Abstract
Background:
Interest in double-row techniques for arthroscopic rotator cuff repair has increased over the last several years, presumably because of a combination of literature demonstrating superior biomechanical characteristics and recent improvements in instrumentation and technique. As a result of the increasing focus on value-based health-care delivery, orthopaedic surgeons must understand the cost implications of this practice. The purpose of this study was to examine the cost-effectiveness of double-row arthroscopic rotator cuff repair compared with traditional single-row repair.
Methods:
A decision-analytic model was constructed to assess the cost-effectiveness of double-row arthroscopic rotator cuff repair compared with single-row repair on the basis of the cost per quality-adjusted life year gained. Two cohorts of patients (one with a tear of <3 cm and the other with a tear of ≥3 cm) were evaluated. Probabilities for retear and persistent symptoms, health utilities for the particular health states, and the direct costs for rotator cuff repair were derived from the orthopaedic literature and institutional data.
Results:
The incremental cost-effectiveness ratio for double-row compared with single-row arthroscopic rotator cuff repair was $571,500 for rotator cuff tears of <3 cm and $460,200 for rotator cuff tears of ≥3 cm. The rate of radiographic or symptomatic retear alone did not influence cost-effectiveness results. If the increase in the cost of double-row repair was less than $287 for small or moderate tears and less than $352 for large or massive tears compared with the cost of single-row repair, then double-row repair would represent a cost-effective surgical alternative.
Conclusions:
On the basis of currently available data, double-row rotator cuff repair is not cost-effective for any size rotator cuff tears. However, variability in the values for costs and probability of retear can have a profound effect on the results of the model and may create an environment in which double-row repair becomes the more cost-effective surgical option. The identification of the threshold values in this study may help surgeons to determine the most cost-effective treatment.
Level of Evidence:
Economic and decision analysis Level II. See Instructions for Authors for a complete description of levels of evidence.
Rotator cuff repair represents one of the most common indications for shoulder surgery, and has been considered a cost-effective intervention compared with other medical or surgical approaches1. Over the last decade, the literature has established that functional outcomes after arthroscopic repair are comparable with those after open surgical techniques2–5. Recently, traditional single-row fixation methods for arthroscopic rotator cuff repair have been called into question over concerns of fixation strength and repair integrity6. Arthroscopic double-row repairs were designed to increase the tendon-bone contact area, creating a reconstruction with a more anatomic footprint7. Several studies have demonstrated an improved in vitro biomechanical advantage with double-row techniques5,8,9, and clinical studies have shown a lower rate of retear after double-row techniques than after single-row techniques6,10. However, as far as we know, no clinical study to date has demonstrated that the improved healing rates and the recreation of a more anatomic footprint translate into a functional improvement in patient outcomes11–13. Despite the paucity of evidence showing a clinical benefit from double-row repair, many surgeons continue to practice arthroscopic double-row rotator cuff repair on the basis of the in vitro and theoretical benefits of this technique. Arthroscopic double-row repair techniques rely on multiple additional points of fixation, most commonly achieved via arthroscopic suture anchors. This additional utilization of surgical implants, combined with the increase in operative time associated with placement of this second row of fixation, adds to the direct surgical costs associated with arthroscopic rotator cuff repair.
In 2008, the United States spent more than $2.3 trillion on health care or roughly 16% of the gross domestic product. This figure is three times the amount spent in 1990, which comprised 12.2% of the gross domestic product14. As a result, studying the cause of this growth to determine methods of curbing costs has become a major public policy priority. Within orthopaedic surgery, it is critical that we examine our interventions to ensure that patients with musculoskeletal disorders receive the most cost-effective treatments.
To date, no study has examined the relationship between the added costs of double-row rotator cuff repair and the potential benefit from establishing a more anatomic footprint for healing. The purpose of this study was to determine, with use of currently available data, whether arthroscopic double-row rotator cuff repair represents a cost-effective alternative to traditional single-row arthroscopic fixation techniques.
Materials and Methods
Patients
A cost-effectiveness model was constructed to represent a typical cohort of patients with a rotator cuff tear who would be appropriate for arthroscopic reconstruction (the so-called base case). A recent study by Sherman et al. characterized the demographic characteristics of a patient undergoing rotator cuff repair11. Within the cohort of 52,485 patients, the average age was fifty-six years, and 56.6% of the patients were male. All patients in our model are assumed to have tear morphologies that would be ideally suited for arthroscopic intervention by means of a single or double-row approach. Patients were divided into two separate cohorts with respect to tear size: small or medium tears (<3 cm) and large or massive tears (≥3 cm). The costs, utilities, and probabilities described below reflect parameter estimates that best represent this population.
