Abstract
Elderly with dementia or cognitive impairment are at increased risk of poor oral health. Oral health education programs targeting carers may be an effective strategy to improve oral hygiene. The aim of this review was to assess the effectiveness of oral health education programs for carers on the oral hygiene of elderly with dementia. A literature search was performed to identify studies published in five electronic databases (PubMed, MEDLINE, EMBASE, CINAHL, and PsycINFO), without time and language restrictions. Two independent coders extracted data and assessed the risk of bias for each included study. Of the 243 studies, only four studies met the inclusion criteria. All four studies reported a significant improvement for some oral health measures in dementia elderly following a carer oral health education program. The included studies did not report any other relevant outcomes of interest for this review. This review identifies limited evidence for a carer oral health education as an efficient means to improve oral health in dementia elderly. The review also clearly highlights the need for well-designed, high-quality studies with more relevant outcome measures to better address this knowledge gap.
Keywords: Carer, dementia, education, elderly, geriatric, oral hygiene, review
INTRODUCTION
With advancements in health care, a significant number of people are living longer and leading healthier lives. On the contrary, a rise in the burden of noncommunicable diseases, particularly dementia is witnessed. The incidence of dementia is nearly 7.7 million/year worldwide, implying one new case every 4 seconds.[1] The estimate of people worldwide living with dementia in 2010 was 35.6 million, and this is expected to triple by 2050, with the world's aging population.[2]
The retention of natural teeth associated with longer life expectancy has contributed to an increased occurrence of oral diseases in the general elderly and to a greater extent in functionally dependent older adults.[3] Elderly with dementia often present with greater burden of oral diseases, with the prevalence of the latter more so evident in the advanced stages of the condition. Evidence demonstrates a higher incidence of dental caries, periodontal disease, increased pain, and other related dental problems in dementia.[4,5,6,7,8] In addition, oral health problems can have a serious impact on many aspects of general health including nutrition, life expectancy, and overall quality of life (QoL).[9]
Previous studies emphasize the focus of dental interventions in elderly on early diagnosis and prevention of oral diseases.[10,11,12,13] As dementia is a progressive condition, individuals face multiple issues with respect to attaining positive oral health and performing adequate oral hygiene and become increasingly dependent on their carers. It is therefore of great importance to make carers aware of the potential benefits associated with the maintenance of good oral health and the risks associated with poor oral hygiene, as they represent the primary oral care providers. Though carers address many of the issues related to the overall health, vast oral health care needs are often unmet.
It is therefore of considerable concern that empirical studies have generally found that carers fail to understand the importance of oral health.[14,15,16,17] This has been attributed to limited knowledge and understanding as well as psychological barriers associated with providing oral health assistance to others. Another complicating factor is that dementia is often associated with behavioral problems such as aggression and combativeness, which may make it more difficult for the carers to provide oral care, and in the longer term, contribute to oral neglect and resultant diseases.[18] Because dementia is heterogeneous in its presentation, effective intervention will require dental professionals to work together within a broader interdisciplinary and multidisciplinary framework, where the goal of promoting oral health extends beyond the elimination of oral disease and instead focuses on promoting gains in oral health that have the potential to improve patient well-being and overall QoL.[19,20]
There is now clear evidence that oral health can be improved through carers' education in general elderly people, with studies showing improved oral hygiene, less gingivitis, a reduced prevalence of denture stomatitis, and improved denture hygiene.[13,21,22,23] Instruction on oral health care, its association with infectious disease, and other degenerative diseases have shown to improve the attitude of caregivers toward the importance of oral health.[13] Furthermore, improvements in the oral health of elderly residents have been linked to a reduced incidence of pneumonia.[13] To consolidate these findings, a recent systematic review concluded that oral health education for caregivers might be effective for improving the oral health of elderly.[24] This advocates dental professionals to develop a therapeutic relationship and positive rapport, not only with elderly with dementia but also with their carers by engaging and educating them to achieve successful long-term goals in attaining improved oral care.[19,20]
With rising oral care needs and for future planning and development of oral health interventions appropriate, it is important to identify the role of these carers in the oral health management of elderly with dementia. This systematic review aims to report available evidence on effectiveness of oral health education programs for carers on the oral hygiene of elderly with dementia. It may help to advocate policies to implement measures for definitive carer education on oral hygiene measures, if found to have beneficial effects toward improved oral health status of elderly with dementia.
