Abstract
Introduction
SHILLA and growth rods are two main surgical correction techniques for patients with early-onset scoliosis. There have been some comparative studies between the two techniques, where a comparison was made between deformity identifying characteristics such as Cobb angle, apical vertebral translation, coronal balance, spinal length gain, etc. However, the SHILLA procedure experiences loss of correction or the reappearance of deformity through crankshafting or adding-on (e.g., distal migration). The current study identifies a solution with a modified approach to SHILLA (which could help in dynamically remodulating the apex of the deformity and mitigating loss of correction) and presents comparative correction data against the long-established traditional growth rod system.
Methods
The active apex correction (APC) group consisted of 20 patients and the growth rod group consisted of 26 patients, both with the same inclusion and exclusion criteria. The APC surgical procedure involved a modified SHILLA technique, that is, insertion of pedicle screws in the convex side of the vertebrae above and below the wedged one for compression and absence of apical fusion.
Results
There were no statistical differences between the various spinal parameters (namely, Cobb angle, apical vertebral translation, sagittal balance, and spinal length gain) of the two groups. However, significant differences existed for coronal balance, which in part may have been due to differences in its pre-op value between the two groups.
Conclusions
APC and the traditional growth rod system showed similar deformity correction parameters at current follow-ups; however, the latter requires multiple surgeries to regularly distract the spine.
Keywords: active apex correction, growth rod, SHILLA, growth guidance, modified SHILLA technique, crankshafting, distal migration, adding-on
Introduction
The growth guidance technique using SHILLA is a clinically accepted alternative to a distraction-based growth rod system1). There have been a few studies comparing these two techniques, where a comparison was made between deformity identifying characteristics such as Cobb angle, apical vertebral translation, coronal balance, spinal length gain, etc2-4). Most noteworthy was the study by Andras et al, a case series demonstrating that patients who received growth rods had a greater improvement in Cobb angle and a greater increase in T1-S1 length than SHILLA2). However, in another case series by Luhmann et al, there were no statistically significant differences in the clinical parameters at follow-up between the two groups (growth rods vs SHILLA)4). In addition to the above variability in data against the traditional growth rod approach, there are still two major disadvantages of using SHILLA: loss of correction and need for osteotomies. To elaborate, a substantial percentage of patients undergoing the SHILLA technique experience loss of correction via crankshafting or adding-on (e.g., distal migration)5-7). In addition, the need for osteotomies on the concave side has the potential of severe complications8,9). Therefore, any modified SHILLA technique that could eliminate (i) the loss of correction via active reverse remodulation at the apex and (ii) complications related to the need for osteotomies on the concave side is very desirable, especially because growth guidance does not require repeated surgeries like traditional growth rods10-22). This nonfusion SHILLA procedure, active apex correction (APC), is performed by placing pedicle screws on the convex side, above and below the wedged vertebrae23). The pedicle screws are then compressed before the final tightening, to artificially create compensatory pressure on the vertebral body by gradually allowing its remodulation (reverse modulation) and reduction in the wedging over time. In contrast to the regular SHILLA approach, the addition of active apex correction does not fuse the apex of the deformity. The objective of the current study is to compare the clinical parameters at follow-up between the new APC technique and the traditional growth rod technique performed by the same team of surgical staff.
Materials and Methods
Institutional review board approval was received, and the study duration spanned 6 years (2013-2019). The APC group consisted of 20 patients with either scoliosis or kyphoscoliosis undergoing index surgery or revision surgery and demonstrating clear radiographic evidence of vertebral wedging at the apex. All patients were under 8 years of age with Risser grade less than or equal to 2 and the major Cobb's angle more than 40°. Following the same criteria, the growth rod group consisted of 26 patients. Refer to Table 1 (used with permission) and Table 2 for further patient details at the time of surgery23).
Table 1.