Model Design
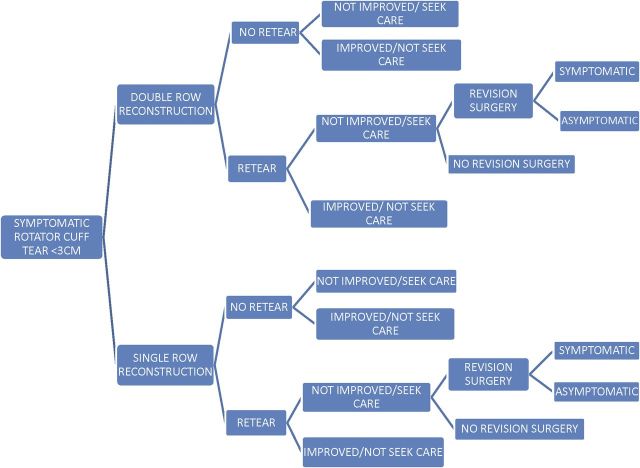
We used a decision-analytic model to determine whether single-row or double-row repair was most cost-effective for the management of a typical population of patients with a rotator cuff tear. The use of cost-effectiveness analyses in health care began in the late 1960s and has been widely recognized by both governmental and nongovernmental payers to be a valid tool to assess health-care decisions12. In order to stratify our analysis on the basis of tear size (<3 cm and ≥3 cm), two models with identical structure, but differing probabilities, were created. A schematic depiction of the cost-effectiveness model (tears of <3 cm) is shown in Figure 1.
Fig. 1.
A simplified decision tree for patients having primary rotator cuff surgery for tears of <3 cm. An identical additional model was created for tears of ≥3 cm (not shown).
The model is structured to follow a patient with a symptomatic rotator cuff tear for two years after the initial surgery, and was chosen because of the currently available data on long-term follow-up for double-row repair13. Initially, patients were assigned to either arthroscopic single or double-row repair. Postoperatively, patients could have a retear of the repaired tendon(s) (“retear”) or the rotator cuff could remain intact (“no retear”). Retear was defined by imaging evidence (magnetic resonance imaging [MRI], ultrasound, or arthrogram) of a tendon that was not in continuity. Individuals in each of these groups could either be improved from the initial surgery (“improved/not seek care”) or not improved (“not improved/seek care”). Individuals with a retear on imaging studies who were not improved could either undergo revision surgery (“revision surgery”) or be treated nonoperatively (“no revision surgery”), and revision surgery could result in improvement in patient symptoms (“asymptomatic”) or no improvement in patient symptoms (“symptomatic”).
In order to complete the model structure above, the following assumptions were made: (1) Patients could only undergo one revision surgery, (2) individuals who had improvement from the initial surgery did not choose to seek further surgical or nonoperative treatment, (3) individuals who had not had improvement were assumed to seek further operative or nonoperative care, and (4) individuals who had not had improvement and had no evidence of retear were assumed to undergo nonoperative treatment; however, further exploration of the possible etiologies of their persistent symptoms was not modeled and was determined to be out of the scope of this analysis.
Each terminal health state was given a defined cost and quality-adjusted life year (QALY) value. QALYs are estimated on the basis of the amount of time spent in each health state and the value of a particular health state with use of “health utilities” or preference weights, which typically range from 0 (assumed equivalent to death) to 1 (equivalent to perfect health). Costs and utilities occurring over time were discounted at an annual rate of 3%, which is consistent with current practices in cost-effectiveness analysis15. As patients move through the model, they are assigned costs and QALYs, which are used to evaluate the cost-effectiveness of the double-row repair relative to single-row rotator cuff repair. The model was constructed with the use of decision analysis software (TreeAge Pro 2009; TreeAge Software, Williamstown, Massachusetts).
Model Parameters
Costs
Costs were estimated on the basis of direct medical costs regardless of the payer and are reported in 2009 U.S. dollars. A societal perspective was utilized to capture both the direct and indirect costs associated with an episode of care. A ratio of cost to charges of 0.63, which is consistent with prior cost analyses for rotator cuff surgery, was utilized1. Use of a ratio of cost-to-charges methodology has been found to be a reliable method for comparing patients in a specific diagnosis-related group at one hospital with those at another hospital16,17.
Vitale et al. used a societal perspective with a breakdown of both hospital and provider costs associated with rotator cuff repair presented in Table I1. With use of these data, the cost associated with single-row repair was assigned at $10,605. The incremental cost associated with double-row rotator cuff repair was determined from institution-specific data and included additional implants utilized as well as the increase in operative time associated with implantation of the second row. A baseline of two additional anchors and fifteen minutes of operative time was assumed for the double-row technique. A baseline incremental cost of $1309 was estimated for a total cost of $11,914 for double-row repairs.
TABLE I.
Assumption of Costs Using the Ratio of Cost-to-Charge Method of 0.63 from Vitale et al.1
| Cost ($) | Standard Deviation ($) | Source of Data | |
| Single row | |||
| Hospital | 6927 | 1354 | Vitale et al.1 |
| Physician | 3678 | 2072 | Vitale et al.1 |
| Total for single row | 10,605 | 2566 | Vitale et al.1 |
| Incremental costs* | |||
| Implants | 784 | ||
| Operating-room time | 525 | ||
| Total incremental | 1309 | ||
| Total for double row | 11,914 | ||
| Physical therapy | 1920 | Moosmayer et al.18 | |
| Revision surgery (total for single row and physical therapy) | 12,525 | ||
Incremental costs obtained from institutional data.
