Abstract
Background:
Recurrence rates are more specific indicators of prognosis than mortality rates in early stage colorectal cancer patients. Data on factors that influence colorectal cancer recurrence are sparse. We report descriptive characteristics of both colon and rectal cancer recurrence in an unselected population.
Material and Methods:
We identified 21,152 patients with colorectal cancer diagnosed between May 2001 and December 2011 and registered with the Danish Colorectal Cancer Group. Recurrences were identified in 3,198 colon and 1,838 rectal cancer patients during follow-up. We calculated the frequency, proportion, and incidence rates of colon and rectal cancer recurrence within descriptive categories, and the cumulative five- and ten-year incidences of recurrence, treating death as a competing risk. We used a Cox proportional hazard model to calculate hazard ratios (HR) and 95% confidence intervals (CI).
Results:
Recurrence risk was highest in the first three years of follow-up. Patients <55 years old at initial diagnosis (incidence rate for colon: 7.2 per 100 person-years; 95% CI: 6.5–7.9; rectum: 8.1 per 100 person-years; 95% CI: 7.2–9.0) and patients diagnosed with stage III cancer (colon HR: 5.70; 95% CI: 4.61–7.06; rectal HR: 7.02; 95% CI: 5.58–8.82) had an increased risk of recurrence. Patients diagnosed with stage III cancer from 2009–2011 had a lower incidence of recurrence than those diagnosed with stage III cancer in the years before.
Conclusions:
Descriptive characteristics of colon and rectal cancer recurrence could be used as indicators of cancer prognosis for these specific diseases and may help to inform patient-physician decision-making.
Keywords: colon cancer, rectal cancer, epidemiology, recurrence, population data
INTRODUCTION
Colorectal cancer is the third-most common cancer in the world; the lifetime risk for developing colorectal cancer is ~5% in both the United States and Denmark [1,2]. In 2012, about 1.4 million cases were diagnosed worldwide with 135,000 cases in the United States [3] and 4,800 in Denmark[4]. Colorectal cancer prognosis largely depends on the stage at which it is diagnosed: at localized stage, treatment is most successful and the five-year survival rate is 90%. In contrast, the five-year survival rates for regional and distant stages are 70% and 13%, respectively [3]. Currently, there are 1.2 million colorectal cancer survivors in the United States alone [3], and they are at risk for recurrence.
Survival rates are often used to measure prognosis for early stage colorectal cancer patients, but recurrence rates provide a more specific prognostic outcome. In patients without metastases at diagnosis, cause-specific mortality rates reflect combined effects of recurrence, receipt and effectiveness of treatments for recurrence, and survival time following recurrence. Cause of death is also susceptible to misclassification [5]. All-cause mortality data, which are widely available, further combine the influence of competing risks of death, such as the influence of comorbid diseases (e.g., diabetes and congestive heart failure) [6] and their interaction with the colorectal cancer diagnosis [7]. Furthermore, studies of cancer incidence and mortality often combine colon and rectal sites, though they may have important differences, particularly in hypermutated tumors [8–10].
Population-wide recurrence data are, unfortunately, seldom available. We have recently validated an algorithm by which recurrence can be identified [11]. We here apply this algorithm to an unselected population of stage I‒III colon and rectal cancer patients to provide the first descriptive data on both colon and rectal cancer recurrence.
MATERIAL AND METHODS
Data sources and data collection
Records in the Danish Colorectal Cancer Group (DCCG) database, the Danish National Registry of Patients (DNPR), Danish Cancer Registry (DCR), and Danish Pathology Registry (DPR) were linked by the Central Personal Registry number, a unique identifying number assigned to Danish citizens and legal residents. The DCCG database is a nearly complete clinical database of Danish colorectal cancer patients [12–14]. In addition to date of surgery, this database provided information on the date of colorectal cancer diagnosis as the date of the first hospital contact with a diagnosis of colon or rectal cancer, stage at diagnosis, and receipt of surgery and chemotherapy. The DNPR contains administrative and clinical data, including information on patient demographics, diagnoses, and surgical procedures, and has estimated 94% sensitivity and 100% specificity for classification of receipt of chemotherapy in colorectal cancer patients [15,16]. Data from the DNPR also informed our measure of prevalent comorbid diseases at the time of colorectal cancer diagnosis. The DCR is a population-based registry that contains all incidences of malignant neoplasms from 1943 onwards, and includes patient and tumor characteristics [17]. The DPR, which contains electronically recorded standard data on biological specimens from all Danish pathology departments since 1998, was used to identify pathologically diagnosed recurrences [18]. The study protocol was approved by the Danish Data Protection Agency (record number 2011–41–6968) and the North Denmark Region Committee on Health Research Ethics (record number N–20130027). Registry-based research in Denmark does not require participants’ informed consent.
Study population
We included Danish colon and rectal cancer patients who had surgery and were registered in the DCCG database between 1 May 2001 and 31 December 2011. We excluded patients with metastatic disease and unknown cancer stage. We also excluded patients with a diagnosis of colorectal cancer or metastases in the DNPR or DCR within 180 days of the date of colorectal cancer diagnosis as recorded in the DCCG database, and excluded patients with a diagnosis of cancer different from colorectal cancer (except non-melanoma skin cancer) or cancer metastases before the date of initial colorectal cancer diagnosis. Patients were followed to December 2012.
