controlled clinical trial. Pharmacopsychiatry. 2000;33:174–81. doi: 10.1055/s-2000-12982. [DOI] [PubMed] [Google Scholar]
- 9.Shear MK, Maser JD. Standardized assessment for panic disorder research. A conference report. Arch Gen Psychiatry. 1994;51:346–54. doi: 10.1001/archpsyc.1994.03950050006001. [DOI] [PubMed] [Google Scholar]
- 10.Chambless DL, Caputo GC, Bright P, Gallagher R. Assessment of fear of fear in agoraphobics: The body sensations questionnaire and the agoraphobic cognitions questionnaire. J Consult Clin Psychol. 1984;52:1090–7. doi: 10.1037//0022-006x.52.6.1090. [DOI] [PubMed] [Google Scholar]
- 11.Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav Res Ther. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- 12.Chambless DL, Caputo GC, Jasin SE, Gracely EJ, Williams C. The mobility inventory for agoraphobia. Behav Res Ther. 1985;23:35–44. doi: 10.1016/0005-7967(85)90140-8. [DOI] [PubMed] [Google Scholar]
- 13.Telch MJ, Brouillard M, Telch CF, Agras WS, Taylor CB. Role of cognitive appraisal in panic-related avoidance. Behav Res Ther. 1989;27:373–83. doi: 10.1016/0005-7967(89)90007-7. [DOI] [PubMed] [Google Scholar]
- 14.Clark DM. A cognitive approach to panic. Behav Res Ther. 1986;24:461–70. doi: 10.1016/0005-7967(86)90011-2. [DOI] [PubMed] [Google Scholar]
- 15.Clark DA, Salkovskis PM. Oxford, UK: Department of Psychiatry, University of Oxford; 1986. Cognitive Treatment of Panic: Therapist's Manual. [Google Scholar]
- 16.Barlow DH, Craske MG. Mastery of Your Anxiety and Panic (MAP-3): Client Workbook for Agoraphobia. 3rd ed. S.L: Academic Press; 2000. [Google Scholar]
- 17.Katzman MA, Bleau P, Blier P, Chokka P, Kjernisted K, Van Ameringen M, et al. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatry. 2014;14(Suppl 1):S1. doi: 10.1186/1471-244X-14-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Overview | Generalised Anxiety Disorder and Panic Disorder in Adults: Management | Guidance | NICE. [Last accessed on 2019 Jun 27]. Available from: https://www.nice.org.uk/guidance/cg113 . [PubMed]
- 19.Pompoli A, Furukawa TA, Efthimiou O, Imai H, Tajika A, Salanti G. Dismantling cognitive-behaviour therapy for panic disorder: A systematic review and component network meta-analysis. Psychol Med. 2018;48:1945–53. doi: 10.1017/S0033291717003919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Imai H, Tajika A, Chen P, Pompoli A, Furukawa TA. Psychological therapies versus pharmacological interventions for panic disorder with or without agoraphobia in adults. Cochrane Database Syst Rev. 2016;10:CD011170. doi: 10.1002/14651858.CD011170.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fava GA, Rafanelli C, Grandi S, Conti S, Ruini C, Mangelli L, et al. Long-term outcome of panic disorder with agoraphobia treated by exposure. Psychol Med. 2001;31:891–8. doi: 10.1017/s0033291701003592. [DOI] [PubMed] [Google Scholar]
- 22.Clark DM, Salkovskis PM, Hackmann A, Wells A, Ludgate J, Gelder M. Brief cognitive therapy for panic disorder: A randomized controlled trial. J Consult Clin Psychol. 1999;67:583–9. doi: 10.1037//0022-006x.67.4.583. [DOI] [PubMed] [Google Scholar]
- 23.White KS, Payne LA, Gorman JM, Shear MK, Woods SW, Saksa JR, et al. Does maintenance CBT contribute to long-term treatment response of panic disorder with or without agoraphobia? A randomized controlled clinical trial. J Consult Clin Psychol. 2013;81:47–57. doi: 10.1037/a0030666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berle D, Starcevic V, Moses K, Hannan A, Milicevic D, Sammut P. Preliminary validation of an ultra-brief version of the Penn state worry questionnaire. Clin Psychol Psychother. 2011;18:339–46. doi: 10.1002/cpp.724. [DOI] [PubMed] [Google Scholar]