The costs of nonoperative treatment for recurrent rotator cuff tears were estimated in a study by Moosmayer et al. comparing operative with nonoperative (physical therapy) treatment of rotator cuff tears18. This cost was based on the average cost per visit and average number of physical therapy visits and was estimated at a total of $1920.
Estimated revision surgery costs were based on the following assumptions: (1) Patients would undergo a trial physical therapy prior to revision surgery, and (2) hospital and provider costs for revision after failure of both single and double-row repair are equal to the base costs estimated by Vitale et al.1, as the ability to characterize the exact nature of these revision surgeries is difficult and has not been reported in the literature, as far as we know.
Utilities
Quality-adjusted life years represent a well-accepted method to measure the disease burden on both quality and quantity of life. QALYs can be determined by utility scores collected either directly from patients (for example, standard gambles) or from generalized health questionnaires (for example, the EuroQol 5D [EQ-5D]19 or the Short Form-36 [SF-36]20) with scores ranging from 0 (death) to 1 (perfect health). The utility score is then multiplied by the amount of time in the specific health state to determine the QALYs. To estimate QALYs, utilities for patients with a symptomatic rotator cuff tear were taken from the literature and were based on Health Utilities Index values1 (Table II). In order to apply these published utilities to our model, the following assumptions were made: (1) Patients who were improved (“improved/not seek care”) from the initial surgery were assigned a utility value equal to the published value of successful primary rotator cuff repair regardless of the presence or absence of a tear on imaging studies, and (2) patients who were not improved or remained symptomatic (“not improved/seek care” or “symptomatic”) were assigned a utility value equal to the published value of a symptomatic rotator cuff tear.
TABLE II.
Utility Health State Scores for Patients with Rotator Cuff Tears After Repair and the Disutilities Associated with Revision Surgery
A utility for patients who were improved after revision surgery (“asymptomatic”) was derived from the time spent in the symptomatic rotator cuff tear state and the successful rotator cuff repair state. Huijsmans et al. demonstrated that a large proportion of both large and small rotator cuff repairs fail within the first three weeks21. As such, patients were assigned the reported utility of an intact rotator cuff for three weeks of the two-year time horizon, and for the remainder of this time period they were assumed to have a health utility equal to a torn rotator cuff as reported in the literature1. To account for a loss in health utility in patients undergoing revision surgery, a “disutility” (i.e., a decrement in health utility) for revision surgery was assigned to all patients who entered the revision surgery portion of the model. This was calculated by assigning a proportion of the total age-based health utility that reflected their level of health during the period of convalescence22.
Probabilities
Probabilities for retear on imaging studies after both single and double-row repair for tears of <3 cm and tears of ≥3 cm were reported in a 2010 systematic review of the cases of 1252 patients by Duquin et al.13 (Table III). The probability of retear after double-row reconstruction was expressed in our model as a function of single-row repair as it allows for the two values to vary with each other by simply changing one value. This more accurately represents the healing potential on the basis of the patient’s clinical scenario. For example, if the model were changed to reflect a patient who had a higher probability of retear with single-row repair (for example, one who had a history of smoking), then the probability of retear after double-row repair should also increase concomitantly. An additional variable, “retear factor,” which represents a ratio of the radiographic retear proportion for single-row compared with double-row repair, was created. This was generated to capture the relative benefit of double-row over single-row repair as it pertains to imaging retear proportion, and would allow for an assessment of the model if this ratio were ranged over a broad range of values. Klepps et al. reported patient satisfaction outcomes after open rotator cuff repair on the basis of the presence or absence of retear as assessed by MRI23. That study was used to determine the probability of a patient entering the “not improved/seek care” state, given the presence or absence or radiographic retear, and is rooted in the assumption that the probabilities would hold true for arthroscopic repair (Tables III and IV). That study was also used, in conjunction with a 2010 study by Keener et al.24, to calculate the probability of a patient entering the “symptomatic” state after revision repair (Table IV).
TABLE III.
Probabilities for Radiographic Retear and Revision
| Parameter | Tears of <3 cm | Tears of ≥3 cm | Source of Data |
| Single-row retear | 0.2 | 0.44 | Duquin et al.13 |
| Double-row retear | 0.6* | 0.27† | Duquin et al.13 |
| Revision | 0.3 | 0.73 | Keener er al.24 |
Single-row probability times 0.3.
Single-row probability times 0.61.
TABLE IV.
