Abstract
Objectives:
Describe a new, multidisciplinary team fall prevention intervention for older adults who seek care in the emergency department (ED) after having a fall, assess its feasibility and acceptability, and to review lessons learned during its initiation
Design:
Single-blind, randomized controlled pilot study
Setting:
Two urban academic EDs
Participants:
Adults ≥ 65 years old (n=110) who presented to the ED within seven days of a fall
Intervention:
Participants were randomized to a usual care (UC) and an intervention (INT) arm. Participants in the INT arm received a brief medication therapy management session delivered by a pharmacist and a fall risk assessment and plan by a physical therapist (PT). INT participants received referrals to outpatient services (e.g. home safety evaluation, outpatient PT).
Measurements:
We used participant, caregiver, and clinician surveys, as well as electronic health record review, to assess feasibility and acceptability of the intervention.
Results:
Of the 110 participants, the median participant age was 81 years old, 67% were female, 94% were white, and 16.3% had cognitive impairment. Of the 55 in the INT arm, all but one participant received the pharmacy consult (98.2%), while the PT consult was delivered to 83.6%. Median consult time was 20 mins for pharmacy and 20 mins for PT. ED length of stay was not increased in the INT arm: UC 5.25 hr. vs. INT 5.0 hrs. (p<0.94). After receiving the GAPcare intervention, 100% of participants and 97.6% of clinicians recommended the pharmacy consult and 95% of participants and 95.8% of clinicians recommended the PT consult.
Conclusion:
These findings support the feasibility and acceptability of the GAPcare model in the ED. A future, larger RCT is planned to determine whether GAPcare can reduce recurrent falls and healthcare visits in older adults.
INTRODUCTION
Falls are the leading cause of injury-related emergency department (ED) visits in older adults,1 result in $50 billion health care expenditures per year,2 and are often preventable. Prior research of community-dwelling older adults who present to the ED after falls shows that their 6-month fall risk was 29.5% higher than age-matched controls and that their functional ability, balance confidence, and depression all worsened over six months.3 Multicomponent fall prevention programs that determine the reasons for falls and modify known fall risk factors have been demonstrated to be helpful in preventing future falls.4 Geriatric Emergency Medicine Guidelines developed and endorsed by national geriatric and emergency medicine specialty organizations suggest ED staff should initiate fall prevention efforts.5 However, when older adults present to the ED after a fall, ED physicians often perform an injury assessment alone, deferring fall risk assessments and interventions to primary care providers (PCPs).3 Unfortunately, only 28% of older adults recall their last fall when presenting to their annual wellness visit.6 As a result, many older adults do not receive fall risk prevention measures after their falls.6,7
Despite the need for an effective, ED-based fall prevention approach, no applicable model exists to guide this care in the US.8 A London based study of 397 patients recruited after falls from the ED into a home-based occupational therapy assessment significantly reduced falls (OR 0.39 (95% CI 0.23–0.60),9 but when this program was implemented in the Netherlands, there was no reduction in falls.10 In the latter study, fall assessments were completed on average 5 to 10 weeks after the initial ED visit. Prompt evaluation and fall risk assessment - as can be done immediately after the injury in the ED - may prevent falls in the high risk immediate post-fall period.7,11–13 The ED visit is an opportune time to initiate fall prevention measures because patients are optimally engaged, caregivers are often present, and hospital-based staff, such as pharmacists and physical therapists (PTs) are available14. However, EDs are busy environments and ED clinicians lack the time and training15 to perform fall risk assessments. A multidisciplinary team with expertise in fall prevention that evaluates these patients in the ED could address these limitations.
We developed and pilot tested a novel fall prevention intervention, which we believe could serve as a model of care for other EDs. With this research we address two research questions identified by geriatric emergency medicine leaders as critical to improve the care of older adults in the ED who fall16: “1) Can simple ED-feasible interventions reduce injurious falls; 2) Would rapid response geriatric evaluation and management services evaluating all geriatric fallers prior to ED disposition reduce injurious falls and inpatient resource utilization?” In this manuscript, we report on the development of the GAPcare, the Geriatric Acute and Post-acute Fall Prevention intervention, and an assessment of its acceptability and feasibility. Specifically, our primary objective was to assess the feasibility of conducting a fall prevention intervention in the ED. Our secondary objective was to determine acceptability of the intervention by patients, caregivers, and clinicians.
MODEL OF CARE
Intervention setting and research context
We initiated a pilot randomized clinical trial of the GAPcare intervention at two urban academic EDs in Providence, Rhode Island: The Miriam Hospital and Rhode Island Hospital. The Miriam Hospital is an academic community hospital with 75,000 ED patient visits per year. The Rhode Island Hospital ED is the only level I trauma and tertiary referral center in the state and has an annual volume of 105,000 ED patients.
Sample and recruitment
ED patients 65 years old and older were eligible to participate if they presented to the ED within 7 days of a fall, could communicate in English or Spanish, and their ED clinician determined they were likely to be discharged from the ED (i.e., not admitted). Patients with cognitive impairment were eligible if a legally authorized representative was present in the ED to provide informed consent to participate. Individuals with altered mental status (e.g., intoxicated), who were undomiciled, or could not provide a phone number for follow-up were excluded.
Research staff reviewed the electronic health record (EHR) of potentially study eligible ED patients when pharmacy and PT were available for consultation; Monday through Friday from 7am to 4pm. Research staff approached all patients 65 and older who were presenting from the community (not from a nursing home) and were not clearly ineligible based on chart review (e.g., fall due to acute stroke or assault). Patients were asked if they experienced a “slip, trip, or fall” in the past seven days. If they replied in the affirmative, research staff asked the remaining eligibility questions and confirmed the ED clinician intended to discharge the patient home. Additionally, research staff performed the Six-Item Screener17 on all patients to determine whether the patient was at risk for cognitive impairment. The principal investigator (EG) trained the research staff how to perform this screening test. For patients that scored less than four on the Six-Item Screener (high risk for cognitive impairment) and were interested in participating in the study, the legally authorized representatives were asked to provide written consent.