- 25.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166:1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 26.Shear K, Belnap BH, Mazumdar S, Houck P, Rollman BL. Generalized anxiety disorder severity scale (GADSS): A preliminary validation study. Depress Anxiety. 2006;23:77–82. doi: 10.1002/da.20149. [DOI] [PubMed] [Google Scholar]
- 27.Behar E, DiMarco ID, Hekler EB, Mohlman J, Staples AM. Current theoretical models of generalized anxiety disorder (GAD): Conceptual review and treatment implications. J Anxiety Disord. 2009;23:1011–23. doi: 10.1016/j.janxdis.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 28.Dugas MJ, Robichaud M. Cognitive-Behavioral Treatment for Generalized Anxiety Disorder: From Science to Practice. Google Books. [Last accessed on 2019 Sep 11]. Available from: https://books.google.co.in/books/about/Cognitive_behavioral_Treatment_for_Gener.html?id=bLGqfBtyMcoC and redir_esc=y .
- 29.Treatment of Generalized Anxiety Disorder: Gavin Andrews: 9780198758846. [Last accessed on 2019 Aug 29]. Available from: https://www.bookdepository.com/Treatment-generalized-anxiety-disorder-Gavin-Andrews/9780198758846 .
- 30.Kim YW, Lee SH, Choi TK, Suh SY, Kim B, Kim CM, et al. Effectiveness of mindfulness-based cognitive therapy as an adjuvant to pharmacotherapy in patients with panic disorder or generalized anxiety disorder. Depress Anxiety. 2009;26:601–6. doi: 10.1002/da.20552. [DOI] [PubMed] [Google Scholar]
- 31.Cuijpers P, Sijbrandij M, Koole S, Huibers M, Berking M, Andersson G. Psychological treatment of generalized anxiety disorder: A meta-analysis. Clin Psychol Rev. 2014;34:130–40. doi: 10.1016/j.cpr.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 32.Hunot V, Churchill R, Silva de Lima M, Teixeira V. Psychological therapies for generalised anxiety disorder. Cochrane Database Syst Rev. 2007;(1):CD001848. doi: 10.1002/14651858.CD001848.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khoury B, Lecomte T, Fortin G, Masse M, Therien P, Bouchard V, et al. Mindfulness-based therapy: A comprehensive meta-analysis. Clin Psychol Rev. 2013;33:763–71. doi: 10.1016/j.cpr.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 34.Andrews G, Basu A, Cuijpers P, Craske MG, McEvoy P, English CL, et al. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: An updated meta-analysis. J Anxiety Disord. 2018;55:70–8. doi: 10.1016/j.janxdis.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 35.Norton PJ, Roberge P. Transdiagnostic therapy. Psychiatr Clin North Am. 2017;40:675–87. doi: 10.1016/j.psc.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 36.Marks IM, Mathews AM. Brief standard self-rating for phobic patients. Behav Res Ther. 1979;17:263–7. doi: 10.1016/0005-7967(79)90041-x. [DOI] [PubMed] [Google Scholar]
- 37.Opriş D, Pintea S, García-Palacios A, Botella C, Szamosközi Ş, David D. Virtual reality exposure therapy in anxiety disorders: A quantitative meta-analysis. Depress Anxiety. 2012;29:85–93. doi: 10.1002/da.20910. [DOI] [PubMed] [Google Scholar]
- 38.Craske MG, Rowe MK. Chichester, England: Wiley; 1997. A comparison of behavioral and cognitive treatments for phobias. In G. C. L. Davey (Ed.), Phobias: A handbook of theory, research, and treatment; pp. 247–80. [Google Scholar]
