INTRODUCTION
Depressive disorders are one of the most common psychiatric disorders that occur in people of all ages across all world regions. Although it may present at any age however adolescence to early adults is the most common age of onset, and females are affected two times more in comparison to the males. Depressive disorders can occur as heterogeneous conditions in clinical scenario ranging from transient minor symptoms to severe and debilitating clinical conditions, causing severe social and occupational impairments. Usually, it presents with constellations of cognitive, emotional, behavioral, physiological, interpersonal, social, and occupational symptoms. The illness can be of various severities, and a significant proportion of the patients can have recurrent illness. Depression is also highly comorbid with several psychiatric and medical illnesses such as anxiety disorders, substance use, obsessive–compulsive disorder, diabetes, hypertension, and cardiovascular illnesses.
Major depressive disorders accounted for around 8.2% global years lived with disability (YLD) in 2010, and it was the second leading cause of the YLDs. In addition, they also contribute to the burden of several other disorders indirectly such as suicide and ischemic heart disease.[1]
EVIDENCE BASE FOR COGNITIVE BEHAVIORAL THERAPY IN DEPRESSION
Cognitive behavioral therapy (CBT) is one of the most evidence-based psychological interventions for the treatment of several psychiatric disorders such as depression, anxiety disorders, somatoform disorder, and substance use disorder. The uses are recently extended to psychotic disorders, behavioral medicine, marital discord, stressful life situations, and many other clinical conditions.
A sufficient number of researches have been conducted and shown the efficacy of CBT in depressive disorders. A meta-analysis of 115 studies has shown that CBT is an effective treatment strategy for depression and combined treatment with pharmacotherapy is significantly more effective than pharmacotherapy alone.[2] Evidence also suggests that relapse rate of patient treated with CBT is lower in comparison to the patients treated with pharmacotherapy alone.[3]
Treatment guidelines for the depression suggest that psychological interventions are effective and acceptable strategy for treatment. The psychological interventions are most commonly used for mild-to-moderate depressive episodes. As per the prevailing situations of India with regards to significant lesser availability of trained therapist in most of the places and patients preferences, the pharmacological interventions are offered as the first-line treatment modalities for treatment of depression.
Indication for Cognitive behavior therapy as enlisted in table 1.
Table 1.
Indications for cognitive behavioral therapy (situations that can call for preferred use of the psychological interventions) are
| 1. Client’s preference |
| 2. Availability and accessibility of the trained therapist |
| 3. Special situations like children and adolescents, pregnancy, lactation, female in fertile age group planning for pregnancy, medical comorbidities, etc. |
| 4. Inability to tolerate psychopharmacological treatments |
| 5. The presence of significant psychosocial factors, intrapsychic conflicts, and interpersonal difficulties |
CONTRAINDICATIONS FOR COGNITIVE BEHAVIORAL THERAPY
There is no absolute contraindication to CBT; however, it is often reported that clients with comorbid severe personality disorders such as antisocial personality disorders and subnormal intelligence are difficult to manage through CBT. Special training and expertise may be needed for the treatment of these clients.
Patient with severe depression with psychosis and/or suicidality might be difficult to manage with CBT alone and need medications and other treatment before considering CBT. Organicity should be ruled out using clinical evaluation and relevant investigations, as and when required.
There are many advantages of CBT in depression as given in table 2
Table 2.
Advantages of cognitive behavioral therapy in depression
| 1. It is used to reduce symptoms of depression as an independent treatment or in combination with medications |
| 2. It is used to modify the underlying schemas or beliefs that maintain the depression |
| 3. It can be used to address various psychosocial problems, for example, marital discord, job stress which can contribute to the symptoms |
| 4. Reduce the chances of recurrence |
| 5. Increase the adherence to recommended medical treatment |
CHOICE OF TREATMENT SETTINGS
CBT can be done on an Out Patient Department (OPD) basis with regular planned sessions. Each session lasts for about 45 min–1 h depending on the suitability for both patients and therapists. In specific situations, the CBT can be delivered in inpatient settings along with treatment as usual such as adjuvant treatment in severe depression, high risk for self-harm or suicidal patients, patients with multiple medical or psychiatric comorbidities and in patients hospitalized due to social reasons.
