Abstract
Introduction
In drop finger, the extension of the finger is limited, although the wrist can be flexed dorsally. There have been no well-organized reports on drop finger pattern caused by cervical nerve root disorder. Moreover, diagnosis and treatment are delayed because of the inability to distinguish cervical radiculopathy from peripheral nerve disease. This study aimed to clarify the operative outcome of microscopic cervical foraminotomy (MCF) for cervical radiculopathy presenting drop finger and to investigate whether our classification based on drop finger patterns is useful retrospectively.
Methods
Overall, 22 patients with drop finger who underwent MCF were included. Grip power (GP) and longitudinal manual muscle test (MMT) score of each finger were examined. Drop finger patterns were classified as types I, II, and III. In type I, the extension disorders of the middle and ring fingers are severe and those of index and little fingers are mild. In type II, the extension disorders are severe from the little finger and slightly to index finger. In type III, the extension disorder is consistently severe in all fingers. Perioperative nerve root disorder and paralysis degree were investigated for all types.
Results
The mean GP was significantly postoperatively improved in all 22 patients. The mean MMT score would benefit from exact data for almost all muscles, except the abductor pollicis brevis at the last follow-up. However, pre- and postoperative paralyses were severe in type III patients. C7 nerve root disorder was confirmed in 5/6 type I patients and C8 nerve root disorder in 12/13 type II and 3/3 type III patients.
Conclusions
The operative results of MCF were relatively good, except in type III patients. As a certain tendency was confirmed between the drop finger types and injured nerve roots, our classification may be useful in reducing misdiagnosis and improving the operative results to some extent.
Keywords: drop finger, descensus pattern, C7 nerve root disorder, C8 nerve root disorder, cervical radiculopathy
Introduction
Drop finger is a condition in which the extension of the finger is limited, although the wrist can be flexed dorsally. Patients with drop finger experience difficulty in washing their faces, typing on computer keyboards, and catching dropped or thrown items, owing to limited finger extension, adduction, and abduction. Thus, these patients experience difficulty in activities of daily living and manual labor. Cervical radiculopathy [cervical foraminal stenosis (FS) and lateral cervical disk hernia (lateral CDH)] causes finger numbness, sensory disturbance (S-D), and pain in the scapular or interscapular region and rarely results in drop finger1-3).
Drop finger due to cervical radiculopathy is considered primarily to be a C8 nerve root disorder but may occasionally present as a C7 nerve root disorder. Notably, the difference is not clear4-8). In addition, it is necessary to differentiate cervical radiculopathy from radial nerve palsy, posterior interosseous nerve paralysis (PIN palsy), ulnar nerve palsy, extensor digitorum muscle tendon rupture, and neurologic diseases9-12). Because both the extensor carpi radialis (ECR) and the extensor carpi ulnaris that are mainly innervated by C6 are preserved in C7 and C8 radiculopathy, wrist extension is possible and differentiating cervical radiculopathy from radial nerve palsy is relatively easy; however, PIN palsy and ulnar nerve palsy are difficult to differentiate from C7 or C8 radiculopathy. Furthermore, drop finger with cervical radiculopathy could be misdiagnosed as PIN palsy if these patients do not experience pain, numbness, and S-D in limbs or fingers1). The surgical outcomes of microscopic cervical foraminotomy (MCF) for drop finger due to cervical radiculopathy are typically not good1-4). As mentioned above, this may be the reason why other diseases could not be differentiated from cervical radiculopathy and the operated levels were mistaken. With regard to radial nerve palsy, ulnar nerve palsy, and PIN palsy, characteristic finger forms have been reported and are very useful in their diagnosis13), but there have not yet been any well-organized reports with respect to the drop finger pattern caused by cervical nerve root disorder. Therefore, diagnosis and treatment are delayed because of the inability to distinguish cervical radiculopathy from peripheral nerve disease. Thus, we aimed to elucidate the operative outcome of MCF for cervical radiculopathy presenting drop finger and to investigate whether our classification based on drop finger patterns is useful for diagnosis and treatment retrospectively.