Diagnoses, Age at Surgery, Gender, and Spinal Parameters at Pre-op and Follow-up in the APC Group, Used with Permission23).
| APC | Diagnosis | Age | Gender | Follow-up time | Cobb angle | AVT | Kyphosis | Sagittal balance | Spine length | Coronal balance | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | FU | Pre | FU | Pre | FU | Pre | FU | Pre | FU | Pre | FU | |||||
| 1 | Syndromic scoliosis | 7 | M | 24 | 57 | 59 | 34 | 69 | N/A | 281 | 299 | 5 | 20 | |||
| 2 | Congenital scoliosis | 5 | F | 15 | 69 | 53 | 38 | 18 | 281 | 293 | 6 | 24 | ||||
| 3 | Syndromic scoliosis | 3 | M | 20 | 40 | 52 | 13 | 29 | 260 | 244 | 2 | 2 | ||||
| 4 | Syndromic scoliosis | 6 | M | 24 | 69 | 33 | 56 | 23 | 244 | 292 | 10 | 25 | ||||
| 5 | Congenital scoliosis | 4 | F | 24 | 61 | 46 | 25 | 25 | 233 | 258 | 6 | 3 | ||||
| 6 | Congenital scoliosis | 3 | F | 24 | 47 | 32 | 26 | 30 | 231 | 238 | 37 | 3 | ||||
| 7 | Congenital scoliosis | 3 | F | 16 | 40 | 32 | 34 | 38 | 273 | 296 | 13 | 8 | ||||
| 8 | Syndromic scoliosis | 6 | F | 8 | 48 | 51 | 32 | 26 | 343 | 396 | 4 | 17 | ||||
| 9 | Neurofibromatosis | 7 | F | 15 | 63 | 60 | 39 | 34 | 299 | 292 | 11 | 18 | ||||
| 10 | Syndromic scoliosis, Noonan syndrome | 5 | F | 14 | 92 | 55 | 56 | 44 | 211 | 245 | 23 | 19 | ||||
| 11 | Neurofibromatosis with scoliosis | 5 | M | 12 | 82 | 79 | 57 | 57 | 284 | 317 | 48 | 22 | ||||
| 12 | Congenital scoliosis | 3 | F | 12 | 62 | 60 | 46 | 52 | 229 | 253 | 2 | 3 | ||||
| 13 | Achondroplasia with kyphoscoliosis | 3 | M | 97 | 53 | 30 | 26 | 24 | 54 | 62 | 24 | 14 | 240 | 251 | 8 | 14 |
| 14 | Congenital kyphoscoliosis | 4 | M | 74 | 42 | 38 | 29 | 27 | 32 | 10 | 40 | 57 | 282 | 322 | 57 | 3 |
| 15 | Muscular dystrophy kyphoscoliosis | 4 | F | 72 | 50 | 34 | 19 | 9 | 40 | 12 | 23 | 65 | 218 | 264 | 2 | 1 |
| 16 | Syndromic kyphoscoliosis | 6 | M | 42 | 55 | 41 | 47 | 14 | 55 | 38 | 28 | 26 | 251 | 278 | 42 | 3 |
| 17 | Congenital kyphoscoliosis | 4.5 | F | 85 | 20 | 21 | 17 | 8 | 45 | 25 | 22 | 8 | 262 | 313 | 21 | 23 |
| 18 | Mucopolysach. kyphoscoliosis | 5 | F | 32 | 27 | 14 | 28 | 9 | 55 | 16 | 124 | 51 | 174 | 216 | 15 | 16 |
| 19 | Achondroplasia with kyphoscoliosis | 5 | M | 12 | 45 | 48 | 42 | 38 | 100 | 23 | 34 | 20 | 274 | 280 | 6 | 12 |
| 20 | Congenital kyphoscoliosis T9-L2 | 3 | F | 24 | 55 | 39 | 8 | 7 | 76 | 24 | 23 | 8 | 227 | 270 | 4 | 3 |
| p-value (2-tailed) | 0.002 | 0.2 | 0.01 | 0.5 | <0.00001 (1-tailed) |
0.3 | ||||||||||
| Average | 5 | 12F & 8M | 32 | 54 | 44 | 34 | 29 | 57 | 26 | 40 | 31 | 255 | 281 | 16 | 12 | |
| Standard deviation | 1 | 27 | 17 | 15 | 14 | 17 | 22 | 17 | 35 | 23 | 37 | 39 | 17 | 9 | ||
| Maximum | 7 | 97 | 92 | 79 | 57 | 69 | 100 | 62 | 124 | 65 | 343 | 396 | 57 | 25 | ||
| Minimum | 3 | 8 | 20 | 14 | 8 | 7 | 32 | 10 | 22 | 8 | 174 | 216 | 2 | 1 | ||
APC, active apex correction; FU, follow-up; AVT, apical vertebral translation; N/A, they didn’t have abnormal sagittal values and it was purely scoliosis .
Table 2.