ASSESSMENT AND EVALUATION FOR THE THERAPY
A detail diagnostic assessment is needed for the assessment of psychopathology, premorbid personality, diagnosis, severity, presence of suicidal ideations, and comorbidities. Baseline assessment of severity using a brief scale will be helpful in mutual understanding of severity before starting therapy and also to track the progress. Clients during depressive illness often fail to recognize early improvement and undermine any positive change. Objective rating scale hence helps in pointing out the progress and can also help in determining agenda during therapy process. Beck Depression Inventory (A. T. Beck, Steer, and Brown, 1996), the Depression Anxiety Stress Scales (Lovibond and Lovibond, 1995), Montgomery-Asberg Depression Rating Scale, Hamilton Rating Scale for Depression are useful rating scales for this purpose. The assessment for CBT in depression is, however, different from diagnostic assessment.
THE USE OF COGNITIVE BEHAVIORAL THERAPY ACCORDING TO SEVERITY OF DEPRESSION
Various trials have shown the benefit of combined treatment for severe depression.
Combined therapy though costlier than monotherapy it provides cost-effectiveness in the form of relapse prevention.
Number of sessions depends on patient responsiveness.
Booster sessions might be required at the intervals of the 1–12th month as per the clinical need.
A model for reference is given in table 3
Table 3.
The use of cognitive behavioral therapy according to the severity of depression
| Type of depression | First line | Adjunctive | Number of sessions |
|---|---|---|---|
| Mild | CBT or medication | CBT or medication | 8–12 |
| Moderate | CBT or medication | CBT or medication | 8–16 |
| Severe | Medication or/and Somatic treatment | CBT | 16 or more |
| Chronic depression and recurrent depression | CBT or medication | CBT or medication | 16 or more and booster sessions up to 1–2 years |
The general outline of CBT for depression has been discussed in table 4
Table 4.
Overview of cognitive behavioral therapy for depression
| 1. Mutually agreed on problem definition by therapist and client |
| 2. Goal settings |
| 3. Explaining and familiarizing client with five area model of CBT |
| 4. Improving awareness and understanding on one’s cognitive activity and behavior |
| 5. Modification of thoughts and behavior - using principles of Socratic dialogue, guided discovery, and behavioral experiments/exposure exercise |
| 6. Application and consolidation of new skills and strategies in therapy sessions and homework sessions to generalize it across situations |
| 7. Relapse prevention |
| 8. End of the therapy |
CBT – Cognitive behavioral therapy
COGNITIVE MODEL FOR DEPRESSION
Cognitive theory conceptualizes that people are not influenced by the events rather the view they take of the events. It essentially means that individual differences in the maladaptive thinking process and negative appraisal of the life events lead to the development of dysfunctional cognitive reactions. This cognitive dysfunction is in turn is responsible for the rest of the symptoms in affective and behavioral domains.
Aaron beck proposed a cognitive model of depression, and it is detailed in Figure 1. Cognitive dysfunctions are of the following categories.
Figure 1.
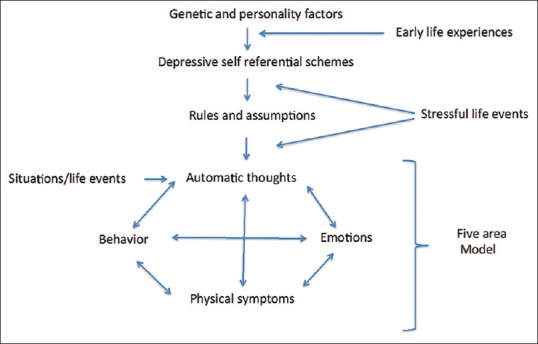
Cognitive behavioral therapy model of depression
Schema - stable internal structure of information usually formed during early life, also include core belief about self
information processing and intermediate belief are usually interpreted as rules of living and usually expressed in terms of “if and then” sentences
Automatic thoughts - proximally related to everyday events and in depression, often reflects cognitive triad, i.e., negative view of oneself, world, and future.
Negative cognitive triad of depression as given beck is as following:
I am helpless (helplessness)
The future is bleak (hopelessness)
I am worthless (worthlessness).
