Abstract
Introduction
To carry out ultrasound-guided cervical nerve root block (CNRB) safely, we investigated the frequency of risky blood vessels around the target nerve root and within the imaginary needle pathway in the actual injecting position.
Methods
30 patients (20 men, 10 women) with cervical radiculopathy who received ultrasound-guided CNRB were included in this study. We defined a risky blood vessel as an artery existing within 4 mm from the center of the target nerve root or located in the range of 2 mm above or below the imaginary needle pathway.
Results
Using the color Doppler method, the frequency of a risky blood vessel existing around 4 mm from the center of the C5 nerve root was 3.3% (1/30), whereas it was 3.3% (1/30) for the C6 nerve root and 23.3% (7/30) for the C7 nerve root. Hence, the C7 level had more blood vessels close to the target nerve root compared to the C5 and C6 levels, but there was no significant difference (p = 0.0523). On the other hand, the frequency of a risky blood vessel existing within 2 mm above and below the imaginary needle pathway was 3.3% (1/30) for the C5 nerve root, whereas it was 3.3% (1/30) for the C6 nerve root and 10.0% (3/30) for the C7 nerve root. The C7 level had more blood vessels within the needle pathway compared to the C5 and C6 levels, but there was no significant difference (p = 0.301).
Conclusions
To reduce the risk of unintended intravascular injections, more careful checking for the presence or absence of blood vessels at the C7 level using color Doppler is necessary.
Keywords: Cervical spine, Selective nerve root block, Ultrasonography
Introduction
Cervical nerve root block (CNRB) has been used for the diagnosis and treatment of cervical spondylotic radiculopathy1). Ma et al. showed a complication rate of 1.64% in a study of 1,036 CNRB cases, but they also reported six patients with transient neurologic deficits and one patient with global amnesia. Most fatal complications reported have been a result of vertebral artery injury2). Moreover, Takeuchi et al. studied 2,067 patients and revealed a prevalence of 0.6% of anomalies in the vertebral artery entry into the C7 transverse foramen3). Unintended intravascular injections might be caused by unknown accessory features of cervical arteries.
Ultrasound-guided CNRB is considered safer than fluoroscopic CNRB because it can confirm the target nerve and surrounding blood vessels. With the development of ultrasound equipment, ultrasound-guided CNRB has been more frequently used4-7). In a case report on the use of ultrasound-guided CNRB, Narouze et al. could identify the vessels in the needle pathway and suggested that cervical arteries have many more anomalies than what has previously been known6). To carry out ultrasound-guided CNRB safely, we investigated the frequency of risky blood vessels existing around the target nerve root and within the imaginary needle pathway in the actual injecting position.
Materials and Methods
1. Patients
30 patients (20 men, 10 women) with cervical radiculopathy who received ultrasound-guided CNRB from January to November 2018 in our hospital were included in this study. Their mean age was 60.7 (range: 42-80) years. This study was approved by the Institutional Review Board of our institution. All patients provided informed consent to undergo ultrasound examinations. We retrospectively analyzed medical records and ultrasound images.
2. Methods
Ultrasound-guided CNRB was performed with the patients placed in a half-lateral decubitus position (Fig. 1). Before the actual injections, we searched for risky blood vessels at each of the C5, C6, and C7 levels in the affected side using color Doppler ultrasonography with a standard ultrasound device (SNiBLE; Konica Minolta, Tokyo, Japan) and a high-frequency linear probe (L11-3; Konica Minolta).
Figure 1.

Patient position during ultrasound-guided nerve root block. Half-lateral decubitus position. The doctor sits on the back of the patient. Needle penetration direction (parallel method), surgeon’s eye direction, insertion site, and monitor in a straight line.
For beginners, it is difficult to insert the needle without deviating from the target. However, the needle tip does not deviate more than 4 mm from the target even if a beginner performs the procedure, because ultrasound-guided CNRB can be performed while confirming the position of the needle in real time. In previous studies8,9), the insertion error was assumed to be about 4 mm. Thus, we defined a risky blood vessel as an artery existing within 4 mm from the center of the target nerve root (Fig. 2(a)) or located in the range of 2 mm above and below the imaginary needle pathway (Fig. 2(b)). Before the actual injection, pulsatile blood flow was judged as an artery on color Doppler ultrasonography, and the distance between arteries and the center of the target nerve root was measured on the basis of the scale of the ultrasound equipment. Further, a straight line drawn from the upper right end of the screen to the center of the target nerve root was assumed to be the imaginary needle pathway. The distance between arteries and the line was measured on the basis of the scale of the ultrasound equipment. To more accurately diagnose the cervical level responsible for the symptoms, nerve root block was performed with the target nerve root on the “crab-claw structure,” which consists of anterior and posterior tubercles, as close to the nerve compression site as possible10) (Fig. 3).