After consent, research staff used REDCap18 to randomly assigned participants to the usual care (UC) or the intervention (INT) arm (1:1 allocation). We used randomization tables that stratified patients by study site with block sizes of six and four. The hospital institutional review board (IRB) approved this study. The trial was registered at www.clinicaltrials.gov (ClinicalTrials.gov identifier: ).
The GAPcare intervention
After conducting a review of the available research on this topic, we formed a multidisciplinary team of emergency physicians, geriatric-trained PTs, an ED-specialized pharmacist, and health services researchers who designed an in-ED intervention aimed to reduce fall risk. As part of the intervention, participants first were assessed by an ED clinician who directed the medical care. Thereafter they were evaluated consecutively by a pharmacist and a PT (Supplementary Figure S1). The pharmacist and PT documented their encounter using a standardized note that was integrated into the EHR to enhance information sharing with other hospital-based and outpatient providers (Supplementary Figures S2 and S3). We purposely included pharmacists and PTs as integral parts of the intervention because most hospitals have these specialists available,19 face-to-face patient-to-pharmacist medication therapy management (MTM) sessions have been demonstrated to be useful in reducing fall risk20,21, and 35% of older adults have an adverse drug event annually.22 In addition, ED-initiated PT has been shown to reduce future fall-related ED visits.23 Since we did not have pharmacists and PTs available in both study sites in the ED, we established an agreement with the health system’s Director of Pharmacy Services and Rehabilitation Services that inpatient pharmacists and PT personnel would come to the ED for these consultations.
We worked together with information technology specialists to automate the transmission of GAPcare consultation notes to the participant’s PCP. The newly created EHR structure contained a headline in the ED visit summary that alerted the PCP that the individual was part of the GAPcare intervention and that recommendations made by the pharmacist and the PT were appended to the standard ED visit summary. This process was automated to ensure the PCP received the information and to reduce burden on the ED clinician.
Research staff procedures
Research staff completed a Timed Up and Go (TUG)24 assessment to ascertain the level of mobility and fall risk of the patient. The principal investigator (EG) and a geriatric-specialized PT completed training with the research staff using simulated and real patients to ensure they could mobilize participants safely and perform the TUG prior to study initiation. The research staff performed a brief inventory of the patient’s activities of daily living (Barthel Index of Activities of Daily Living), and recorded information about the participants’ health history, prior falls, circumstances surrounding the current fall, and demographics. For patients randomized to the INT arm, the research staff initiated a pharmacist and PT consult. They recorded the time to pharmacist/PT arrival at the bedside, and time to consult completion in the data collection software. The type and timing of all study assessments are summarized in Supplementary Table S1.
Research staff were trained to report all potential adverse events to the research coordinator and principal investigator. As per local IRB guidance, a serious adverse event was defined as death. All adverse events, expected and unexpected, related to the participant’s participation in the study were reported to the Data Safety Monitoring Board on a semi-annual basis and to the IRB.
Pharmacist-led MTM session
During the brief MTM session, pharmacists evaluated participants at their bedside and asked open-ended questions to determine their knowledge of their medications and willingness to change medications to reduce fall risk. The pharmacists performed the following steps:
Reviewed the research staff-obtained medication list for accuracy using previously published best practices for medication reconciliation25
Performed motivational interviewing with participants and/or caregivers to identify one to three medications that could be stopped or modified to reduce fall risk
Communicated the medication-related action plan in writing to participants and ED treatment team. The medication-related action plan was automatically faxed to each participants’ PCP at the end of the ED visit via the newly created EHR structure.
Pharmacists communicated with the patient in person and the PCP in writing that the responsibility to change prescription medication remained with the PCP.
PT-led fall risk assessment and plan
After diagnostic imaging was reviewed by the ED clinicians and they determined it was safe to perform exercises with the participants, PT evaluated GAPcare participants at the bedside. The GAPcare PTs performed the following steps:
Performed a gait, balance, and lower extremity strength assessment (see Supplementary Table S1 for instruments)
Assessed each participants’ ability to function independently on discharge and assisted with discharge planning
Recommended outpatient services/referrals, such as referral to outpatient or home PT and occupational therapy, a home-safety evaluation, community fall prevention program, or if necessary, direct admission to a skilled nursing facility
Communicated the PT action plan in writing and in person to each participant and ED treatment team. The PT action plan was automatically faxed together with the medication-related action plan to PCPs at the conclusion of the visit via the newly created EHR structure.
Usual care arm
Participants randomly assigned to the UC arm received standard medical care as guided by the ED clinician. No consults were initiated by the research staff. Research staff reviewed the contents of a brochure created by the Centers for Disease Control and Prevention for the STEADI (Stop Elderly Accidents, Deaths, and Injuries) program, with the participant.26 It was at the discretion of the ED clinician to contact the PCP, consult case management, and provide medical equipment (e.g. walkers, canes) for participants in both arms.
