Supplemental Digital Content is Available in the Text.
Key Words: rib fractures, surgical stabilization of rib fractures, flail chest, pulmonary contusion, stabilization index, rib plating
Abstract
Objectives:
To compare outcomes in patients with rib fractures (RFX) who underwent surgical stabilization of rib fractures (SSRF) to those treated nonoperatively.
Design:
Retrospective cohort study.
Setting:
Two Level 1 Trauma Centers.
Patients:
One hundred seventy-four patients with multiple RFX divided into 2 groups: patients with surgically stabilized RFX (n = 87) were compared with nonoperatively managed patients in the matched control group (MCG) (n = 87).
Intervention:
SSRF.
Outcome Measurements:
Age, sex, injury severity score, RFX, mortality, hospital length of stay (HLOS) and intensive care unit length of stay (ICULOS), duration of mechanical ventilation (DMV), co-injuries, and time to surgery. Patients were further stratified by presence or absence of flail chest and pulmonary contusion (PC).
Results:
Flail chest, displaced RFX, and PC were present significantly more often in SSRF patients compared with the MCG. Mortality was lower in SSRF group. HLOS and ICULOS were longer in SSRF group compared with the corresponding MCG patients regardless of timing to surgery (P < 0.01 for all). SSRF patients with flail chest had comparable HLOS, ICULOS, and DMV to MCG patients with flail chest (P > 0.3 for all). SSRF patients without flail chest had significantly longer HLOS and ICULOS than MCG patients without flail chest (P < 0.001 for both). Presence of PC did not affect lengths of stay.
Conclusions:
SSRF patients had reduced mortality compared with nonoperatively managed patients. HLOS, ICULOS, and DMV were longer in SSRF patients than in MCG. When flail chest was present, lengths of stay were comparable. PC did not seem to affect the surgical outcome.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
INTRODUCTION
Operative management of rib fractures (RFX) has remained underutilized with some studies showing that only 0.7% of patients with flail chest undergo surgical treatment.1 An analysis of the National Trauma Data Bank for patients with RFX revealed that nationwide, only 4.36% underwent surgical stabilization of rib fractures (SSRF).2 Most patients who underwent SSRF (96.6%) did not have flail chest, whereas only 14.5% of patients with flail chest underwent SSRF.2 This is an interesting statistic because flail chest is often considered a primary indication for SSRF. Recently, however, the use of SSRF has expanded as an alternative to nonoperative treatment. Dehghan et al3 reported a substantial increase in the rate of surgical fixation of flail chest from 1% to 10% during an 11-year period. There are still many unresolved questions regarding the indications and contraindications for SSRF, and particularly, disagreement remains concerning SSRF in patients with pulmonary contusion (PC) or without flail chest.4,5
The aim of this study was to investigate whether surgery was beneficial compared with a nonoperative treatment. Our primary goal was to analyze selected variables of patients with SSRF and a nonsurgical matched control group (MCG). Our secondary goal was to delineate conditions when SSRF was beneficial, especially in the subgroups of RFX patients with PC and without flail chest.
PATIENTS AND METHODS
This IRB-approved retrospective cohort–matched control study included patients with radiologically confirmed (computed tomography scans and x-rays) RFX evaluated at 2 state certified Level 1 Trauma Centers over a 6-year period (2011–2017). The SSRF group contained 87 patients who were compared with 87 patients with RFX in the MCG. SSRF patients from the 2 hospitals were matched to nonoperatively managed patients with rib fractures (MCG) from that same hospital using the propensity score method. Propensity matching introduces randomization into the retrospective study and therefore reduces bias in the selection process.6 Based on their importance in outcomes and treatment options selection, the covariates used as independent variables were age and number of ribs fractured. This yielded 2 groups of 87 patients for the analysis that also had identical injury severity score (ISS). The MCG was further divided into several subgroups for comparison with the matching patients from SSRF subgroups into flail chest, PC, and preoperative interval categories. In all groups, patients with mortality within the first 24 hours were excluded.