- 39.Ost LG, Fellenius J, Sterner U. Applied tension, exposure in vivo, and tension-only in the treatment of blood phobia. Behav Res Ther. 1991;29:561–74. doi: 10.1016/0005-7967(91)90006-o. [DOI] [PubMed] [Google Scholar]
- 40.Wolitzky-Taylor KB, Horowitz JD, Powers MB, Telch MJ. Psychological approaches in the treatment of specific phobias: A meta-analysis. Clin Psychol Rev. 2008;28:1021–37. doi: 10.1016/j.cpr.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 41.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liebowitz MR. Social Phobia. Anxiety. 1987;22:141–73. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- 43.Leary MR. A brief version of the fear of negative evaluation scale. Pers Soc Psychol Bull. 1983;9:371–5. [Google Scholar]
- 44.Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behav Res Ther. 1998;36:455–70. doi: 10.1016/s0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- 45.Connor KM, Davidson JR, Churchill LE, Sherwood A, Foa E, Weisler RH. Psychometric properties of the Social Phobia Inventory (SPIN). New self-rating scale. Br J Psychiatry. 2000;176:379–86. doi: 10.1192/bjp.176.4.379. [DOI] [PubMed] [Google Scholar]
- 46.Wells A. 1st ed. Chichester : New York: Wiley; 1997. Cognitive Therapy of Anxiety Disorders: A Practice Manual and Conceptual Guide. [Google Scholar]
- 47.Clark DM, Wells A. Social Phobia: Diagnosis, Assessment, and Treatment. New York, NY, US: The Guilford Press; 1995. A cognitive model of social phobia; pp. 69–93. [Google Scholar]
- 48.Rapee RM, Heimberg RG. A cognitive-behavioral model of anxiety in social phobia. Behav Res Ther. 1997;35:741–56. doi: 10.1016/s0005-7967(97)00022-3. [DOI] [PubMed] [Google Scholar]
- 49.Wells A. Metacognitive Therapy for Anxiety and Depression. New york: Guilford Press; 2011. [Google Scholar]
- 50.Butler G. A Self-Help Guide Using Cognitive Behavioral Techniques. 1st ed. London: Robinson; 2009. Overcoming Social Anxiety and Shyness. [Google Scholar]
- 51.Butler G, Cullington A, Munby M, Amies P, Gelder M. Exposure and anxiety management in the treatment of social phobia. J Consult Clin Psychol. 1984;52:642–50. doi: 10.1037//0022-006x.52.4.642. [DOI] [PubMed] [Google Scholar]
- 52.Mayo-Wilson E, Dias S, Mavranezouli I, Kew K, Clark DM, Ades AE, et al. Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. Lancet Psychiatry. 2014;1:368–76. doi: 10.1016/S2215-0366(14)70329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ponniah K, Hollon SD. Empirically supported psychological interventions for social phobia in adults: A qualitative review of randomized controlled trials. Psychol Med. 2008;38:3–14. doi: 10.1017/S0033291707000918. [DOI] [PubMed] [Google Scholar]
- 54.Beidel DC, Alfano CA, Kofler MJ, Rao PA, Scharfstein L, Wong Sarver N. The impact of social skills training for social anxiety disorder: A randomized controlled trial. J Anxiety Disord. 2014;28:908–18. doi: 10.1016/j.janxdis.2014.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pinjarkar GR, Sudhir PM, Mariamma P, Math BS, Wells A. Brief cognitive therapy plus treatment as usual for social anxiety disorder: A randomized trial of adults in India. J Cogn Ther. 2018;11:299–310. [Google Scholar]
- 56.Boettcher J, Carlbring P, Renneberg B, Berger T. Internet-based interventions for social anxiety disorder – An overview. VER. 2013;23:160–8. [Google Scholar]
- 57.Carlbring P, Andersson G, Cuijpers P, Riper H, Hedman-Lagerlöf E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: An updated systematic review and meta-analysis. Cogn Behav Ther. 2018;47:1–8. doi: 10.1080/16506073.2017.1401115. [DOI] [PubMed] [Google Scholar]