CHOICE OF THE PATIENT
Patient-related factors that facilitated response are
Psychological mindedness of patients: Patients who are able to understand and label their feelings and emotions generally respond better to CBT. Although some patients in the course of treatment learn those skills during treatment
Intellectual level of the patient might also affect the overall effectiveness of the treatment
Willingness and motivation on the part of patients: Although it is not prerequisite, patients who are motivated to analyze their feelings and ready to undergo various homework show a better response to treatment
Patient preference is single most important factor: After initial assessment of the patient those who prefer psychological treatment can be offered CBT alone or in combination depending on type of depression
Those with mild to moderate depression CBT can be recommended as a first line of treatment
Patients with severe depression might need combination of both CBT and medications (and or other treatments)
Special situations such as children and adolescents, pregnancy, lactation, female in fertile age group planning for pregnancy, medical comorbidities
Inability to tolerate psychopharmacological treatment
The presence of significant psychosocial factors, intrapsychic conflicts, and interpersonal difficulties.
Therapist related factors
Availability of cognitive behavioral therapist/psychiatrist
The ability of therapist to form therapeutic alliance with the patient.
CLINICAL INTERVIEW FOR COGNITIVE BEHAVIORAL THERAPY
Symptoms and associated cognitions
Negative automatic thoughts both trigger and enhance depression. It might be helpful to identify unhealthy automatic thoughts associated with symptoms of depression.
Some common symptoms and associated automatic thoughts are given in table 5.
Table 5.
Symptoms of depression and associated cognitions
| Serial number | Symptoms | Automatic thoughts |
|---|---|---|
| 1 | Behavioral: lower activity levels | I cants do it. It is too much for me |
| 2 | Guilt | I am letting everybody down |
| 3 | Shame | What everyone must be thinking about me |
Impact on functioning
it is important to know the extent and effect of depression on the overall functioning and interpersonal relationships.
Coping strategies
Sometimes patients with depression might have adapted a coping strategies which make them feel good for short duration (e.g., alcohol consumption) but might be unhealthy in long term.
Onset of current symptoms
Patient's perception about the situation at the onset of symptoms might provide useful information about underlying cognitive distortions.
Background information
Detailed history of patient is necessary, including patients premorbid personality.
The therapist should be able to do the cognitive case conceptualization for the patient as given in Figure 2.
Figure 2.
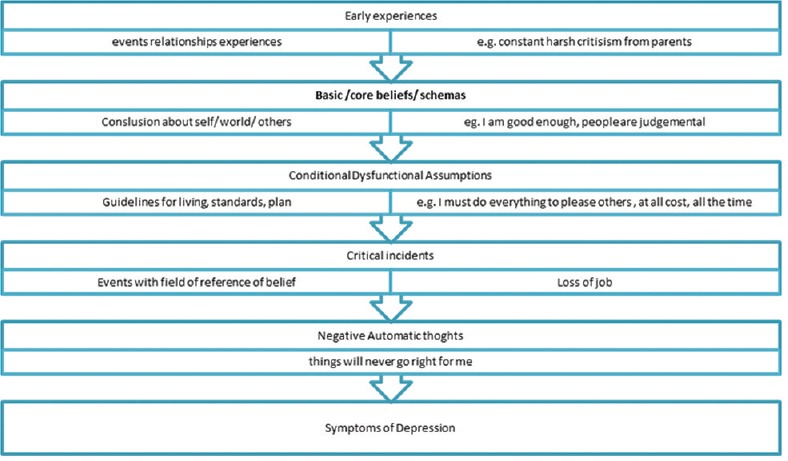
Case conceptualization for the cognitive model of depression
MANAGING TREATMENT
An outline of the breakup of typical session of CBT is given in table 6.
Table 6.
Session structure of cognitive behavioral therapy
| Serial number | Component | Time (min) |
|---|---|---|
| 1 | Beginning of the session | |
| Mood check | 5–10 | |
| Agenda setting | ||
| Reviewing homework | ||
| 2 | Discussion of agenda items/problems | 35–40 |
| Description of occurrence of specific problem | ||
| Elicitation and confirmation of elements of the cognitive model | ||
| Collaborative discussion regarding how to approach a problem | ||
| Rationale for the introduction of intervention | ||
| Assessment of the efficacy of intervention | ||
| Summary by patient | ||
| Collaborative action plan in writing | ||
| Planning and discussing a homework and how to approach it | ||
| 3 | Feedback to the therapist | 1–2 |
Starting treatment
First treatment interview has mainly four objectives:
To establish a warm collaborative therapeutic alliance
To list specific problem set and associated goals
To psycho-educate patient regarding the cognitive model and vicious cycle that maintains the depression
Give the patient idea about further treatment procedures.