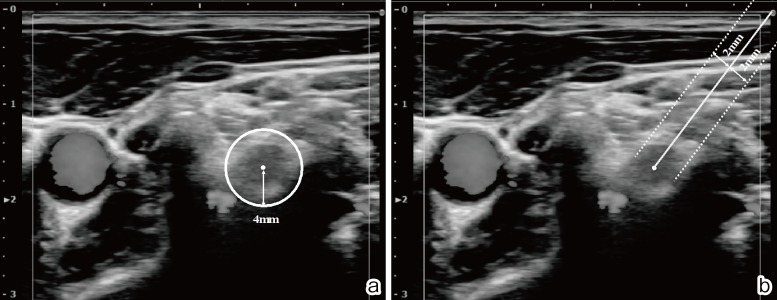
Figure 2.
(a) Risky blood vessel around the target nerve root: when a blood vessel is identified on color Doppler within 4 mm from the center of the target nerve root. (b) Risky blood vessel in the needle insertion pathway: when a blood vessel is identified on color Doppler, located in the range of 2 mm above and below the imaginary needle pathway.
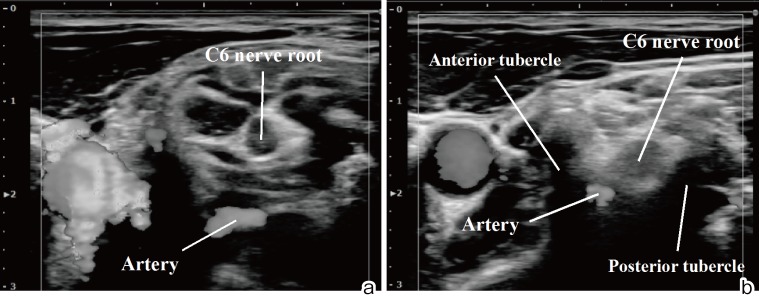
Figure 3.
(a) The target nerve root is positioned more distally than the “crab-claw structure,” which consists of anterior and posterior tubercles. (b) The target nerve root is located in the “crab-claw structure.”
3. Identification method of nerve root elevation
The anatomical features of cervical vertebrae were used to identify the cervical level under ultrasound guidance. An anterior tubercle is in front of the cervical transverse process, and a posterior tubercle is behind it. The nerve root travels through a tubercle groove composed of an anterior tubercle and a posterior tubercle. From the third to the sixth cervical vertebra, there is a tubercle groove consisting of anterior and posterior tubercles; however, the seventh cervical vertebra does not have an anterior tubercle, and the vertebral artery is present along its side (Fig. 4(a)). In the ultrasound image, the tubercle groove looked like a crab claw (Fig. 4(b)), with the nerve root above it. When identifying nerve roots, the crab-claw structures are used as a landmark. A crab claw appears for the first time at the C6 level when the probe is moved to the head side from the C7 level where no crab claw exists because C7 does not have an anterior tubercle (Fig. 4(c)). Using the anatomical features of the cervical vertebrae in such a procedure, it is possible to identify the cervical level.
Figure 4.
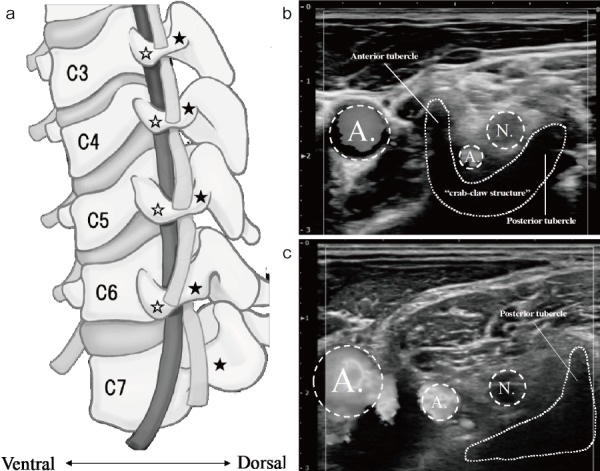
(a) Anatomical features of cervical vertebrae. ☆: anterior tubercle, ★: posterior tubercle. (b) From the third to the sixth cervical vertebra, there is a “crab-claw structure,” which consists of anterior and posterior tubercles. (c) The seventh cervical vertebra does not have an anterior tubercle and the vertebral artery accompanies it. The C7 nerve root on the slope consisting of the posterior tubercle.