Clinical data were obtained from the trauma registries of both hospitals and the Palm Beach County Health Care District Trauma Agency's registry. As necessary, data were supplemented with information obtained from the patients' electronic medical records. International Classification of Diseases, Ninth and Tenth Revisions, were used to identify abstracted variables. Analyzed variables included age, sex, ISS, mortality, number of RFX, number of total fractures of the ribs, number of displaced fractures, segmental location of RFX, incidences of flail chest, bilateral fractures, first RFX, PC, and multiple co-injuries. Flail chest was defined as fractures of 3 or more consecutive ribs in 2 or more places. Data regarding hospital length of stay (HLOS), intensive care unit length of stay (ICULOS), duration of mechanical ventilation (DMV), timing to surgery, and insurance status were collected as well. To quantify the proportion of surgically stabilized ribs, we calculated the Stabilization Index (SI). SI was computed as a ratio between plated and fractured ribs per patient, and it ranged from 0% to 100%. SI helps to compare data from different patient cohorts, to describe the level of stabilization achieved.7–9
Statistical analysis was performed using IBM SPSS version 24.0 (IBM, Armonk, NY). The analysis included group characteristics and bivariate correlation comparisons. Categorical variables were analyzed with χ2 test. In all groups, 2-sided independent sample t-tests for normally distributed variables were used to compare differences between variable means. Statistical significance was assumed when the calculated P value was below 0.05.
RESULTS
Comparison of demographic and clinical characteristics of patients between SSRF and MCG groups is presented in Table 1. Comparison of co-injuries between those groups is presented in Supplemental Digital Content 1 (see Table, http://links.lww.com/JOT/A510). Distribution of fractured ribs versus surgically stabilized ribs is presented in Figure 1.
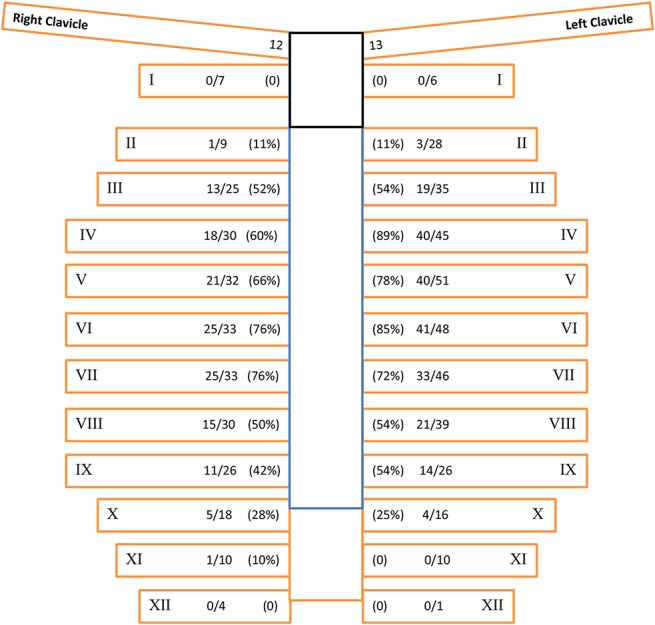
TABLE 1.
Characteristics of Patients in SSRF Group Versus MCG
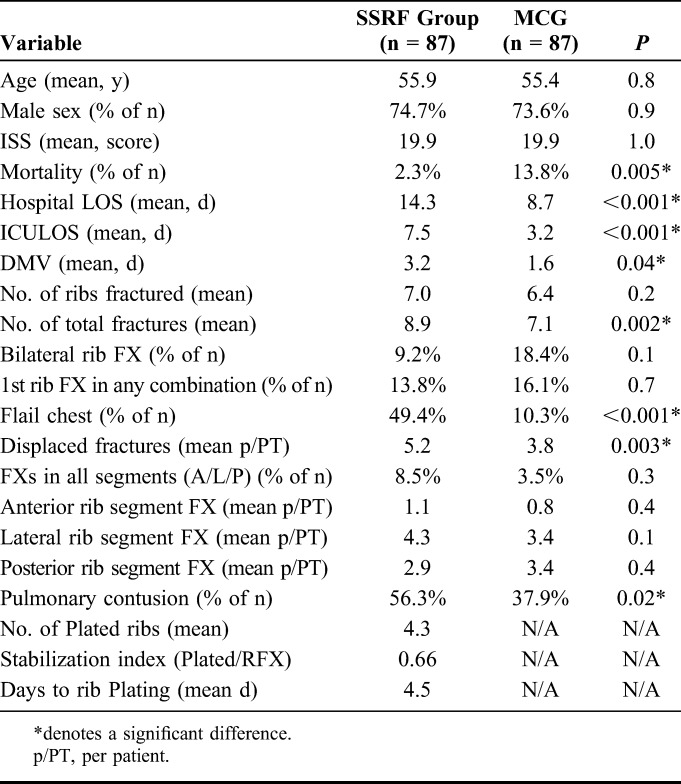
FIGURE 1.