Diagnoses, Age at Surgery, Gender, and Spinal Parameters at Pre-op and Follow-up in the Growth Rod Group.
| Growth rods | Diagnosis | Age | Gender | Follow-up time | Cobb angle | AVT | Kyphosis | Sagittal balance | Spine length | Coronal balance | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | FU | Pre | FU | Pre | FU | Pre | FU | Pre | FU | Pre | FU | |||||
| 1 | Congenital scoliosis | 3 | F | 72 | 88 | 43 | 60 | 44 | N/A | 241 | 311 | 12 | 34 | |||
| 2 | Congenital scoliosis | 2.5 | M | 60 | 55 | 63 | 22 | 44 | 211 | 221 | 33 | 27 | ||||
| 3 | Congenital scoliosis | 2.5 | F | 84 | 90 | 50 | 26 | 25 | 180 | 193 | 55 | 44 | ||||
| 4 | Infantile idiopathic scoliosis | 5 | F | 36 | 70 | 30 | 40 | 26 | 273 | 306 | 30 | 4 | ||||
| 5 | Syndromic scoliosis, hemi L1, bony bar T12-L2 | 5 | M | 81 | 87 | 79 | 72 | 57 | 275 | 324 | 32 | 27 | ||||
| 6 | Syndromic scoliosis, NF, T4-10 | 8 | F | 77 | 73 | 61 | 42 | 57 | 308 | 404 | 32 | 29 | ||||
| 7 | Congenital scoliosis | 7.5 | F | 54 | 58 | 59 | 52 | 52 | 281 | 300 | 16 | 23 | ||||
| 8 | Neuromuscular scoliosis | 3.5 | F | 63 | 58 | 72 | 24 | 23 | 226 | 288 | 34 | 80 | ||||
| 9 | Neuromuscular scoliosis | 7 | M | 60 | 79 | 47 | 70 | 52 | 212 | 251 | 8 | 13 | ||||
| 10 | Congenital scoliosis | 6.5 | F | 57 | 80 | 60 | 44 | 30 | 258 | 273 | 22 | 21 | ||||
| 11 | Congenital scoliosis | 8.5 | M | 34 | 77 | 71 | 16 | 30 | 230 | 247 | 71 | 52 | ||||
| 12 | Idiopathic scoliosis | 8.5 | F | 53 | 49 | 33 | 48 | 29 | 304 | 369 | 18 | 44 | ||||
| 13 | Neuromuscular scoliosis | 4 | M | 26 | 48 | 36 | 19 | 2 | 262 | 284 | 47 | 17 | ||||
| 14 | Congenital scoliosis | 2 | F | 72 | 45 | 18 | 12 | 8 | 242 | 297 | 18 | 23 | ||||
| 15 | Congenital scoliosis | 8 | F | 54 | 71 | 61 | 20 | 40 | 215 | 255 | 23 | 20 | ||||
| 16 | Congenital scoliosis | 2.5 | F | 84 | 56 | 62 | 37 | 66 | 219 | 273 | 4 | 17 | ||||
| 17 | Congenital scoliosis | 7 | F | 24 | 62 | 46 | 33 | 49 | 323 | 367 | 21 | 12 | ||||
| 18 | Juvenile idiopathic scoliosis | 10 | F | 44 | 47 | 35 | 30 | 21 | 351 | 386 | 2 | 3 | ||||
| 19 | Syndromic kyphoscoliosis, Marfan | 4 | F | 72 | 50 | 34 | 19 | 9 | 40 | 12 | 23 | 65 | 218 | 264 | 2 | 1 |
| 20 | Congenital kyphoscoliosis | 3 | F | 70 | 100 | 91 | 46 | 60 | 68 | 39 | 60 | 35 | 201 | 246 | 48 | 82 |
| 21 | Neuromuscular kyphoscoliosis | 7.5 | M | 60 | 67 | 46 | 51 | 18 | 85 | 56 | 39 | 7 | 235 | 283 | 52 | 33 |
| 22 | Congenital kyphoscoliosis | 10 | M | 24 | 70 | 57 | 15 | 67 | 91 | 53 | 3 | 32 | 184 | 251 | 44 | 33 |
| 23 | Congenital scoliosis | 4 | M | 116 | 52 | 44 | 23 | 18 | 67 | 56 | 7 | 18 | 218 | 326 | 5 | 62 |
| 24 | Syndromic kyphoscoliosis, NF, T4-9 | 4.5 | F | 50 | 50 | 74 | 20 | 27 | 68 | 57 | 6 | 5 | 220 | 254 | 3 | 42 |
| 25 | Syndromic (achondroplasia) kyphoscoliosis | 3 | M | 91 | 53 | 29 | 26 | 21 | 54 | 47 | 24 | 27 | 240 | 311 | 8 | 23 |