CBT can be explained in the following headings
Starting treatment
Behavioral interventions
Working with negative automatic thoughts
Ending session.
Starting treatment
The first treatment interview has four main objectives:
To establish a warm, collaborative therapeutic alliance
To list specific problems and associated goals, and select a first problem to tackle
To educate the patient about the cognitive model, especially the vicious circle that maintains depression
To give the patient first-hand experience of the focused, workman-like, empirical style of CBT.
These convey two important messages: (1) It is possible to make sense of depression; (2) there is something the patient can do about it. These messages directly address hopelessness and helplessness.
Identifying problems and goals:-The various problems faced by patients should be included in a list which can include symptoms of depression or social problems (e.g., family conflict). Developing this list at the end of the first session helps in planning treatment goals
Introducing cognitive model of depression:- In the first session at least a basic idea about how our cognitions affect our emotions and behavior is taught to the patient. The data provided by patient can be used to give insight into behaviors
Where to start:-Common treatment goal is agreed upon by patient and therapist, therapeutic alliance is of key importance in CBT. Appropriate homework assignment should be given to patient according to predecided goal.
Behavioural interventions
Reducing ruminations
It has been seen that depressed patients spend a significant amount of time and attention focusing on their shortcomings. Making patient aware of those negative ruminations and consciously diverting attention toward certain positive aspects can be taught to patients.
Monitoring activities
Loss of interest in day to day activities is central to the depression. It has been seen that early behavioral intervention has been increased sense of autonomy in the patients.
Patients are taught to record each and every activity hour by hour on the activity schedule. Each activity is rated 0–10 for Pleasure (P) and Mastery (M). P ratings indicate how enjoyable the activity was, and M ratings how much of an achievement it was. Mostly depressed patients feel low on achievement all the time. Hence, M should be explained as “achievement how you felt at the time of doing.” Patients are instructed to rate activities immediately and not retrospectively.
Example of activity schedule is
Activity Chart Write in each box, activity performed and depression rating from 0-100% (0-minimal, 100-maximum)
| Time | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
| 6-7 AM | |||||||
| 7-8 AM | |||||||
| 8-9 AM* | Breakfast, talk with wife, 40% | Breakfast alone, 60% | Walk, 30% | Breakfast with son, 50% | Talk with friend on phone, 20% | Breakfast alone, 60% | Breakfast with everyone in family, 20% |
| 10-11 PM | Hourly rating from waking up till time to sleep | What everyone must be thinking about me |
*example
Planning activities
Once the patient learns to self-monitor activities each day is planned in advance.
This helps patients by:
This provides a structure and helps with setting priorities
This avoids the need to keep making decisions about what to do next
This changes perception from chaos to manageable tasks
This increases the chances that activities will be carried out
This enhances patients’ sense of control.
A plan for activities is made in such a way that both pleasure and mastery are balanced (e.g., ironing cloths followed by listening to music). The tasks which are generally avoided by patient can be divided into graded tasks.
The patient is taught to evaluate each and every day in detail also encouraged to keep the record of unhelpful negative thoughts regarding tasks.
Other important behavioral activities are:-
Mindfulness meditation: Helps people stay grounded in the present by keeping away from ruminations
Successive approximation: Breaking larger tasks into smaller tasks which are easy to accomplish
Visualizing the best part of the day
Pleasant activity scheduling.
Scheduling an activity in near future which one can look on with mastery and with sense of achievement.
Working with negative automatic thoughts
The main tool for this negative automatic thought record.