Definition of analytic variables
Cohort characteristics
Eligible patients were categorized as having colon or rectal cancer. Rectal cancers were clinically defined as those 0–15 centimeters from the anus. Within these cancer types, patients were categorized by sex, age group at cancer diagnosis (<55, 55–64, 65–74, 75–84, or ≥85 years old), AJCC stage at diagnosis (I, II, or III) [19], Charlson comorbidity score [20] at diagnosis (0, 1 or 2, or ≥3), surgical procedure, number of lymph nodes with metastases (0, 1‒3, 4‒6, or ≥7), calendar period of cancer diagnosis (2001‒2004, 2005‒2008, or 2009‒2011), surgical approach (laparotomy, laparoscopy, or endoscopy), and surgical urgency (elective or acute). Surgeries converted from laparoscopy to laparotomy were categorized as the latter. Data on utilization of neoadjuvant and adjuvant therapy were available for patients diagnosed with colon or rectal cancer from 2009‒2011.
Recurrences
To identify colon and rectal cancer recurrences, we used a previously-developed algorithm with sensitivity of 95%, specificity of 97%, positive-predictive value of 86%, and negative-predictive value of 99% when compared to an actively followed cohort of colorectal cancer patients [11]. We defined colon or rectal cancer recurrences as (a) tumor growth at or near the site of the original tumor and in the same organ (colon or rectum), or (b) metastases to tissue adjacent to the original tumor site or to a distant organ. We identified recurrences as having codes for metastasis, cytostatic therapy, or Systematized Nomenclature of Medicine (SNOMED) combinations corresponding to malignant biopsies recorded 180 or more days after first colorectal cancer surgery, 60 or more days after last cytostatic therapy code, and without a new primary cancer diagnosis registered in DNPR or DCR between the date of the first colorectal cancer surgery and the date of the DNPR cytostatic therapy code [11].
We categorized “early” colon or rectal cancer recurrences as occurring within five years of cancer diagnosis. “Late” colon or rectal cancer recurrence was defined as occurring more than five years after the cancer diagnosis.
Statistical Analysis
For both colon and rectal cancer, we calculated the frequency and proportion of recurrence for members of the cohort within categories of sex, age group, Charlson comorbidity score, stage, surgical procedure, number of lymph nodes with metastasis, calendar period of diagnosis, surgical approach, surgical urgency, and use of neoadjuvant or adjuvant therapy. We also calculated incidence rates for each of the previous categories, with the exception of neoadjuvant or adjuvant therapy use. Using a Cox proportional hazard model, we calculated crude hazard ratios (HR) and 95% confidence intervals (CI) as well as adjusted hazard ratios and confidence intervals simultaneously modeling sex, age group at surgery date, Charlson comorbidity score, tumor stage, surgical procedure, number of metastatic lymph node category, calendar period of cancer diagnosis, surgical approach, and surgical urgency for both colon and rectal cancer. The assumption of proportionality was tested by plotting the log-log functions of the estimated survival function. The separation between the curves remained parallel across analysis time, satisfying the assumption of proportionality. We also calculated the five- and ten-year cumulative incidences of colon and rectal cancer recurrence within each of the listed categories treating death as a competing risk, as well as the proportion of late recurrences. To visualize the cumulative incidence of colon and rectal cancer recurrence, we constructed cumulative incidence curves according to sex, calendar period of diagnosis, and neoadjuvant and adjuvant therapy use, all stratified by cancer stage. Statistical analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC). All statistical tests were two-sided.
RESULTS
