Abstract
Necrobiotic xanthogranuloma (NXG) is a rare form of inflammatory granulomatous disease of the skin characterized by the presence of pruritic to painful lesions, generally located in the periorbital area, although trunk and proximal extremities may also be involved. We report a case of a 69-year-old male patient with extensive involvement of the trunk, upper and lower extremities, and an associated gamma monoclonal gammopathy. The skin biopsy was consistent with the diagnosis of NXG. Necrobiosis lipoidica and granuloma annulare were the major differential diagnosis in this case. We highlight the importance of searching for clinical and histological features that may differentiate these entities, which is crucial to select an adequate therapeutic and surveillance strategy.
Keywords: Monoclonal gammopathy, plaques, ulcers, xanthogranuloma
Introduction
Non-infectious granulomatous disorders represent a group of diseases with substantial clinical and histological overlap, contributing to a significant diagnostic challenge.[1] Necrobiotic xanthogranuloma (NXG), necrobiosis lipoidica (NL) and granuloma annulare (GA) are included in this group, and their distinction is not always obvious.
Case History
A 69-year-old male patient presented to dermatology outpatient department with extensive cutaneous lesions evolving during the last 7 years. The lower legs were the first affected sites with progressive involvement of the trunk and upper extremities. His past medical history included type 2 diabetes, arterial hypertension, and ischemic heart disease. We observed atrophic red-brown plaques on the trunk and tender red-brown ulcerated patches on the forearms, lower legs, and feet [Figure 1a and b]. In addition, on the dorsum of the left hand there was a shiny patch of variable red, brown, and yellowish colors with telangiectasia, and on the dorsum of the right hand there was a firm, non-tender, yellowish-red nodule [Figure 2a and b]. There was no regional lymphadenopathy or hepato-splenomegaly. Biopsies of the abdomen, right forearm, and left hand lesions were performed. The histological examination of the three samples revealed a necrobiotic granulomatous dermatitis. Confluent layers of necrobiotic collagen, with an eosinophilic hyalinized appearance, alternating with inflammation were observed. The lesions were centered in the reticular dermis and extended into the subcutaneous tissue, sparing the papillary dermis [Figure 3a]. In the periphery of the necrobiotic foci, there was a palisading inflammatory infiltrate, composed predominantly of histiocytes (CD68 positive), with focal participation of lymphocytes and plasma cells [Figure 3b]. Occasional foreign body-type multinucleated giant cells were identified. Colloidal iron staining highlighted the presence of mucin in the necrobiotic foci, and orcein stain showed loss of elastic fibers. Moreover, in the specimen from the right forearm [Figure 3c], a more cellular inflammatory infiltrate in the lower dermis and focally extending to the subcutaneous tissue was observed. It was composed predominantly of histiocytes (CD68 positive, S100 negative), focally with vacuolated/foamy cytoplasm. There were cholesterol clefts along with foreign body-type giant cells, histiocytes with foamy cytoplasm, and rare atypical Touton-type giant cells [Figure 3d-e]. No evidence of granulomatous involvement of muscular vessels was observed, and no microorganisms were identified in the histochemical study with PAS, Grocott, and Ziehl-Neelsen stains.
Figure 1.
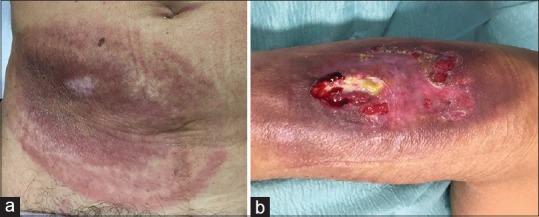
(a) Red-brown plaque with central atrophy of the abdomen and (b) ulcer with pallid center and discrete peripheral scaling of the lateral aspect of the right forearm
Figure 2.

(a) Red-brown well-demarcated plaque with central telangiectasia of the left hand and (b) yellowish-red nodule of the dorsum of the right hand
Figure 3.