Materials and Methods
Finger extension with a manual muscle test (MMT) score of <3 in a unilateral neutral position of the wrist and with dorsal flexion of the wrist, without weakness in other muscles, was defined as drop finger. In total, 22 patients (18 men, 4 women) with drop finger due to cervical radiculopathy who underwent MCF including herniotomy during a medical examination at our institutions from May 2005 to November 2018 were included in this retrospective study14). The operative criteria included patients who showed no improvement in their condition even after >1 month of the appearance of drop finger.
Classification of the drop finger pattern due to cervical radiculopathy
Three drop finger patterns during maximal extension in the neutral position of the wrist were identified. In type I, the middle and ring finger extension disorders are severe compared with index and little finger extension disorders, and the MMT score of the abductor pollicis brevis (APB) is ≥3. In type II, the degree of severity of extension disorders from the little to the index finger is not the same; the extension disorder of the little finger is most severe, followed by the ring finger, middle finger, and index finger, whereas the index finger extension disorder is mild; the MMT score of APB is ≥3. In type III, all four finger (from index finger to little finger) extension disorders are similarly severe; the MMT score of APB is <3 (Fig. 1). All 22 drop finger patterns were divided into three patterns, and no other patterns were seen.
Figure 1.
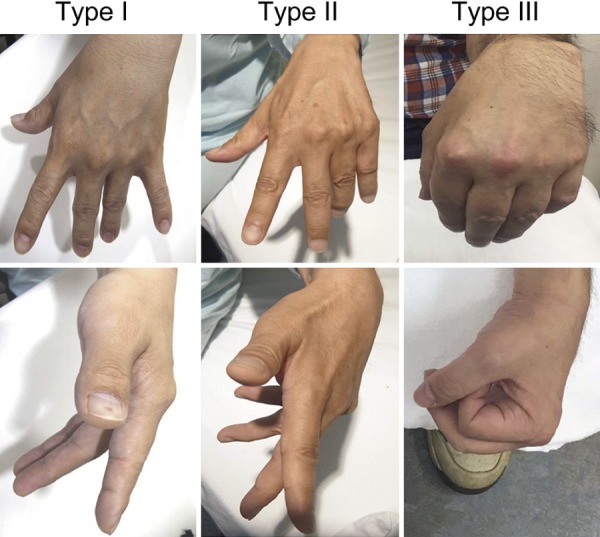
Classification of the drop finger pattern due to cervical radiculopathy in the neutral position of the wrist.
For type I pattern, extension disorders of the middle and ring fingers are severe and those of index and little fingers are mild; the MMT score of APB is ≥3.
For type II pattern, extension disorders are severe (in descending order) from the little finger to the ring finger, middle finger, and (slight) index finger; the MMT score of APB is ≥3.
For type III pattern, extension disorder is consistently severe in all fingers; the MMT score of APB is <3.
Postoperative care
Postoperatively, all patients wore cervical braces for 1 week; a reverse knuckle-bender splint with an outrigger (BUNNELL, CA, USA) was used for patients with severe paralysis15).
Assessment parameters
The following parameters were assessed for all patients: (1) numbness range; (2) S-D range, (3) presence or absence of dorsal interosseous (DI) muscle atrophy; (4) presence or absence of triceps weakness; (5) imaging findings (presence or absence of lateral CDH and/or cervical FS); and (6) electromyography (EMG) results [the ulnar, radial, and median nerves were examined for sensory nerve conduction and motor nerve conduction velocities. Moreover, the biceps brachii, ECR, flexor carpi radialis, triceps, extensor indicis proprius (EIP), extensor digitorum muscle (EDC), APB, first DI, and C8 paraspinal muscle were examined for denervation potential using the polyphasic neuropathic unit in needle EMG]16,17); (7) operative methods; (8) perioperative findings (presence or absence of lateral CDH and/or FS); (9) consistency in imaging findings and perioperative findings; (10) pre- and postoperative grip power (GP); and (11) the mean MMT score, which was investigated for the extensor of the index finger (EIP and EDC), middle finger (EDC), ring finger (EDC), and little finger [the extensor digiti minimi (EDM) and EDC], the interosseous palmaris (measured between the ring and little fingers), the abductor digiti mini (ADM), and APB pre- and postoperatively at 1 month, 6 months, 1 year, and at the last observation. The mean MMT score of each muscle was pre- and postoperatively compared using the Mann-Whitney U test (BellCurve for Excel ver 2.20). In this study, *p<0.05 and **p<0.01 were considered significant.