There were 34,801 patients registered in the DCCG from 1 May 2001 to 31 December 2011, including 4,649 patients with metastases and 4,189 with unknown cancer stage who were excluded from analyses. The total number of eligible individuals in the DCCG database cohort was 21,152; of these, there were 5,036 recurrences identified from May 2001 to December 2012. Colon cancer patients had 3,198 of these recurrences while rectal cancer patients had 1,838. Table 1 describes general characteristics of the study population. The frequency of colon cancer was similar among males and females, and highest in individuals between ages 65‒74 and those with fewer comorbidities. The frequency of rectal cancer was highest in males, individuals between ages 65‒74, and those with fewer comorbidities.
Table 1:
Characteristics of the Danish Colorectal Cancer Group by cancer type
| Variable | Colon n (%) |
Rectum n (%) |
Total n (%) |
|---|---|---|---|
| Sex | |||
| Females | 7070 (51%) | 2888 (39%) | 9958 (47%) |
| Males | 6752 (49%) | 4442 (61%) | 11194 (53%) |
| Age group at surgery date | |||
| <55 years | 1250 (9.0%) | 924 (13%) | 2174 (10%) |
| 55–64 years | 2825 (21%) | 2006 (27%) | 4831 (23%) |
| 65–74 years | 4538 (33%) | 2467 (34%) | 7005 (33%) |
| 75–84 years | 4060 (29%) | 1624 (22%) | 5684 (27%) |
| ≥85 years | 1149 (8.0%) | 309 (4.0%) | 1458 (7.0%) |
| Charlson comorbidity index | |||
| Comorbidity 0 | 8853 (64%) | 5260 (72%) | 14113 (67%) |
| Comorbidity 1–2 | 4066 (29%) | 1777 (24%) | 5843 (27%) |
| Comorbidity 3+ | 903 (7.0%) | 293 (4.0%) | 1196 (6.0%) |
| AJCC tumor stage | |||
| I | 1790 (13%) | 1734 (23%) | 3524 (17%) |
| II | 6874 (50%) | 2982 (41%) | 9856 (46%) |
| III | 5158 (37%) | 2614 (36%) | 7772 (37%) |
| Lymph nodes with metastasis | |||
| None | 8664 (63%) | 4716 (64%) | 13380 (63%) |
| 1–3 | 3190 (23%) | 1611 (22%) | 4801 (23%) |
| 4–6 | 1051 (7.5%) | 512 (7.0%) | 1563 (7.4%) |
| 7+ | 917 (6.5%) | 491 (7.0%) | 1408 (6.6%) |
| Calendar period for date of cancer diagnosis | |||
| 2001–2004 | 4543 (33%) | 2533 (35%) | 7076 (33%) |
| 2005–2008 | 5234 (38%) | 2801 (38%) | 8035 (38%) |
| 2009–2011 | 4045 (29%) | 1996 (27%) | 6041 (29%) |
| Surgical technique | |||
| Laparotomy | 10122 (73%) | 5701 (78%) | 15823 (75%) |
| Laparoscopy | 3648 (26%) | 1555 (21%) | 5203 (24%) |
| Endoscopy | 52 (1.0%) | 74 (1.0%) | 126 (1.0%) |
| Surgical urgency | |||
| Missing | 2 (<0.1%) | 1 (<0.1%) | 3 (<0.1%) |
| Elective | 12005 (87%) | 7247 (99%) | 19252 (91%) |
| Acute | 1815 (13%) | 82 (1.0%) | 1897 (9.0%) |
Table 2 describes incidence rates and hazard ratios within stratified characteristics for colon and rectal cancer recurrence. Colon cancer recurrence rates were highest in patients <55 years old (7.2 per 100 person-years; 95% CI: 6.5–7.9) and lowest among those ≥85 years old (5.0 per 100 person-years; 95% CI: 4.3–5.8) and were highest in patients with regional spread to at least seven lymph nodes (22 per 100 person-years; 95% CI: 20–24). Adjusted hazard ratios indicated that patients with stage III cancer (HR: 5.70; 95% CI: 4.61–7.06, compared with stage I) or patients with acute surgical urgency (HR: 1.89; 95% CI: 1.65–2.17, compared with elective surgeries) had a higher rate of colon cancer recurrence. Patients diagnosed between 2009–2011 (HR: 0.79; 95% CI: 0.68–0.91, compared with 2001‒2004) had a decreased rate of recurrence.
Table 2:
Incidence rates and hazard ratios for selected characteristics of colon and rectal cancer patients
| Category | Colon cancer recur-rences | Person-years | Rate per 100 years (95% CI) | Colon cancer recurrence, hazard ratio (95% CI) | Colon cancer recurrence, adjusted hazard ratio* (95% CI) | Rectal cancer recur-rences | Person-years | Rate per 100 years (95% CI) | Rectal cancer recurrence, hazard ratio (95% CI) | Rectal cancer recurrence, adjusted hazard ratio* (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||||
| Females | 1550 | 26952 | 5.8 (5.5–6.0) |
1.00 | 1.00 | 683 | 11416 | 6.0 (5.6–6.4) |
1.00 | 1.00 |
| Males | 1648 | 24488 | 6.7 (6.4–7.1) |
1.13 (1.06–1.21) |
1.02 (0.93–1.12) |
1155 | 16841 | 6.9 (6.5–7.3) |
1.13 (1.03–1.24) |
1.13 (1.01–1.27) |
| Age group at surgery date | ||||||||||
| <55 years | 370 | 5156 | 7.2 (6.5–7.9) |
1.00 | 1.00 | 300 | 3722 | 8.1 (7.2–9.0) |
1.00 | 1.00 |
| 55–64 years | 766 | 11385 | 6.7 (6.3–7.2) |
0.91 (0.80–1.03) |
0.86 (0.74–1.01) |
554 | 8390 | 6.6 (6.1–7.2) |
0.82 (0.71–0.94) |
0.86 (0.73–1.02) |
| 65–74 years | 1085 | 17309 | 6.3 (5.9–6.7) |
0.82 (0.73–0.93) |
0.85 (0.73–0.99) |
616 | 9487 | 6.5 (6.0–7.0) |
0.78 (0.68–0.89) |
0.86 (0.73–1.02) |
