Abstract
Background:
Chronic venous leg ulcers are difficult to treat and recurrences are common. Among various modalities of treatment, platelet-rich fibrin (PRF) has shown promising results in ulcer healing by providing necessary growth factors. Unna's paste dressing has also proven to enhance wound healing.
Aim:
The aim of this study is to compare the efficacy of autologous PRF versus Unna's paste dressing in chronic venous leg ulcer patients and to compare the mean reduction in ulcer area at the end of 4 weeks.
Materials and Methods:
Twenty patients with chronic venous leg ulcers were randomly divided into two groups. Group 1: Patients received PRF dressing which was repeated every week for 4 weeks. Group 2: Patients received Unna's paste dressing once a week for 4 weeks. The ulcer size was assessed with the help of photographs, and ulcer area was measured.
Results:
The mean reduction in the area of the ulcer size in the PRF group was 86.03% and in the Unna's paste group was 71.97%, which was not statistically significant with a P value of 0.223.
Conclusion:
We conclude that though there was no statistical significance between the groups, PRF showed a significant reduction in ulcer size.
Keywords: Platelet-rich fibrin, Unna's paste, venous leg ulcer
Introduction
Venous ulcers are the most common cause of chronic leg ulcers. The chronicity and high recurrence rate of venous ulcer are the two fundamental factors causing grave impact on patients’ well-being.[1] One of the reasons for chronicity of the ulcer has been attributed to lack of growth factors and nutrients which are essential for wound healing.
A major revolution in the treatment of leg ulcer is cellular therapy, where the patient's own blood is used, which contains various cytokines and growth factors. Platelet-derived products such as platelet-rich fibrin (PRF) have shown promising results in wound healing.
Another dressing for chronic leg ulcer is zinc oxide paste (Unna's paste). It has re-epithelialization and anti-inflammatory properties which can enhance wound healing. Hence, we conducted an open-label randomized study to compare the efficacy of PRF and Unna's paste dressing in chronic venous leg ulcers.
Materials and Methods
A total of 20 patients were randomly divided into two groups based on the inclusion and exclusion criteria. Patients suffering from chronic venous ulcers of the lower extremity for more than 6 months, attending the outpatient department of Dermatology Venereology and Leprosy, and having an ulcer area of 1 cm × 1 cm to 5 cm × 5 cm were included in the study.[2] A thorough clinical examination and ultrasound venous Doppler were performed to confirm the diagnosis of venous ulcer. Ethical clearance was taken from the Institutional Ethics Committee.
Patients with ulcers of less than 6 months duration and of other etiology such as arterial ulcer, diabetic ulcer, neuropathic and vasculitic ulcers; patients with osteomyelitis affecting the area of the ulcer; patients with exposed tendons or bones; patients with infection; and patients receiving anticoagulants/antiplatelet drugs/bleeding diathesis were excluded from this study.
All patients in our study continued using compression stockings.
Preparation of platelet-rich fibrin
Procedure
After obtaining informed consent, 10 ml of the patient's blood was withdrawn into the vacutainer without any anticoagulant and immediately centrifuged (to prevent blood from clotting) at 3000 rpm for 15 mins. After 15 mins, a fibrin gel appears in the center of the vacutainer with red blood cells (RBCs) at the base and acellular plasma above. The PRF obtained was removed with the help of a toothed forcep and placed on the ulcer after removing the adherent RBCs. On an average, 10 ml of whole blood yields about 2.5 ml of the clot.[2]
Dressing procedure
Group 1: The measurements of the ulcer were taken. The PRF gel was then placed on the ulcer floor and covered with a sterile gauze piece (primary dressing), which was, in turn, covered with a sterile gauze pad (secondary dressing) held in place with a sterile roller bandage. The dressing was removed after 1 week. This treatment was repeated every week for 4 weeks.[2]
Preparation of Unna's paste
Procedure
Sixty grams of zinc oxide was mixed with 100 ml of glycerine and stirred well. This mixture was heated for 10–20 mins.
Dressing procedure
The measurements of the ulcer were taken. Ulcers were covered with a gauze impregnated with Unna's paste which was in turn covered with a sterile gauze-pad followed by a sterile roller bandage. This dressing was left in place for 1 week. This treatment was repeated every week for 4 weeks.