MATERIALS AND METHODS
This review was conducted and reported in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.[25]
Search strategy and criteria
The following electronic databases were searched for identification of potential studies (Cochrane Library [Central], PubMed, MEDLINE, EMBASE, CINAHL, PsycINFO). An initial online search was performed using the search terms that were carefully identified in accordance to the stated PICO question [provided in Supplementary Table S1]. The search terms used were either medical subject headings terms or identical terms/keywords. The search terms were then combined with an “OR” and PICO categories were combined using “AND” to create a final logic search query. This query was then run in the above-mentioned databases, with adjustments made to suit specific databases to yield the results. In addition, hand searches and bibliographies of included articles were scanned manually to identify any additional relevant publications.
Table S1.
Focus question, search terms, search filters, and search dates
| Focus question | Are oral health education programs for carers effective in improving the oral hygiene status of elderly with dementia? |
|---|---|
| Search terms | #1: Mesh - dental health OR oral care OR dental care OR mouth care OR dental hygiene OR mouth hygiene |
| #2: Mesh - dementia OR Alzheimer OR Alzheimer’s OR cognitive impairment | |
| #3: Mesh - education OR intervention OR program OR promotion | |
| #4: Mesh - caregiver OR caregivers OR carer OR nurse OR care aide OR health care aide | |
| Search strategy | #1 AND #2 AND #3 AND #4 |
| Filters | Language: Not applied |
| Species: Humans (Mesh) | |
| Ages: Aged (Mesh) | |
| Search date | Final confirmatory online search was performed on March 31, 2018 |
Eligibility criteria
We included all human studies, irrespective of the study design to maximize the study pool, which evaluated oral health of elderly with dementia before and after a carer oral health education program. The elderly could be living in the community or residential aged care facilities. Studies excluded were (i) those involving oral health education for carers of elderly having conditions other than dementia, (ii) educational interventions/programs only for elderly with dementia, and (iii) non-English articles.
Study selection and data extraction
All titles retrieved were exported to Endnote (version X9) and duplicates removed. One of the authors screened the titles of the searched record to exclude obviously irrelevant articles. Full texts of potentially eligible studies meeting the criteria were obtained and included for review. Personal communications were sent to the author(s) where required. Data was extracted using piloted forms. The extracted data consisted of information on design characteristics, follow-up period, intervention, outcome evaluation, and critical findings. Where discrepancies between authors occurred consensus was reached through discussion. The Cochrane's risk of bias tool was used for assessing the methodological quality of the included studies.[26]
Summary measures
The primary outcome was to evaluate improvement in oral hygiene of elderly with dementia before and after an oral health education program for carers. Any clinical outcome measure (e.g., dental plaque, dental caries, and periodontal status) used to assess/evaluate oral hygiene was considered. Secondary outcome included for assessment comprised: (i) oral health-related knowledge, attitude and practices of carers before and after an oral health education program.
RESULTS
Literature identified
The original search identified 243 articles, of which two studies were identified by screening the reference list of the included studies. After removing duplicates, 236 unique articles remained. A further 227 articles were excluded based on screening of titles and abstract. Full-text review of nine articles indicated that four studies[27,28,29,30] met the inclusion criteria. Two of the five excluded studies were in foreign languages, German[31] and Korean,[32] respectively. Of the remaining studies excluded, one study[33] described the caregiver's perception and its importance in dementia patients. Another study reported oral health behavior and sociodemographic profile of individuals with Alzheimer's disease from the perspective of family caregivers.[34] Neither of these studies had an educational program for their carers nor evaluated the oral health of patients with dementia.[33,34] One article excluded was a review protocol.[18] The results of the screening and search process is presented in Figure 1.
Figure 1.