| 75–84 years | 812 | 14292 | 5.7 (5.3–6.1) |
0.71 (0.63–0.81) |
0.75 (0.64–0.88) |
323 | 5725 | 5.6 (5.1–6.3) |
0.65 (0.55–0.75) |
0.74 (0.61–0.90) |
| ≥85 years | 165 | 3299 | 5.0 (4.3–5.8) |
0.56 (0.46–0.67) |
0.64 (0.50–0.82) |
45 | 933 | 4.8 (3.6–6.5) |
0.51 (0.37–0.70) |
0.54 (0.35–0.81) |
| AJCC tumor stage | ||||||||||
| I | 203 | 7372 | 2.8 (2.4–3.2) |
1.00 | 1.00 | 206 | 7050 | 2.9 (2.5–3.4) |
1.00 | 1.00 |
| II | 1223 | 27882 | 4.4 (4.1–4.6) |
1.63 (1.40–1.89) |
1.47 (1.22–1.78) |
614 | 12936 | 4.7 (4.4–5.1) |
1.73 (1.48–2.02) |
1.75 (1.44–2.13) |
| III | 1772 | 16186 | 11 (10–11) |
3.73 (3.22–4.31) |
5.70 (4.61–7.06) |
1018 | 8272 | 12 (12–13) |
4.09 (3.52–4.75) |
7.02 (5.58–8.82) |
| Lymph nodes with metastasis | ||||||||||
| None | 1426 | 35255 | 4.0 (3.8–4.3) |
1.00 | 1.00 | 820 | 19986 | 4.1 (3.8–4.4) |
1.00 | 1.00 |
| 1–3 | 913 | 11023 | 8.3 (7.8–8.8) |
1.94 (1.78–2.11) |
0.44 (0.38–0.51) |
545 | 5773 | 9.4 (8.7–10) |
2.23 (2.00–2.49) |
0.49 (0.41–0.59) |
| 4–6 | 418 | 3119 | 13 (12–15) |
3.02 (2.70–3.36) |
0.70 (0.59–0.83) |
227 | 1388 | 16 (14–19) |
3.49 (3.02–4.05) |
0.74 (0.59–0.92) |
| 7+ | 441 | 2043 | 22 (20–24) |
4.44 (3.99–4.94) |
— † | 246 | 1110 | 22 (20–25) |
4.59 (3.98–5.29) |
— † |
| Calendar period for date of cancer diagnosis | ||||||||||
| 2001–2004 | 1284 | 24927 | 5.2 (4.9–5.4) |
1.00 | 1.00 | 799 | 13878 | 5.8 (5.4–6.2) |
1.00 | 1.00 |
| 2005–2008 | 1307 | 19752 | 6.6 (6.3–7.0) |
0.98 (0.91–1.06) |
0.96 (0.86–1.07) |
735 | 10887 | 6.8 (6.3–7.3) |
0.92 (0.83–1.02) |
0.95 (0.83–1.08) |
| 2009–2011 | 607 | 6761 | 9.0 (8.3–9.7) |
0.84 (0.76–0.93) |
0.79 (0.68–0.91) |
304 | 3492 | 8.7 (7.8–9.7) |
0.80 (0.70–0.92) |
0.81 (0.67–0.99) |
| Surgical technique | ||||||||||
| Laparotomy | 2592 | 41415 | 6.3 (6.0–6.5) |
1.00 | 1.00 | 1543 | 24368 | 6.3 (6.0–6.7) |
1.00 | 1.00 |
| Laparoscopy | 600 | 9731 | 6.2 (5.7–6.7) |
0.74 (0.68–0.81) |
0.96 (0.86–1.07) |
274 | 3641 | 7.5 (6.7–8.5) |
0.86 (0.76–0.98) |
0.93 (0.78–1.11) |
| Endoscopy | 6 | 295 | 2.0 (0.1–4.5) |
0.38 (0.17–0.85) |
3.26 (0.50–21.1) |
21 | 247 | 8.5 (5.5–13) |
1.27 (0.83–1.96) |
4.29 (0.94–19.5) |
| Surgical urgency | ||||||||||
| Elective | 2528 | 45908 | 5.5 (5.3–5.7) |
1.00 | 1.00 | 1806 | 28037 | 6.4 (6.2–6.7) |
1.00 | 1.00 |
| Acute | 670 | 5515 | 12 (11–13) |
2.09 (1.91–2.27) |
1.89 (1.65–2.17) |
32 | 217 | 15 (10–21) |
2.18 (1.53–3.09) |
1.85 (1.07–3.20) |
Hazard ratio adjusted for categories of sex, age, Charlson comorbidity score, tumor stage, main surgical procedure type, number of metastatic lymph nodes, calendar period of cancer diagnosis, surgical technique, and surgical urgency.
No estimation due to lack of model convergence
Like colon cancer, rectal cancer recurrence rates were highest in patients <55 years old (8.1 per 100 person-years; 95% CI: 7.2–9.0) and decreased with increasing age. Adjusted hazard ratios indicated that males (HR: 1.13; 95% CI: 1.01–1.27, compared to females), patients with stage III cancer (HR: 7.02; 95% CI: 5.58–8.82, compared with stage I) or patients with acute surgical urgency (HR: 1.85; 95% CI: 1.07–3.20, compared with elective surgeries) had a higher rate of rectal cancer recurrence. Crude hazard ratios were not appreciably different within either cancer type for most descriptive characteristic categories.
Table 3 shows the five- and ten-year cumulative incidences of recurrence and the proportion of late recurrences for colon and rectal cancer. Though males had higher five- and ten-year cumulative incidences of colon cancer recurrence (five-year: 26%; 95% CI: 25%−27%, ten-year: 30%; 95% CI: 28%−31%) than females (five-year: 23%; 95% CI: 22%−24%, ten-year: 27%; 95% CI: 25%−28%), females had a slightly higher proportion of late colon cancer recurrences (6.0% vs. 5.5%). Patients diagnosed with stage III colon cancer (five-year: 36%; 95% CI: 35%−38%, ten-year: 40%; 95% CI: 38%−41%) and patients who underwent laparotomies (five-year: 26%; 95% CI: 25%−26%, ten-year: 29%; 95% CI: 28%−30%) had the highest five- and ten-year cumulative incidences of colon cancer recurrence when compared with other categories within the same strata. A higher proportion of late colon cancer recurrences occurred in patients who specifically underwent resection of the transverse or sigmoid colon (Supplemental Table 4).
