Abstract
Background: Detailed descriptions of meniscus and articular cartilage lesions associated with anterior cruciate ligament injury have not been presented in the literature. Our goal was to determine the associations between patient sex, age, and surgical delay and the frequency and location of meniscus and articular cartilage lesions seen at the time of the anterior cruciate ligament reconstruction.
Methods: Data were obtained retrospectively from a database of 1209 consecutive patients undergoing anterior cruciate ligament reconstruction between 1988 and 2002. All knee cartilage, meniscus, and ligament injuries were documented on anatomic maps at the time of surgery, and the data were analyzed.
Results: Meniscus injuries were identified in 722 (65%) of the 1104 patients who met the criteria for inclusion in the study. Female patients were less likely to have a meniscus injury than male patients were (56% compared with 71%), and male patients were more likely to have combined medial and lateral meniscus injuries than female patients were (20% compared with 11%). Patients with a surgical delay of less than three months were less likely to have a medial meniscus injury (8% compared with 19%). Femoral articular cartilage injuries were identified in 472 patients (43%). Patients who were twenty-five years of age or older were more likely to have multiple cartilage lesions throughout the knee (7.7% compared with 1.3%) and to have more isolated medial femoral condyle lesions (24.2% compared with 13.3%). Patients with a surgical delay of more than one year were more likely to have a lesion (60% compared with 47% for all others), and a surgical delay of more than one year resulted in a greater proportion of large and grade-3 lesions of the lateral femoral condyle. Female patients had a greater proportion of grade-1 lesions of the medial femoral condyle (29% compared with 16%), whereas male patients had a greater proportion of grade-3 and 4 lesions of the medial femoral condyle (49% compared with 35%). In patients who were thirty-five years of age or older, meniscus injuries were more frequent and were located more frequently on the medial side; femoral articular cartilage lesions were also located more frequently on the medial side.
Conclusions: Increased age, male sex, and increased surgical delay all increase the frequency and severity of injuries of the meniscus and/or articular cartilage after an anterior cruciate ligament tear.
Level of Evidence: Prognostic Level II. See Instructions to Authors for a complete description of levels of evidence.
Although several studies have evaluated patterns of meniscus and articular cartilage injury in knees with an anterior cruciate ligament injury1-6, detailed descriptions of meniscus and articular cartilage injury have not been presented for the general population of individuals who commonly sustain anterior cruciate ligament injury. The length of time from anterior cruciate ligament injury to anterior cruciate ligament reconstruction has been associated with the development of intra-articular cartilage damage1,3,4,6, and delay has been shown to increase the number of intra-articular injuries (i.e., articular cartilage defects and meniscus tears)4,6. Following anterior cruciate ligament tears, male patients have also been shown to have more meniscus injuries than female patients and meniscus injuries have been demonstrated to be accompanied by increasing articular cartilage damage4,5. Furthermore, the age of the patient at the time of anterior cruciate ligament injury and the level of sport participation have not been shown to increase the risk of meniscus or cartilage lesions4,6. However, most of those studies had relatively small sample sizes, selected populations, a multicenter design, or several surgeons grading the lesions. More importantly, most of them failed to characterize the precise location and the severity of cartilage and meniscus injuries in adequate detail.
Accurate documentation of cartilage and meniscus injury is important in order to permit comparative analysis of similar injuries. The IKDC (International Knee Documentation Committee) has provided a widely used tool to assess outcomes after anterior cruciate ligament injury and to grade the severity of cartilage lesions7-9. Precise documentation of the cartilage surface can be obtained by mapping with use of the ICRS (International Cartilage Repair Society) classification system10. The classification of meniscus lesions has been based on patterns of injury or arthroscopic appearance, and the systems have varied considerably in the literature11-13. In order to better classify meniscus injuries, Cooper et al.12 divided the meniscus into eighteen different anatomical zones.