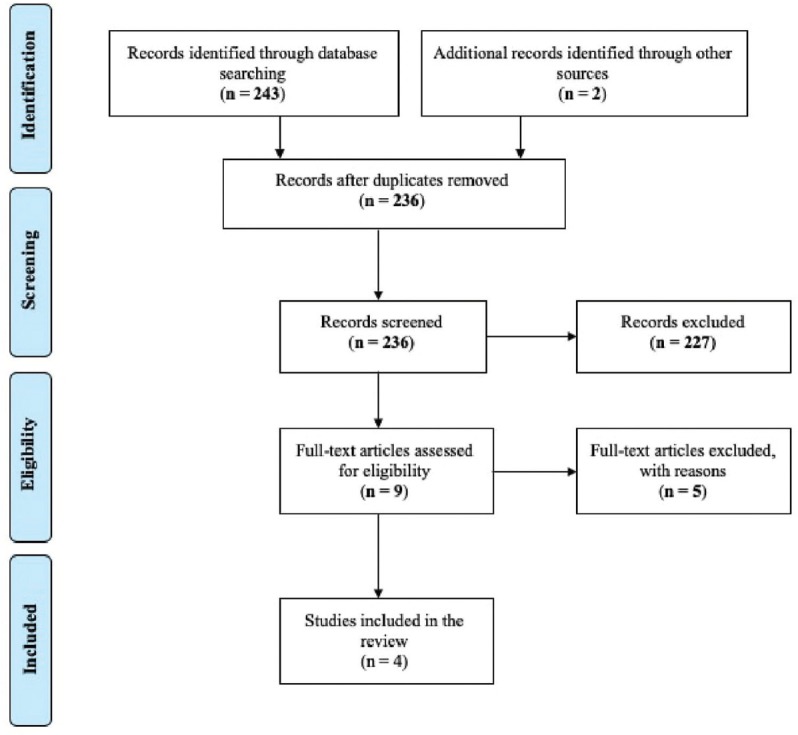
Adapted preferred reporting items for systematic reviews and meta-analysis diagram illustrating the study selection process.
Common study characteristics and quality assessment
A summary of each included article is summarized in Table 1. Among the four contributing studies, two studies[28,29] employed a longitudinal cohort design, one a quasi-experimental[27] and another a controlled clinical trial.[30] All studies were based in care homes or nursing homes, with majority (three of the four) conducted in Europe. Nursing staff and carers formed target groups as recipients of educational intervention. The number of carers in the studies varied from 14 to 87. Precisely, in one study only, full-time formal carers were included.[29] The sample size of the elderly residents ranged from 40 to 219, with females as majority. Cognitive status was established using the Mini-Mental State Examination[35] in two studies.[29,30] For the remaining two studies, one used medical records,[28] and another obtained information from nurses of the related participants.[27] Only two studies[28,30] reported the level of care needed, using Barthel index.[36]
Table 1.
Characteristics of included studies
| Study (Year) | Design and follow-up | Study location and population | Intervention | Duration of intervention and educator | Outcome measures | Risk of Bias |
|---|---|---|---|---|---|---|
| Samson et al. (2009) | Quasi-experimental At 3 months and after 6 years | Norway Nursing home residents Sample size: n=88 (n=52; residents presented with dementia manifestations at end of the follow-up) Mean age: NR Female (%): NR |
Nursing staff received oral health education composed of theoretical and practical components Intervention also included Motivational training Introduction of picture based cards for oral care delivery Distribution of oral hygiene aids Appointed an “oral-care contact” for each ward Routine oral hygiene checks and feedbacks provided |
4 h course Provided through a dentist, dental hygienist and competent nursing staff | MPI | High |
| Zenthofer et al. (2016) | Longitudinal cohort After 6 months | Germany Care homes Sample size: n=93 (n=33; residents with dementia, n=60; residents without dementia) Mean age: 82.9 years (SD 9.9) Female (%): 65 |
Lecturers provided information on: (i) age-related oral changes and diseases, (ii) strategies to improve oral health, and (iii) feasible brushing techniques and effective handling of oral hygiene aids Practical demonstration on use of oral hygiene aids and handling of removable dentures Hands on training to help evaluate oral hygiene using ROAG and perform denture hygiene care Implementation of ultrasonic baths for denture cleaning |
2-day oral care training programme Provided through a dentist | PCR, GBI, CPITN and DHI | High |
| Zenthofer et al. (2016) | Controlled clinical trial After 6 months | Germany Nursing home residents Sample size: n=219 (IG=144, CG=75) Mean age: 83.1 years (SD 9.0) Female (%): 68.5 |
Lecturers provided information on: (i) age-related oral changes and diseases, (ii) strategies to improve oral health, and (iii) feasible brushing techniques and effective handling of oral hygiene aids Practical demonstration on use of oral hygiene aids and effective handling of removable dentures Hands on training to help evaluate oral hygiene using ROAG and perform denture hygiene care Implementation of ultrasonic baths for denture cleaning |
2-day oral care training programme Provided through a dentist | PCR, GBI, CPITN and DHI | Low |
| Lago et al. (2017) | Longitudinal study At 6, 12, 18 and 24 months | Brazil Institutionalized elderly Sample size: n=40 Mean age: 82.3 years (SD-NR) Female (%): 52.5 |
Oral health education Practical demonstrations | Monthly lectures | GPI, TD and TC | High |
MPI: Mucosal Plaque Index; PCR: Plaque control record; GBI: Gingival Bleeding Index; CPITN: Community periodontal index of treatment need; DHI: Denture Hygiene Index; GPI: Global Plaque Index; TD: Tongue discoloration; TC: Tongue coating; NR: Not reported; SD: Standard deviation; ROAG: Revised Oral Assessment Guide; IG: Intervention group; CG: Control group