Rates of Shoulders with and without Symptoms After Initial Surgery and After Revision Surgery*
| Parameter | Asymptomatic Shoulders (%) | Symptomatic Shoulders (%) |
| Healed | 95 | 5 |
| Retear | 80 | 20 |
| Revision of small tear | 94 | 6 |
| Revision of large tear | 85 | 15 |
Data are from Klepps et al.23
The probability of revision surgery, given the presence of a retear on imaging studies and the absence of improvement, was estimated at 10%. No published data that would provide an accurate estimate of this value are currently available, as far as we know. This probability was ranged through all plausible values (0% to 100%) in our model to assess the impact of this value on the output of the model.
Analysis
Using this model, we evaluated two treatment strategies by calculating the incremental cost-effectiveness ratio, defined as the difference in expected costs divided by the difference in expected QALYs for the two approaches to rotator cuff repair. Incremental cost-effectiveness ratios are reported as cost per QALY gained for double-row repair relative to single-row repair. We used an incremental cost-effectiveness ratio of <$100,000 per QALY gained to be the threshold defining a cost-effective modality, a commonly used threshold for determining cost-effectiveness25. The effects of variation in probabilities, costs, and utilities on the cost-effectiveness of each strategy were examined with use of sensitivity analyses. Any variable that altered the preferred strategy was reported.
Source of Funding
There was no source of external funding for this study.
Results
Base Case Analysis
For both rotator cuff tears of <3 cm and those of ≥3 cm, single-row rotator cuff repair is less costly than double-row repair. On the basis of the costs, QALYs, and probabilities used in our base case, double-row reconstruction resulted in an increased overall cost of $1238 and increased effectiveness of 0.0022 QALY for rotator cuff tears of <3 cm. Similarly, double-row reconstruction resulted in an increased overall cost of $1222 and an increased effectiveness of 0.0027 QALY for tears of ≥3 cm. These values resulted in incremental cost-effectiveness ratios of $571,500 and $460,200 per QALY gained for rotator cuff tears of <3 cm and those of ≥3 cm, respectively.
Sensitivity Analysis
In the base case analysis, the radiographic proportion of repair failure (retear proportion) was assumed to be 20% following single-row and 6% following double-row repair for tears of <3 cm versus 44% for single-row and 27% for double-row repair for tears of ≥3 cm (Table III)13. When the proportions of radiographic retear following both single-row and double-row repair were ranged between the extremes reported in the literature, the incremental cost-effectiveness ratio for double-row repair for both the small to medium (<3 cm) and large to massive (≥3 cm) tears never fell below the threshold value of $100,000/QALY gained.
Patients who sustained a rotator cuff tear after the initial surgery (a retear) were presumed to have symptoms of this tear substantial enough to seek further treatment 20% of the time (Table IV), whereas patients whose repair remained intact after the initial surgery had a fair or poor result in 5% of the cases. These variables were ranged throughout all possible values, for both tears of <3 cm and tears of ≥3 cm. If >63% of patients with a tear of ≥3 cm sought additional care for a recurrent tear, then double row-repair became cost-effective. For initial tears of <3 cm, if >76% of patients were symptomatic following retear, then double-row repair was a cost-effective initial surgical option. The rate at which patients underwent revision surgery had no impact on the overall cost-effectiveness of double-row repair.
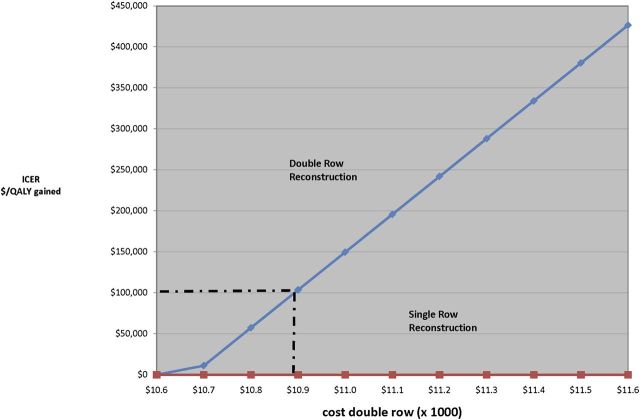
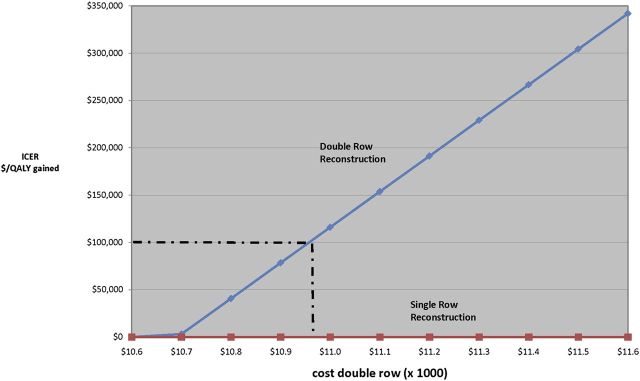
The cost of single-row and double-row repair was assigned at $10,605 and $11,914, respectively. A sensitivity analysis on the added cost of double-row repair indicates that, if double-row surgery could be reduced to <$10,892 for small tears and to <$10,957 for large tears, then the cost/QALY gained would decrease to <$100,000 and double-row repair would be a cost-effective surgical alternative (Figs. 2-A and 2-B). This translates into an incremental cost of $287 and $352 for tears of <3 cm and tears of ≥3 cm, respectively.