| 26 | Congenital kyphoscoliosis | 4 | M | 84 | 42 | 41 | 29 | 28 | 32 | 11 | 40 | 33 | 282 | 322 | 57 | 2 |
| p-value (2-tailed) | 0.0005 | 0.9 | 0.0009 | 0.8 | <0.00001 (1-tailed) |
0.6 | ||||||||||
| Average | 5 | 16F & 10M | 62 | 65 | 52 | 34 | 35 | 63 | 41 | 25 | 28 | 246 | 292 | 27 | 29 | |
| Standard Deviation | 3 | 22 | 16 | 18 | 17 | 18 | 20 | 19 | 20 | 19 | 43 | 51 | 20 | 21 | ||
| Maximum | 10 | 116 | 100 | 91 | 72 | 67 | 91 | 57 | 60 | 65 | 351 | 404 | 71 | 82 | ||
| Minimum | 2 | 24 | 42 | 18 | 12 | 2 | 32 | 11 | 3 | 5 | 180 | 193 | 2 | 1 | ||
TGR, traditional growth rods; FU, follow-up; AVT, apical vertebral translation; N/A, they didn’t have abnormal sagittal values and it was purely scoliosis.
The surgical procedure was a modified version of SHILLA (Fig. 1, used with permission), using either the rod to screw (SHILLA screws from Medtronic) sliding mechanism or the analogous rod to domino (4.5 mm rod in 5.5 mm domino hole) sliding mechanism23). In this modified technique, the most wedged vertebra was selected followed by the insertion of pedicle screws in the convex side of the vertebrae above and below the wedged one. No screws were placed on the concave side of the apex. For the growth rod surgery, the domino remained locked, distraction was applied every 6-9 months, and no apical screws were used, Fig. 2. All surgeries were performed under an intraoperative neuromonitor and a C-arm. Additionally, no cast or brace was used for these patients postoperatively. The patients were followed up for an average period of 32 and 62 months in the APC and growth rod groups, respectively. Statistical comparisons (with significance set at ≤ 0.05) were made among the different parameters between the two groups using the t-test (and the Fisher test for gender) with unequal variances in Microsoft Excel. The Cobb angle of the curve in the coronal view was measured from the superior endplate of a superior vertebra to the inferior endplate of an inferior vertebra. Apical vertebral translation was measured as the distance between the center of the thoracic (or lumbar) apical vertebra and the C7 plumb line (or central sacral vertical line). Kyphosis was measured between the most tilted upper endplate of the superior vertebra in the curve to the most tilted inferior endplate of the inferior vertebra. Sagittal balance was measured as the distance of the vertical line drawn from the middle of the body of C7 to the superior-medial border of S1. Spinal length included the whole spine length T1-L5. Coronal balance was measured as the horizontal distance between the vertical line going from C7 to mid-S2.
Figure 1.
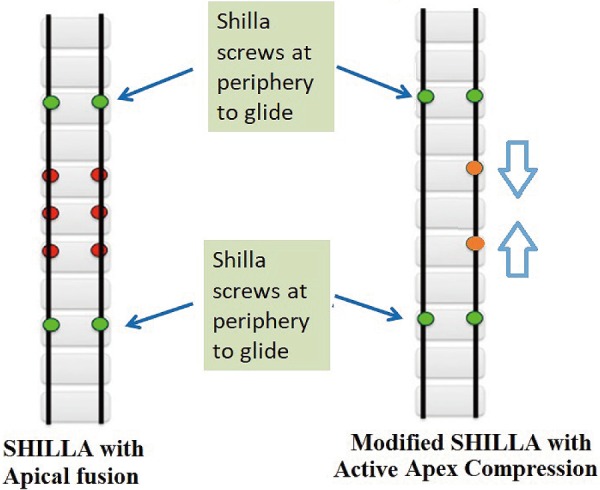
Schematic showing key differences in the established SHILLA procedure and the modified SHILLA (APC) approach used in this study, used with permission23).
Figure 2.