The oral health educational interventions focused mainly on delivering information to carers on oral health and hygiene practices, and the contents of the intervention varied widely across each study. The teachers of the program ranged from dentists, dental hygienists to trained nursing staff. All of the intervention programs consisted of more than one component, with lectures and some form of practical training. In all but one study, carers were exposed to educational sessions related to various themes of oral health.[29] Of the four studies, only three reported the mode of presentation and provided handouts with information to carers for further reading after the program.[28,29,30] With the exception of all, carers of two studies[28,30] underwent further training toward effective handling of removable dentures and use of the Revised Oral Assessment Guide for oral hygiene evaluation. While most studies delivered some form of oral hygiene aids, the intervention program of Zenthöfer et al. provided ultrasonic baths to nursing homes' residents for denture cleaning.[28,30] Moreover, in the controlled trial,[30] training was provided to 25 professional carers selected from the participating interventional homes in leading positions to act as multipliers to provide information and training to their colleagues. The follow-up of the included studies varied from 6 months to 2 years. No studies reported any information on characteristics of the carers. Three studies[27,28,29] reported high risk of bias. The Zenthöfer et al.[30] study used a controlled trial design and hence had a low risk of bias [Table 2].
Table 2.
Quality (risk of bias) of included studies
| Studies | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Samson et al.[27] | − | − | − | − | + | + | − |
| Zenthöfer et al.[28] | − | − | − | − | − | + | − |
| Zenthöfer et al.[30] | + | + | + | − | + | + | − |
| Lago et al.[29] | − | − | − | − | − | + | − |
+: Low risk of bias; −: High risk of bias; ?: Unclear risk of bias
Characteristics of individual studies included
Samson et al.[27] investigated the long-term effect of an oral health care program on the oral hygiene of elderly residents at a nursing home. Mucosal Plaque Score (MPS) was used to index oral hygiene at baseline, 3 months, and at the end of 6 years. MPS significantly improved after 3 months, with this being consistent until the end of the study. Participants who manifested with dementia had better oral hygiene than those with uncertain cognitive impairment at the end of 6 years.
The aim of two studies[28,30] by Zenthöfer et al. was to evaluate the potential effects of an oral health care education for carers on the oral health of elderly with dementia. In both the studies, oral hygiene assessment was primarily through measurement of dental plaque, gingival inflammation, periodontal status, and denture hygiene. Dental plaque and gingival inflammation were evaluated using the plaque control record[37] and gingival bleeding index.[38] The community periodontal index of treatment needs (CPITN)[39] and denture hygiene index[40] was used to report the periodontal and denture hygiene status, respectively.
The first article[28] reports oral and denture hygiene among institutionalized older people with and without dementia following a career oral health education program. Summarizing the results, a significant improvement was seen in denture hygiene, gingival bleeding, and CPITN scores in the dementia group at the end of 6 months. However, for dental plaques scores, no significant difference was observed between the groups of participants (with and without dementia) following the intervention. Further, on adjusted findings, no significances sustained. The second article[30] reports the effectiveness of carer education on oral and denture hygiene on the oral health of cognitively impaired elderly compared to a control group. Fourteen nursing homes were randomly allocated to an intervention and control group. Participants were evaluated at baseline and the end of 6 months for changes in oral and denture hygiene measures. No oral care was provided to the control group. Dental plaque and denture hygiene scores significantly reduced in the intervention group compared to the control group at follow-up. On the contrary, gingival index and CPITN scores remained unchanged in both the groups. The results were identical on adjusted findings.
Lago et al.[29] aimed to evaluate the impact of an oral health education program for carers of institutionalized elderly in Brazil. Improvements in oral hygiene were indexed using the global plaque index and with changes in tongue discoloration and tongue coating. In addition, carers' knowledge on oral health was assessed. Changes in carer knowledge and oral hygiene of the participants were evaluated at 6, 12, 18, and 24 months after baseline. A statistically progressive reduction in plaque and tongue coating scores were evident, with changes evident as early as within 6 months. Furthermore, a concomitant increase in number of participants without tongue discoloration and a significant change in carers' knowledge were reported following the oral health education program.