Moreover, the following parameters were examined in each type of descensus patterns: (12) the frequency of triceps weakness; (13) the frequency of DI atrophy; (14) the presence or absence of C7 and C8 nerve root disorders based on perioperative findings (nerve root disorder was considered present when both operator and assistant identified flattening and hyperemia of the nerve root) (Fig. 2); and (15) the mean MMT score of each muscle with type III pattern, which was compared with those of muscles with other types preoperatively and at the last observation.
Figure 2.
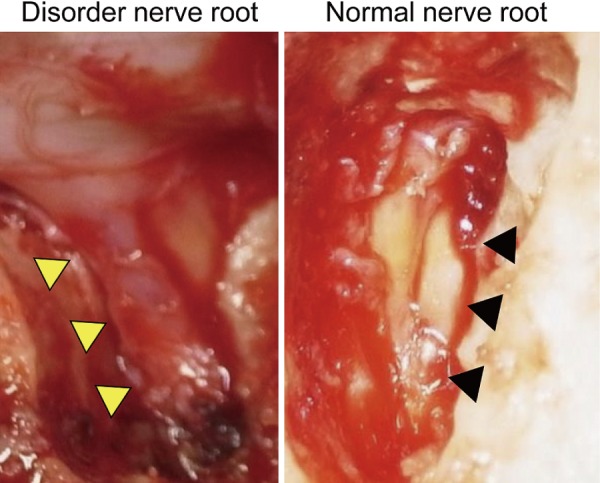
Nerve root disorder and normal nerve root.
The diseased nerve root (yellow arrowheads) shows flattening and hyperemia compared with the normal nerve root (black arrowheads).
The frequencies of parameters 12 and 13 were examined using the chi-square test, whereas those of parameter 15 were examined using the Mann-Whitney U test (BellCurve for Excel ver 2.20). *p<0.05 and **p<0.01 were considered significant.
Results
This study included 22 patients (18 men, 4 women) with drop finger due to cervical radiculopathy who underwent MCF. The average patient age was 60 (range, 40-88) years. The number of patients with right- and left-hand paralysis was 11 each. The mean follow-up period was 13.8 (range, 1-40) months. The mean period from the onset of paralysis to surgery was 5.3 (range, 2-16) months. The mean surgery time was 127 (range, 86-191) min, and the mean bleeding volume was 103 (range, uncountable-470) ml.
The results and summary of each parameter for all the 22 patients are summarized in Table 1, 2, respectively. Numbness and S-D were frequently confirmed from the middle to little fingers. DI atrophy was noted in 41% and triceps weakness in 23% patients. EMG performed in 15 of 22 patients revealed no peripheral neuropathy in all examined patients (7 patients were diagnosed with cervical radiculopathy without using EMG). The operative method was MCF at C6/7 for 1 patient, at C7/Th1 for 5, and at C6/7 and C7/Th1 for 16 patients. Five of the 22 patients underwent prophylactic expansion of the spinal canal because of mild central stenosis.
Table 1.
Types of Pattern, Somatology Findings, Imaging Findings, and Surgery Findings of All 22 Cases.
In the column of Pre-op numbness, 2 means index finger, 3 means middle finger, 4 means ring finger, and 5 means little finger.