Evaluation
ED visit outcomes
Our primary objective was to determine feasibility of GAPcare. We obtained key measures of feasibility, including participant enrollment, reasons for accepting or declining enrollment, and drop-out rates. We also collected measures important to ED clinical operations, including time to pharmacy and PT consult, length of each consult, and ED length of stay (LOS) for participants in both study arms. We assessed acceptability by surveying patients, caregivers, and ED clinicians at the conclusion of the ED visit. In this survey, participants were asked whether they would recommend the GAPcare intervention to their peers, if they had suggestions for improvement of the intervention, and how they would rate their satisfaction with their ED visit. The survey was adapted from the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey27 and participants had the option of entering survey results on the research tablets on their own or having the research staff input their verbal answers to questions (e.g. to accommodate participants with vision impairment). We followed the recommendations of the CONSORT extension for pilot or feasibility trials for reporting this work.28 Additional details on the methods of the GAPcare intervention can be found in our protocol manuscript.29
RESULTS
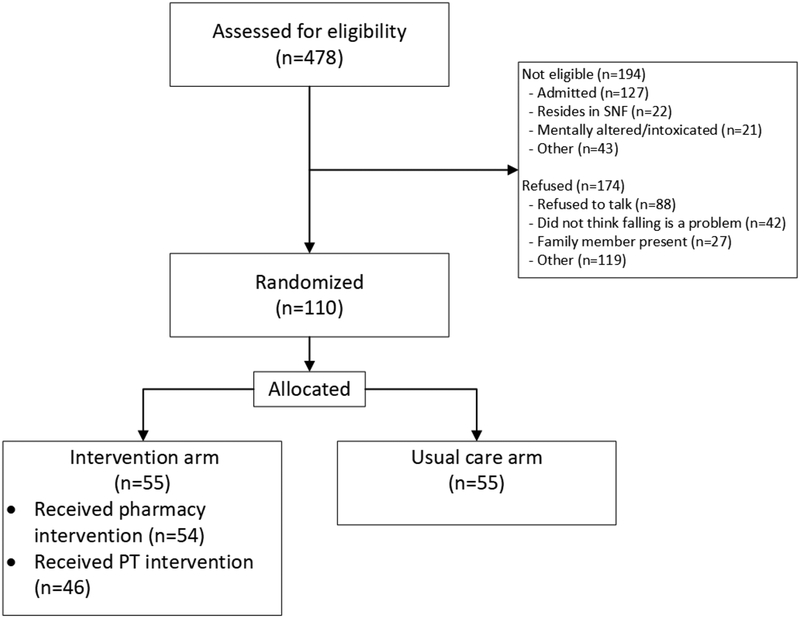
Of 478 assessed for study eligibility from January 25, 2018 to March 31, 2019, 287 were eligible for inclusion, and 110 consented to participate (Figure 1). The main reasons for ineligibility were that the ED clinician planned to admit the patient to the hospital, the patient resided in a SNF, or the patient had altered mental status. The primary reasons patients cited for declining to participate were a belief that falls were not a problem for them and because family members were present in the ED. Other reasons for exclusion and declining participation are listed in Supplementary Tables S2 and S3.
FIGURE 1. CONSORT flow diagram showing eligibility and inclusion.
This figure shows the main reasons for ineligibility and exclusion in the study.
We enrolled 110 participants in GAPcare. Although the study team initially intended to recruit 120 not 110 participants, the study was closed early to recruitment upon the receipt of advice by the Data Safety Monitoring Board who felt feasibility was sufficiently established. There were no statistically significant differences in key demographic factors between groups (Table 1). Participants were predominantly female, white, and living at home with others. 14.5% of the 55 UC participants and 18.1% of the 55 INT participants were at high risk for cognitive impairment per the Six Item Screener.
Table 1.
Participant characteristics and outcomes among 110 participants in the Geriatric Acute and Post- Acute Fall Prevention Intervention in the Emergency Department
| Characteristics | Control (n=55) | Intervention (n=55) | p-value |
|---|---|---|---|
| Age, median (IQR) | 78 (74, 88) | 82 (76, 90) | 0.17 |
| Female, n (%) | 37 (67.3) | 37 (67.3) | >0.99 |
| Race | 0.37 | ||
| White | 53 (96.4) | 51 (92.7) | |
| Black | 2 (3.6) | ||
| American Indian/Alaskan Native | 1 (1.8) | ||
| Other | 1 (1.8) | ||
| White and Asian | 1 (1.8) | ||
| Refused | 1 (1.8) | ||
| Hispanic1 | 2 (1.8) | 0.49 | |
| Living situation | 0.89 | ||
| At home alone | 18 (32.5) | 17 (30.9) | |
| At home with others | 26 (47.3) | 25 (45.5) | |
| Assisted living | 10 (18.2) | 12 (21.8) | |
| Missing | 1 (1.8) | 1 (1.8) | |
| Use assistive device | 40 (72.7) | 40 (72.7)2 | >0.99 |
| Number of prior falls in the last three months, (median (IQR)) | 1 (0, 2) | 0 (0, 2) | 0.39 |
| Cognition (SIS) (median (IQR))3 | 5 (4, 6) | 5 (5, 6) | 0.18 |
| Cognitively impaired as indicated by SIS, n (%) | 8 (14.5) | 10 (18.1) | 0.61 |
| Function (Number of ADL deficiencies, median (IQR) | 18 (16, 20) | 18 (15, 20) | 0.34 |
| ED Disposition, n (%) | |||
| Discharged to home | 39 (70.9) | 35 (63.6) | 0.58 |
| Discharged to SNF | 6 (10.9) | 10 (18.8) | |
| Admitted | 10 (18.8) | 10 (18.8) |
Missing one intervention group participant
Missing one usual care group participant
One SIS score missing. One SIS score is incomplete (one item missing)- this score is excluded from median/IQR, but included in the pass/fail breakdown.
Feasibility
Participants in the INT arm did not have a longer ED LOS than the UC arm participants (5.0 hrs. vs. 5.25 hrs.; p<0.94) (see Table 2.). Of the 55 INT participants, 98.2% underwent pharmacy consultation and 83.6% PT evaluation. Both the pharmacy and PT evaluation lasted a median of 20 minutes. Reasons cited for PT not conducting their evaluation were that one participant had a newly diagnosed spine fracture, one wanted to leave the ED prior to PT arrival, one had intractable dizziness, one was not cleared to ambulate by the ED physician after intracranial hemorrhage was discovered on CT brain imaging, and one participant was advised not to ambulate by the orthopedic surgeon due to fall-related injuries. Three additional participants were admitted to the hospital and PT consultation was deferred and one participant was deemed inappropriate by PT for an ED consult.
Table 2.