DISCUSSION
To our understanding, this is the first review that aimed to provide cumulative evidence from empirical research on the potential effect of oral health education intervention for carers on oral hygiene of dementia elderly. Oral health problems are increasingly common in dependent elderly and in those suffering from neurodegenerative diseases.[41] With the prevalence of dementia on the rise and the need to improve oral health, the role of nondental professionals can be of great predominance. Over the years, a substantial literature has emerged on studies evaluating the effectiveness and describing the importance of oral health education in a variety of settings.[34] This review was only able to identify limited information, on oral health intervention for carers concerning this population. Taken together from all the included studies, it was evident that the oral health of people with dementia improved significantly following a carer oral education program.
Carers commonly cite lack of motivation and psychological barriers as common reasons for poor oral care delivery.[18] Only one study in this review motivated nursing staffs to provide oral care as part of the oral health program. This could be a contributing factor to good oral care delivery, with the results of the study being reflective.[27] Hence, it is vital that carers be motivated and provided with effective evidence-based strategies to overcome associated barriers and increase facilitation contributing to improved oral hygiene in the long term.
Denture hygiene practice reflected significant changes with the use of ultrasound baths.[28,30] This is important from a clinical perspective because research has shown strong associations between denture plaque and pneumonia; and on the other hand, care-dependent multimorbid older people are especially prone to diseases such as bacteremia because of their reduced immune status.[41,42,43,44] The latter highlights the strong evidence and advocates the need for ultrasound bath in nursing homes as an effective and standard means to improve denture hygiene in dementia elderly. It is of concern that none of the studies[27,28,29,30] discussed the role of an underlying theory or provided an empirical evidence base for the use of these specific interventions. Although these interventions provided improved oral hygiene, no intervention could be considered the most effective. Future carer interventions are required to be developed with multiple components to include strategies to deal with and tackle complex behavioral and psychological barriers often associated with dementia elderly.[45] Currently, no much information exists with interventions focusing on these components together and regarding the type of oral health training thought to be useful in training carers concerning oral care in elderly with dementia.
The studies[27,28,29,30] reported data on short-term and long-term effects on oral health following the oral health education intervention for carers. It may be appropriate for outcomes such as dental plaque, denture hygiene, gingivitis, tongue discoloration, and tongue coating to manifest changes. However, follow-up is inadequate for outcomes such as for periodontal status assessed,[28,30] which requires a relatively long time for the effects to manifest in the oral cavity. Further to this, no support was given to manage the periodontal conditions, during the intervention period. This might provide the reason for no significant changes in the controlled trial for periodontal status (CPITN scores) between the participants of the control and intervention at the end of follow-up.[30] Previous studies reports elderly with dementia suffer from a considerable amount of decay.[46] In the current review, no studies reported findings regarding the presence or absence of dental caries. The associated pain arising from dental decay has shown to have a significant impact on the oral health[47] and hence needs consideration.
Qualitative studies have shown carers lack the knowledge and training to provide oral care for the general elderly.[48] Sustainable effects on knowledge, attitudes, and practices of carers demand consideration in any intervention before and after implementing it into practice. Only one study aimed to capture the knowledge of carers on oral health. The findings revealed carers possessed limited knowledge and expressed interest in obtaining further information.[29] None of the included studies evaluated carers' attitude and existing practices of oral hygiene in elderly with dementia. It is important for future studies to consider this to facilitate better understanding and to identify common misconceptions, which may help in developing an effective intervention focused on addressing the oral needs of elderly with dementia better. In addition, no studies reported whether the carers had any previous oral health care training. It is to consider the fact that these measures could have an impact on the efficacy of the intervention. The findings of this study were similar to another review evaluating the evidence on oral health education for caregivers of elderly, which found limited evidence.[24] None of the included studies assessed precisely measures of secondary outcomes considered in this review.
Future studies require consideration of designs that are more stringent and include range of standardized measures to evaluate oral hygiene and cognition. Studies with longer follow-ups and carers of all types providing care are to be included, as the role of these carers can vary considerably based on the institution they provide care for. Majority of studies investigated the oral health of dementia elderly living in care homes or nursing homes. There exist a significant 70% of elderly with dementia who are homebound and depend on their family members for the provision of oral care. No studies to date have taken into consideration the oral care needs of community-dwelling elderly with dementia and evaluated interventions for family carers to improve oral hygiene in homebound elderly with dementia. There also exists insufficient evidence on the development of, piloting, and validation of an oral health education intervention explicitly developed for carers of dementia elderly. Therefore, there exists a need for the development of an evidence-based oral health intervention manual tailored to the specific needs of elderly with varying levels of cognitive impairment that could serve as a standard manual for carer education.