- 58.Kampmann IL, Emmelkamp PM, Morina N. Meta-analysis of technology-assisted interventions for social anxiety disorder. J Anxiety Disord. 2016;42:71–84. doi: 10.1016/j.janxdis.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 59.Wells A, Matthews G. London: Psychology Press; 1994. Attention and Emotion: A Clinical Perspective. [Google Scholar]
- 60.Lakshmi J, Sudhir PM, Sharma MP, Math SB. Effectiveness of metacognitive therapy in patients with social anxiety disorder: A pilot investigation. Indian J Psychol Med. 2016;38:466–71. doi: 10.4103/0253-7176.191385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jakobsons LJ, Brown JS, Gordon KH, Joiner TE. When are clients ready to terminate? Cogn Behav Pract. 2007;14:218–30. [Google Scholar]
- 62.Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15:53–63. doi: 10.1038/mp.2008.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Janardhan Reddy YC, Sundar AS, Narayanaswamy JC, Math SB. Clinical practice guidelines for obsessive-compulsive disorder. Indian J Psychiatry. 2017;59:S74–S90. doi: 10.4103/0019-5545.196976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown obsessive compulsive scale. I. development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–11. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 65.Mataix-Cols D, Fernández de la Cruz L, Nordsletten AE, Lenhard F, Isomura K, Simpson HB. Towards an international expert consensus for defining treatment response, remission, recovery and relapse in obsessive-compulsive disorder. World Psychiatry. 2016;15:80–1. doi: 10.1002/wps.20299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, et al. The Obsessive-compulsive inventory: Development and validation of a short version. Psychol Assess. 2002;14:485–96. [PubMed] [Google Scholar]
- 67.Hodgson RJ, Rachman S. Obsessional-compulsive complaints. Behav Res Ther. 1977;15:389–95. doi: 10.1016/0005-7967(77)90042-0. [DOI] [PubMed] [Google Scholar]
- 68.Storch EA, Kaufman DA, Bagner D, Merlo LJ, Shapira NA, Geffken GR, et al. Florida obsessive-compulsive inventory: Development, reliability, and validity. J Clin Psychol. 2007;63:851–9. doi: 10.1002/jclp.20382. [DOI] [PubMed] [Google Scholar]
- 69.Cooper J. The Leyton obsessional inventory. Psychol Med. 1970;1:48–64. doi: 10.1017/s0033291700040010. [DOI] [PubMed] [Google Scholar]
- 70.Rosario-Campos MC, Miguel EC, Quatrano S, Chacon P, Ferrao Y, Findley D, et al. The dimensional Yale-Brown obsessive-compulsive scale (DY-BOCS): An instrument for assessing obsessive-compulsive symptom dimensions. Mol Psychiatry. 2006;11:495–504. doi: 10.1038/sj.mp.4001798. [DOI] [PubMed] [Google Scholar]
- 71.Abramowitz JS, Deacon BJ, Olatunji BO, Wheaton MG, Berman NC, Losardo D, et al. Assessment of obsessive-compulsive symptom dimensions: Development and evaluation of the dimensional obsessive-compulsive scale. Psychol Assess. 2010;22:180–98. doi: 10.1037/a0018260. [DOI] [PubMed] [Google Scholar]
- 72.Eisen JL, Phillips KA, Baer L, Beer DA, Atala KD, Rasmussen SA. The Brown assessment of beliefs scale: Reliability and validity. Am J Psychiatry. 1998;155:102–8. doi: 10.1176/ajp.155.1.102. [DOI] [PubMed] [Google Scholar]
- 73.Neziroglu F, McKay D, Yaryura-Tobias JA, Stevens KP, Todaro J. The overvalued ideas scale: Development, reliability and validity in obsessive-compulsive disorder. Behav Res Ther. 1999;37:881–902. doi: 10.1016/s0005-7967(98)00191-0. [DOI] [PubMed] [Google Scholar]
