A cervical rib, also called as an accessory or a supernumerary rib, is a congenital anomaly that usually develops from the seventh vertebra and extremely rarely from the fifth or sixth vertebra. It may blindly end up in the soft tissues of the neck, articulate with the first thoracic rib and sternum, or connect to a fibrous band. Cervical ribs can bilaterally appear in approximately 50% of patients. The presence of two ribs on the same side is an unusual finding (1).
A 53-year-old Hispanic woman with a history of fibromyalgia visited our rheumatology office for a second opinion about a lump in the neck. Although she detected the mass several years ago, it did not cause any symptoms. Two months ago, the patient visited her primary doctor for medical advice because her family was concerned about any malignancy. At the time of presentation to the rheumatology office, the patient denied fatigue, weight lost, fever, and local manifestations including pain or difficulty to swallow. Symptoms related to regional conditions such as upper limb pain, paresthesia, coldness, or color changes in the fingertips were not experienced.
On physical examination, a firm, non-pulsatile, non-tender, and immobile rounding mass of approximately 1.5 cm2 was noted at the anterior triangle of the right side of the neck. No regional enlarged lymph nodes or satellite nodules were observed. Phalen’s and Tinel’s test were both normal. Adson’s maneuver test and the Upper Limb Tension Test (Elvey’s) were both negative. Several studies were prescribed at a previous visit by the primary doctor including hemoglobin level, white cell count, erythrocyte sedimentation rate, thyroid panel (TSH, free T4, and T3), vascular carotid Doppler, and thyroid ultrasound, which showed no abnormality.
Ultrasonography of the neck protuberance at the rheumatology office revealed a hyperechoic enhancement with acoustic shadowing, consistent with a bony pattern. This was immediately followed by a simple anteroposterior radiograph of the chest, which confirmed the bony structure at the seventh cervical rib on the right side (Figure 1).
Figure 1.
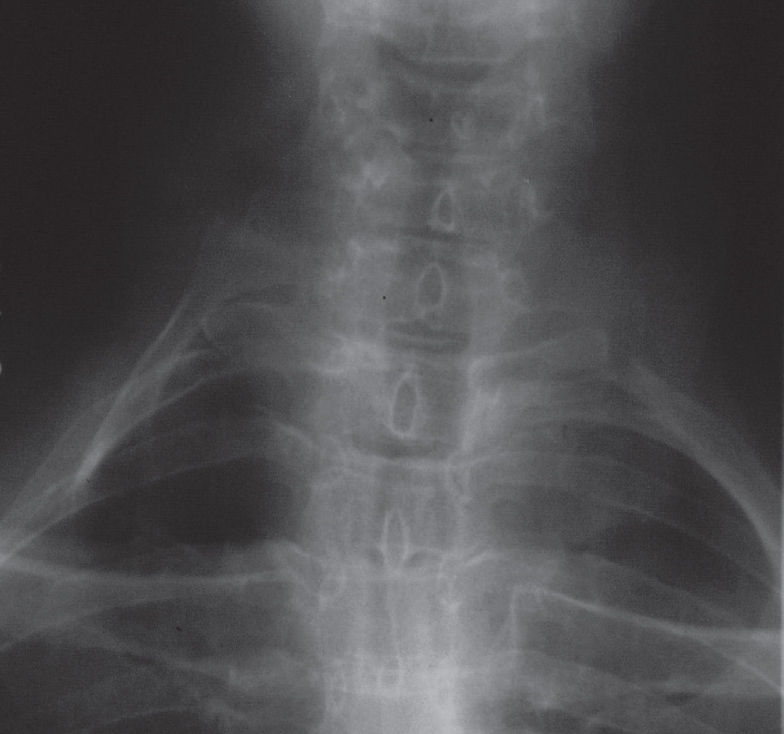
A supernumerary rib (arrow) is emerging from the last cervical vertebral body on the right side of the cervical spine.
Based on results of radiographies, the incidence of supernumerary ribs is approximately 0.05%–3% (2). These ribs are observed more commonly in females than in males. In a report that included 5000 chest X-rays, these ribs were found in 70% females and 50% males (3, 4).
Regarding clinical manifestation, cervical ribs are often asymptomatic throughout life. In patients who required surgery due to thoracic outlet syndrome, only 8%–10% had a supernumerary rib (3, 5). Leong and Karkos (6) described a woman in Singapore with a hard lump in the neck due to a protruding rib without any other symptoms. A teenage male with a similar clinical feature was recently reported (2). The occurrence of a palpable mass has been overlocked, perhaps as a result of physical examination based on neurovascular clinical maneuvers. However, among 19 patients with a thoracic outlet syndrome due to a cervical rib, Brannon (7) found that 68% had a firm mass in the neck.
The presence of an indolent firm mass in the neck should alert clinicians about the possibility of a cervical rib in the lower cervical spine, even in cases without any symptoms of neurovascular compression. Ultrasound, in addition to physical examination, can be helpful as a first diagnostic step to confirm the bony prominence in the neck region.
Omitting or postponing a simple diagnostic test using modern tests, such as in this case, can cause a tortuous and delayed diagnosis process. Despite the extreme usefulness of novel imaging modalities in the assessment of symptoms due to a supernumerary rib (8, 9), a simple chest radiograph is still the first step in the diagnosis of a cervical rib.
Footnotes
Peer-review: Externally peer-reviewed.
Conflict of Interest: The author has no conflict of interest to declare.
Financial Disclosure: The author declared that this study has received no financial support.
References
- 1.Abson AW, Coffey JR. Cervical rib. A method of anterior approach for relief of symptoms by division of the scalenus anticus. Ann Surg. 1927;85:839–57. doi: 10.1097/00000658-192785060-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chandak S, Kumar A. Usefulness of 3D CT in diagnosis of cervical rib presenting as supraclavicular swelling of short duration. J Clin Diagn Res. 2014;8:RD01–2. doi: 10.7860/JCDR/2014/7977.4374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brewin J, Hill M, Ellis H. The prevalence of cervical ribs in a London population. Clin Anat. 2009;23:331–6. doi: 10.1002/ca.20774. [DOI] [PubMed] [Google Scholar]
- 4.Haven H. Neurocirculatory scalenus anticus syndrome in the presence of developmental defects of the first rib. Yale J Bio. 1939;11:443–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Sanders RJ, Hammond SL, Rao NM. Thoracic outlet syndrome: a review. Neurologist. 2008;14:365–73. doi: 10.1097/NRL.0b013e318176b98d. [DOI] [PubMed] [Google Scholar]
- 6.Leong SC, Karkos PD. “hard” neck lump. Singapore Med J. 2009;50:e141–2. [PubMed] [Google Scholar]
- 7.Brannon EW. Cervical rib syndrome. An analysis of nineteen cases and twenty-four operations. J Bone Joint Surg Am. 1963;45:977–98. doi: 10.2106/00004623-196345050-00007. [DOI] [PubMed] [Google Scholar]
- 8.Viertel VG, Intrapiromkul J, Maluf F, Patel NV, Zheng W, Alluwaimi F, et al. Cervical ribs: A common variant overlooked in CT imaging. AJNR Am J Neuroradiol. 2012;33:2191–4. doi: 10.3174/ajnr.A3143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walden MJ, Adin ME, Visagan R, Viertel VG, Intrapiromkul J, Maluf F, et al. Cervical ribs: identification on MRI and clinical relevance. Clin Imaging. 2013;37:938–41. doi: 10.1016/j.clinimag.2013.01.005. [DOI] [PubMed] [Google Scholar]