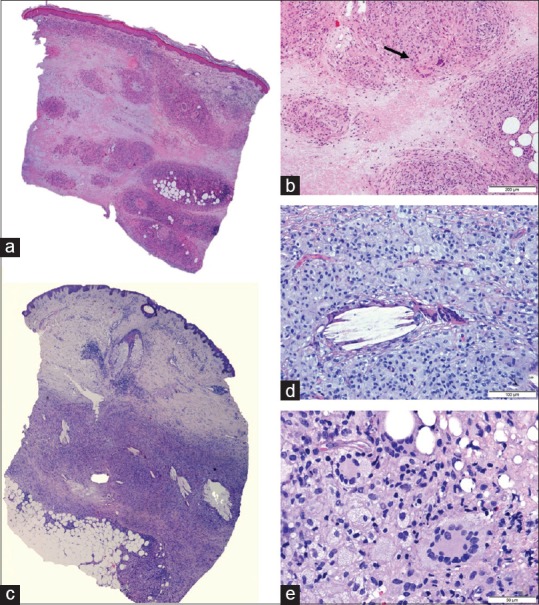
(a) Low-power view of the biopsy performed in the left hand. Confluent areas of necrobiotic collagen in the reticular dermis and subcutaneous tissue (H and E, low-power view); (b) Non-palisading inflammatory infiltrate, predominantly histiocytic with participation or rare multinucleated giant cells (arrows) (H and E, 100x); (c) Low-power view of the biopsy performed in the right forearm, disclosing a more cellular infiltrate centered in the lower dermis and extending to subcutaneous tissue; (d) cholesterol clefs, involved by multinucleated giant cells and foamy histiocytes (H and E, 200x); (e) Touton-type giant cells (H and E, 400x)
Due to the persistence of the cutaneous lesions and atypical clinical features, a broad blood analysis was performed, which revealed a gamma monoclonal gammopathy, without fulfilling the criteria for multiple myeloma. There were no other relevant changes in the blood analysis. To exclude extracutaneous involvement of the disease, abdominal ultrasound and echocardiogram were performed, without changes. There were no ophthalmologic findings suggestive of eye involvement.
The patient was started on treatment with pentoxifylline 400 mg three times per day and topical tacrolimus 0.1% ointment applied on the borders of the skin lesions resulting in mild improvement. Due to the association with monoclonal gammopathy and extensive involvement of skin, chemotherapy with cyclophosphamide, bortezomib, and dexamethasone was initiated. After 3 cycles, there was an improvement of the skin lesions, especially in the forearms and legs [Figures 4 and 5].
Figure 4.

Complete healing of the ulcer of the right forearm
Figure 5.
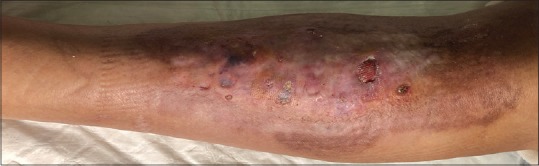
Left lower leg with a small ulcerated area and clear improvement after initiating targeted treatment
Discussion
NXG is an extremely rare form of inflammatory granulomatous disease of the skin.[1,2,3] It usually occurs in middle-aged and elderly patients, with no gender predilection.[3,4] Lesions are typically pruritic to painful and are predominantly located in the periorbital area, although trunk and proximal extremities can also be involved.[3,5] Possible evolution to scaring, telangiectasia, and ulceration has been described.[2,3] The association with an underlying monoclonal gammopathy is present in about 80% of the cases: the most frequent type is IgG-κ monoclonal gammopathy (65%), followed by IgG-λ (35%) and less commonly IgA.[1,4] In this situation, 10–25% of the patients may develop multiple myeloma in the future.[6]
NL is one of the major differential diagnosis of NXG. It usually manifests between the 3rd to 4th decades of life, with a female predominance.[7] Most of the patients with NL have diabetes.[1] Skin lesions may occur before, simultaneously or after this diagnosis, although they are also described as appearing independently from the glucose dysregulation.[1] Classically, well-demarcated patches to plaques develop in the pretibial area, although other sites like forearms, hands, and trunk may be involved.[7]
GA is a benign inflammatory dermatosis that may appear in all age groups.[8] It can develop in anywhere, although more frequently in the lateral and dorsal aspects of the extremities.[8] Clinically, there may be flesh colored to erythematous papules that coalesce to form annular plaques (localized and disseminated types), subcutaneous nodules (subcutaneous type), erythematous patches (interstitial type), and umbilicated papules with keratotic core (perforating type).[8]
There may be clinical and histological similarities between these three entities and, in some cases, it is difficult to completely separate them.
Clinically, while NXG and NL may show similarities, the presence of indurated and sharply demarcated yellowish to red-brown papules, nodules, and plaques, frequently with ulceration, favor the diagnosis of NXG.[5,9] Typical lesions of GA include erythematous to violaceus papules that may coalesce to form large plaques with well-demarcated border without ulceration.[9] The most common location is the periorbital area in the case of NXG, while in NL and GA there are predominant lesions in the pretibial region and extremities, respectively.[5]
Histological differentiation between NXG, NL, and GA is challenging due to overlapping features. NXG and NL lesions are characterized by confluent areas of necrobiosis, centered in the lower dermis. In NXG, there may be an extension of foci of necrobiosis to the subcutaneous tissue contrasting with NL and GA where it usually appears in the upper dermis.[5,9] GA usually shows necrobiotic areas containing basophilic mucin and palisaded by mononuclear cell histiocytic forms, while giant cells are usually absent.[2,10] Mucin deposition may also be observed in NXG but is not a feature of NL.[8,9] Classically, NXG tends to be more cellular and features numerous cholesterol clefts, bizarre multinucleated giant cells, and Touton-type giant cells.[2,5] The absence of vascular changes also favors the diagnosis of NXG, while in NL vessel involvement may include features as hyalinization and thrombosis.[3,11] Small punch biopsies may be misleading, and clinical correlation should be taken into consideration before making a definitive diagnosis.