| Age | Type | Pre-op Numbness |
Pre-op G/P |
MRI and CT findings | Operative methods | Operative findings | Post-op G/P |
|||
|---|---|---|---|---|---|---|---|---|---|---|
| Hernia | Foraminal stenosis | Hernia | Foraminal stenosis | Injured root | ||||||
| 44 | I | 2, 3, 4 | 21.1 | C6/7 | - | C6/7, C7/Th1 FOM | C6/7 | - | 7 | 43.9 |
| 44 | I | 4, 5 | 32.4 | C6/7 | - | C6 LAM, C6/7, C7/Th1 FOM | C6/7 | - | 7 | 32.7 |
| 72 | I | 4, 5 | Not examined | C7/Th1 | C6/7, C7/Th1 FOM | C7/Th1 | - | 8 | Not examined | |
| 64 | I | 3, 4, 5 | 0 | - | C6/7 | C5-C7 LAM, C6/7 FOM | - | C6/7 | 7 | 12 |
| 62 | I | - | 10 | - | C6/7 | C6 LAM, C6/7, C7/Th1 FOM | - | C6/7 | 7 | 19.3 |
| 88 | I | 3, 4 | Not examined | - | C6/7, C7/Th1 | C5-C6 LAM, C6/7, C7/Th1 FOM | - | C6/7 | 7 | Not examined |
| 47 | II | 3, 4, 5 | 11.5 | C6/7 | C7/Th1 | C6/7, C7/Th1 FOM | C6/7 | C7/Th1 | 7, 8 | 24 |
| 57 | II | - | Not examined | C7/Th1 | - | C6/7, C7/Th1 FOM | C7/Th1 | - | 8 | Not examined |
| 58 | II | - | Not examined | C7/Th1 | - | C7/Th1 FOM | C7/Th1 | - | 8 | Not examined |
| 63 | II | - | Not examined | C7/Th1 | - | C6-C7 LAM, C7/Th1 FOM | C7/Th1 | - | 8 | Not examined |
| 57 | II | 4, 5 | 33 | C7/Th1 | C6/7 | C7/Th1 FOM | C7/Th1 | - | 8 | 37.6 |
| 56 | II | 3, 4, 5 | 30.3 | C7/Th1 | C6/7 | C6/7, C7/Th1 FOM | C7/Th1 | - | 8 | 35.6 |
| 74 | II | 5 | 20 | - | C6/7 | C6/7, C7/Th1 FOM | - | C6/7, C7/Th1 | 7, 8 | 29 |
| 54 | II | 2, 3, 4 | Not examined | - | C7/Th1 | C7/Th1 FOM | - | C7/Th1 | 8 | Not examined |
| 78 | II | 2, 3, 4 | 11 | - | C7/Th1 | C7/Th1 FOM | - | C7/Th1 | 8 | 15 |
| 38 | II | 4, 5 | 27 | - | C6/7, C7/Th1 | C6/7, C7/Th1 FOM | - | C7/Th1 | 8 | 32.6 |
| 43 | II | 4, 5 | 32 | - | C6/7, C7/Th1 | C6/7, C7/Th1 FOM | - | C6/7 | 7 | 44.7 |
| 66 | II | 4, 5 | 19 | - | C6/7, C7/Th1 | C6/7, C7/Th1 FOM | - | C6/7, C7/Th1 | 7, 8 | 22 |
| 70 | II | 4, 5 | 20.3 | - | C6/7, C7/Th1 | C6/7, C7/Th1 FOM | - | C6/7, C7/Th1 | 7, 8 | 34 |
| 55 | III | Unknown | 14.3 | C7/Th1 | C6/7 | C6/7, C7/Th1 FOM | C7/Th1 | - | 8 | 17.4 |
| 60 | III | 3, 4, 5 | 21.2 | - | C6/7 | C6/7, C7/Th1 FOM | - | C7/Th1 | 8 | 27.2 |
| 69 | III | 3, 4, 5 | 14.1 | - | C6/7 | C6/7, C7/Th1 FOM | - | C7/Th1 | 8 | 20.3 |
-, none; FOM, foraminotomy; LAM, laminoplasty
Table 2.