Distribution of surgically stabilized versus fractured ribs in the SSRF group. Legend for Figure 1. Rib number; # of ribs plated/# of ribs fractured; % of surgical stabilization per rib. Editor's Note: A color image accompanies the online version of this article.
Characteristics and co-injuries of SSRF patients plated within 3 days versus plated after 3 days are presented in Figure 2, Supplemental Digital Content 2 (see Table, http://links.lww.com/JOT/A511) and Supplemental Digital Content 3 (see Table, http://links.lww.com/JOT/A512).
FIGURE 2.
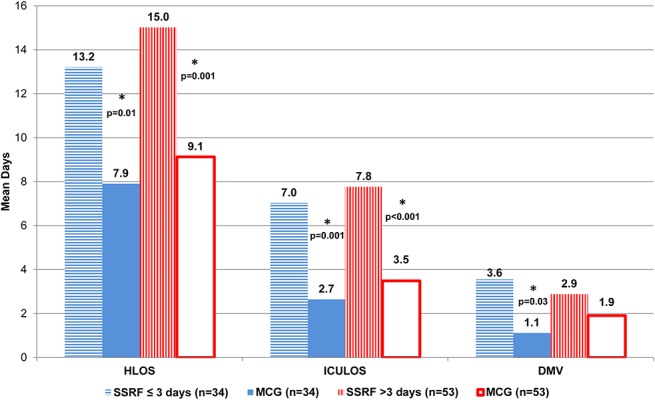
Mean lengths of stay and DMV for patients with SSRF within and after 3 days of admission versus corresponding MCG patients.
The differences between lengths of stay, DMV, and characteristics of patients with and without flail chest, as well as with and without PC are presented in Figures 3 and 4 and Supplemental Digital Content 4–5 (see Tables, http://links.lww.com/JOT/A513, http://links.lww.com/JOT/A514).
FIGURE 3.
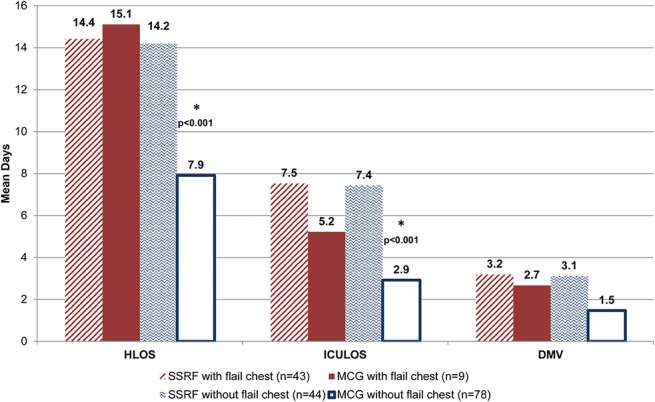
Mean lengths of stay and DMV for SSRF group with flail chest versus MCG with flail chest, and SSRF group without flail chest versus MCG without flail chest.
FIGURE 4.
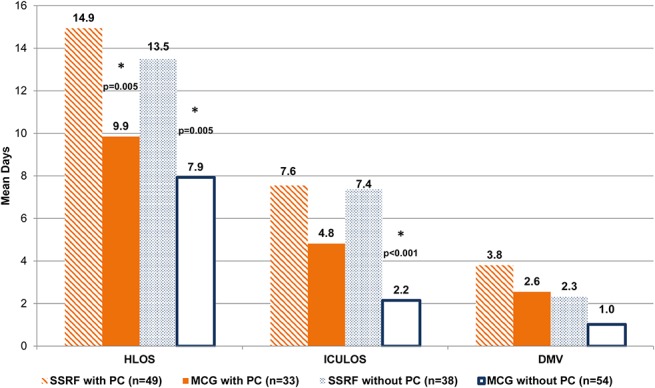
Mean lengths of stay and DMV for SSRF group with PC versus MCG with PC and SSRF group without PC versus MCG without PC.
Insurance status was comparable between the surgical and nonsurgical groups with 94.3% of patients insured in the SSRF group and 87.4% covered in the MCG (P = 0.1). Calculated mean SI value in our patients was 66%, meaning that only two-thirds of fractured ribs in the SSRF group were surgically stabilized.