The review is not free from limitations and is acknowledged. First, it is possible that despite the comprehensive search, relevant articles were not captured. Second, the included studies used a range of cognitive and oral health measures to report outcomes. Finally, limited number and the considerable heterogenicity between the studies were too large to perform a meta-analysis.
CONCLUSION
To conclude, this review identifies that a carer oral health education intervention had a positive effect for few oral health measures in elderly with dementia. However, the findings drawn require careful interpretation owing to evidence from limited studies of questionable quality and methodological weakness. Further, well-designed studies are necessary to substantiate implementation of definitive carer oral health education and its beneficial aspects in the long term for dementia elderly.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or nonfinancial in this article.
Acknowledgements
The author (NM) would like to thank Dr. Bernadette McGuinness, Clinical Senior Lecturer, Centre for Public Health, Queen's University, Belfast, for her inputs to produce this thesis work as a part of the Master of Public Health (MPH) program.
REFERENCES
- 1.World Alzheimer's Report 2009. London: Alzheimer's Disease International; 2009. Neurological Disorders: Public Health Challenges. Geneva: World Health Organization; 2006. [Google Scholar]
- 2.Pahlavanzadeh S, Heidari FG, Maghsudi J, Ghazavi Z, Samandari S. The effects of family education program on the caregiver burden of families of elderly with dementia disorders. Iran J Nurs Midwifery Res. 2010;15:102–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Ornstein KA, DeCherrie L, Gluzman R, Scott ES, Kansal J, Shah T, et al. Significant unmet oral health needs of homebound elderly adults. J Am Geriatr Soc. 2015;63:151–7. doi: 10.1111/jgs.13181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dolan TA, Atchison KA. Implications of access, utilization and need for oral care by the non-institutionalized and institutionalized elderly in the dental delivery system In Oral Health and Primary Care. Integrating Dentistry into Health Care Reform Workshop The University of Iowa. 1993 [PubMed] [Google Scholar]
- 5.Jones JA, Lavallee N, Alman J, Sinclair C, Garcia RI. Caries incidence in patients with dementia. Gerodontology. 1993;10:76–82. doi: 10.1111/j.1741-2358.1993.tb00086.x. [DOI] [PubMed] [Google Scholar]
- 6.Ship JA. Oral health of patients with Alzheimer's disease. J Am Dent Assoc. 1992;123:53–8. doi: 10.14219/jada.archive.1992.0005. [DOI] [PubMed] [Google Scholar]
- 7.Rejnefelt I, Andersson P, Renvert S. Oral health status in individuals with dementia living in special facilities. Int J Dent Hyg. 2006;4:67–71. doi: 10.1111/j.1601-5037.2006.00157.x. [DOI] [PubMed] [Google Scholar]
- 8.Henry RG, Wekstein DR. Providing dental care for patients diagnosed with Alzheimer's disease. Dent Clin North Am. 1997;41:915–43. [PubMed] [Google Scholar]
- 9.Razak PA, Richard KM, Thankachan RP, Hafiz KA, Kumar KN, Sameer KM. Geriatric oral health: A review article. J Int Oral Health. 2014;6:110–6. [PMC free article] [PubMed] [Google Scholar]
- 10.Locker D, Matear D, Stephens M, Jokovic A. Oral health-related quality of life of a population of medically compromised elderly people. Community Dent Health. 2002;19:90–7. [PubMed] [Google Scholar]
- 11.Canadian Dental Association. Optimal Health for Frail Older Adults: Best Practices along the Continuum of Care. Ottawa, ON: Canadian Dental Association; 2009. [Google Scholar]
- 12.Chalmers JM. Minimal intervention dentistry: Part 1. Strategies for addressing the new caries challenge in older patients. J Can Dent Assoc. 2006;72:427–33. [PubMed] [Google Scholar]
- 13.Nicol R, Petrina Sweeney M, McHugh S, Bagg J. Effectiveness of health care worker training on the oral health of elderly residents of nursing homes. Community Dent Oral Epidemiol. 2005;33:115–24. doi: 10.1111/j.1600-0528.2004.00212.x. [DOI] [PubMed] [Google Scholar]