Table 3:
Cumulative incidence and proportions of late recurrences of colon and rectal cancer patients
| Category | Five-year cumulative incidence of colon cancer recurrence (95% CI) | Ten-year cumulative incidence of colon cancer recurrence (95% CI) | Proportion of late colon cancer recur-rences* | Five-year cumulative incidence of rectal cancer recurrence (95% CI) | Ten-year cumulative incidence of rectal cancer recurrence (95% CI) | Proportion of late rectal cancer recur-rences* |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Females | 23% (22%−24%) | 27% (25%−28%) | 6.0% | 25% (23%−26%) | 29% (27%−31%) | 7.2% |
| Males | 26% (25%−27%) | 30% (28%−31%) | 5.5% | 27% (26%−28%) | 32% (30%−33%) | 6.9% |
| Age group at surgery date | ||||||
| <55 years | 30% (28%−33%) | 35% (32%−38%) | 5.1% | 34% (31%−37%) | 40% (36%−44%) | 6.3% |
| 55–64 years | 28% (26%−30%) | 34% (32%−36%) | 8.0% | 28% (26%−31%) | 34% (31%−37%) | 7.8% |
| 65–74 years | 25% (24%−27%) | 29% (28%−31%) | 5.4% | 26% (24%−28%) | 30% (28%−33%) | 6.8% |
| 75–84 years | 21% (20%−22%) | 24% (22%−26%) | 5.2% | 21% (19%−23%) | 24% (22%−27%) | 6.8% |
| ≥85 years | 16% (14%−18%) | 16% (14%−19%) | 1.8% | 15% (11%−20%) | 18% (13%−23%) | 6.7% |
| AJCC tumor stage | ||||||
| I | 12% (10%−14%) | 17% (14%−21%) | 10% | 13% (12%−15%) | 16% (13%−18%) | 5.8% |
| II | 18% (17%−19%) | 22% (21%−24%) | 8.4% | 20% (19%−22%) | 26% (24%−28%) | 12% |
| III | 36% (35%−38%) | 40% (38%−41%) | 3.4% | 41% (39%−43%) | 45% (43%−47%) | 4.2% |
| Lymph nodes with metastasis | ||||||
| None | 17% (16%−18%) | 21% (20%−22%) | 8.7% | 18% (17%−19%) | 23% (21%−24%) | 10% |
| 1–3 | 30% (29%−32%) | 34% (32%−36%) | 4.4% | 35% (33%−38%) | 39% (37%−42%) | 5.5% |
| 4–6 | 42% (39%−46%) | 45% (42%−49%) | 2.4% | 47% (42%−52%) | 52% (46%−57%) | 4.0% |
| 7+ | 50% (47%−54%) | 54% (50%−58%) | 2.3% | 54% (49%−59%) | 57% (51%−61%) | 1.6% |
| Calendar period for date of cancer diagnosis | ||||||
| 2001–2004 | 25% (24%−26%) | 29% (28%−30%) | 11% | 28% (26%−29%) | 32% (30%−34%) | 13% |
| 2005–2008 | 25% (24%−26%) | — † | — † | 26% (24%−27%) | — † | — † |
| 2009–2011 | — † | — † | — † | — † | — † | — † |
| Surgical technique | ||||||
| Laparotomy | 26% (25%−26%) | 29% (28%−30%) | 6.7% | 27% (25%−28%) | 31% (30%−32%) | 8.1% |
| Laparoscopy | 20% (19%−22%) | 22% (20%−24%) | 1.5% | 23% (20%−26%) | — † | — † |
| Endoscopy | 11% (3.9%−22%) | 15% (5.7%−28%) | 17% | 31% (21%−43%) | — † | — † |
| Surgical urgency | ||||||
| Elective | 22% (21%−23%) | 26% (25%−27%) | 6.5% | 26% (25%−27%) | 30% (29%−32%) | 7.1% |
| Acute | 39% (36%−41%) | 41% (38%−43%) | 3.0% | 42% (31%−53%) | — † | — † |
Number of late recurrences divided by total number of recurrences
No data reported; follow-up time is too short
Compared to females (five-year: 25%; 95% CI: 23%−26%, ten-year: 29%; 95% CI: 27%−31%), males had slightly higher five- and ten-year cumulative incidences of rectal cancer recurrence (five-year: 27%; 95% CI: 26%−28%, ten-year: 32%; 95% CI: 30%−33%). Patients diagnosed with stage III rectal cancer (five-year: 41%; 95% CI: 39%−43%, ten-year: 45%; 95% CI: 43%−47%) and patients who underwent conventional abdominoperineal rectal resections (five-year: 30%; 95% CI: 27%−32%, ten-year: 35%; 95% CI: 32%−38%) had the highest five- and ten-year cumulative incidences of rectal cancer recurrence when compared with other categories within the same strata (Supplemental Table 4).
Cumulative incidence curves stratified by tumor stage show that males had a slightly higher cumulative incidence of recurrence than females over the ten-year follow-up period for stages I-III colon and rectal cancer (Figure 1). Figure 2 shows that patients with stages I and II colon or rectal cancers had almost the same incidence of recurrence when comparing time periods of initial cancer diagnosis, with slight decreases in the cumulative incidence of colon cancer recurrence for the 2009–2011 period. However, patients diagnosed with stage III colon or rectal cancer in the period 2009–2011 had a lower incidence of recurrence after one year of follow-up than those diagnosed with stage III cancer in the years before. All three figures show that the greatest increases in recurrence occurred within three years of follow-up; the largest increase in recurrence risk occurred between the first and second year after cancer diagnosis (Supplemental Table 5).
Figure 1.