GAPcare intervention and services delivered
| Characteristic | Value |
|---|---|
| Services provided during ED visit | |
| Number and % of eligible participants received pharmacy consult4 | 54 (98.2) |
| Time to pharmacy consult, minutes (median (IQR)) | 14 (10, 20) |
| Length of pharmacy consult, minutes (median (IQR)) | 19.5 (13, 24) |
| Number and % of eligible participants received PT consult | 46 (83.6) |
| Time to PT consult, minutes (median (IQR)) | 21.5 (14, 34) |
| Length of PT consult, minutes (median (IQR)) | 19.5 (14, 29) |
| ED LOS (intervention vs. control) (Median (p-value)) | 5.0 hrs. vs. 5.25 hrs. (<0.94) |
| Recommendations by pharmacy during ED visit5 | |
| Stop fall risk increasing medication | 19 (35.2) |
| Adjust dose of fall risk increasing medication | 12 (22.2) |
| Change timing of medication | 20 (37.0) |
| Start new medication | 6 (11.1) |
| Recommendations by PT during ED visit5 | |
| Assistive device use | 27 (58.7) |
| Outpatient services (PT, OT, home safety) | 26 (56.5) |
| Discharge to SNF | 19 (41.3) |
| Hospital admission | 0 (0) |
One participant withdrew from the study after consent and randomization. They stated they did not want to stay in the ED to receive research procedures after the ED clinician told them they were ready for discharge.
Several recommendations could be made for each participant.
Acceptability
Of the 110 participants, 90% completed the index visit satisfaction survey. 96.7% of these participants were satisfied or very satisfied with their care in the INT arm, compared to 92.3% in the UC arm. Participants recommended the pharmacy consult 100% of the time and PT consult 95% of the time. Thirty-five caregivers completed their survey. 94.1% of caregivers were satisfied or very satisfied with the care their loved one received in the INT arm, compared to 94.4% in the UC arm. ED clinicians responded to the survey for 48 participants. When asked whether they believed these consultations should be integrated into routine care of ED patients with falls, most ED clinicians indicated that they were in favor of integration of pharmacy consultation (95.8%) and PT consultation (97.6%) (Supplementary Table S4).
Lessons Learned
In Table 3. we outline several lessons learned during the GAPcare intervention initiation and possible solutions when challenges were encountered.
Table 3.
Lessons learned during GAPcare implementation and possible solutions
| Category | Lessons learned | Adaptations and planned improvements |
|---|---|---|
| Recruitment | Patients did not self-identify as “fallers” | Change approach to ask about slips, trips, or falls. |
| Recruitment | Delayed identification of potentially eligible participants with falls by the research staff, and disqualification due to missed falls | Instituted automated alert in EHR to research staff for ≥65-year-old patient receiving head/neck imaging (probable fall). Broadened eligibility to include falls one week prior to ED visit. |
| Eligibility criteria | PT assessment of INT participants changed planned ED disposition to rehabilitation instead of home for INT participants | Changed eligibility criteria - participants remained in study regardless of ED disposition to allow for observation of PT effect on disposition (intention-to-treat principle) |
| Staffing | Limited availability of PT and pharmacists during evening and weekend hours | Board-certified resident pharmacists will be trained to supplement the main ED pharmacist’s activities. Consider using pharmacy students or community health workers for some tasks. |
| PCP communication | Limited communication with PCPs | EHR tools created to allow PTs, pharmacists and clinicians to share notes and fax notes automatically at discharge to PCPs to engage them more in care. |
Adverse Events
No participants experienced any serious adverse events during the ED visit as a result of participating in the intervention. We followed the CONSORT guidelines for pilot and feasibility studies and the completed CONSORT checklist can be viewed in the supplement (Supplementary Table S5).
DISCUSSION
Our data suggest that GAPcare can be delivered in the ED without prolonging ED LOS and has high acceptability to patients, caregivers, and ED clinicians. We were able successfully to incorporate pharmacist-led medication review and motivational interviewing and PT fall risk assessment into routine ED care. Lessons learned include that older individuals may not believe fall prevention is necessary for them and efforts to tailor recruitment to better address why fall prevention is helpful may lead to fewer refusals of the intervention. Because not all patients may benefit from both the PT and pharmacy component of the intervention, we are conducting a follow-up study to understand the benefit and impact of these consultations on participants and caregivers.
Although the efficacy of GAPcare to reduce recurrent falls and healthcare utilization has not yet been established, these preliminary findings suggest that a multidisciplinary fall prevention intervention can be initiated in the ED setting. There is a notable lack of research in EDs evaluating interventions to reduce the occurrence of recurrent falls among older adults.4,8,30,31 The STRIDE study and other current fall prevention protocols have attempted to address this need; however, they are not initiated in the ED immediately after a fall when patients and caregivers are highly engaged in care and fall prevention.32–35 A multicenter randomized trial in the Netherlands, which recruited older adults within two and a half months of an ED visit for a fall did not show a reduction in recurrent falls by targeting the cessation of fall-risk increasing medication.36 This trial had to prolong its recruitment window from two to four years in order to recruit its desired sample size of 620 individuals, likely in part because the investigators required patients to follow-up at their outpatient research clinic and be available for another in-person follow-up one year later.37 A strength of GAPcare is that the intervention is initiated while the participant is in the ED immediately after the fall. We believe the participants at highest risk for recurrent falls are likely those that would face the greatest difficulties with follow-up in a research clinic, and are likely to have higher rates of frailty, multimorbidity, and poor caregiver support. Therefore, it is plausible that the aforementioned deprescribing trial inadvertently recruited the patients that were least likely to benefit.