- 14.Khanagar S, Kumar A, Rajanna V, Badiyani BK, Jathanna VR, Kini PV. Oral health care education and its effect on caregivers' knowledge, attitudes, and practices: A randomized controlled trial. J Int Soc Prev Community Dent. 2014;4:122–8. doi: 10.4103/2231-0762.139843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frenkel H, Harvey I, Newcombe RG. Improving oral health in institutionalised elderly people by educating caregivers: A randomised controlled trial. Community Dent Oral Epidemiol. 2001;29:289–97. doi: 10.1034/j.1600-0528.2001.290408.x. [DOI] [PubMed] [Google Scholar]
- 16.Rabbo MA, Mitov G, Gebhart F, Pospiech P. Dental care and treatment needs of elderly in nursing homes in Saarland: Perceptions of the homes managers. Gerodontology. 2012;29:e57–62. doi: 10.1111/j.1741-2358.2010.00409.x. [DOI] [PubMed] [Google Scholar]
- 17.Reis SC, Marcelo VC, da Silva ET, Leles CR. Oral health of institutionalised elderly: A qualitative study of health caregivers' perceptions in Brazil. Gerodontology. 2011;28:69–75. doi: 10.1111/j.1741-2358.2010.00366.x. [DOI] [PubMed] [Google Scholar]
- 18.Yi Mohammadi JJ, Franks K, Hines S. Effectiveness of professional oral health care intervention on the oral health of residents with dementia in residential aged care facilities: A systematic review protocol. JBI Database System Rev Implement Rep. 2015;13:110–22. doi: 10.11124/jbisrir-2015-2330. [DOI] [PubMed] [Google Scholar]
- 19.Martin CR, Preedy VR. Diet and Nutrition in Dementia and Cognitive Disorders. 1st ed. Amsterdam: Elsevier; 2014. [Google Scholar]
- 20.Pynn T, Kolic J. Oral health and dementia: Obstacles, assessments, and management of patients with dementia Oral Health. 2014. [Last accessed on 2018 Oct 10]. p. 6. Available from: https://wwworalhealthgroupcom/features/oralhealth-and-dementia-obstacles-assessments- and-management-of-patients-with-dementia/
- 21.Ribeiro DG, Pavarina AC, Giampaolo ET, Machado AL, Jorge JH, Garcia PP, et al. Effect of oral hygiene education and motivation on removable partial denture wearers: Longitudinal study. Gerodontology. 2009;26:150–6. doi: 10.1111/j.1741-2358.2008.00272.x. [DOI] [PubMed] [Google Scholar]
- 22.Zenthöfer A, Dieke R, Dieke A, Wege KC, Rammelsberg P, Hassel AJ. Improving oral hygiene in the long-term care of the elderly – A RCT. Community Dent Oral Epidemiol. 2013;41:261–8. doi: 10.1111/cdoe.12007. [DOI] [PubMed] [Google Scholar]
- 23.Kullberg E, Forsell M, Wedel P, Sjögren P, Johansson O, Herbst B, et al. Dental hygiene education for nursing staff. Geriatr Nurs. 2009;30:329–33. doi: 10.1016/j.gerinurse.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 24.Wang TF, Huang CM, Chou C, Yu S. Effect of oral health education programs for caregivers on oral hygiene of the elderly: A systemic review and meta-analysis. Int J Nurs Stud. 2015;52:1090–6. doi: 10.1016/j.ijnurstu.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Viswanathan M, Ansari MT, Berkman ND, Chang S, Hartling L, McPheeters M, et al. Assessing the risk of bias of individual studies in systematic reviews of health care interventions Methods Guide for Comparative Effectiveness Review AHRQ Publication No 12-EHC047-EF. Agency for Healthcare Research and Quality. 2012. [Last accessed on 2017 Dec 25]. Available from: http://wwweffectivehealthcareahrqgov/ [PubMed]
- 27.Samson H, Berven L, Strand GV. Long-term effect of an oral healthcare programme on oral hygiene in a nursing home. Eur J Oral Sci. 2009;117:575–9. doi: 10.1111/j.1600-0722.2009.00673.x. [DOI] [PubMed] [Google Scholar]
- 28.Zenthöfer A, Cabrera T, Rammelsberg P, Hassel AJ. Improving oral health of institutionalized older people with diagnosed dementia. Aging Ment Health. 2016;20:303–8. doi: 10.1080/13607863.2015.1008986. [DOI] [PubMed] [Google Scholar]
- 29.Lago JD, Fais LM, Montandon AA, Pinelli LA. Educational program in oral health for caregivers on the oral hygiene of dependent elders. Rev Odontol UNESP. 2017;46:284–91. [Google Scholar]