4. Statistical analysis
Statistical analyses were performed using JMP (version 14; SAS Inc., Cary, NC, USA), with the level of significance set at p < 0.05.
Results
Using the color Doppler method, the frequency of a risky blood vessel existing around 4 mm from the center of the C5 nerve root was 3.3% (1/30), whereas it was 3.3% (1/30) for the C6 nerve root and 23.3% (7/30) for the C7 nerve root. Thus, the C7 level had more blood vessels close to the target nerve root compared to the C5 and C6 levels, but there was no significant difference (p = 0.0523). On the other hand, the frequency of a risky blood vessel existing within 2 mm above and below the imaginary needle pathway was 3.3% (1/30) for the C5 nerve root, whereas it was 3.3% (1/30) for the C6 nerve root and 10.0% (3/30) for the C7 nerve root. The C7 level had more blood vessels within the needle pathway compared to the C5 and C6 levels, but there was no significant difference (p = 0.301) (Table 1).
Table 1.
Frequency of the Presence of a Risky Blood Vessel.
| C5 | C6 | C7 | |
|---|---|---|---|
| ①RISK AROUND THE TARGET NERVE ROOT | 3.3% (1/30) | 3.3% (1/30) | 23.3% (7/30) |
| ②RISK OF the NEEDLE PATHWAY | 3.3% (1/30) | 3.3% (1/30) | 10.0% (3/30) |
①Risk around the target nerve root: when a blood vessel is identified on color Doppler within 4 mm from the center of the target nerve root.
②Risk of needle pathway: when a blood vessel identified on color Doppler in the range of 2 mm above and below the imaginary needle pathway.
Discussion
Ultrasound-guided CNRB is considered safer than fluoroscopic CNRB because the target nerve and surrounding blood vessels can be confirmed. Nevertheless, blood vessels (including disqualified blood vessels and the like) are also found in the needle pathway, and irreversible damage of the cerebral spinal cord due to the injected medicine is possible; this may occur because of unintended intravascular injections8,9,11). In fluoroscopic nerve root blocks, unintended drug injection into the blood vessel was found to be significantly more common at cervical vertebral levels than at lumbar vertebral levels (31% versus 10%)12). In contrast, the color Doppler method for ultrasound-guided CNRB made it possible to check for the presence of blood vessels around the target nerve root or the needle pathway to prevent inadvertent puncture (Fig. 5). Thus, CNRB can be performed more safely under ultrasound guidance than fluoroscopic guidance. At 2 weeks and 12 weeks after the procedure, no significant differences were found in terms of pain relief with underlying nerve block and ultrasound-guided CNRB; nevertheless, reports revealed that, under ultrasound guidance, it is possible to avoid inadvertent puncture (5/55 cases under fluoroscopy and 0/55 cases under ultrasonography), with no additional radiation exposure4,13,14).
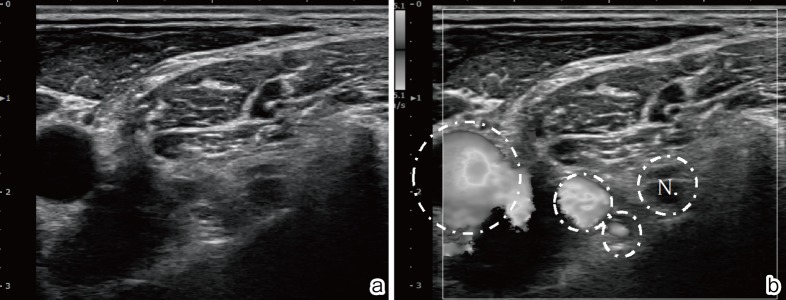
Figure 5.
Effect of the color Doppler. (a) Image of the seventh nerve root. (b) Color Doppler shows the surrounding blood vessels in red or blue signals.
To carry out ultrasound-guided CNRB safely, we investigated the frequency of risky blood vessels around the target nerve root and within the imaginary needle pathway in the actual injecting position. The C7 level had significantly more blood vessels close to the target nerve root compared to the C5 and C6 levels because the vertebral artery runs parallel to the C7 nerve root and then enters the foramen of the C6 transverse process. Therefore, more care is necessary to prevent damage to blood vessels and to implement blocks safely. Clearly, confirmation by color Doppler is useful.