The GAPcare model differs from other fall prevention trials in its generalizability. We recruited patients with and without cognitive impairment and did not perform a fall risk stratification in order to enroll only those with traditional risk factors for recurrent falls. The American Geriatric Society recommends all patients presenting to the ED for a fall receive a fall risk assessment and often the professionals best able to perform risk stratification are also best able to offer interventions.38 Fortunately, our intervention is brief (20 minutes per consultation) and our pharmacy and PT professionals could provide both an assessment and actionable advice to participants in this short period of time. There is no universally acceptable screening method for falls in EDs and fall frequency and mortality are increasing.39 This argues for a prompt response to this epidemic. However, there is evidence that not all older adults with falls presenting to the ED may need an intervention.40,41 As the science on fall screening progresses, it will be worthwhile to revisit the criteria for which patients should be included in fall prevention interventions to prevent the potential over-testing that can be a burden to patients.42
Approaches to address fall prevention in US EDs have included studies evaluating staff-directed educational initiatives43,44 and fall risk factors45–47 with and without referral to outpatient resources. ED interventions that consist of outpatient referrals alone suffer from poor compliance, with patients often citing lack of transportation, disinterest, and lack of sufficient motivation as the reason they do not present for follow-up after a fall.7,8 GAPcare addresses these barriers by initiating assessments immediately after the fall while the patient is in the ED. In another study of 117 older adult ED patients, only half of those discharged after a fall were scheduled for follow-up for their fall-related injury.48 None were provided with follow-up to initiate fall prevention measures. This finding demonstrates that the status quo in US EDs is to defer fall prevention to PCPs. Even amongst self-reported geriatric EDs, only 57% have a falls screening or prevention protocol.49 In our study, all of the INT participants received a tailored plan from a pharmacist and PT to reduce fall risk. This plan was communicated to PCPs to alert them of the need for follow-up and provide guidance to reduce future fall risk. Since only one-quarter of older adults report falls to their PCPs this communication is likely to improve the uptake of fall prevention measures.6
Some EDs currently employ pharmacists and PTs to evaluate geriatric patients once the individual is moved to an ED observation unit. A recent retrospective study of 221 older patients evaluated in an ED observation unit by a multidisciplinary team including pharmacists, PTs, case managers, and geriatricians had a mean length of stay of 12.2 (+/− 5) hours and a hospital admission rate of 41.7%.50 Subsequent healthcare utilization and falls were not reported. The authors of that study concluded that incorporating elements of multidisciplinary geriatric assessment is feasible within an observation time frame; however, it has not previously been demonstrated to be feasible in the ED without prolonging ED LOS. ED LOS is a nationally reported hospital metric and an important consideration for patients and administrators.51 While fall prevention interventions could be initiated in the observation unit, interventions that prolong ED LOS are unlikely to be adopted given the association of long ED wait times with increased mortality, hospital admission, and lower patient satisfaction.51,52 Another recent study of patients admitted to an older adult emergency medicine unit in France after a fall received a pharmacist-led medication reconciliation intervention and demonstrated a significant reduction in 90-day unplanned rehospitalization (OR 0.45 (0.26, 0.79).53 The authors do not report on the length of stay or recurrent fall events.
How was it possible for the GAPcare intervention to provide more care without prolonging ED LOS? We believe that there are efficiencies to be gained in the standard ED evaluation of patients with a fall by recognizing the patient’s post-injury level of functional impairment and discharge needs early in the ED visit. Usual care in our EDs is to complete an ambulatory trial at the end of the ED visit to determine if traumatic injuries were missed during the initial ED evaluation and gauge the appropriateness of discharge (Can the patient walk home?). By completing the TUG early on and bringing other specialists to the bedside to help with discharge planning “more” could be done without increasing ED LOS.
Policy implications
The mortality of falls54 and fall-related ED visits by older adults are increasing.1,39,55 Falls are a leading reason for skilled nursing facility placement, which are more costly than community-based care.56 Geriatric assessments are associated with a higher likelihood of discharge to the community.55 Our research shows that geriatric assessments by pharmacists and PTs can be feasibly integrated into ED care for older adults. The Centers for Medicare and Medicaid Services and accountable care organizations could provide incentives to provide improved care transitions from the ED by investing in interventions such as GAPcare and other geriatric ED initiatives.57 This paper describes our GAPcare model and the feasibility of the intervention. We address further policy questions raised in peer-review in Table 4. Additional policy implications could be supported when there are more outcomes.
Table 4.
Practice and policy questions raised in peer-review and lessons learned from GAPcare
| Question | Lessons learned from GAPcare |
|---|---|
| What are the ramifications of these results for future emergency medicine falls interventional and implementation scientists? | A multidisciplinary approach to falls in the ED is overdue and ripe for implementation.30 Older adults will soon outnumber pediatric patients and the demand for valuable hospital beds will grow.58 A standardized, individually-tailored approach like GAPcare can be implemented without a negative impact on ED operations. |
| Can this early feasibility trial inform downstream implementation scientists? | This work was championed by an emergency medicine and aging research fellowship-trained champion with over ten years of clinical experience at both hospital sites. A pharmacy and PT champion were engaged early on in the planning of this trial. We conducted quarterly meetings to share early results and came up with solutions for early challenges. Patients that present to EDs for a fall are at higher risk than the general population for recurrent falls and many develop functional impairment. A team-based approach to fall risk assessment with pre-defined assessments and coaching on elements of motivational interviewing may help accelerate uptake. It is paramount to minimize disruptions to normal ED workflow. |
| How should ED-based fall risk assessment be adapted to accelerate efforts to reduce injurious falls?40 | There are many barriers to fall risk assessment in the ED; time, lack of personnel, and willingness of patients to engage in fall prevention measures. Even among patients who presented for falls during the study period, 1 in 4 did not want to participate in fall prevention measures. Efforts to use machine learning that do not require ED staff to perform screening and do not add additional burden on ED patients may be most likely to be adopted and are already underway.46 |
| Since a substantial proportion of fallers never reach the ED, could Emergency Medical Services (EMS) systems adapt to deliver falls interventions in the home?59 | In order for interventions to reach most older adults with falls in the United States more attention will need to be paid on providing these assessments in the home. Expediency is important and providing fall risk assessments early and consistently after a fall could be achieved through EMS training programs. EMS personnel could follow a template similar to the GAPcare consultation notes provided in the supplement (e.g. assess footwear, recommend walkers, check for home safety). |
| Could falls be an emergency marker of frailty60 or delirium? | GAPcare is not a comprehensive multifactorial fall risk assessment program and did not use validated frailty or delirium screening instruments. A 2015 systematic review of risk stratification tools using in prior ED-based research concluded that none sufficiently predicted post-ED adverse outcomes.61 Falls, however, could be a marker of future adverse outcomes. More research is needed to follow patients who present to the ED with a fall prospectively. |
| Should post-ED visit falls become a patient safety trigger tool? | Falls have been identified as a predictor of subsequent adverse events62 and should trigger intervention. Like GAPcare, interventions could be brief and focused on identifying high-risk medications, functional impairment, and determining the safety of discharge. |
LIMITATIONS
The GAPcare intervention was designed to be delivered by pharmacists and PTs. While most hospitals have these professionals available14, they may not perform consultations in the ED, thereby limiting the potential scalability of the intervention. However, the two academic EDs where we initiated this intervention also did not have PTs or pharmacists available for consultation and the intervention was still feasible at those sites. In addition, ideally ED clinicians would communicate directly with PCPs about the pharmacy and PT recommendations. However, it was important to us to integrate the model into ED care without increasing ED clinician burden. Therefore, we leveraged the EHR to facilitate communication with PCPs and other in-hospital providers. While the GAPcare intervention does not address all possible risk factors for falls, it improves upon the current evaluation, requires no additional actions from busy ED clinicians, and does not prolong ED LOS. This study was supported by a grant, but US EDs who hope to institute this intervention could have PTs and pharmacists bill for their services. Medicare recipients taking multiple medications have pharmacist-delivered MTM services covered by Medicare and PTs can bill payors for their ED-based assessments. This manuscript summarizes the feasibility and acceptability outcomes of GAPcare, but work is underway to report on the initial efficacy of the intervention including whether it reduces recurrent falls and healthcare utilization at six months.