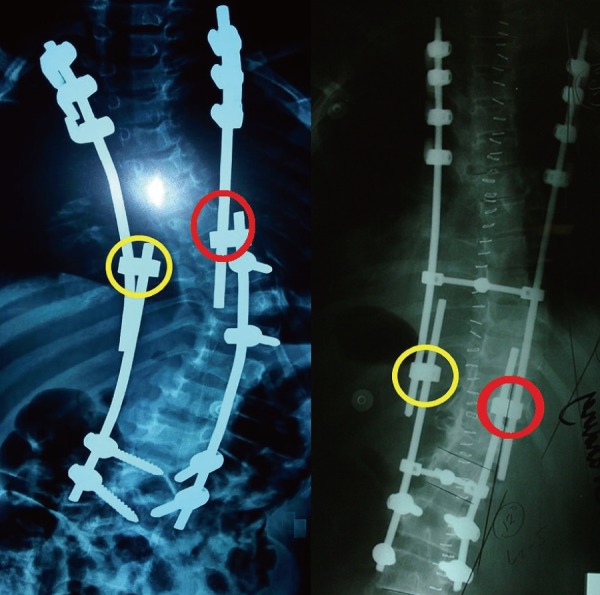
Radiograph of two patients exemplifying the two groups. Left: the APC approach using dominos (4.5 mm rod in 5.5 mm domino hole) for sliding with growth. Right: traditional growth rods. Yellow/red (concave/convex sides, respectively) circles on the left identify the sliding units of this modified SHILLA construct and on the right identify the locked dominos only used for consecutive distraction every 6-9 months.
Results
Both the surgical groups showed significant correction of the Cobb angle and kyphosis (where applicable) at follow-ups (compared with the pre-op values) but no differences between the two groups at follow-up, Table 1 (used with permission) and Table 2, 323). For spinal height gain, after adjusting for differences in the individual follow-up times, there was no statistical difference between the groups (0.8 ± 0.5 mm/month for growth rods vs 1.2 ± 1.6 mm/month for APC), Table 3. Apical vertebral translations and sagittal balance showed no statistical differences between the pre-op and follow-up or between the two surgical groups, Table 1 (used with permission) and Table 2, 3. There was a significant difference (p-value = 0.0006) in coronal balance between APC (12 ± 9 mm) and the growth rod (29 ± 21 mm) approach (at follow-up); there was also a borderline significant difference between the two groups at pre-op (16 ± 17 mm for APC vs 27 ± 20 mm for the growth rod approach, p-value = 0.052). Table 4 summarizes the complication rates at the latest follow-ups.
Table 3.
Statistical Differences between the Two Groups at Pre-op and Follow-up.
| Parameters | Age | Gender | Follow-up time | Cobb angle | AVT | Kyphosis | Sagittal balance | Spine length | Coronal balance | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | FU | Pre | FU | Pre | FU | Pre | FU | Pre | FU | Pre | FU | ||||
| p-value | 0.15 | NS (Fisher test) | 0.00037 | 0.037 | 0.12 | 0.87 | 0.29 | 0.58 | 0.12 | 0.32 | 0.76 | 0.48 | 0.39 | 0.052 | 0.0006 |
NS, not significant; FU, follow-up; AVT, apical vertebral translation
Table 4.
Biomechanical Complications in the Two Groups.
| Biomechanical complications | No. of such complications (n) | |
|---|---|---|
| TGR | APC | |
| Proximal hook dislodgement | 5 | 1 |
| Proximal junctional kyphosis | 2 | 1 |
| New proximal coronal curve | 1 | 0 |
| Distal screw protrusion associated with infection | 1 | 0 |
| Distal screw dislodgement | 1 | 0 |
| Iliac screw and rod loosening | 1 | 1 |
| Dislodgement of iliac screws | 1 | 1 |
| Implant prominence and infection | 1 | 0 |
| Rod fracture | 0 | 1 |
| Total (limited to current follow-up times) | 13 | 5 |
TGR, traditional growth rods; APC, active apex correction
Discussion
This study presents comparative deformity identifiers on the active apex correction, a modified SHILLA procedure, and traditional growth rods with an average follow-up period of 32 and 62 months, respectively. In the former procedure, instead of apical fusion, apex compression was applied at the wedged vertebra. In addition to allowing a foundation for fixation at the apex, traditionally sought to control the curve, this procedure also seeks to dynamically modify the peak of the curve. The immediate benefits of the procedure alone are avoidance of risky osteotomies required to insert screws at the concave end of the apex and more economical surgery (two screws instead of six at the apex of the curve) for underprivileged patients globally with no added risk over SHILLA8,9). Furthermore, in the presence of more than one curve, this procedure is still applicable, whereas the SHILLA technique may not be as practical.