- 74.Calvocoressi L, Mazure CM, Kasl SV, Skolnick J, Fisk D, Vegso SJ, et al. Family accommodation of obsessive-compulsive symptoms: Instrument development and assessment of family behavior. J Nerv Ment Dis. 1999;187:636–42. doi: 10.1097/00005053-199910000-00008. [DOI] [PubMed] [Google Scholar]
- 75.Obsessive Compulsive Cognitions Working Group. Psychometric validation of the obsessive beliefs questionnaire and the interpretation of intrusions inventory: Part I. Behav Res Ther. 2003;41:863–78. doi: 10.1016/s0005-7967(02)00099-2. [DOI] [PubMed] [Google Scholar]
- 76.Wells A, Cartwright-Hatton S. A short form of the metacognitions questionnaire: Properties of the MCQ-30. Behav Res Ther. 2004;42:385–96. doi: 10.1016/S0005-7967(03)00147-5. [DOI] [PubMed] [Google Scholar]
- 77.Overveld VW, Jong DP, Peters ML, Cavanagh K, Davey GC. Disgust propensity and disgust sensitivity: Separate constructs that are differentially related to specific fears. Pers Individ Diff. 2006;41:1241–52. [Google Scholar]
- 78.Rosario MC, Prado HS, Borcato S, Diniz JB, Shavitt RG, Hounie AG, et al. Validation of the University of São Paulo sensory phenomena scale: Initial psychometric properties. CNS Spectr. 2009;14:315–23. doi: 10.1017/s1092852900020319. [DOI] [PubMed] [Google Scholar]
- 79.Abramowitz JS, Blakey SM, Reuman L, Buchholz JL. New directions in the cognitive-behavioral treatment of OCD: Theory, research, and practice. Behav Ther. 2018;49:311–22. doi: 10.1016/j.beth.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 80.Andersson E, Ljótsson B, Hedman E, Kaldo V, Paxling B, Andersson G, et al. Internet-based cognitive behavior therapy for obsessive compulsive disorder: A pilot study. BMC Psychiatry. 2011;11:125. doi: 10.1186/1471-244X-11-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Skapinakis P, Caldwell DM, Hollingworth W, Bryden P, Fineberg NA, Salkovskis P, et al. Pharmacological and psychotherapeutic interventions for management of obsessive-compulsive disorder in adults: A systematic review and network meta-analysis. Lancet Psychiatry. 2016;3:730–9. doi: 10.1016/S2215-0366(16)30069-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hezel DM, Simpson HB. Exposure and response prevention for obsessive-compulsive disorder: A review and new directions. Indian J Psychiatry. 2019;61:S85–92. doi: 10.4103/psychiatry.IndianJPsychiatry_516_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pozza A, Dèttore D. Drop-out and efficacy of group versus individual cognitive behavioural therapy: What works best for obsessive-compulsive disorder? A systematic review and meta-analysis of direct comparisons. Psychiatry Res. 2017;258:24–36. doi: 10.1016/j.psychres.2017.09.056. [DOI] [PubMed] [Google Scholar]
- 84.Veale D, Naismith I, Miles S, Gledhill LJ, Stewart G, Hodsoll J. Outcomes for residential or inpatient intensive treatment of obsessive-compulsive disorder: A systematic review and meta-analysis. J Obsessive Compuls Relat Disord. 2016;8:38–49. [Google Scholar]
- 85.Stewart SE, Stack DE, Tsilker S, Alosso J, Stephansky M, Hezel DM, et al. Long-term outcome following Intensive Residential Treatment of Obsessive-Compulsive Disorder. J Psychiatr Res. 2009;43:1118–23. doi: 10.1016/j.jpsychires.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 86.Balachander S, Bajaj A, Hazari N, Narayanaswamy JC, Kumar A, Anand N, et al. Outcome of Intensive Inpatient Care for Severe, Resistant Obsessive-Compulsive Disorder in Young Adults: Experience of a Specialty OCD Clinic in South India. Vancouver, British Columbia. 2019 [Google Scholar]