CONCLUSION
GAPcare is a novel fall prevention intervention that is feasible in the ED and acceptable to patients, caregivers, and ED clinicians. GAPcare has the potential to provide a model of care to other EDs in the US and provide age-appropriate care for the millions of older adults who seek care after a fall.
Supplementary Material
Supplementary Figure S1. ED workflow and timing by arm
Supplementary Figure S2. Pharmacist consult note.
Supplementary Figure S3. Physical therapist consult note
Supplementary Table S1. Study instruments
Supplementary Table S2. Reasons for exclusion of participants
Supplementary Table S3: Reasons cited by patients for refusal
Supplementary Table S4: Patient and ED clinician survey findings
Supplementary Table S5: CONSORT 2010 checklist of information to include when reporting a pilot or feasibility trial
ACKNOWLEDGMENTS
Meeting presentations/funding:
This work was presented at the 2019 U13 Workshop on Embedding/Sustaining a Focus on Function in Specialty Research and Care, 2019 New England Regional Meeting, and 2019 Society of Academic Emergency Medicine Annual Meeting. Research reported in this publication received support from the National Institute on Aging (R03AG056349), AHRQ (T32AG023482) and SAEMF/EMF GEMSSTAR for Emergency Medicine Supplemental Funding (RF2017-010).
Other Contributions: The authors would like to acknowledge the leadership and teamwork of Patricia Wolfe, PT, Carol Petrie, PT, Sophia Bonenfant, Jessica Nagy, PharmD, and Joseph Aquilante Jr, PharmD. Without their contributions to GAPcare this work would not have been possible.
Sponsors role: The content is solely the responsibility of the authors and the sponsors did not play a role in the statistical analysis or presentation of the results.
Financial Disclosure: Research reported in this publication received support from the National Institute on Aging (R03AG056349), Agency for Healthcare Research and Quality (T32AG023482), and Society for Academic Emergency Medicine Foundation and the Emergency Medicine Foundation (RF2017-010). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest: The authors have no conflicts of interest.
REFERENCES:
- 1.Bergen GSM, Burns ER. Falls and Fall Injuries Among Adults Aged ≥65 Years — United States, 2014. Morbidity and Mortality Weekly Report (MMWR) Web site. https://www.cdc.gov/mmwr/volumes/65/wr/mm6537a2.htm?s_cid=mm6537a2_w. Published 2016. Accessed October 1, 2016. [DOI] [PubMed] [Google Scholar]
- 2.Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. J Am Geriatr Soc. 2018;66(4):693–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salter AE, Khan KM, Donaldson MG, et al. Community-dwelling seniors who present to the emergency department with a fall do not receive Guideline care and their fall risk profile worsens significantly: a 6-month prospective study. Osteoporos Int. 2006;17(5):672–683. [DOI] [PubMed] [Google Scholar]
- 4.Tricco AC, Thomas SM, Veroniki AA, et al. Comparisons of Interventions for Preventing Falls in Older Adults: A Systematic Review and Meta-analysis. Jama. 2017;318(17):1687–1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Geriatric emergency department guidelines. Ann Emerg Med. 2014;63(5):e7–25. [DOI] [PubMed] [Google Scholar]
- 6.Hoffman GJ, Ha J, Alexander NB, Langa KM, Tinetti M, Min LC. Underreporting of Fall Injuries of Older Adults: Implications for Wellness Visit Fall Risk Screening. J Am Geriatr Soc. 2018;66(6):1195–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shankar KN, Treadway NJ, Taylor AA, Breaud AH, Peterson EW, Howland J. Older adult falls prevention behaviors 60 days post-discharge from an urban emergency department after treatment for a fall. Inj Epidemiol. 2017;4(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carpenter CR, Cameron A, Ganz DA, Liu S. Older Adult Falls in Emergency Medicine-A Sentinel Event. Clin Geriatr Med. 2018;34(3):355–367. [DOI] [PubMed] [Google Scholar]
- 9.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet. 1999;353(9147):93–97. [DOI] [PubMed] [Google Scholar]
- 10.Hendriks MRC, Bleijlevens MHC, Van Haastregt JCM, et al. Lack of Effectiveness of a Multidisciplinary Fall-Prevention Program in Elderly People at Risk: A Randomized, Controlled Trial. Journal of the American Geriatrics Society. 2008;56(8):1390–1397. [DOI] [PubMed] [Google Scholar]
- 11.Lam C, Kang J-H, Lin H-Y, Huang H-C, Wu C-C, Chen P-L. First Fall-Related Injuries Requiring Hospitalization Increase the Risk of Recurrent Injurious Falls: A Nationwide Cohort Study in Taiwan. PLoS ONE. 2016;11(2):e0149887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sri-On J, Tirrell GP, Bean JF, Lipsitz LA, Liu SW. Revisit, Subsequent Hospitalization, Recurrent Fall, and Death Within 6 Months After a Fall Among Elderly Emergency Department Patients. Ann Emerg Med. 2017;70(4):516–521.e512. [DOI] [PubMed] [Google Scholar]
- 13.Liu S Frequency of ED revisits and death among older adults after a fall. The American journal of emergency medicine. 2015;33(8):1012 - EOA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wharton Research Data Services. American Hospital Association (AHA) Annual Survey Database,. In: Wharton Research Data Services, ed2017. [Google Scholar]