Thought Record -1
| Situation (write down exact details of specific situation) | Emotions (Rate 0-100%) | Behaviour | Physical reactions | Automatic thoughts/ images (Identify most important thought) |
Thought Record – 2
| Situation (write down exact details of specific situation) | Emotions (Rate 0-100%) | Automatic thoughts/ images (Identify most important thought) | Evidence for automatic thoughts | Evidence against automatic thoughts | Balanced thought | Rate emotion now (0-100%) |
Identifying negative automatic thoughts
Patients learn to record upsetting incidents as soon as possible after they occur (delay makes it difficult to recall thoughts and feelings accurately). They learn:
To identify unpleasant emotions (e.g., despair, anger, guilt), signs that negative thinking is present. Emotions are rated for intensity on a 0–100 scale. These ratings (though the patient may initially find them difficult) help to make small changes in emotional state obvious when the search for alternatives to negative thoughts begins. This is important since change is rarely all-or-nothing, and small improvements may otherwise be missed
To identify the problem situation. What was the patient doing or thinking about when the painful emotion occurred (e.g., “waiting at the supermarket checkout,” “worrying about my husband being late home”)?
To identify negative automatic thoughts associated with the unpleasant emotions. Sessions direct the therapist towards asking: “And what went through your mind at that moment?” Patients become aware of thoughts, images, or implicit meanings that are present when emotional shifts occur, and record. Belief in each thought is also rated on a 0%–100%.
Questioning negative automatic thoughts
Therapist can help patient to discover dysfunctional automatic thoughts through “guided discovery.”
What is evidence?
What are alternative views?
What are advantages and disadvantages of this way of thinking?
What are my thinking biases?
Common cognitive distortions are
Black– and– white (also called all– or– nothing, polarized, or dichotomous thinking): Situations viewed in only two categories instead of on a continuum. Example: “If I don’t top the exams. I’m a failure”
Fortune-telling (also called catastrophizing): Future is predicted negatively without considering other possible, more likely outcomes. Example: “I ll be so upset, i won’t be able to function at all”
Disqualifying or discounting the positive: The person unreasonably tell oneself that positive experiences, deeds, or qualities do not count. Example: “I cracked the examl, but that doesn’t mean I’m competent; It was a fluke”
Emotional reasoning: One thinks something must be true because he/she “feels” (actually believe) it so strongly, ignoring or discounting evidence to the contrary. Example: “I know I successfully complete most of my tasks, but I still feel like I’ m incompetent”
Labeling: One puts a fixed, global label on oneself or others without considering that the evidence might more reasonably lead to a less disastrous conclusion. Example: “I’m a failure. He's not good enough”
Magnification/minimization: When one evaluates oneself, another person, or a situation, one unreasonably magnifies the negative and/or minimizes the positive. Example: “Getting a C Grade in exams proves how mediocre I am. Getting high marks doesn’t mean I’m smart”
Selective abstraction (also called mental filter): One pays undue attention to one's negative detail instead of seeing the whole picture. Example: “Because I got just passing marks in one subject in my examinations (which also contained distinctions in other subjects) it means I’m not a good student”
Mind reading: One believes that he/she knows what others are thinking, failing to consider other, more likely possibilities. Example: “He assumes that his boss thinks that he is a novice for this assignment”
Overgeneralization: One makes a negative conclusion that goes far beyond the current situation. Example: “(Because I felt uncomfortable at the meeting) I don’t have what it takes to be a group leader”
Personalization: O ne believes others are behaving negatively because of him/her, without exploring alternative explanations for their behavior. Example: “The watchman didn’t smile at me because I did something wrong”
Imperatives (also called “Should” and “must” statements): One has a precise, fixed idea of how one or others should behave, and they overestimate how bad it is that these expectations are not met with. Example: “It's terrible that I sneeze as I am a Gym Trainer”
Tunnel vision: One only views the negative aspects of a situation. Example: “My subordinate can’t do anything right. He's callous, casual and insensitive towards his job.”
Testing negative automatic thoughts: What can I do now?
It is important that cognitive changes that are brought out by questioning are consolidated by behavior experiments.
Ending the treatment
CBT is time-limited goal-directed form of therapy. Hence, the patient is made aware about end of treatment in advance. This can be done through the following stages.
Dysfunctional assumptions identification
Consolidating learning blueprint
Preparation for the setback.
Dysfunctional assumptions identification
Once the patient is able to identify negative automatic thoughts. Before ending treatment patient patients should be made aware about dysfunctional assumptions.