Summary of Parameters.
| I | M | R | L | |
|---|---|---|---|---|
| Numbness (N=18) | 3 | 9 | 15 | 14 |
| S-D (N=10) | 2 | 8 | 9 | 7 |
| DI atrophy | 41% (9/22) | |||
| Triceps weakness | 23% (5/22) | |||
| Imaging findings | C6/7 | C7/Th1 | ||
| CDH (N=10) | 3 | 7 | ||
| FS (N=16) | 13 | 8 | ||
| Operative level | C6/7 | C7/Th1 | C6/7 and C7/Th1 | |
| 1 | 5 | 16 | ||
| Perioperative findings | C6/7 | C7/Th1 | ||
| CDH (N=10) | 3 | 7 | ||
| FS (N=13) | 7 | 9 | ||
| Coincidence image and perioperative findings | CDH | FS | ||
| 100% | 53.80% | |||
| GP | Preoperative | Postoperative | ||
| 19.8 kg | 28 kg* | |||
I, index finger; M, middle finger; R, ring finger; L, little finger; CDH, cervical disk hernia; DI, dorsal interosseous muscle; FS, foraminal stenosis; GP, grip power; S-D, sensory disturbance
GP was significantly improved postoperatively (*p<0.05).
The disk level of lateral CDH occurrence observed during perioperative findings was consistent with that determined using imaging findings. However, the disk level of cervical FS occurrence coincided in only 53.8% of patients. The mean GP was significantly improved on the disorder side postoperatively (*p<0.05).
Muscular strength improvement was noted in either finger in all patients at the 1st postoperative month. At the 1st postoperative month (N = 22), the mean MMT scores were improved for the middle finger (*p<0.05) and ADM (*p<0.05) compared with the preoperative scores. At 6 postoperative months (N = 18), the mean MMT scores were improved for the middle finger (**p<0.01), ring finger (*p< 0.05), and ADM (*p<0.05) compared with the preoperative scores. At the 1st postoperative year (N = 14), the mean MMT scores were improved for the middle finger (**p<0.01), ring finger (**p<0.01), little finger (p<0.05), interosseous palmaris (**p<0.01), and ADM (*p<0.05) compared with the preoperative scores. At the last observation (N = 22), the mean MMT scores were improved for the index finger (*p<0.05), middle finger (**p<0.01), ring finger (**p<0.01), little finger (**p<0.01), interosseous palmaris (**p<0.01), and ADM 3.7 (*p<0.05) compared with the preoperative scores (Fig. 3).
Figure 3.
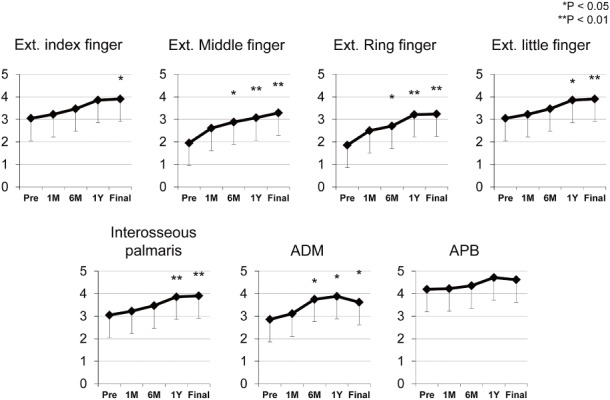
Pre- and postoperative mean MMT score in each muscle.
At the last observation, all muscles, except APB, showed significant improvement (**p<0.01).
The number of type I, II, and III cases was 6, 13, and 3, respectively. Differences between the frequencies of triceps weakness and DI atrophy were not statistically significant among the three types. In patients with type I pattern, abnormal findings of nerve root disorders included radicular flattening and hyperemia; perioperatively, C7 and C8 nerve root disorders were noted in of 5 and 1 patient, respectively. Regarding patients with type II pattern, perioperatively, none of these patients exhibited C7 nerve root disorders alone, 8 exhibited C8 nerve root disorder alone, and 5 exhibited C7 and C8 nerve root disorders. In patients with type III patterns, perioperatively, C8 nerve root disorders were found in all patients.