- 15.Ringer T, Dougherty M, McQuown C, et al. White Paper-Geriatric Emergency Medicine Education: Current State, Challenges, and Recommendations to Enhance the Emergency Care of Older Adults. AEM Educ Train. 2018;2(Suppl Suppl 1):S5–s16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carpenter CR, Shah MN, Hustey FM, Heard K, Gerson LW, Miller DK. High yield research opportunities in geriatric emergency medicine: prehospital care, delirium, adverse drug events, and falls. J Gerontol A Biol Sci Med Sci. 2011;66(7):775–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carpenter CR, DesPain B Fau - Keeling TN, Keeling Tn Fau - Shah M, Shah M Fau - Rothenberger M, Rothenberger M The Six-Item Screener and AD8 for the detection of cognitive impairment in geriatric emergency department patients. 2011(1097–6760 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bond CA, Raehl CL. 2006 National Clinical Pharmacy Services Survey: Clinical Pharmacy Services, Collaborative Drug Management, Medication Errors, and Pharmacy Technology. Pharmacotherapy. 2008;28(1):1–13. [DOI] [PubMed] [Google Scholar]
- 20.Blalock SJ, Casteel C, Roth MT, Ferreri S, Demby KB, Shankar V. Impact of enhanced pharmacologic care on the prevention of falls: a randomized controlled trial. Am J Geriatr Pharmacother. 2010;8(5):428–440. [DOI] [PubMed] [Google Scholar]
- 21.Mott DA, Martin B, Breslow R, et al. Impact of a medication therapy management intervention targeting medications associated with falling: Results of a pilot study. J Am Pharm Assoc (2003). 2016;56(1):22–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kahn JH, Magauran BG, Jr., Olshaker JS, Shankar KN. Current Trends in Geriatric Emergency Medicine. Emerg Med Clin North Am. 2016;34(3):435–452. [DOI] [PubMed] [Google Scholar]
- 23.Lesser A, Israni J, Kent T, Ko KJ. Association Between Physical Therapy in the Emergency Department and Emergency Department Revisits for Older Adult Fallers: A Nationally Representative Analysis. J Am Geriatr Soc. 2018. [DOI] [PubMed] [Google Scholar]
- 24.Huded JM, Dresden SM, Gravenor SJ, Rowe T, Lindquist LA. Screening for Fall Risks in the Emergency Department: A Novel Nursing-Driven Program. Western Journal of Emergency Medicine. 2015;16(7):1043–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pippins JR, Gandhi TK, Hamann C, et al. Classifying and predicting errors of inpatient medication reconciliation. J Gen Intern Med. 2008;23(9):1414–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stevens JA. The STEADI Tool Kit: A Fall Prevention Resource for Health Care Providers. The IHS primary care provider. 2013;39(9):162–166. [PMC free article] [PubMed] [Google Scholar]
- 27.Press Ganey Associates Inc. About Press Ganey. http://www.pressganey.com/about Accessed August 7, 2019, 2019.
- 28.Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldberg EM, Resnik L, Marks SJ, Merchant RC. GAPcare: the Geriatric Acute and Post-acute Fall Prevention Intervention—a pilot investigation of an emergency department-based fall prevention program for community-dwelling older adults. Pilot and Feasibility Studies. 2019;5(1):106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cameron ID, Dyer SM, Panagoda CE, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev. 2018;9:Cd005465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harper KJ, Barton AD, Arendts G, Edwards DG, Petta AC, Celenza A. Controlled clinical trial exploring the impact of a brief intervention for prevention of falls in an emergency department. Emerg Med Australas. 2017;29(5):524–530. [DOI] [PubMed] [Google Scholar]
- 32.National Institutes of Health. NIH, PCORI announce major award to prevent falls injuries in older people. https://www.nih.gov/news-events/news-releases/nih-pcori-announce-major-award-prevent-falls-injuries-older-people. Published 2014. Accessed July 5, 2017. [Google Scholar]
- 33.Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, Beil TL, Thompson JH. U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews In: Interventions to Prevent Falls in Community-Dwelling Older Adults: A Systematic Review for the U.S. Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality (US); 2018. [PubMed] [Google Scholar]
- 34.Bhasin S, Gill TM, Reuben DB, et al. Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE): A Cluster-Randomized Pragmatic Trial of a Multifactorial Fall Injury Prevention Strategy: Design and Methods. J Gerontol A Biol Sci Med Sci. 2018;73(8):1053–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johnston YA, Bergen G, Bauer M, et al. Implementation of the Stopping Elderly Accidents, Deaths, and Injuries Initiative in Primary Care: An Outcome Evaluation. The Gerontologist. 2018:gny101-gny101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boye ND, van der Velde N, de Vries OJ, et al. Effectiveness of medication withdrawal in older fallers: results from the Improving Medication Prescribing to reduce Risk Of FALLs (IMPROveFALL) trial. Age Ageing. 2017;46(1):142–146. [DOI] [PubMed] [Google Scholar]
- 37.Hartholt KA, Boye ND, Van der Velde N, et al. [Cost] effectiveness of withdrawal of fall-risk increasing drugs versus conservative treatment in older fallers: design of a multicenter randomized controlled trial (IMPROveFALL-study). BMC Geriatr. 2011;11:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.American Geriatrics Society, British Geriatrics Society, American Academy of Orthopaedic Surgeons. Guideline for the prevention of falls in older persons. https://geriatricscareonline.org/application/content/products/CL014/html/CL014_BOOK001.html. Published 2019. Accessed. [PubMed]
- 39.Shankar KN, Liu SW, Ganz DA. Trends and Characteristics of Emergency Department Visits for Fall-Related Injuries in Older Adults, 2003–2010. West J Emerg Med. 2017;18(5):785–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carpenter CR, Avidan MS, Wildes T, Stark S, Fowler SA, Lo AX. Predicting geriatric falls following an episode of emergency department care: a systematic review. Acad Emerg Med. 2014;21(10):1069–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carpenter CR. Deteriorating functional status in older adults after emergency department evaluation of minor trauma--opportunities and pragmatic challenges. J Am Geriatr Soc. 2013;61(10):1806–1807. [DOI] [PubMed] [Google Scholar]