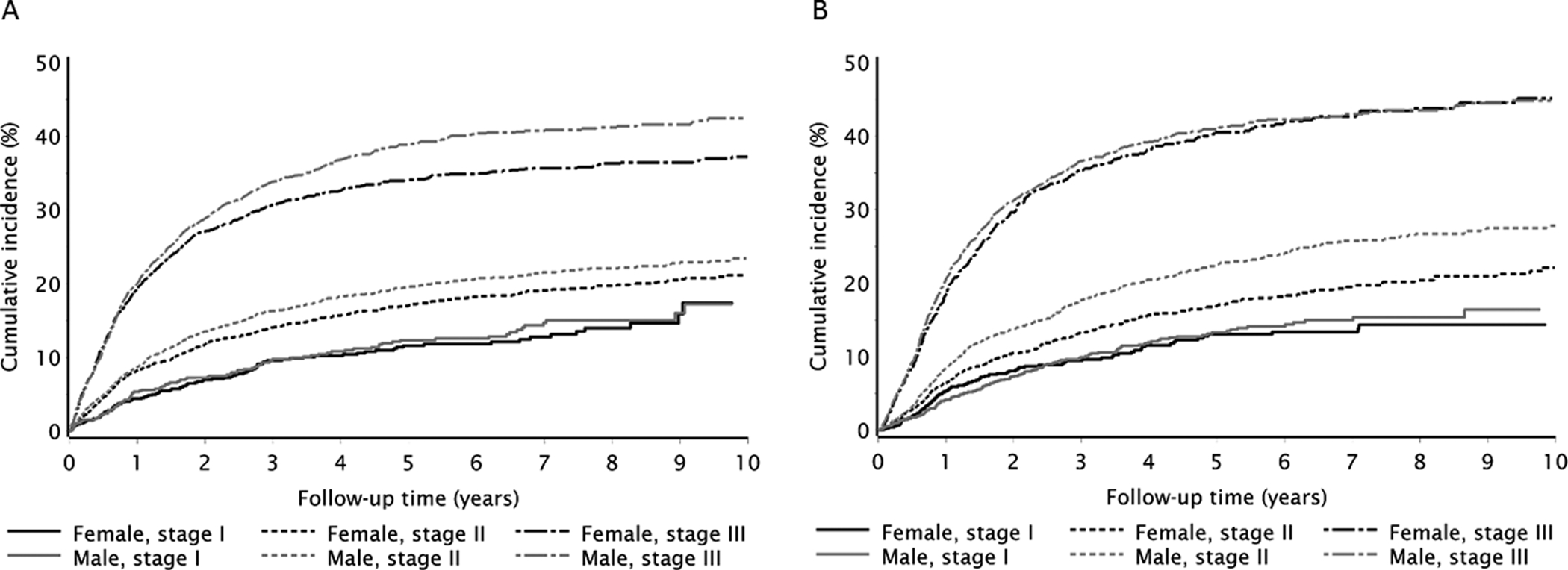
Cumulative incidence of colon (A) and rectal (B) cancer recurrence by sex, stratified by stage
Figure 2.

Cumulative incidence of colon (A) and rectal (B) cancer recurrence by calendar period of diagnosis, stratified by stage
DISCUSSION
Although many studies describe incidence and survival rates for colorectal cancer, none has systematically measured colon or rectal cancer recurrence as an outcome, overall or with respect to descriptive characteristics. In our study, age was associated with colon and rectal recurrence risk; patients who were <55 years old at initial surgery date were more likely to have a recurrence. For patients <55 years old, a higher risk of recurrence may be due in part to hereditary cancers or these individuals having more aggressive or advanced cancers than their older counterparts [21,22]. More studies, perhaps using pathology data, are warranted to further elucidate this pattern of recurrence. An initial diagnosis of stage III colorectal cancer, in which there is metastasis to regional lymph nodes, was strongly associated with recurrence. This risk factor is unsurprising, because tumor stage and lymph node involvement are used as morphological indicators of prognosis [23]. Our results showed that increasing lymph node involvement was similarly predictive of both colon and rectal cancer recurrence.
In our crude model, patients who initially underwent laparoscopic surgery had a decreased risk of recurrence compared with patients who underwent laparotomies; however, this association was attenuated in our adjusted model. Recent randomized controlled trials also demonstrated similar recurrence rates between the two techniques [24, 25]. Because laparoscopic procedures are more technically complex and not recommended for certain tumor locations (notably, obstructive right-sided or transverse colorectal cancers) [26], laparotomies are still the more common procedure.
We used cumulative incidence plots to estimate absolute differences in colon and rectal cancer recurrences over time. Each of these curves showed that the greatest recurrence hazard occurred within the first three years of follow-up, and are supported by other studies showing that recurrence is most likely to occur within the first two years of an intended curative resection [27–29]. Our tables depicting the cumulative incidences of colon and rectal cancer recurrence showed that the cumulative incidence of recurrence was similar for both cancer types, whereas previous studies have suggested that rectal cancer recurrence was higher [30,31]. These differences, as well as the figure illustrating lower cumulative incidences of recurrence for colon and rectal cancers diagnosed between 2009–2011, may be due to ever-improving surgical procedures (e.g., total mesorectal excision) and adjuvant treatment over time [32,33]. As a whole, our findings support current Danish guidelines for postoperative surveillance in colorectal cancer patients recommending CT scans after one and three years.
One limitation to our study is the lack of data on detailed tumor histopathology, as histological classification of colon and rectal tumors is also a marker of disease prognosis. This type of information may have influenced treatment decision-making, so partly explain the patterns and associations between recurrence and surgery types and other treatments. Another limitation is possible misclassification of comorbidities or surgical procedures due to inaccurate coding within the databases. However, the positive-predictive value of initial cancer diagnosis in the DCR is between 95–98% [34] and the performance characteristics of our algorithm to ascertain recurrences is also quite good [11]. The strengths of our study include a population-based design with high-quality clinical registry data and complete follow-up. In addition, this is also the first population-based study to address potential risk factors for colon or rectal cancer recurrence up to ten years after cancer diagnosis. Our ability to link population-wide information across several data sources allows for more generalizable interpretations regarding factors that may affect recurrence risk, particularly as oncology care is considered to be fairly uniform due to nationalized healthcare in Denmark [1,35]. Without systematic registry data, research on recurrence is limited to clinical trial settings, patient self-reporting, and small cancer cohorts with active surveillance, each of which have substantial limitations [36–38].
Among colorectal cancer patients, recurrence is a common event. In our population, nearly a quarter of patients diagnosed with colon or rectal cancer had a recurrence during the ten-year follow-up period. Though there are several registries that record colorectal cancer recurrence, they are often incomplete [39,40]. In addition, data on factors that influence recurrence are sparse. Here we used a validated algorithm on population-based registry data to report on several descriptive characteristics of colon and rectal cancer recurrence, which could be used as indicators of cancer prognosis for these specific diseases and may help to inform patient-physician decision-making.