A one-way sensitivity analysis evaluating the cost of double-row repair (a baseline of $11,914) compared with incremental cost-effectiveness ratio (ICER) for tears of <3 cm (Fig. 2-A) and tears of ≥3 cm (Fig. 2-B). The dashed line indicates the threshold value of $100,000/QALY (quality-adjusted life year) under which double-row repair becomes cost-effective.
Fig. 2-A.
Fig. 2-B.
Both the costs associated with nonoperative and revision surgery are uncertain. Given the wide variation of nonoperative treatment, the sensitivity analysis was varied from $0 to $10,000 (no treatment to the cost of primary surgery), and it had no effect on the outcome regardless of tear size. Values for revision surgery could also vary widely. A sensitivity analysis between one and two times the cost of primary surgery ($10,605 to $21,210) was performed. The cost of revision surgery had no effect on the cost-effectiveness outcome.
The utilities or health states for patients with rotator cuff pathology were determined from the literature. Utility states decline with increasing age. The average age for rotator cuff surgery in this model was fifty-six years. A health utility of 0.803 and 0.851 was assigned for patients preoperatively and postoperatively, respectively1. In addition, patients who had a symptomatic retear after single or double-row repair were assigned a health utility that was equivalent to their preoperative state. The utility for this symptomatic state ranged from 0 (death) to 1 (perfect health), and, if the value decreased to <0.53, then double-row repair represented a cost-effective operative alternative.
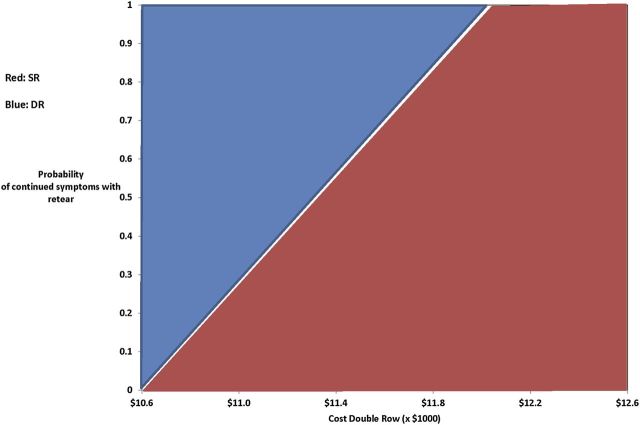
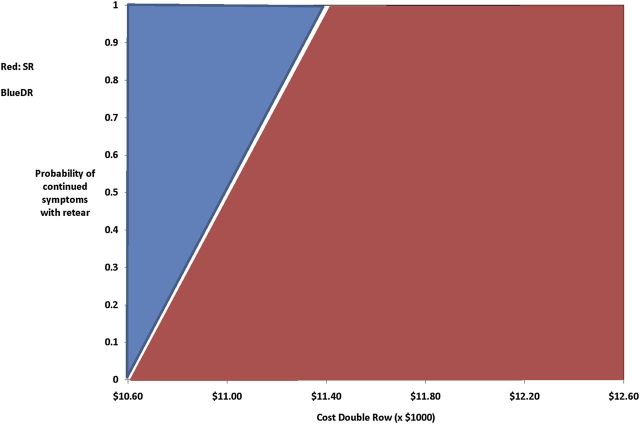
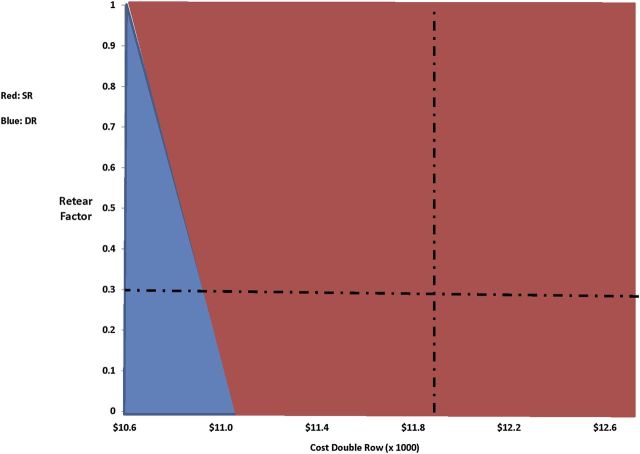
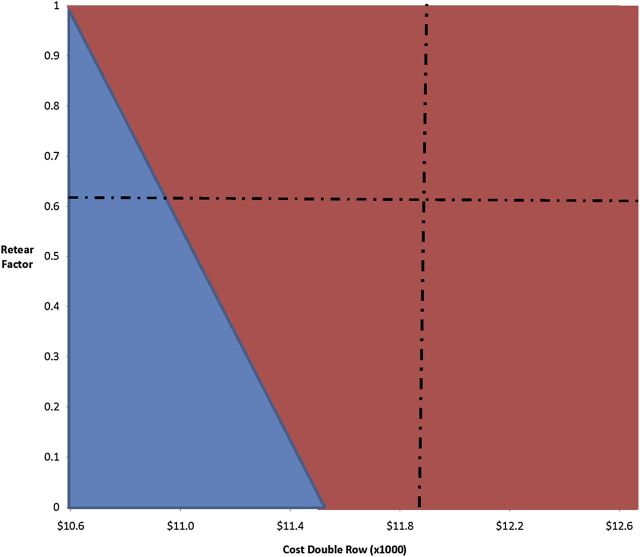
Two-way sensitivity analysis was used to vary multiple model assumptions simultaneously and determine their impact on cost-effectiveness. The cost associated with double-row repair was evaluated against the proportion of retear on imaging studies and the proportion of reduction in retear from double-row repair, i.e., the retear factor (Figs. 3-A, 3-B, 4-A, and 4-B). As double-row repair becomes more effective at reducing retear proportions, a greater amount of incremental costs can be allotted to double-row repair, while still remaining cost-effective.