The preoperative mean MMT score of each muscle in patients with type III pattern (N = 3) was as follows: 1, 1, 1, 1, 1.3, 1.3, and 0.7 for the index finger, middle finger, ring finger, little finger, interosseous palmaris, ADM, and APB, respectively. In other types (N = 18), the mean MMT score was 3.4, 2.2, 2, 2.4, 3.1, 3.1, and 4.7 for the index finger, middle finger (*p<0.05), ring finger (**p<0.01), little finger (**p<0.01), interosseous palmaris, ADM, and APB (**p<0.01), respectively. At the last observation, in patients with type III pattern (N = 3), the mean MMT score was 2.7, 2.7, 2.7, 2.7, 3, 2.7, and 3 for the index finger, middle finger, ring finger, little finger, interosseous palmaris, ADM, and APB, respectively. In other types (N = 18), the mean MMT score was 4.1, 3.4, 3.3, 3.6, 4.1, 3.9, and, 4.8 for the index finger, middle finger, ring finger, little finger, interosseous palmaris, ADM, and APB (**p<0.01), respectively.
The extensor muscles from the middle to little fingers, as well as APB, showed a significantly lower preoperative mean MMT score; moreover, postoperative muscular strength improvement in APB was poor in patients with type III pattern (Table 3).
Table 3.
Characteristics of Each Drop Finger Type.
| Type | N | Muscle weakness of triceps | First DI atrophy | Nerve roots with disorder (perioperative findings) |
||
|---|---|---|---|---|---|---|
| C7 | C8 | C7 and C8 | ||||
| I | 6 | 50% (3/6) | 33% (2/6) | 5 | 1 | 0 |
| II | 13 | 23% (3/13) | 31% (4/13) | 0 | 8 | 5 |
| III | 3 | 66% (2/3) | 100% (3/3) | 0 | 3 | 0 |
DI, dorsal interosseous muscle
( ) represents the number of cases.
Discussion
After MCF, muscular strength improvement of either finger was noted at the 1st postoperative month along with significantly improved MMT scores of all muscles, except that of APB at the last observation compared with the preoperative score. Unexpectedly, these results were relatively good. However, the surgical results in type III patients were poor, when the drop finger pattern due to cervical radiculopathy was classified into three types.
In this study, drop finger did not improve for an average of 5 months from the onset of paralysis without surgical treatment; therefore, it is resistant to conservative management. Moreover, misdiagnosis or inappropriate diagnosis can delay treatment. As a characteristic of drop finger due to cervical radiculopathy, numbness and S-D ranges frequently involved the middle to little fingers. Moreover, triceps weakness was also noted, similar to that noted in a previous report1). However, some patients did not experience numbness and triceps weakness. Furthermore, it was particularly difficult to diagnose FS solely on the basis of imaging findings, and many patients were diagnosed only after we confirmed nerve root disorder via perioperative findings.
Initially, we seem to indicate that case reports of drop finger provide inadequate details of the postures, and then we say that the postures reported in case reports correspond well to our classification system1,6,8). Thus, we devised a classification from drop finger postures to avoid misdiagnosis of diseases and nerve root disorders.
In type I pattern, index and little finger extensions are relatively stable, although the middle and ring fingers hang down; this is a very specific finger posture, which is not observed in peripheral nerve disorders. The surgical results for this type were relatively good. Because some anatomy books have described that both C7 and C8 nerve roots similarly innervate EIP, EDC, EDM, and triceps (Table 2), we cannot explain why the descensus degree between the index and little fingers was the same; however, these degrees differed from those of the middle and ring fingers18-21). We found that 5 of 6 patients with type I pattern exhibited C7 nerve root disorders, as noted perioperatively. Moreover, we found that 1 patient in this study showed improvement at C6/7 alone using MCF, which is consistent with the findings in a patient with similar descensus pattern reported by Hori et al6). Thus, type I patterns may mainly be associated with C7 nerve root disorders.