Supplementary Material
Figure 3.
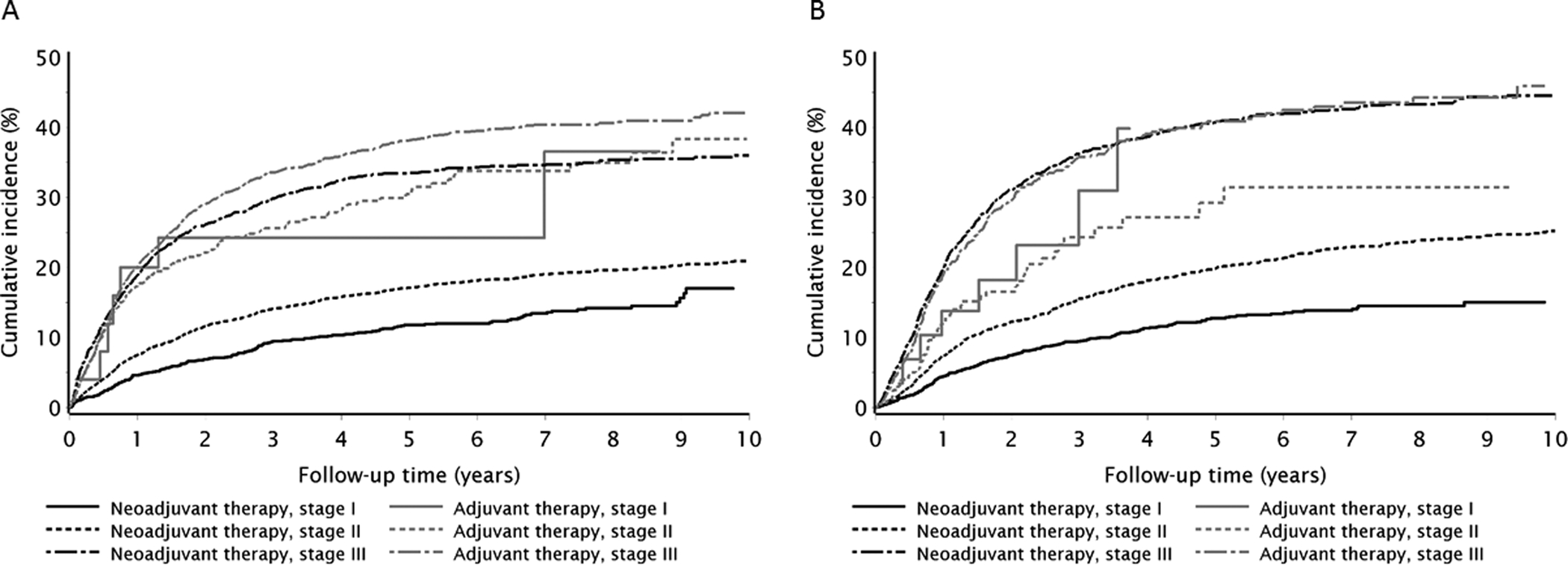
Cumulative incidence of colon (A) and rectal (B) cancer recurrence by therapy type, stratified by stage
ACKNOWLEDGEMENTS
The authors thank all patients in the Danish Colorectal Cancer Group Database.
FUNDING: This work was supported by the Danish Research and Innovation Fund (#0602-01980).
Role of funding source: The funding source had no role in the design, conduct, interpretation, or presentation of the research findings.
Footnotes
Conflict of interest statement: None declared. All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Reference List
- [1].Kraftplan II. Sundhedsstyrelsen reference information Available from URL: http://www.sst.dk/publ/publ2005/plan/kraeftplan2/Kraeftepidemiologi_rapport.pdf [accessed April 3, 2015].
- [2].Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2011, National Cancer Institute Available from URL: http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER; data submission, posted to the SEER web site [accessed April 3, 2015].