There were a total of 21 surgeons that were involved in the treatment of patients with RFX, either as consultants (15 physicians) or operators (6 physicians). Of the 6 active operators, 2 were working at both institutions, therefore contributing to the uniformity of treatment decisions. Operators were recommending SSRF in 65% of their patients, whereas consultants were advising surgery in 45% of their cases.
DISCUSSION
Patients in both SSRF and MCG groups were predominantly male, had similar age, mean number of fractured ribs, segmental distribution of RFX, and frequency of bilateral RFX. However, the mean number of total fractures of the ribs was significantly higher in SSRF patients. Despite the fact that the 2 groups had identical ISS, mortality was statistically significantly lower in the SSRF group than in the MCG (Table 1). First rib fracture was encountered similarly often in both groups. This confirms the notion that upper ribs do not contribute considerably to the chest wall stability, while requiring technically challenging access and therefore are not routinely operated upon.4
Predictably, displacement of the fragments played an important role in the decision for SSRF. Displaced RFX were present significantly more often in the SSRF group. The calculated SI among our SSRF patients of 66% is in agreement with previously reported values of 0.6 in patients treated with plating and 0.71 in those cases treated with intramedullary fixation.7–9 These SI reflect the reality that not all of fractured ribs need to be plated to achieve a stable thoracic wall. In a prospective, controlled clinical evaluation of SSRF in patients with severe RFX, Pieracci et al9 described as 5.0, the median number of ribs stabilized. Taylor et al10 reported 5.0 ribs instrumented, with a mean of 5.8 plates placed per patient, whereas among our patients, there was a mean of 4.3 ribs plated. Marasco et al7 described the median number of ribs stabilized by intramedullary fixation per patient being 5.
Analysis of the distribution of RFX revealed that ribs on the left side were fractured more frequently (Fig. 1). Also, the left side was stabilized surgically more often than the right side (61.3% vs. 52.5%). On both sides, ribs 4 to 7 were broken and plated most often.
One of our major findings was that HLOS, ICULOS, and DMV were statistically significantly longer in SSRF patients compared with the MCG.
Comparison of co-injuries between groups revealed a very similar array of co-injuries in the SSRF and the MCG with pulmonary co-injuries being the most common, followed by orthopedic co-injuries. Pulmonary co-injuries were statistically significantly more frequent in SSRF patients (see Supplemental Digital Content 1, Table, http://links.lww.com/JOT/A510).
The main indications, although relative, for SSRF have been described as (1) flail chest, (2) failure to control pain, (3) respiratory failure due to chest wall injury/pain, (4) chest wall deformity and noticeable loss of thoracic volume.11–13 Considerations for SSRF are usually stronger with multiple RFX and particularly with presence of displaced RFX. Traditional contraindications, in addition to traumatic brain injury, include PC (so called parenchymal pathology).11,14
Timing of Surgery
Among our patients, SSRF was performed between 1 and 23 days of admission with the mean time to surgery being 4.5 days (Table 1). There were only 3 cases when SSRF was performed within the first 24 hours of admission. The effect of preoperative interval (time from the admission to the time of surgery) on HLOS, ICULOS, and DMV was evaluated by comparison of 2 surgical subgroups: SSRF performed within first 3 days of admission (mean 1.4 days) and SSRF after 3 days (mean 6.4 days and 4–23 days range). Patients in these SSRF subgroups were also compared with their counterparts in the MCG (Fig. 2).
HLOS and ICULOS were longer in plated patients, regardless of the timing of surgery, compared with the MCG (Fig. 2). Patients who were treated surgically earlier (within 3 days) were different from the delayed surgical patients by higher number of fractured ribs and more frequent displaced fractures (see Table, Supplemental Digital Content 2 http://links.lww.com/JOT/A511). Also, in the delayed surgical patients, there was a statistically significantly higher incidence of traumatic brain injury, which could be a possible explanation for the postponement of surgery (see Table, Supplemental Digital Content 3, http://links.lww.com/JOT/A512).