In patients with type II pattern, the little finger exhibits the greatest descensus with a decreasing degree of descensus in the ring, middle, and index fingers; this explains most of the cases that we encountered. The surgical results for this type were relatively good. Although this type may resemble the pattern observed due to tendon rupture in EDM, drop finger caused by cervical radiculopathy limits the extension of the little finger and other extensors, making differentiation easy. Furthermore, Campbell et al. reported the posture between the ring and little drop fingers, which was similar to that observed in type II pattern, and named it pseudo-pseudo ulnar claw hand8). Differentiating claw hand due to ulnar nerve disorder from drop finger due to cervical radiculopathy is based on the posture at finger extension. A hand in the ulnar claw position has the ring and little fingers extended at the metacarpophalangeal (MCP) joints and flexed at the interphalangeal (IP) joints. In contrast, drop finger due to cervical radiculopathy has both ring and little fingers extended at IP joints and flexed at MCP joints13). These patients experience difficulty in delicate activities, including typing on computer keyboards; therefore, ADM, interosseous palmaris with C8 innervation, and finger extensor muscle exhibited weakness (Table 2)18-22). Four patients who underwent MCF only at the C7/Th1 level exhibited type II pattern; all the 4 patients showed improvement, and 12 cases with C6/7 and C7/Th1 MCF showed C8 nerve root disorders, as confirmed on the basis of perioperative findings. Based on these facts, type II pattern is considered the primary descensus pattern of C8 nerve root disorders.
In type III pattern, all extensor muscles and the APB were found to be severely paralyzed; this pattern showed the highest similarity with that observed in severe PIN palsy. Thus, this pattern is accompanied with a risk that neurolysis may be performed for PIN palsy and that cervical radiculopathy may be overlooked. Therefore, EMG is necessary to differentiate cervical radiculopathy from PION. Tanaka et al. reported a pattern similar to our type III pattern; they noted drop finger in almost all C8 nerve root disorders and suggested that their observed pattern may be a representative finger posture of C8 nerve root disorders1). EIP, EDC, and EDM with common C7 and C8 innervation showed weakness similar to DI, ADM, and APB with only C8 innervation18-22). Therefore, this pattern may be associated with C8 nerve root disorders. In the present report, 3 patients were classified with type III pattern, and C8 nerve root disorder was confirmed for all these patients based on perioperative findings. Preoperative paralysis was severe in these patients, and it was difficult for them to catch things postoperatively because of reduced APB muscular strength. Therefore, it is necessary to consider the postoperative effects on activities of daily living and manual labor.
Limitations
The primary limitation of this study is its retrospective nature and small sample size. Moreover, the classification was subjectively biased because both the operator and the assistant judged nerve root disorders based on perioperative findings. Therefore, additional cases are necessary to confirm these findings.
Conclusions
The operative outcomes of MCF for cervical radiculopathy presenting drop finger were relatively good, but the surgical results for only type III patterns were poor. Type I pattern is specific for cervical radiculopathy and usually indicates C7 root injury, but C8 is also possible. Type II pattern appears most commonly with C8 root injury. Type III pattern is caused by C8 injury, but due to similar clinical presentation to PIN palsy, EMG is necessary to distinguish between the two.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Acknowledgement
We thank Dr. Yasuhisa Tanaka, Dr. Yusuke Kawano, and Dr. Hirokazu Tochigi for their critical assistance.
References
- 1.Tanaka Y. Drop fingers caused by cervical radiculopathies: its features in symptomatologies. Orthop Surg Traumatol. 2006;49(11):1261-7. Japanese. [Google Scholar]