The patient presented a history of diabetes mellitus in association with paraproteinemia. The history of type 2 diabetes and the predominance of pretibial lesions without the involvement of the periorbital regions support the hypothesis of an NL. On the other hand, the monoclonal gammopathy in association with the presence of ulcerated lesions, as well as the histological findings including the depth of the granulomatous inflammation, the hyalinized collagen, the presence of cholesterol clefts and Touton-type giant cells as well as the absence of vascular changes favor the diagnosis of NXG.
This report represents an extensive cutaneous involvement of a patient with NXG. The clinical and histological findings in association with the presence of paraproteinemia lead to the diagnosis of NXG. This case emphasizes the clinical and histological similarities between several entities which may lead to difficulty in reaching a diagnosis. However definitive diagnosis is fundamental in order to select an adequate therapeutic and surveillance strategy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hawryluk EB, Izikson L, English JC., 3rd Non-infectious granulomatous diseases of the skin and their associated systemic diseases: An evidence-based update to important clinical questions. Am J Clin Dermatol. 2010;11:171–81. doi: 10.2165/11530080-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 2.Cioc AM, Frambach GE, Magro CM. Light-chain-restricted plasmacellular infiltrates in necrobiosis lipoidica - A clue to an underlying monoclonal gammopathy. J Cutan Pathol. 2005;32:263–7. doi: 10.1111/j.0303-6987.2005.00303.x. [DOI] [PubMed] [Google Scholar]
- 3.Ito Y, Nishimura K, Yamanaka K, Hakamada A, Isoda K, Kurokawa I, et al. Necrobiotic xanthogranuloma with paraproteinemia; An atypical case. J Dtsch Dermatol Ges. 2008;6:40–3. doi: 10.1111/j.1610-0387.2007.06392.x. [DOI] [PubMed] [Google Scholar]
- 4.Herd TJ, Fischer R, Christensen LC, Rajpara A. Irregular yellow-brown plaques on the trunk and thighs. Cutis. 2018;101:12;5. [PubMed] [Google Scholar]
- 5.Hilal T, DiCaudo DJ, Connolly SM, Reeder CB. Necrobiotic xanthogranuloma: A 30-year single-center experience. Ann Hematol. 2018;97:1471–9. doi: 10.1007/s00277-018-3301-1. [DOI] [PubMed] [Google Scholar]
- 6.Ugurlu S, Bartley GB, Gibson LE. Necrobiotic xanthogranuloma: Long-term outcome of ocular and systemic involvement. Am J Ophthalmol. 2000;129:651–7. doi: 10.1016/s0002-9394(99)00469-9. [DOI] [PubMed] [Google Scholar]
- 7.Reid SD, Ladizinski B, Lee K, Baibergenova A, Alavi A. Update on necrobiosis lipoidica: A review of etiology, diagnosis, and treatment options. J Am Acad Dermat. 2013;69:783–91. doi: 10.1016/j.jaad.2013.05.034. [DOI] [PubMed] [Google Scholar]
- 8.Pokharel A, Koirala IP. Necrobiotic granuloma: An update. Indian J Dermatopathol Diagn Dermatol. 2018;5:27–33. [Google Scholar]
- 9.Ziemer M, Norgauer J, Simon JC, Koehler MJ. An unusual histologic variant of necrobiotic xanthogranuloma. Am J Dermatopathol. 2012;34:e22–6. doi: 10.1097/DAD.0b013e3182222aa8. [DOI] [PubMed] [Google Scholar]
- 10.Mohan H, Bal A, Dhami GP. Non-infectious granulomatous dermatitis: A clinicopathological study. J Cutan Pathol. 2006;33:767–71. doi: 10.1111/j.1600-0560.2006.00566.x. [DOI] [PubMed] [Google Scholar]
- 11.Gibson LE, Reizner GT, Winkelmann RK. Necrobiosis lipoidica diabeticorum with cholesterol clefts in the differential diagnosis of necrobiotic xanthogranuloma. J Cutan Pathol. 1988;15:18–21. doi: 10.1111/j.1600-0560.1988.tb00509.x. [DOI] [PubMed] [Google Scholar]