A two-way sensitivity analysis evaluating the cost of double-row repair (a baseline of $11,914) and the probability of symptoms following double-row repair (a baseline of 0.20) for tears of <3 cm (Fig. 3-A) and tears of ≥3 cm (Fig. 3-B). The red shaded area indicates where a single-row repair (SR) would be the favored strategy, while the blue shaded region indicates that double-row repair (DR) becomes cost-effective. As the percentage of patients with symptoms from a retear increases, more could be spent on the second row.
Fig. 3-A.
Fig. 3-B.
A two-way sensitivity analysis evaluating the retear factor (the proportion reduction of recurrent tear following double-row repair compared with single-row repair) versus the cost of double-row repair for initial tears of <3 cm (Fig. 4-A) and initial tears of ≥3 cm (Fig. 4-B). As the relative rate of retear goes down in double-row repair (DR) compared with single-row repair (SR), a greater amount of money could be spent on the additional row of anchors. Baseline rates are shown in dashed lines.
Fig. 4-A.
Fig. 4-B.
Discussion
Arthroscopic rotator cuff repair remains one of the most common orthopaedic surgical procedures and, independent of repair type, has been shown to be a cost-effective treatment for symptomatic rotator cuff tears1. Despite the frequency of rotator cuff repair, there remains no consensus on the best repair technique. Much of the focus on rotator cuff surgery has been on a reduction in failure rates. The rate of healing has been reported to range from 10% to 91%, depending on the method of evaluation, the size of tear, and the mode of repair13. A recent review by Dines et al. grouped rotator cuff repairs that had failed to heal into four categories: technical, biologic, anatomic, and mechanical failures26. Apreleva et al. were the first, as far as we know, to propose that recreation of the normal rotator cuff footprint may reduce the rate of anatomic failures27.The double-row technique of rotator cuff repair was designed to more anatomically reestablish this footprint. Further, in vitro biomechanical modeling has demonstrated superior mechanical strength associated with double-row repair compared with single-row repair. Yet, to date, no large series, as far as we know, has demonstrated a functional improvement following double-row repair versus single-row repair. The addition of a second row of anchors adds both implant costs and increased operative time. The aim of this study was to determine whether arthroscopic double-row rotator-cuff repair represents a cost-effective alternative to traditional single-row arthroscopic fixation techniques. We found that, for the baseline case of a patient presenting for first-time rotator cuff surgery, double-row rotator cuff repair is not cost-effective. However, if the additional costs associated with double-row repair could be reduced to <$287 for small tears (<3 cm) and <$352 for larger tears (≥3 cm), the double-row repair would then be a cost-effective mode of operative fixation.
Clinically, it was assumed a double-row repair would, on average, require two additional anchors and fifteen minutes of operating-room time. To stay below this additional cost threshold for tears of <3 cm, a surgeon would not be able to incur the costs of even a single second-row anchor and would require incremental operating-room time to be less than ten minutes. For larger tears (≥3 cm), the surgeon would be limited to a single lateral row implant and less than three additional minutes of operative time to stay within the cost-effective threshold for a double-row repair. Given current implant costs, the addition of a second row of anchors is not an economically sound option. Therefore, implant costs represent an important target to create a more cost-effective environment. In addition, these results provide impetus for further investigation and development of “anchorless” fixation techniques.