The purpose of the present investigation was to build on the earlier studies and to determine the association between patient sex, age at the time of surgery, and surgical delay (the time between an injury and anterior cruciate ligament reconstruction) with the frequency and location of meniscus and femoral articular cartilage lesions seen at the time of anterior cruciate ligament reconstruction. Our hypothesis was that advancing age and surgical delay will increase the frequency and severity of articular cartilage and meniscus lesions in the knee.
Materials and Methods
Approval for this study was obtained from the institutional review board at the University of Vermont College of Medicine.
The data for the present study were obtained from a database of 1209 consecutive patients who had undergone anterior cruciate ligament reconstruction, performed with use of the same operative procedure by the same orthopaedic surgeon (R.J.J.), between 1988 and 2002. Ligament, femoral articular cartilage, and meniscus injuries were recorded in the charts by the senior surgeon (R.J.J.) at the time of the index procedure.
Any person with an anterior cruciate ligament injury who elected to have a primary anterior cruciate ligament reconstruction was considered for inclusion in the study. We excluded all individuals who had a grade-3 medial collateral ligament, lateral (fibular) collateral ligament, or posterior cruciate ligament injury (evaluated and recorded at the time of surgery by means of examination with the patient under anesthesia); a knee dislocation; or a revision procedure involving the anterior cruciate ligament. The study sample consisted of the remaining 1104 patients.
All articular cartilage, meniscus, and ligament injuries of the knee were confirmed in the operating room by means of physical examination and arthroscopy. The surgeon identified articular cartilage and meniscus injuries at the time of surgery and recorded the results on anatomic maps that were retrospectively converted to appropriate categorization systems. Specifically, meniscus injuries were classified according to the system described by Cooper et al.12 (see Appendix), the grade and depth of articular cartilage lesions were classified according to the ICRS system (see Appendix), and the surface area of cartilage loss was measured with use of the IKDC system (with the lesions being classified as small [<5 mm], medium [5 to 10 mm], or large [>10 mm]).
A certain proportion of the meniscus tears were complex. Some tears crossed the middle and posterior one-third zones and were categorized separately as crossing zone AB (posteromedially) or zone EF (posterolaterally) (see Appendix). Other meniscus tears were identified in a radial direction across zones 1, 2, and 3 and were categorized separately as spanning zones 1, 2, and 3 (see Appendix). Relatively few meniscus injuries were identified in the anterior two-thirds of the medial or lateral meniscus. Therefore, the analysis of the data involving the meniscus combined the injuries in the anterior two-thirds of the medial and lateral meniscus into two groups (see Appendix).
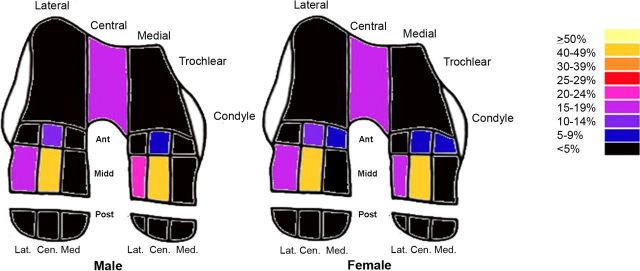
The articular cartilage injuries were located primarily in the central area of the ICRS 3 × 3 matrix on the femoral condyle with extensions to adjacent portions (see Appendix). Cartilage injuries in the middle-central area with a minor extension to any other portion of the 3 × 3 matrix were only counted in the middle-central area. For the purpose of data analysis, the matrix was collapsed into seven areas: anterior-central, middle-central, and peripheral on the lateral side, and anterior-central, middle-central, peripheral, and middle-lateral on the medial side (see Appendix).