Measurements documentation
The greatest length and the greatest breadth were measured using a thread and a scale (the clock face method). This was done before starting the treatment, before repeating the treatment each time at weekly intervals, and after the treatment was completed (the final measurement). Digital photographs in both groups were taken before starting the treatment and after the treatment was completed.[2]
Results
A total of 20 patients enrolled in the study met the inclusion and exclusion criteria. The result was assessed on the basis of the ulcer area reduction. The mean reduction in the ulcer area in the PRF group was 7.50% after the 1st week, 35.04% after the 2nd week, 62.23% after the 3rd week, and 86.03% after the 4th week [Table 1]. However, in the Unna's paste group, the mean reduction in the ulcer size was 14.80%, 29.57%, 56.16%, and 71.97%, respectively [Table 2]. The overall mean reduction in the ulcer area was 86.03% in the patients treated with PRF dressing compared to 71.97% in the patients treated with Unna's paste dressing [Figure 1]. There was a complete closure of the ulcer in four patients (40%) in the PRF group [Figure 2a and b; 3a and b]. There was no case of complete closure of the ulcer in the Unna's paste group [Figure 4a and b; 5a and b].
Table 1.
Patients treated with PRF dressing
| Sr. no of patients | Initial measurement of ulcer size (cm2) | Measurement of ulcer size after 1st week (cm2) | Measurement of ulcer size after 2nd week (cm2) | Measurement of ulcer size after 3rd week (cm2) | Final measurement of ulcer size (cm2) | Percentage of improvement |
|---|---|---|---|---|---|---|
| 1 | 4.76 | 4 | 3.84 | 3.68 | 2.8 | 41.17% |
| 2 | 0.96 | 0.96 | 0.8 | 0.25 | 0 | 100% |
| 3 | 5.25 | 5 | 3.96 | 3.6 | 1.84 | 64.95% |
| 4 | 3.5 | 3.5 | 2 | 1.125 | 0.5 | 85.71% |
| 5 | 1.25 | 1.25 | 0.75 | 0.5 | 0.25 | 80% |
| 6 | 2.4 | 2.2 | 1 | 0.25 | 0 | 100% |
| 7 | 5.72 | 5.5 | 3.5 | 1.25 | 0.5 | 91.25% |
| 8 | 8.9 | 5.6 | 3.97 | 3 | 0.25 | 97.19% |
| 9 | 5.8 | 5.5 | 3.8 | 1.15 | 0 | 100% |
| 10 | 10.5 | 10.5 | 8.4 | 5 | 0 | 100% |
| Mean % of improvement | 0 | 7.50% | 35.04% | 62.23% | 86.03% | 86.03% |
Table 2.
Patients treated with Unna’s paste dressing
| S. no of patients | Initial measurement of ulcer size (cm2) | Measurement of ulcer size after 1st week (cm2) | Measurement of ulcer size after 2nd week (cm2) | Measurement of ulcer size after 3rd week (cm2) | Final measurement of ulcer size (cm2) | Percentage of improvement |
|---|---|---|---|---|---|---|
| 1 | 10 | 9 | 5.4 | 3.75 | 1 | 90% |
| 2 | 0.25 | 0.25 | 0.15 | 0.1 | 0.06 | 76% |
| 3 | 6.75 | 6.5 | 1 | 0.3 | 0.3 | 95.55% |
| 4 | 3.75 | 3.5 | 3.45 | 2.64 | 3.23 | 13.86% |
| 5 | 5 | 4.75 | 4.4 | 3.23 | 0.25 | 95% |
| 6 | 13.5 | 12.5 | 8.4 | 5 | 2 | 85.18% |
| 7 | 13.5 | 12.5 | 9 | 5.6 | 0.5 | 96.29% |
| 8 | 22.5 | 20.5 | 15.6 | 9 | 3 | 86.66% |
| 9 | 5 | 3.75 | 5 | 5.75 | 3 | 40% |
| 10 | 2.55 | 2.55 | 2.25 | 1.5 | 1.5 | 41.17% |
| Mean % of improvement | 0 | 14.80% | 29.57% | 56.16% | 71.97% | 71.97% |
Figure 1.
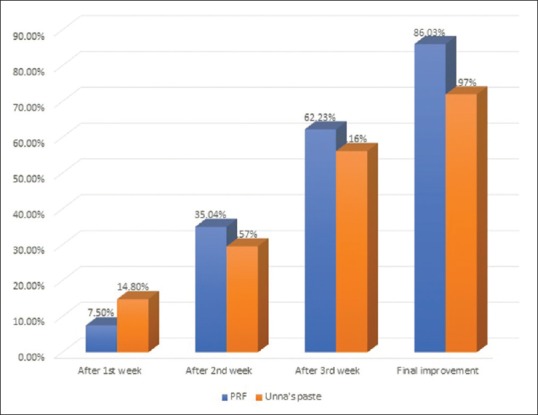
Bar diagram showing percentage of size reduction with platelet-rich fibrin and Unna's paste dressing
Figure 2.