- [3].American Cancer Society. Colorectal Cancer Facts & Figures 2014–2016 Atlanta: American Cancer Society, 2014. [Google Scholar]
- [4].Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 2013;49(6):1374–1403. [DOI] [PubMed] [Google Scholar]
- [5].German RR, Fink AK, Heron M, et al. ; Accuracy of Cancer Mortality Study Group. The accuracy of cancer mortality statistics based on death certificates in the United States. Cancer Epidemiol 2011;35(2):126–131. [DOI] [PubMed] [Google Scholar]
- [6].Edwards BK, Noone AM, Mariotto AB, et al. Annual Report to the Nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer 2014;120(9):1290–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Erichsen R, Horváth-Puhó E, Iversen LH, Lash TL, Sørensen HT. Does comorbidity interact with colorectal cancer to increase mortality? A nationwide population-based cohort study. Br J Cancer 2013;109(7):2005–2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin 2014;64(2):104–117. [DOI] [PubMed] [Google Scholar]
- [9].Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer . Nature 2012;487(7407):330–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Matanoski G, Tao X, Almon L, Adade AA, Davies-Cole JO. Demographics and tumor characteristics of colorectal cancers in the United States, 1998–2001. Cancer 2006;107(suppl 5):1112–1120. [DOI] [PubMed] [Google Scholar]
- [11].Lash TL, Riis AH, Ostenfeld EB, Erichsen R, Vyberg M, Thorlacius-Ussing O. A validated algorithm to ascertain colorectal cancer recurrence using registry resources in Denmark. Int J Cancer 2015;136(9):2210–2215. [DOI] [PubMed] [Google Scholar]
- [12].Harling H, Nickelsen T. The Danish Colorectal Cancer Database . Ugeskr Laeger 2005;167(44):4187–4189. [PubMed] [Google Scholar]
- [13].Nickelsen TN, Harling H, Kronborg O, Bulow S, Jorgensen T. The completeness and quality of the Danish Colorectal Cancer clinical database on colorectal cancer. Ugeskr Laeger 2004;166:3092–3095. [PubMed] [Google Scholar]
- [14].Gogenur I, Ingeholm P, Iversen LH. Danish Colorectal Cancer Database. Ugeskr Laeger 2012;174(42):2525. [PubMed] [Google Scholar]
- [15].Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health 2011;39(suppl 7):30–33. [DOI] [PubMed] [Google Scholar]
- [16].Lund JL, Frøslev T, Deleuran T, et al. Validity of the Danish National Registry of Patients for chemotherapy reporting among colorectal cancer patients is high. Clin Epidemiol 2013;5:327–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Gjerstorff ML. The Danish Cancer Registry. Scand J Public Health 2011;39(suppl 7):42–45. [DOI] [PubMed] [Google Scholar]
- [18].Erichsen R, Lash TL, Hamilton-Dutoit S, Bjerregaard B, Vyberg M, Pedersen L. Existing data sources for clinical epidemiology: the Danish National Pathology Registry and Data Bank. Clin Epidemiol 2010;2:51–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual (7th ed). New York, NY: Springer; 2010. [Google Scholar]
- [20].Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- [21].Kanwar SS, Poolla A, Majumdar AP. Regulation of colon cancer recurrence and development of therapeutic strategies. World J Gastrointest Pathophysiol 2012;3(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Aghili M, Izadi S, Madani H, Mortazavi H. Clinical and pathological evaluation of patients with early and late recurrence of colorectal cancer. Asia Pac J Clin Oncol 2010;6(1):35–41. [DOI] [PubMed] [Google Scholar]
- [23].Zlobec I, Lugli A. Prognostic and predictive factors in colorectal cancer. J Clin Pathol 2008; 61(5):561–569. [DOI] [PubMed] [Google Scholar]
- [24].Buunen M, Veldkamp R, Hop WC, et al. ; Colon Cancer Laparoscopic or Open Resection Study Group. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 2009;10(1):44–52. [DOI] [PubMed] [Google Scholar]
- [25].Bonjer HJ, Deijen CL, Abis GA, et al. ; COLOR II Study Group. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 2015. April 2;372(14):1324–1332. [DOI] [PubMed] [Google Scholar]
- [26].Zerey M, Hawver LM, Awad Z, Stefanidis D, Richardson W, Fanelli RD; Members of the SAGES Guidelines Committee. SAGES evidence-based guidelines for the laparoscopic resection of curable colon and rectal cancer. Surg Endosc 2013;27(1):1–10. [DOI] [PubMed] [Google Scholar]
- [27].Waldron RP, Donovan IA. Clinical follow-up and treatment of locally recurrent colorectal cancer. Dis Colon Rectum 1987;30(6):428–430. [DOI] [PubMed] [Google Scholar]
- [28].Obrand DI, Gordon PH. Incidence and patterns of recurrence following curative resection for colorectal carcinoma. Dis Colon Rectum 1997;40(1):15–24. [DOI] [PubMed] [Google Scholar]
- [29].Goldberg RM. Intensive surveillance after stage II or III colorectal cancer: is it worth it? J Clin Oncol 2006;24(3):330–331. [DOI] [PubMed] [Google Scholar]
- [30].Hellinger MD, Santiago CA. Reoperation for recurrent colorectal cancer. Clin Colon Rectal Surg 2006;19(4):228–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Shumate CR, Rich TA, Skibber JM, Ajani JA, Ota DM. Preoperative chemotherapy and radiation therapy for locally advanced primary and recurrent rectal carcinoma. A report of surgical morbidity. Cancer 1993;71(11):3690–3696. [DOI] [PubMed] [Google Scholar]
- [32].Quirke P, Durdey P, Dixon MF, Williams NS. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. Lancet 1986;2(8514):996–999. [DOI] [PubMed] [Google Scholar]
- [33].Kapiteijn E, Marijnen CA, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 2001;345(9):638–646. [DOI] [PubMed] [Google Scholar]
- [34].Storm HH, Michelsen EV, Clemmensen IH, Pihl J. The Danish Cancer Registry‒history, content, quality and use. Dan Med Bull 1997;44(5):535–539. [PubMed] [Google Scholar]
- [35].National Cancer Plan, Copenhagen, Denmark: National Board of Health; 2004. Available from URL: http://www.sst.dk/publ/Publ2004/The_Nat_Cancer_Plan_02.pdf [accessed June 1, 2015].
- [36].Ford JG, Howerton MW, Lai GY, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer 2008;112(2):228–242. [DOI] [PubMed] [Google Scholar]
- [37].Bonevski B, Randell M, Paul C, et al. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med Res Methodol 2014;14:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Barisic A, Glendon G, Weerasooriya N, Andrulis IL, Knight JA. Accuracy of self-reported breast cancer information among women from the Ontario site of the Breast Cancer Family Registry. J Cancer Epidemiol 2012;2012:310804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Vukasin P, Ortega AE, Greene FL, et al. Wound recurrence following laparoscopic colon cancer resection. Results of the American Society of Colon and Rectal Surgeons Laparoscopic Registry. Dis Colon Rectum 1996;39(sup 10):20–23. [DOI] [PubMed] [Google Scholar]
- [40].Hansen MH, Balteskard L, Dorum LM, Eriksen MT, Vonen B. Locally recurrent rectal cancer in Norway. Br J Surg 2009;96(10):1176–1182. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