- 42.Carpenter CR, Raja AS, Brown MD. Overtesting and the Downstream Consequences of Overtreatment: Implications of “Preventing Overdiagnosis” for Emergency Medicine. Acad Emerg Med. 2015;22(12):1484–1492. [DOI] [PubMed] [Google Scholar]
- 43.Baraff LJ, Lee TJ, Kader S, Penna RD. Effect of a Practice Guideline on the Process of Emergency Department Care of Falls in Elder Patients. Academic Emergency Medicine. 1999;6(12):1216–1223. [DOI] [PubMed] [Google Scholar]
- 44.Baraff LJ, Della Penna R, Williams N, Sanders A. Practice guideline for the ED management of falls in community-dwelling elderly persons. Kaiser Permanente Medical Group. Ann Emerg Med. 1997;30(4):480–492. [DOI] [PubMed] [Google Scholar]
- 45.Southerland LT, Slattery L, Rosenthal JA, Kegelmeyer D, Kloos A. Are triage questions sufficient to assign fall risk precautions in the ED? Am J Emerg Med. 2017;35(2):329–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Patterson BW, Repplinger MD, Pulia MS, et al. Using the Hendrich II Inpatient Fall Risk Screen to Predict Outpatient Falls After Emergency Department Visits. J Am Geriatr Soc. 2018;66(4):760–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carpenter CR, Scheatzle MD, D’Antonio JA, Ricci PT, Coben JH. Identification of fall risk factors in older adult emergency department patients. Acad Emerg Med. 2009;16(3):211–219. [DOI] [PubMed] [Google Scholar]
- 48.Paniagua MA, Malphurs JE, Phelan EA. Older patients presenting to a county hospital ED after a fall: missed opportunities for prevention. Am J Emerg Med. 2006;24(4):413–417. [DOI] [PubMed] [Google Scholar]
- 49.Hogan TM, Olade TO, Carpenter CR. A profile of acute care in an aging America: snowball sample identification and characterization of United States geriatric emergency departments in 2013. Acad Emerg Med. 2014;21(3):337–346. [DOI] [PubMed] [Google Scholar]
- 50.Southerland LT, Vargas AJ, Nagaraj L, Gure TR, Caterino JM. An Emergency Department Observation Unit Is a Feasible Setting for Multidisciplinary Geriatric Assessments in Compliance With the Geriatric Emergency Department Guidelines. Academic Emergency Medicine. 2018;25(1):76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Berg LM, Ehrenberg A, Florin J, Ostergren J, Discacciati A, Goransson KE. Associations Between Crowding and Ten-Day Mortality Among Patients Allocated Lower Triage Acuity Levels Without Need of Acute Hospital Care on Departure From the Emergency Department. Ann Emerg Med. 2019. [DOI] [PubMed] [Google Scholar]
- 52.Vermeulen MJ, Guttmann A, Stukel TA, et al. Are reductions in emergency department length of stay associated with improvements in quality of care? A difference-in-differences analysis. BMJ Qual Saf. 2016;25(7):489–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Clementz A, Jost J, Lacour A, et al. Effect of Clinical Pharmacy Services in an Older Adult Emergency Medicine Unit on Unplanned Rehospitalization of Older Adults Admitted for Falls: MUPA-PHARM Study. J Am Med Dir Assoc. 2019;20(8):947–948. [DOI] [PubMed] [Google Scholar]
- 54.Hartholt KA, Lee R, Burns ER, van Beeck EF. Mortality From Falls Among US Adults Aged 75 Years or Older, 2000–2016. Jama. 2019;321(21):2131–2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Saha S, DiRusso SM, Welle S, et al. Integration of Geriatrician Consultation for Trauma Admissions May Benefit Patient Outcomes. Gerontol Geriatr Med. 2019;5(1–6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sirois MJ, Emond M, Ouellet MC, et al. Cumulative incidence of functional decline after minor injuries in previously independent older Canadian individuals in the emergency department. J Am Geriatr Soc. 2013;61(10):1661–1668. [DOI] [PubMed] [Google Scholar]
- 57.Howland J, Shankar KN, Peterson EW, Taylor AA. Savings in acute care costs if all older adults treated for fall-related injuries completed matter of balance. Inj Epidemiol. 2015;2(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.United States Census Bureau. Older People Projected to Outnumber Children for First Time in U.S. History. https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-projections.html. Published 2018. Accessed 8/8/19.
- 59.Zozula A, Carpenter CR, Lipsey K, Stark S. Prehospital emergency services screening and referral to reduce falls in community-dwelling older adults: a systematic review. Emerg Med J. 2016;33(5):345–350. [DOI] [PubMed] [Google Scholar]
- 60.Walston J, Robinson TN, Zieman S, et al. Integrating Frailty Research into the Medical Specialties-Report from a U13 Conference. Journal of the American Geriatrics Society. 2017;65(10):2134–2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Carpenter CR, Shelton E, Fowler S, et al. Risk factors and screening instruments to predict adverse outcomes for undifferentiated older emergency department patients: a systematic review and meta-analysis. Acad Emerg Med. 2015;22(1):1–21. [DOI] [PubMed] [Google Scholar]
- 62.Lindblad M, Schildmeijer K, Nilsson L, Ekstedt M, Unbeck M. Development of a trigger tool to identify adverse events and no-harm incidents that affect patients admitted to home healthcare. BMJ Quality & Safety. 2018;27(7):502–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure S1. ED workflow and timing by arm
Supplementary Figure S2. Pharmacist consult note.
Supplementary Figure S3. Physical therapist consult note
Supplementary Table S1. Study instruments
Supplementary Table S2. Reasons for exclusion of participants
Supplementary Table S3: Reasons cited by patients for refusal
Supplementary Table S4: Patient and ED clinician survey findings
Supplementary Table S5: CONSORT 2010 checklist of information to include when reporting a pilot or feasibility trial