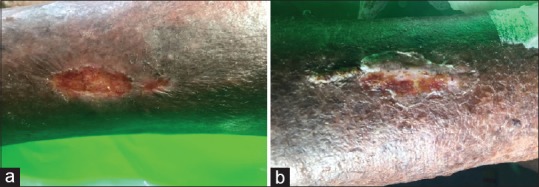
(a) Patient 1: A 54-year-old female with a venous ulcer over the left leg before treatment with platelet-rich fibrin dressing; (b) 80% improvement after 4 weeks of treatment with platelet-rich fibrin dressing
Figure 3.
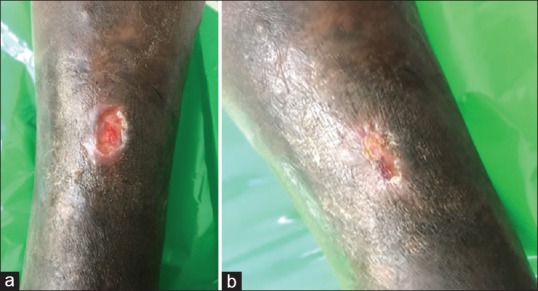
(a) Patient 2: A 62-year-old male presented with an ulcer over the right leg before treatment with platelet-rich fibrin dressing, (b) showing complete closure after 4 weeks of treatment with platelet-rich fibrin dressing
Figure 4.

(a) Patient 3: A 50-year-old female with an ulcer over the right leg before treatment with Unna's paste dressing; (b) 90% improvement after 4 weeks of treatment with Unna's paste dressing
Figure 5.
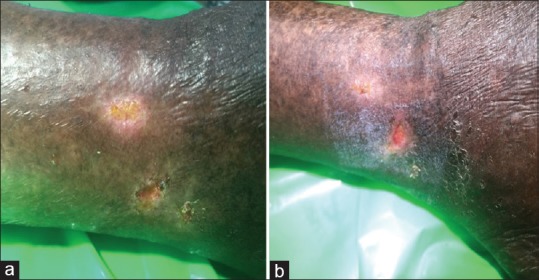
(a) Patient 4- 49-year-old male with ulcer near right lateral malleolus before treatment with Unna's paste dressing, (b) showing 70% improvement after 4 weeks of treatment with Unna's paste dressing
Statistical analysis using independent t-test and Chi-square test showed no significant reduction of the ulcer size between both groups [Table 3].
Table 3.
Statistical analysis
| Variables | No. of Patients | Mean | Std. Deviation | P |
|---|---|---|---|---|
| PRF | 10 | 86.03 | 19.510 | 0.223 |
| Unna’s paste | 10 | 71.97 | 29.358 |
Discussion
Wound healing is a complicated process which involves a cascade of events such as clotting, neutrophil chemotaxis, epithelialization, angiogenesis, and scar formation. Any interruption in these events leads to failure of wound closure whereby an acute wound is converted to a chronic one. Chronic ulcers are difficult to treat.[3] Therefore, an ideal dressing which offers nutritional support has a significant impact on wound repair leading to complete closure of the wound.
PRF offers the growth factors necessary for wound healing, and have been used in various fields of medicine and surgery. The derived PRF acts as a biodegradable scaffold for cell migration, proliferation, and differentiation, and delivers growth factors.[4] Platelets trapped within the three-dimensional mesh ensures slow and continuous release of growth factors over time which lasts until the 28th day.[5] Various growth factors such as platelet-derived growth factor help in angiogenesis, neutrophilic chemotaxis, and collagen synthesis; transforming growth factor-beta helps in regulating fibroblast proliferation and deposition of bone matrix; insulin-like growth factor-1 and fibroblast growth factor enhance proliferation and differentiation of osteoblast and activate protein synthesis; vascular endothelial growth factor aids angiogenesis and endothelial cell migration; epidermal growth factor exerts collagen secretion and epithelial mitogenesis; and connective tissue growth factor helps in cartilage regeneration.[6,7]
Unna's paste dressing has a dual action, one by its anti-inflammatory and antibacterial action and offers graded compression.
Various studies with PRF and Unna's paste dressing for chronic venous leg ulcers have shown good results.