Stratification by 3 days for timing of SSRF was based on the recently published practice guidelines that advocate for a 72-hour window due to a technically easier surgery before the beginning of inflammation and callus formation and, therefore, less difficult fracture reduction.15 In institutions with advanced experience with SSRF, the mean time from the admission to surgery has been reported to be 2.4 days.9 It also seems that over time, proponents of SSRF are moving toward faster initiation of the surgical procedure.16
Stratification by Presence of Flail Chest
In our study, the incidence of flail chest was 5 times higher in SSRF patients, and it was statistically significant (Table 1). We also found that SSRF patients with flail chest had comparable HLOS, ICULOS, and DMV with the MCG patients with flail chest (Fig. 3). SSRF patients without flail chest had statistically significantly longer HLOS and ICULOS compared with the MCG patients without flail chest (Fig. 3). In recent study, Farguhar et al17 observed longer hospital and ICU stays in patients with flail chest after surgical fixation. DeFreest et al18 also reported longer hospitalization in polytrauma patients with flail chest treated with SSRF compared to those treated with nonoperative management.
In surgically treated patients, there were almost identical lengths of stay and DMV regardless of the presence of flail chest (see Table, Supplemental Digital Content 4, http://links.lww.com/JOT/A513). Although SSRF patients with flail chest had significantly higher ISS and number of ribs fractured than those plated without flail chest, it did not adversely affect HLOS, ICULOS, and DMV (see Table, Supplemental Digital Content 4, http://links.lww.com/JOT/A513). These findings would support SSRF in more severely injured patients with flail chest. In the recent study published by Dehghan et al,3 it was found that surgical stabilization of flail chest reduces the mortality to that of stable chest wall injuries. In our SSRF patients, mortality was not statistically significantly different between those with flail chest and those without (see Table, Supplemental Digital Content 4, http://links.lww.com/JOT/A513). Occurrence of flail chest did not prompt earlier surgical intervention, which can be attributed to the presence of multiple RFX (>6) in both groups.
Stratification by Presence of Pulmonary Contusion
The incidence of PC in our SSRF group was statistically significantly higher than in the MCG (Table 1). Our data compare with a recent report by Farguhar et al17 that PC is present in most patients treated with a surgical approach.
There was longer HLOS in the SSRF patients with PC, compared to the MCG patients with PC, and this was statistically significant (Fig. 4). There was also longer HLOS and ICULOS in the SSRF patients without PC in comparison with the MCG patients without PC, and this was also statistically significant. In both subgroups (with and without PC), DMV was comparable in surgically and nonoperatively managed patients (P > 0.4 for both).
SSRF patients with PC and without PC had comparable number of RFX, mortality, lengths of stay, and days to surgical intervention, whereas ISS was higher in the first subgroup (Fig. 4, see Table, Supplemental Digital Content 5, http://links.lww.com/JOT/A514).
It seems that PC was not a factor affecting outcomes of surgical procedures and therefore recommendations to resolve PC before SSRF are not supported by our findings. This observation is contradictory to the previously suggested notion of PC as a contraindication for SSFR.11,14 Furthermore, Taylor et al10 have also found that the presence of PC did not eliminate improvements after surgical stabilization of flail chest.
Other advantages described with SSRF included a decreased incidence of retained hemothorax and empyema.16 In addition, it was reported that 2 years after discharge patients who were not treated with operative rib fixation demonstrated significant reduction in quality of life with particularly poor return to work.19
The insurance status was similar in the 2 groups, therefore allowing us to assume that insurance was unlikely to be a factor in the decision for treatment option.
Our study has several limitations to be noted. This is a retrospective chart review and therefore is inherent to all known shortcomings of analysis of the prerecorded data.20 Patient selection was limited to 2 Level 1 trauma centers. Prevalence of flail chest was higher in the SSRF group; however, this observation is also in support of this condition as an indication for surgical stabilization. The long-term follow-up was not included. The whole continuum of care of patients with RFX, which includes longstanding results, may reveal additional benefits of SSRF such as relief from chronic pain, prevention of deformity formation, return to work, etc. and, therefore, warrants further investigations. The comparison of surgical groups to MCGs of nonoperatively managed patients adds to the validity of the findings.
CONCLUSIONS
Mortality was lower in surgically treated patients; however, patients with SSRF had longer HLOS, ICULOS, and DMV compared with the MCG patients. Displaced RFX and flail chest were observed more often in patients with SSRF in comparison with corresponding patients in the MCG. Presence of PC did not seem to affect the outcomes of surgical treatment. Additional benefits of rib plating, including pain reduction and return to work, may be more pronounced in a long-term follow-up.
Supplementary Material
Footnotes
The authors report no conflict of interest.