- 87.Hansen B, Hagen K, Öst LG, Solem S, Kvale G. The Bergen 4-day OCD treatment delivered in a group setting: 12-month follow-up. Front Psychol. 2018;9:639. doi: 10.3389/fpsyg.2018.00639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Baruah U, Pandian RD, Narayanaswamy JC, Bada Math S, Kandavel T, Reddy YC. A randomized controlled study of brief family-based intervention in obsessive compulsive disorder. J Affect Disord. 2018;225:137–46. doi: 10.1016/j.jad.2017.08.014. [DOI] [PubMed] [Google Scholar]
- 89.Julien D, O’Connor K, Aardema F. The inference-based approach to obsessive-compulsive disorder: A comprehensive review of its etiological model, treatment efficacy, and model of change. J Affect Disord. 2016;202:187–96. doi: 10.1016/j.jad.2016.05.060. [DOI] [PubMed] [Google Scholar]
- 90.Braga DT, Manfro GG, Niederauer K, Cordioli AV. Full remission and relapse of obsessive-compulsive symptoms after cognitive-behavioral group therapy: A two-year follow-up. Braz J Psychiatry. 2010;32:164–8. doi: 10.1590/s1516-44462010000200012. [DOI] [PubMed] [Google Scholar]
- 91.O’Neill J, Feusner JD. Cognitive-behavioral therapy for obsessive-compulsive disorder: Access to treatment, prediction of long-term outcome with neuroimaging. Psychol Res Behav Manag. 2015;8:211–23. doi: 10.2147/PRBM.S75106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hiss H, Foa EB, Kozak MJ. Relapse prevention program for treatment of obsessive-compulsive disorder. J Consult Clin Psychol. 1994;62:801–8. doi: 10.1037//0022-006x.62.4.801. [DOI] [PubMed] [Google Scholar]
- 93.Veale D, Gledhill LJ, Christodoulou P, Hodsoll J. Body dysmorphic disorder in different settings: A systematic review and estimated weighted prevalence. Body Image. 2016;18:168–86. doi: 10.1016/j.bodyim.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 94.Phillips KA, Hollander E, Rasmussen SA, Aronowitz BR, DeCaria C, Goodman WK. A severity rating scale for body dysmorphic disorder: Development, reliability, and validity of a modified version of the Yale-Brown obsessive compulsive scale. Psychopharmacol Bull. 1997;33:17–22. [PubMed] [Google Scholar]
- 95.Brohede S, Wingren G, Wijma B, Wijma K. Validation of the body dysmorphic disorder questionnaire in a community sample of Swedish women. Psychiatry Res. 2013;210:647–52. doi: 10.1016/j.psychres.2013.07.019. [DOI] [PubMed] [Google Scholar]
- 96.Krebs G, Fernández de la Cruz L, Mataix-Cols D. Recent advances in understanding and managing body dysmorphic disorder. Evid Based Ment Health. 2017;20:71–5. doi: 10.1136/eb-2017-102702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wilhelm S, Phillips KA, Steketee G. 1st ed. New York: The Guilford Press; 2012. Cognitive-Behavioral Therapy for Body Dysmorphic Disorder: A Treatment Manual. [Google Scholar]
- 98.Veale D. Advances in a cognitive behavioural model of body dysmorphic disorder. Body Image. 2004;1:113–25. doi: 10.1016/S1740-1445(03)00009-3. [DOI] [PubMed] [Google Scholar]
- 99.Mataix-Cols D, Fernández de la Cruz L, Isomura K, Anson M, Turner C, Monzani B, et al. A pilot randomized controlled trial of cognitive-behavioral therapy for adolescents with body dysmorphic disorder. J Am Acad Child Adolesc Psychiatry. 2015;54:895–904. doi: 10.1016/j.jaac.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 100.Wilhelm S, Phillips KA, Greenberg JL, O’Keefe SM, Hoeppner SS, Keshaviah A, et al. Efficacy and posttreatment effects of therapist-delivered cognitive behavioral therapy vs. supportive psychotherapy for adults with body dysmorphic disorder: A randomized clinical trial. JAMA Psychiatry. 