- 2.Tanaka Y, Kokubun S, Sato T, et al. Cervical roots as origin of pain in the neck or scapular regions. Spine (Phila Pa 1976). 2006;31(17):E568-73. [DOI] [PubMed] [Google Scholar]
- 3.Mizutamari M, Sei A, Tokiyoshi A, et al. Corresponding scapular pain with the nerve root involved in cervical radiculopathy. J Orthop Surg. 2010;18(3):356-60. [DOI] [PubMed] [Google Scholar]
- 4.Kawada T, Tani S, Taniguchi S, et al. [Clinical features in patients with C8 radiculopathy]. Cent Jpn J Orthop Surg Traumatol. 2008;51(3):521-2. Japanese. [Google Scholar]
- 5.Kaneko K, Taguchi T, Toyoda K, et al. Unilateral drop finger due to cervical spondylosis at the C6/7 intervertebral level. J Orthop Sci. 2003;8(4):616-20. [DOI] [PubMed] [Google Scholar]
- 6.Hori J, Nakamura S, Murao T, et al. Clinical results of surgical treatment for unilateral drop finger due to cervical radiculopathy. Cent Jpn J Orthop Surg Traumatol. 2014;57(6):1241-2. Japanese. [Google Scholar]
- 7.Wallace D. Disc compression of the eighth cervical nerve: pseudo ulnar palsy. Surg Neurol. 1982;18(4):295-9. [DOI] [PubMed] [Google Scholar]
- 8.Campbell WW, Buschbacher R, Pridgeon RM, et al. Selective finger drop in cervical radiculopathy: the pseudopseudo ulnar claw hand. Muscle Nerve. 1995;18(1):108-10. [DOI] [PubMed] [Google Scholar]
- 9.Kleinert JM, Mehta S. Radial nerve entrapment. Orthop Clin North Am. 1996;27(2):305-15. [PubMed] [Google Scholar]
- 10.Goldman S, Honet JC, Sobel R, et al. Posterior interosseous nerve palsy in the absence of trauma. Arch Neurol. 1969;21(4):435-41. [DOI] [PubMed] [Google Scholar]
- 11.Omer GE Jr. Green's operative hand surgery. 3rd ed. Philadelphia (The United States of America): Churchill Livingstone; c1999. Chapter 49, Ulnar nerve palsy; p. 1526-41. [Google Scholar]
- 12.Leslie BM. Rheumatoid extensor tendon ruptures. Hand Clin. 1989;5(2):191-2. [PubMed] [Google Scholar]
- 13.Carp SJ. Peripheral nerve injury: an anatomical and physiological approach for physical therapy intervention. 1st ed. Philadelphia (The United States of America): F.A. Davis Company; c2015. Chapter 5, Special considerations; p. 292-302. [Google Scholar]
- 14.Fessler RG, Khoo LT. Minimally invasive cervical microendoscopic foraminotomy: an initial clinical experience. Neurosurgery 2002;51(5 Suppl):S37-45. [PubMed] [Google Scholar]
- 15.Carp SJ. Peripheral nerve injury: an anatomical and physiological approach for physical therapy intervention. 1st ed. Philadelphia (The United States of America): F.A. Davis Company; c2015. Chapter 4, Rehabilitative procedural intervention for peripheral nerve injury; p. 212-4. [Google Scholar]
- 16.Dumitru D. Single muscle fiber discharges (insertional activity, end-plate potentials, positive sharp waves, and fibrillation potentials): a unifying proposal. Muscle Nerve. 1996;19(2):221-6; discussion 227-30. [DOI] [PubMed] [Google Scholar]
- 17.Dumitru D, King JC, McCarter RJ. Single muscle fiber discharge transformations: fibrillation potential to positive sharp wave. Muscle Nerve. 1998;21(12):1759-68. [DOI] [PubMed] [Google Scholar]
- 18.Michael S, Erik S, Udo S. Prometheus. LernAtlas der Anatomie. Allgemeine Anatomie und Bewegungssystem. 2nd ed. Stuttgart (Germany); Auflage: Thieme; c2005. Chapter Obere Extremitat 2. Systematik der Muskulatur; p. 274-82. [Google Scholar]
- 19.Hoppenfeld S, Hutton R. Physical examination of the spine and extremities. 1st ed. New York (The United States of America): Prentice-Hall, Inc.; c1976. Physical examination of the cervical spine; p. 118-24. [Google Scholar]
- 20.Murphey F, Simmons JCH, Brunson B. Surgical treatment of laterally ruptured cervical disc. Review of 648 cases, 1939 to 1972. J Neurosurg. 1973;38(6):679-83. [DOI] [PubMed] [Google Scholar]
- 21.Haymaker W, Woodhall B. Peripheral nerve injuries principles of diagnosis. 2nd ed. Philadelphia (The United States of America): W.B. Saunders; c1967. Chapter 6, movements tested in neurological examinations; p. 87-102. [Google Scholar]
- 22.Yoss RE, Corbin KB, MacCarty CS, et al. Significance of symptoms and signs in localization of involved root in cervical disk protrusion. Neurology. 1957;7(10):673-83. [DOI] [PubMed] [Google Scholar]