- 30.Zenthöfer A, Meyer-Kühling I, Hufeland AL, Schröder J, Cabrera T, Baumgart D, et al. Carers' education improves oral health of older people suffering from dementia – Results of an intervention study. Clin Interv Aging. 2016;11:1755–62. doi: 10.2147/CIA.S118330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jäger S, Köster-Schmidt A, Schade M, Heudorf U. Oral hygiene in nursing home residents. Impact of an oral health education programme for the nursing personnel on the residents' oral health. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2009;52:927–35. doi: 10.1007/s00103-009-0940-3. [DOI] [PubMed] [Google Scholar]
- 32.Park MS, Choi-Kwon S. The effects of oral care education on caregivers' knowledge, attitude, & behavior toward oral hygiene for elderly residents in a nursing home. J Korean Acad Nurs. 2011;41:684–93. doi: 10.4040/jkan.2011.41.5.684. [DOI] [PubMed] [Google Scholar]
- 33.Sonde L, Emami A, Kiljunen H, Nordenram G. Care providers perception of the importance of oral care and its performance within everyday caregiving for nursing homes residents with dementia. Scand J Caring Sci. 2010;10:1–8. doi: 10.1111/j.1471-6712.2010.00795.x. [DOI] [PubMed] [Google Scholar]
- 34.Hugo FN, Hilgert JB, Bertuzzi D, Padilha DM, De Marchi RJ. Oral health behaviour and socio-demographic profile of subjects with Alzheimer's disease as reported by their family caregivers. Gerodontology. 2007;24:36–40. doi: 10.1111/j.1741-2358.2007.00149.x. [DOI] [PubMed] [Google Scholar]
- 35.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 36.Wade DT, Collin C. The barthel ADL index: A standard measure of physical disability? Int Disabil Stud. 1988;10:64–7. doi: 10.3109/09638288809164105. [DOI] [PubMed] [Google Scholar]
- 37.O’Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol. 1972;43:38. doi: 10.1902/jop.1972.43.1.38. [DOI] [PubMed] [Google Scholar]
- 38.Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975;25:229–35. [PubMed] [Google Scholar]
- 39.Ainamo J, Barmes D, Beagrie G, Cutress T, Martin J, Sardo-Infirri J. Development of the World Health Organization (WHO) community periodontal index of treatment needs (CPITN) Int Dent J. 1982;32:281–91. [PubMed] [Google Scholar]
- 40.Wefers KP. Der “denture hygiene index”. Dent Forum. 1999;1:3–15. [Google Scholar]
- 41.Gil-Montoya JA, Ferreira de Mello AL, Barrios R, Gonzalez-Moles MA, Bravo M. Oral health in the elderly patient and its impact on general well-being: A non-systematic review. Clin Inter Aging. 2015;10:461–7. doi: 10.2147/CIA.S54630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scannapieco FA. Position paper of the American Academy of Periodontology: Periodontal disease as a potential risk factor for systemic diseases. J Periodontol. 1998;69:841–50. [PubMed] [Google Scholar]
- 43.Scannapieco FA. Pneumonia in nonambulatory patients. The role of oral bacteria and oral hygiene. J Am Dent Assoc. 2006;137(Suppl 2):21S–5S. doi: 10.14219/jada.archive.2006.0400. [DOI] [PubMed] [Google Scholar]
- 44.Adachi M, Ishihara K, Abe S, Okuda K, Ishikawa T. Effect of professional oral health care on the elderly living in nursing homes. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:191–5. doi: 10.1067/moe.2002.123493. [DOI] [PubMed] [Google Scholar]
- 45.Hoben M, Kent A, Kobagi N, Huynh KT, Clarke A, Yoon MN, et al. Effective strategies to motivate nursing home residents in oral care and to prevent or reduce responsive behaviors to oral care: A systematic review. PLoS One. 2017;12:e0178913. doi: 10.1371/journal.pone.0178913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ellefsen B, Holm-Pedersen P, Morse DE, Schroll M, Andersen BB, Waldemar G. Assessing caries increments in elderly patients with and without dementia: A one-year follow-up study. J Am Dent Assoc. 2009;140:1392–400. doi: 10.14219/jada.archive.2009.0076. [DOI] [PubMed] [Google Scholar]
- 47.Philip P, Rogers C, Kruger E, Tennant M. Caries experience of institutionalized elderly and its association with dementia and functional status. Int J Dent Hyg. 2012;10:122–7. doi: 10.1111/j.1601-5037.2011.00525.x. [DOI] [PubMed] [Google Scholar]
- 48.Lewis A, Wallace J, Deutsch A, King P. Improving the oral health of frail and functionally dependent elderly. Aust Dent J. 2015;60(Suppl 1):95–105. doi: 10.1111/adj.12288. [DOI] [PubMed] [Google Scholar]