2019;76:363–73. doi: 10.1001/jamapsychiatry.2018.4156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Harrison A, Fernández de la Cruz L, Enander J, Radua J, Mataix-Cols D. Cognitive-behavioral therapy for body dysmorphic disorder: A systematic review and meta-analysis of randomized controlled trials. Clin Psychol Rev. 2016;48:43–51. doi: 10.1016/j.cpr.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 102.Veale D, Miles S, Anson M. Long-term outcome of cognitive behavior therapy for body dysmorphic disorder: A naturalistic case series of 1 to 4 years after a controlled trial. Behav Ther. 2015;46:775–85. doi: 10.1016/j.beth.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 103.Enander J, Andersson E, Mataix-Cols D, Lichtenstein L, Alström K, Andersson G, et al. Therapist guided internet based cognitive behavioural therapy for body dysmorphic disorder: Single blind randomised controlled trial. BMJ. 2016;352:i241. doi: 10.1136/bmj.i241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Greenberg JL, Phillips KA, Steketee G, Hoeppner SS, Wilhelm S. Predictors of response to cognitive-behavioral therapy for body dysmorphic disorder. Behav Ther. 2019;50:839–49. doi: 10.1016/j.beth.2018.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Grant JE, Chamberlain SR. Trichotillomania. Am J Psychiatry. 2016;173:868–74. doi: 10.1176/appi.ajp.2016.15111432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Grant JE, Stein DJ. Body-focused repetitive behavior disorders in ICD-11. Braz J Psychiatry. 2014;36(Suppl 1):59–64. doi: 10.1590/1516-4446-2013-1228. [DOI] [PubMed] [Google Scholar]
- 107.Jafferany M, Patel A. Skin-picking disorder: A guide to diagnosis and management. CNS Drugs. 2019;33:337–46. doi: 10.1007/s40263-019-00621-7. [DOI] [PubMed] [Google Scholar]
- 108.Jones G, Keuthen N, Greenberg E. Assessment and treatment of trichotillomania (hair pulling disorder) and excoriation (skin picking) disorder. Clin Dermatol. 2018;36:728–36. doi: 10.1016/j.clindermatol.2018.08.008. [DOI] [PubMed] [Google Scholar]
- 109.Keuthen NJ, O'Sullivan RL, Ricciardi JN, Shera D, Savage CR, Borgmann AS, et al. The Massachusetts general hospital (MGH) hairpulling scale: 1. development and factor analyses. Psychother Psychosom. 1995;64:141–5. doi: 10.1159/000289003. [DOI] [PubMed] [Google Scholar]
- 110.Rehm I, Moulding R, Nedeljkovic M. Psychological treatments for trichotillomania: Update and future directions. Australas Psychiatry. 2015;23:365–8. doi: 10.1177/1039856215590029. [DOI] [PubMed] [Google Scholar]
- 111.Morris SH, Zickgraf HF, Dingfelder HE, Franklin ME. Habit reversal training in trichotillomania: Guide for the clinician. Expert Rev Neurother. 2013;13:1069–77. doi: 10.1586/14737175.2013.827477. [DOI] [PubMed] [Google Scholar]
- 112.Keuthen NJ, Rothbaum BO, Fama J, Altenburger E, Falkenstein MJ, Sprich SE, et al. DBT-enhanced cognitive-behavioral treatment for trichotillomania: A randomized controlled trial. J Behav Addict. 2012;1:106–14. doi: 10.1556/JBA.1.2012.003. [DOI] [PubMed] [Google Scholar]
- 113.Lee EB, Homan KJ, Morrison KL, Ong CW, Levin ME, Twohig MP. Acceptance and commitment therapy for trichotillomania: A randomized controlled trial of adults and adolescents. Behav Modif. 2020;44:70–91. doi: 10.1177/0145445518794366. [DOI] [PubMed] [Google Scholar]
- 114.Selles RR, McGuire JF, Small BJ, Storch EA. A systematic review and meta-analysis of psychiatric treatments for excoriation (skin-picking) disorder. Gen Hosp Psychiatry. 2016;41:29–37. doi: 10.1016/j.genhosppsych.2016.04.001. [DOI] [PubMed] [Google Scholar]