The two-way sensitivity analysis illustrates multiple cases in which the clinical outcomes would impact the ability to afford a double-row repair. For example, in a massive tear, if the expected proportion of recurrent tear is 80% following single-row repair, then an additional $600 (or one anchor and fifteen minutes of operating-room time) could still be cost-effective (Fig. 3-B). Another example is if the surgeon determines that he or she could reduce the retear proportion to 10% of that of single-row repair by using the second row, then an additional $800 (two anchors and ten minutes of operating-room time) could be spent and remain cost-effective (Fig. 3-B).
As with any cost-effective analysis, there are limitations within this study. Model assumptions are based on the results in the literature. As such, the model is only as strong as the composite of its assumptions. The meta-analysis by Duquin et al13. from 2010 was utilized as the primary proportions of retear for both single-row and double-row repair. In the systematic review, only two level-I studies compared the two techniques, and twenty-one of the twenty-three articles evaluated had a level of evidence of III or higher. However, the sensitivity analysis reveals that the model is robust (assessing the variables throughout their range in the literature did not change the incremental cost-effectiveness). Except for the incremental costs associated with double-row repair and the health utility associated with repair failure, the other variables (probabilities and costs) were ranged throughout all plausible values with no change in the favored strategy.
In addition, the results of surgery were only evaluated over a two-year window as this is the limit of follow-up in the meta-analyses13. However, in a recent study, Kluger et al. followed patients for up to eleven years after repair28. The majority of retears occurred early (as in the study by Huijsmans et al21.), and good results in patients at six months predicted good long-term outcomes at the time of final follow-up. It is possible that longer-term follow-up will reveal that the difference in retear rates between the two techniques will translate into long-term functional difference or decreased utility states in the single-row group. If future literature indicates a difference in patient outcomes, the baseline model would need to be adjusted to illustrate changes over a longer time window.
This cost-effectiveness analysis used decision-analytic modeling to reflect average outcomes for two groups of patients with rotator cuff tears. Therefore, our analysis provides a population-based analysis using averages for rates, costs, and utilities. This study is not intended to take the place of individual characteristics or surgeon or patient preferences. Instead, this model provides a tool illustrating critical variables that may affect decision making. As such, it serves as a springboard for guiding important variables to analyze in future clinical research. In addition, there are subsets of patients who may be at higher risk for retear following surgery when the double-row repair may become a cost-effective option. For example, Björnsson et al. recently showed that older patients have a higher retear proportion than their younger counterparts29. However, since they did not stratify results on the basis of repair type (single-row compared with double-row repairs), this was not included in the analysis but may be a direction of future investigations.
With use of current data for the average patient presenting with a rotator cuff tear, irrespective of tear size, double-row repair is not a cost-effective method of rotator cuff repair. The incremental cost associated with a second row of implants and associated operating-room time is not offset by the reduction in retear proportions, the potential improved clinical rate, or the potential decreased need for revision surgery. There are, however, specific clinical scenarios of primary injuries with higher retear proportions or persistent symptoms that would justify some additional costs. The challenge of future research is to identify characteristics of rotator cuff tears that would best be suited for this added expense.
Investigation performed at the Steadman Hawkins Clinic-Denver, Lone Tree, Colorado, and Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. One or more of the authors, or his or her institution(s), has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, one or more of the authors has had another relationship, or has engaged in another activity, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1. Vitale MA Vitale MG Zivin JG Braman JP Bigliani LU Flatow EL. Rotator cuff repair: an analysis of utility scores and cost-effectiveness. J Shoulder Elbow Surg. 2007;16:181-7. [DOI] [PubMed] [Google Scholar]
- 2. Bennett WF. Arthroscopic repair of massive rotator cuff tears: a prospective cohort with 2- to 4-year follow-up. Arthroscopy. 2003;19:380-90. [DOI] [PubMed] [Google Scholar]
- 3. Gartsman GM Khan M Hammerman SM. Arthroscopic repair of full-thickness tears of the rotator cuff. J Bone Joint Surg Am. 1998;80:832-40. [DOI] [PubMed] [Google Scholar]