Presented in part at the 13th Annual Academic Surgical Congress on January 30–February 1, 2018, Jacksonville, FL.
This retrospective cohort study was approved by MetroWest Medical Center IRB.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jorthotrauma.com).
REFERENCES
- 1.Dehghan N, deMestral C, McKee MD, et al. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76:462–468. [DOI] [PubMed] [Google Scholar]
- 2.Kane E, Jeremitsky E, Pieracci FM, et al. Quantifying and exploring the recent national increase in surgical stabilization of rib fractures. J Trauma Acute Care Surg. 2017;83:1047–1052. [DOI] [PubMed] [Google Scholar]
- 3.Dehghan N, Mah JM, Schemitsch EH, et al. Operative stabilization of flail chest injuries reduces mortality of that of stable chest wall injuries. J Orthop Trauma. 2018;32:15–21. [DOI] [PubMed] [Google Scholar]
- 4.Kasotakis G, Hasenboehler EA, Streib EW, et al. Operative fixation of rib fractures after blunt trauma: a practice management guideline from Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2017;82:618–626. [DOI] [PubMed] [Google Scholar]
- 5.Vana PG, Neubauer DC, Luchette FA. Contemporary management of flail chest. Am Surg. 2014;80:527–535. [DOI] [PubMed] [Google Scholar]
- 6.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marasco S, Quayle M, Summerhayes R, et al. An assessment of outcomes with intermedullary fixation of fractured ribs. J Cardiothorac Surg. 2016;11:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marasco S, Saxena P. Surgical rib fixation: technical aspects. Injury. 2015;46:929–932. [DOI] [PubMed] [Google Scholar]
- 9.Pieracci FM, Lin Y, Rodil M, et al. A prospective controlled clinical evaluation of surgical stabilization of severe rib fractures. J Trauma Acute Care Surg. 2016;80:187–194. [DOI] [PubMed] [Google Scholar]
- 10.Taylor BC, Fowler TT, French BG, et al. Clinical outcomes of surgical stabilization of flail chest injury. J Am Acad Orthop Surg. 2016;24:575–580. [DOI] [PubMed] [Google Scholar]
- 11.Sarani B, Schulte L, Diaz JJ. Pitfalls associated with open reduction and internal fixation of fractured ribs. Injury. 2015;46:2335–2340. [DOI] [PubMed] [Google Scholar]
- 12.Lafferty PM, Anavian J, Will RE, et al. Operative treatment of chest wall injuries: indications, technique, and outcomes. J Bone Joint Surg Am. 2011;93:97–110. [DOI] [PubMed] [Google Scholar]
- 13.Fowler TT, Taylor BC, Bellino MJ, et al. Surgical treatment of flail chest and rib fractures. J Am Acad Orthop Surg. 2014;22:751–760. [DOI] [PubMed] [Google Scholar]
- 14.Voggenreiter G, Nuedeck F, Aufmkolk M, et al. Operative chest wall stabilization in flail chest: outcomes of patients with or without pulmonary contusion. J Am Coll Surg. 1998;187:130–138. [DOI] [PubMed] [Google Scholar]
- 15.Pieracci FM, Majercik S, Ali-Osman F, et al. Consensus statement: surgical stabilization of rib fractures rib fracture colloquium clinical practice guidelines. Injury. 2017;48:307–321. [DOI] [PubMed] [Google Scholar]
- 16.Majercik S, Vijayakumar S, Olsen G, et al. Surgical stabilization of severe rib fractures decreases incidence of retained hemothorax and empyema. Am J Surg. 2015;210:1112–1117. [DOI] [PubMed] [Google Scholar]
- 17.Farguhar J, Almarhabi Y, Slobogean G, et al. No benefit to surgical fixation of flail chest injuries compared with modern comprehensive management: results of a retrospective cohort study. Can J Surg. 2016;59:299–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DeFreest L, Tafen M, Bhakta A, et al. Open reduction and internal fixation of rib fractures in polytrauma patients with flail chest. Am J Surg. 2016;211:761–767. [DOI] [PubMed] [Google Scholar]
- 19.Marasco S, Lee G, Summerhayes R, et al. Quality of life after major trauma with multiple rib fractures. Injury. 2015;46:61–65. [DOI] [PubMed] [Google Scholar]
- 20.Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: reducing bias in emergency medicine chart review studies. Ann Emerg Med. 2014;64:292–298. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