The current study demonstrates equivalent clinical results between the two groups at short to mid-term follow-up. Biomechanical complications were higher with the growth rod system and included the following: new proximal coronal curve (n = 1), distal screw protrusion associated with infection (n = 1), proximal hook dislodgement (n = 5), distal screw dislodgement (n = 1), iliac screw and rod loosening (n = 1), dislodgement of iliac screws (n = 1), implant prominence and infection (n = 1), and proximal junctional kyphosis (n = 2). The APC group included the following complications: dislodgement of iliac screws (n = 1), proximal hook dislodgement (n = 1), iliac screw and rod loosening (n = 1), rod fracture (n = 1), and proximal junctional kyphosis (n = 1). Besides the higher complication rate, which could easily have been due to longer follow-up times with growth rods (compared with APC), traditional growth rods had an obvious surgical disadvantage of repeated invasive procedures for lengthening.
Although one may argue the need for a more homogeneous sample besides the presence of the same surgical team, it is seldom possible for the following reasons: differences in the deformity parameters at pre-op, variability between the construct even within a single surgical group (e.g., using cross-links vs not using cross-links), varied pathogenesis of scoliosis, and overall unpredictable growth and development differences among children with such pathology. The main limitation of the current study is that there was a statistically significant difference between the pre-op values between both groups concerning follow-up time, Cobb angle, and coronal balance. The follow-up times varied because the two surgical methods were used in a consecutive series, as an evolution in the treatment philosophy itself. Nevertheless, the age of surgery and the female to male ratio were similar between the two groups. The differences in Cobb angle were inherent in the data set but not statistically significant at follow-up. However, the differences in coronal balance at pre-op became more prominent (statistically) at follow-up between the two groups. Furthermore, height gain, unlike other parameters, is unidirectionally proportional to follow-up times; that is, it gradually increases with time. Therefore, for accurate comparison we divided the total height for each subject with the follow-up times (duration of growth) and then made a statistical comparison between the two groups (the APC and the growth rod groups).
In conclusion, the result of this study suggests clinical equivalency with respect to correction between the two clinical procedures (APC and traditional growth rod systems) at the current follow-up period. However, the latter procedure presents an obvious disadvantage because it requires multiple surgeries to regularly distract the spine.
Conflicts of Interest: AA reports royalties from Paradigm Spine, Joimax, consultancy from Spinal Balance, Editorial Board membership from Clinical Spine Surgery, Spine, outside the submitted work. LA and AAA have nothing to disclose.
Author Contributions: Each co-author satisfied the four criteria as defined by ICMJE.
References
- 1.McCarthy RE, McCullough FL. Shilla growth guidance for early-onset scoliosis: results after a minimum of five years of follow-up. JBJS. 2015;97(19):1578-84. [DOI] [PubMed] [Google Scholar]
- 2.Andras LM, Joiner ER, McCarthy RE, et al. Growing rods versus Shilla growth guidance: better cobb angle correction and T1-S1 length increase but more surgeries. Spine Deform. 2015;3(3):246-52. [DOI] [PubMed] [Google Scholar]
- 3.Luhmann SJ, McCarthy RE. A comparison of Shilla growth guidance system and growing rods in the treatment of spinal deformity in children less than 10 years of age. J Pediatr Orthop. 2017;37(8):e567-74. [DOI] [PubMed] [Google Scholar]
- 4.Luhmann SJ, Smith JC, McClung A, et al. Radiographic outcomes of Shilla growth guidance system and traditional growing rods through definitive treatment. Spine Deform. 2017;5(4):277-82. [DOI] [PubMed] [Google Scholar]