In this study, to more accurately diagnose the cervical level responsible for the symptoms, CNRB was performed with the target nerve root on the “crab-claw structure”, which consists of anterior and posterior tubercles, as close to the nerve compression site as possible (Fig. 3). Therefore, a high risk of inadvertent puncture is possible in any nerve root. If the only aim of nerve root block is pain relief, vessels such as the adjacent vertebral artery can be moved away from the target nerve root by shifting the probe slightly to the periphery (Fig. 4(a)). Using the color Doppler method and slightly adjusting the probe position, it is possible to block more securely by decreasing the frequency of encountering blood vessels around the target nerve root and within the needle pathway.
Conclusion
Ultrasound-guided CNRB has been reported to not only have an equivalent analgesic effect but also pose a lower risk of intravascular injection compared to procedures under fluoroscopy. In this study, more blood vessels were present at the C7 level than at the C5 and C6 levels around the nerve root and in the needle pathway. To reduce the risk of unintended intravascular injections, more careful checking for the presence or absence of blood vessels at the C7 nerve root using color Doppler is necessary.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Author Contributions: Shizumasa Murata wrote and prepared the manuscript. All authors participated in the study design. All authors read, reviewed, and approved the article.
References
- 1.Slipman CW, Lipetz JS, DePalma MJ, et al. Therapeutic selective nerve root block in the nonsurgical treatment of traumatically induced cervical spondylotic radicular pain. Am J Phys Med Rehabil. 2004;83(6):446-54. [DOI] [PubMed] [Google Scholar]
- 2.Ma DJ, Gilula LA, Riew KD. Complications of fluoroscopically guided extraforaminal cervical nerve blocks. An analysis of 1036 injections. J Bone Joint Surg. 2005;87(5):1025-30. [DOI] [PubMed] [Google Scholar]
- 3.Takeuchi M, Aoyama M, Wakao N, et al. Prevalence of C7 level anomalies at the C7 level: an important landmark for cervical nerve ultrasonography. Acta Radiologica. 2016;57(3):318-24. [DOI] [PubMed] [Google Scholar]
- 4.Jee H, Lee JH, Kim J, et al. Ultrasound-guided selective nerve root block versus fluoroscopy-guided transforaminal block for the treatment of radicular pain in the lower cervical spine: a randomized, blinded, controlled study. Skeletal Radiol. 2013;42(1):69-78. [DOI] [PubMed] [Google Scholar]
- 5.Takeuchi M. Progress of cervical nerve root block. Orthopedics & Traumatology. 2015;58:737-41. Japanese. [Google Scholar]
- 6.Narouze SN, Vydyanathan A, Kapural L, et al. Ultrasound-guided cervical selective nerve root block: a fluoroscopy-controlled feasibility study. Reg Anesth Pain Med. 2009;34(4):343-8. [DOI] [PubMed] [Google Scholar]
- 7.Contreras R, Ortega-Romero A. Ultrasound-guided interventional procedures for cervical pain. Tech Reg Anesth Pain Manag. 2013;17(3):64-80. [Google Scholar]
- 8.Lee H, Park D, Oh Y, et al. Ultrasonography evaluation of vulnerable vessels around cervical nerve roots during selective cervical nerve root block. Ann Rehabil Med. 2017;41(1):66-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huntoon MA. Anatomy of the cervical intervertebral foramina- vulnerable arteries and ischemic neurologic injuries after transforaminal epidural injections. Pain. 2005;117(1):104-11. [DOI] [PubMed] [Google Scholar]
- 10.Kang S, Yang SN, Kim SH, et al. Ultrasound-guided cervical nerve root block- does volume affect the spreading pattern? Pain Med. 2016;17(11):1978-84. [DOI] [PubMed] [Google Scholar]
- 11.Park D. Distribution patterns of the vulnerable vessels around cervical nerve roots: a computed tomography-based study. Am J Phys Med Rehabil. 2018;97(4):242-7. [DOI] [PubMed] [Google Scholar]
- 12.Kim DW, Han KR, Kim C, et al. Intravascular flow patterns in transforaminal epidural injections: a comparative study of the cervical and lumbar vertebral segments. Anesth Analg. 2009;109(1):233-9. [DOI] [PubMed] [Google Scholar]
- 13.Ikeura A, Kushida T, Adachi T. Radiation exposure dose at nerve root block. Orthopedics & Traumatology. 2015;58:781-6. Japanese. [Google Scholar]
- 14.Yamashita K, Ikuma H, Tokashiki T, et al. Radiation exposure to the hand of a spinal interventionalist during fluoroscopically guided procedures. Asian Spine J. 2017;11(1):75-81. [DOI] [PMC free article] [PubMed] [Google Scholar]