- 4. Murray TF Jr Lajtai G Mileski RM Snyder SJ. Arthroscopic repair of medium to large full-thickness rotator cuff tears: outcome at 2- to 6-year follow-up. J Shoulder Elbow Surg. 2002;11:19-24. [DOI] [PubMed] [Google Scholar]
- 5. Wilson F Hinov V Adams G. Arthroscopic repair of full-thickness tears of the rotator cuff: 2- to 14-year follow-up. Arthroscopy. 2002;18:136-44. [DOI] [PubMed] [Google Scholar]
- 6. Sugaya H Maeda K Matsuki K Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am. 2007;89:953-60. [DOI] [PubMed] [Google Scholar]
- 7. Lo IK Burkhart SS. Double-row arthroscopic rotator cuff repair: re-establishing the footprint of the rotator cuff. Arthroscopy. 2003;19:1035-42. [DOI] [PubMed] [Google Scholar]
- 8. Waltrip RL Zheng N Dugas JR Andrews JR. Rotator cuff repair. A biomechanical comparison of three techniques. Am J Sports Med. 2003;31:493-7. [DOI] [PubMed] [Google Scholar]
- 9. Bell J Ahmad CS. Current concepts in arthroscopic rotator cuff repair: single vs double row repair. Curr Opin Orthop. 2007;18:363-8. [Google Scholar]
- 10. Park JY Lhee SH Choi JH Park HK Yu JW Seo JB. Comparison of the clinical outcomes of single- and double-row repairs in rotator cuff tears. Am J Sports Med. 2008;36:1310-6. [DOI] [PubMed] [Google Scholar]
- 11. Sherman SL Lyman S Koulouvaris P Willis A Marx RG. Risk factors for readmission and revision surgery following rotator cuff repair. Clin Orthop Relat Res. 2008;466:608-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Elixhauser A Halpern M Schmier J Luce BR. Health care CBA and CEA from 1991 to 1996: an updated bibliography. Med Care. 1998;36(5 Suppl):MS1-9, MS18-147. [DOI] [PubMed] [Google Scholar]
- 13. Duquin TR Buyea C Bisson LJ. Which method of rotator cuff repair leads to the highest rate of structural healing? A systematic review. Am J Sports Med. 2010;38:835-41. [DOI] [PubMed] [Google Scholar]
- 14. Organization for Economic Co-operation and Development. OECD health data. OECD health statistics. 2010. doi:10.178/data-00350-en. Accessed 2011 Dec 16. [Google Scholar]
- 15. Hirskyj P. QALY: an ethical issue that dare not speak its name. Nurs Ethics. 2007;14:72-82. [DOI] [PubMed] [Google Scholar]
- 16. Hunink M Glasziou P Siegel JE Weeks JC Pliskin JS Elstein AS Weinstein MC. Decision making in health and medicine: integrating evidence and values. New York: Cambridge University Press; 2001. [Google Scholar]
- 17. Finkler SA. The distinction between cost and charges. Ann Intern Med. 1982;96:102-9. [DOI] [PubMed] [Google Scholar]
- 18. Moosmayer S Lund G Seljom U Svege I Hennig T Tariq R Smith HJ. Comparison between surgery and physiotherapy in the treatment of small and medium-sized tears of the rotator cuff: a randomised controlled study of 103 patients with one-year follow-up. J Bone Joint Surg Br. 2010;92:83-91. [DOI] [PubMed] [Google Scholar]
- 19. Brooks R. EuroQol: The current state of play. Health Policy. 1996;37:53-72. [DOI] [PubMed] [Google Scholar]
- 20. McHorney CA Ware JE Jr Raczek AE. The MOS 36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247-63. [DOI] [PubMed] [Google Scholar]
- 21. Huijsmans PE Pritchard MP Berghs BM van Rooyen KS Wallace AL de Beer JF. Arthroscopic rotator cuff repair with double-row fixation. J Bone Joint Surg Am. 2007;89:1248-57. [DOI] [PubMed] [Google Scholar]
- 22. Fryback DG Dunham NC Palta M Hanmer J Buechner J Cherepanov D Herrington SA Hays RD Kaplan RM Ganiats TG Feeny D Kind P. US norms for six generic health-related quality-of-life indexes from the National Health Measurement study. Med Care. 2007;45:1162-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Klepps S Bishop J Lin J Cahlon O Strauss A Hayes P Flatow EL. Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med. 2004;32:1716-22. [DOI] [PubMed] [Google Scholar]
- 24. Keener JD Wei AS Kim HM Paxton ES Teefey SA Galatz LM Yamaguchi K. Revision arthroscopic rotator cuff repair: repair integrity and clinical outcome. J Bone Joint Surg Am. 2010;92:590-8. [DOI] [PubMed] [Google Scholar]
- 25. Laupacis A Feeny D Detsky AS Tugwell PX. How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ. 1992;146:473-81. [PMC free article] [PubMed] [Google Scholar]
- 26. Dines JS Bedi A ElAttrache NS Dines DM. Single-row versus double-row rotator cuff repair: techniques and outcomes. J Am Acad Orthop Surg. 2010;18:83-93. [DOI] [PubMed] [Google Scholar]
- 27. Apreleva M Ozbaydar M Fitzgibbons PG Warner JJ. Rotator cuff tears: the effect of the reconstruction method on three-dimensional repair site area. Arthroscopy. 2002;18:519-26. [DOI] [PubMed] [Google Scholar]
- 28. Kluger R Bock P Mittlböck M Krampla W Engel A. Long-term survivorship of rotator cuff repairs using ultrasound and magnetic resonance imaging analysis. Am J Sports Med. 2011 May 24 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 29. Björnsson HC Norlin R Johansson K Adolfsson LE. The influence of age, delay of repair, and tendon involvement in acute rotator cuff tears: structural and clinical outcomes after repair of 42 shoulders. Acta Orthop. 2011;82:187-92. [DOI] [PMC free article] [PubMed] [Google Scholar]