Where did this rule come from? Identifying the source of a dysfunctional assumption (e.g., parental criticism) often helps to encourage distance by suggesting that its development is understandable, though it may no longer be relevant or useful
In what ways is the rule unrealistic? Dysfunctional assumptions do not fit the way the world works. They operate by extremes, which are reflected in their language (always/never rather than some of the time; must/should/ought rather than want/prefer/would like)
In what ways is the rule helpful? Dysfunctional assumptions are not usually wholly negative in their effects. For example, perfectionism may lead to genuine, high-quality performance. If such advantages are not recognized and taken into account when new assumptions are formulated, the patient may be reluctant to move forward
In what ways is the rule unhelpful? The advantages of dysfunctional assumptions are normally outweighed by their costs. Perfectionism leads to rewards, but it also undermines satisfaction with achievements and stops people learning from constructive criticism
What alternative rule might be more realistic and helpful? Once the old assumption has been undermined, it is helpful to formulate an explicit alternative (e.g., "It is good to do things well, but I am only human-sometimes I make mistakes"). This provides a new guideline for living, rather than simply undermining the old system
What needs to be done to consolidate the new rule? As with negative automatic thoughts, re-evaluation is best made real through experience: Behavioral experiments.
Consolidating learning blueprint
The patient should be able to summarize whatever he has learned throughout the sessions.
The following questions might help to set the framework:
How did my problems develop? (unhelpful beliefs and assumptions, the experiences that led to their formation, events precipitating onset)
What kept them going? (maintenance factors)
What did I learn from therapy that helped? Techniques (e.g., activity scheduling) and Ideas (e.g., "I can do something to influence my mood")
What were my most unhelpful negative thoughts and assumptions? What alternatives did I find to them? (summarized in two columns)
How can I build on what I have learned? (a solid, practical, clearly specified action plan).
Preparation for the setback
Since depression is recurring illness patient should be made aware about the possibility of relapse.
What might lead to a setback for me? For example, future losses (e.g., children leaving home) and stresses (e.g., financial difficulties), i.e., events which impinge on patients’ vulnerabilities and are thus liable to be interpreted negatively
What early warning signs do I need to be alert for?
Feelings, behaviors, and symptoms that might indicate the beginning of another depression are identified and listed
If I notice that I am becoming depressed again, what should I do? Clear simple instructions, which will make sense despite low mood, are needed here. Specific ideas and techniques summarized earlier in the blueprint should be referred to.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Beck J, Hindman R. Cognitive therapy. In: Sadock B, Sadock V, Ruiz P, editors. Kaplan & Sadock's Comprehensive Textbook of Psychiatry. New Delhi: Wolter Kluwer India Pvt Ltd; 2017. pp. 2760–74. [Google Scholar]
- 2.Fennell M. Cognitive behaviour therapy for depressive disorders. In: Gelder M, Andreasen N, Lopez-Ibor J, Geddes J, editors. New Oxford Textbook of Psychiatry. New York: Oxford University Press; 2012. pp. 1304–12. [Google Scholar]
- 3.American Psychiatric Association. Practice Guideline for the Treatment of Patients with Major Depressive Disorder. American Psychiatric Association. 2010. Available from: http://psychiatryonline.org/content.aspx?bookid=28§ionid=1667485 .
- 4.Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol. 2006;74:658–70. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- 5.Pampallona S, Bollini P, Tibaldi G, Kupelnick B, Munizza C. Combined pharmacotherapy and psychological treatment for depression: A systematic review. Arch Gen Psychiatry. 2004;61:714–9. doi: 10.1001/archpsyc.61.7.714. [DOI] [PubMed] [Google Scholar]
- 6.Shapiro DA, Barkham M, Rees A, Hardy GE, Reynolds S, Startup M. Effects of treatment duration and severity of depression on the effectiveness of cognitive-behavioral and psychodynamic-interpersonal psychotherapy. J Consult Clin Psychol. 1994;62:522–34. doi: 10.1037/0022-006x.62.3.522. [DOI] [PubMed] [Google Scholar]
- 7.Boyes A. 2012. Available from: https://www.psychologytoday.com/blog/in-practice/201212/cognitive-behavioral-therapy-techniques-work .