A randomized controlled trial conducted by Somani et al.[2] compared the efficacy of PRF and saline dressing in chronic venous leg ulcers concluded that the mean reduction in the area of the ulcer size in PRF group was 85.51% and in the saline group was 42.74% which was statistically significant.
Similarly in another randomized controlled study, Goda[8] compared PRF dressing and conventional dressing for venous ulcers. He concluded that the mean percentage of wound reduction was higher in the PRF group than the control group which was statistically significant.
A randomized double-blinded study was conducted by Stromberg and Agren[9] to compare the efficacy of local zinc oxide gauze compress and a placebo. It showed 83% improvement in the zinc oxide group when compared to the placebo group which showed only 42% improvement. Therefore, they concluded that zinc oxide accelerates wound healing.
A case series by Parboteeah and Brown[10] concluded that zinc paste therapy along with compression bandage is more efficacious in the treatment of venous leg ulcers that are difficult to treat with other therapies.
Luz et al.[11] conducted a study wherein 43 venous ulcer patients were randomized into two groups. Out of 43 patients, 32 patients in Unna's boot group showed a significant reduction in the ulcer when compared to 11 patients in the control group who received simple dressing. They concluded that though there was no statistical significance between the groups, Unna's boot group showed better improvement at the end of 3 months.
Conclusion
In conclusion, the reduction in ulcer size was better in PRF group (86.03%) when compared to Unna's paste group (71.97%), but it was not statistically significant. PRF dressing is simple, cost-effective, and patient-friendly. However, the sample size was small and so large-scale studies are needed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Vasudevan B. Venous leg ulcers: Pathophysiology and classification. Indian Dermatol Online J. 2014;5:366–70. doi: 10.4103/2229-5178.137819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Somani A, Rai R. Comparison of efficacy of autologous platelet-rich fibrin versus saline dressing in chronic venous leg ulcers: A randomized controlled trial. J Cutan Aesthet Surg. 2017;10:8–12. doi: 10.4103/JCAS.JCAS_137_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ashcroft GS, Jeong MJ, Ashworth JJ, Hardman M, Jin W, Moutsopoulos N, et al. Tumor necrosis factor-alpha (TNF-α) is a therapeutic target for impaired cutaneous wound healing. Wound Repair Regen. 2012;20:38–49. doi: 10.1111/j.1524-475X.2011.00748.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borie E, Oliví DG, Orsi IA, Garlet K, Weber B, Beltrán V, et al. Platelet-rich fibrin application in dentistry: A literature review. Int J Clin Exp Med. 2015;8:7922–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Chignon-Sicard B, Georgiou CA, Fontas E, David S, Dumas P, Ihrai T, et al. Efficacy of leukocyte-and platelet-rich fibrin in wound healing: A randomized controlled clinical trial. Plast Reconstr Surg. 2012;130:819–29. doi: 10.1097/PRS.0b013e31826d1711. [DOI] [PubMed] [Google Scholar]
- 6.Raja VS, Naidu EM. Platelet rich fibrin: Evolution of a second-generation platelet concentrate. Indian J Dent Res. 2008;19:42–6. doi: 10.4103/0970-9290.38931. [DOI] [PubMed] [Google Scholar]
- 7.Hotwani K, Sharma K. Platelet rich fibrin-a novel acumen into regenerative endodontic therapy. Restor Dent Endod. 2014;39:1–6. doi: 10.5395/rde.2014.39.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goda AA. Autogenous leucocyte-rich and platelet-rich fibrin for the treatment of leg venous ulcer: A randomized control study. Egypt J Surg. 2018;37:316–21. [Google Scholar]
- 9.Stromberg HE, Agren MS. Topical zinc oxide treatment improves arterial and venous leg ulcers. Br J Dermatol. 1984;111:461–8. doi: 10.1111/j.1365-2133.1984.tb06610.x. [DOI] [PubMed] [Google Scholar]
- 10.Parboteeah S, Brown A. Managing chronic venous leg ulcers with zinc oxide paste bandages. Br J Nurs. 2008;17:S30. doi: 10.12968/bjon.2008.17.Sup3.28913. S32, S34-6. [DOI] [PubMed] [Google Scholar]
- 11.Luz BS, Araujo CS, Atzingen DA, Mendonca AR, Filho MM, Medeiros ML. Evaluating the effectiveness of the customized Unna boot when treating patients with venous ulcers. An Bras Dermatol. 2013;88:41–9. doi: 10.1590/S0365-05962013000100004. [DOI] [PMC free article] [PubMed] [Google Scholar]