- 5.Bumpass DB, McCullough L, McCarthy RE. Shilla growth guidance―Evolution of a new procedure: rate of complications in the first two years following implantation in the first 80 patients. Spine J. 2017;17(10):S106-7. [Google Scholar]
- 6.Wilkinson JT, Songy CE, Bumpass DB, et al. Curve modulation and apex migration using Shilla growth guidance rods for early-onset scoliosis at 5-year follow-up. J Pediatr Orthop. 2017. [DOI] [PubMed] [Google Scholar]
- 7.Murphy RF, Mooney III JF. The Crankshaft Phenomenon. JAAOS. 2017;25(9):e185-93. [DOI] [PubMed] [Google Scholar]
- 8.Collins M, Saleh A, Razi A. Evaluation of infantile and juvenile scoliosis and osteotomies in spinal deformity surgery. Curr Orthop Pract. 2018;29(5):440-4. [Google Scholar]
- 9.Ruf M, Jensen R, Letko L, et al. Hemivertebra resection and osteotomies in congenital spine deformity. Spine. 2009;34(17):1791-9. [DOI] [PubMed] [Google Scholar]
- 10.Betz RR, Ranade A, Samdani AF, et al. Vertebral body stapling: a fusionless treatment option for a growing child with moderate idiopathic scoliosis. Spine. 2010;35(2):169-76. [DOI] [PubMed] [Google Scholar]
- 11.Miyanji F, Parent S. Early Onset Scoliosis. Springer, Cham; 2018. Anterior vertebral body tethering (AVBT) for early-onset scoliosis; p. 117-34. [Google Scholar]
- 12.Cebeci BO, Ergene G, Sogunmez N, et al. Non-fusion growth modulation with anterior vertebral body tethering via thoracoscopic approach for adolescent idiopathic scoliosis. Spine J. 2017;17(10):S106-7. [Google Scholar]
- 13.Agarwal A, Goswami A, Vijayaraghavan GP, et al. Quantitative characteristics of consecutive lengthening episodes in early onset scoliosis (EOS) patients with dual growth rods. Spine (Phila Pa 1976). 2019;44(6):397-403. [DOI] [PubMed] [Google Scholar]
- 14.Beaven A, Gardner AC, Marks DS, et al. Magnetically controlled growing rods: the experience of mechanical failure from a single center consecutive series of 28 children with a minimum follow-up of 2 years. Asian Spine J. 2018;12(5):794-802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mak H, Redmond A, Quidwai S, et al. The use of magnetically-controlled growth rods (MCGR) and traditional growth rods (TGR) in a paediatric population. Spine J. 2017;17(11):S331. [Google Scholar]
- 16.Agarwal A, Jayaswal A, Goel VK, et al. Patient-specific distraction regimen to avoid growth-rod failure. Spine. 2018;43(4):E221-6. [DOI] [PubMed] [Google Scholar]
- 17.Agarwal A, Agarwal AK, Jayaswal A, et al. Smaller interval distractions may reduce chances of growth rod breakage without impeding desired spinal growth: a finite element study. Spine Deform. 2014;2(6):430-6. [DOI] [PubMed] [Google Scholar]
- 18.Agarwal A, Agarwal AK, Jayaswal A, et al. Effect of distraction force on growth and biomechanics of the spine: a finite element study on normal juvenile spine with dual growth rod instrumentation. Spine Deform. 2014;2(4):260-9. [DOI] [PubMed] [Google Scholar]
- 19.Agarwal A, Agarwal AK, Jayaswal A, et al. Outcomes of optimal distraction forces and frequencies in growth rod surgery for different types of scoliotic curves: An in silico and in vitro study. Spine Deform. 2017;5(1):18-26. [DOI] [PubMed] [Google Scholar]
- 20.Agarwal A, Jayaswal AK, Goel VK, et al. Letter to the editor concerning “rod fracture and lengthening intervals in traditional growing rods: is there a relationship?” by P. Hosseini et al. Eur Spine J (2016). Eur Spine J. 2017;26(6):1696-7. [DOI] [PubMed] [Google Scholar]
- 21.Agarwal A, Zakeri A, Agarwal AK, et al. Distraction magnitude and frequency affects the outcome in juvenile idiopathic patients with growth rods: Finite element study using a representative scoliotic spine model. Spine J. 2015;15(8):1848-55. [DOI] [PubMed] [Google Scholar]
- 22.Lemans J, Kodigudla M, Kelkar A, et al. Spring distraction system for early onset scoliosis provides continuous distraction without a potential increase in rod fractures, compared to traditional growing rods. Spine Deform. 2018;6(6):819-20. [Google Scholar]
- 23.Agarwal A, Aker L, Ahmad AA. Active apex correction with guided growth technique for controlling spinal deformity in growing children: a modified SHILLA technique. Global Spine J. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]