Three independent variables were considered in the present study: sex, age at the time of surgery, and surgical delay (defined as the interval, in days, between the index anterior cruciate ligament injury and anterior cruciate ligament reconstruction). These data were obtained from the patient's chart. For the purpose of statistical analysis and comparisons, age at the time of surgery was divided into two groups (less than twenty-five years and twenty-five years or more) on the basis of the median age of the patients in the sample (twenty-five years). To explore the effect of advancing age, a second age comparison was performed between patients who were less than thirty-five years old and those who were thirty-five years old or more. Surgical delay was divided into three categories according to when the anterior cruciate ligament reconstruction was performed (less than three months after the injury, between three and twelve months after the injury, and more than one year after the injury). The grouping categories for surgical delay affected the comparisons that were made. Any patient whose injury date was too vague or who had multiple injuries was deleted from the analysis when the model included this variable. The exact dates of injury were not always known. A sensitivity analysis was not performed because patients clearly fell into one of the selected groups.
Lesion types and locations were first evaluated with log-linear analysis. This approach allows for adjustments by including covariates (e.g., there were more young female patients) and by checking for possible interactions. The post hoc analyses were done with use of the binomial test with an adjusted alpha (0.05/number of comparisons). This test is known to be very conservative; therefore, when the overall test was significant but the binomial test was not, the comparison with the largest discrepancy was reported as a trend. Lesion size and grade were evaluated with use of the Wilcoxon-Mann-Whitney test. Analyses of the patterns of specific injury sites (“location”) were done separately for the medial and lateral sides because a number of patients had injuries on both sides, indicating a lack of independence.
For group comparisons, some patients were excluded from analysis because of missing data. For example, 112 patients without clear-enough information were excluded from the surgical delay comparisons because the time of the injury was not reported or because the anterior cruciate ligament injury was thought to have been caused by multiple injury episodes, sometimes spanning several years. Patients in whom the injury had occurred less than three months before the procedure were most likely to have an exact date for the injury.
One patient was excluded from the comparisons based on sex because the sex of the patient could not be determined from the files. Six patients were excluded from the comparisons based on age because age was not recorded or could not be determined accurately from the charts.
Source of Funding
Salary support was provided by the Academy of Finland and by an Orthopaedic Research and Education Foundation (OREF) Clinician Scientist Award.
Results
Thirty-nine percent (431) of the 1104 patients were female. The mean age at the time of surgery was twenty-six years (range, twelve to fifty-six years). For 112 patients, the time of the injury was not reported. Of the 992 patients who were analyzed with regard to surgical delay, 412 (42%) had surgery less than three months after the injury, 274 (28%) had surgery between three and twelve months after the injury, and 306 (31%) had surgery more than one year after the injury. Most of the injuries occurred during downhill skiing or snowboarding (40%), basketball (16%), American football (6%), other sports and activities (15%), or work-related events (2%); for the remaining injuries (21%), no cause was listed.
Significant associations were found between the three independent variables. Among patients who were less than twenty-five years old, female patients tended to be younger than male patients. Patients who were twenty-five years old or more were more likely to have longer surgical delays. Log-linear analyses were used to adjust for these associations in the results reported below.
Meniscus Injury
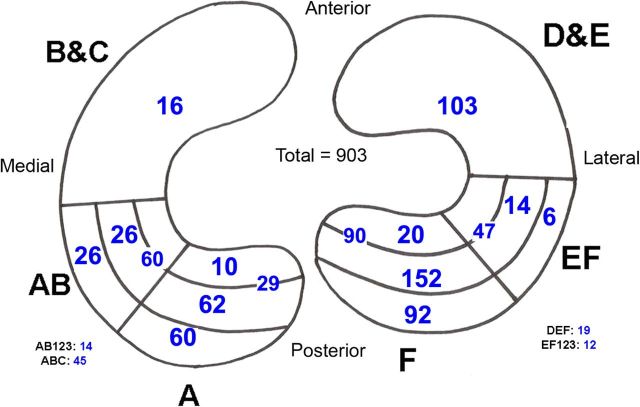
Meniscus injuries were identified in 722 patients (65%). In this group, both the medial and the lateral meniscus were injured in 186 patients (26%), the lateral meniscus was injured in 378 patients (52%), and the medial meniscus was injured in 157 patients (22%). One meniscus injury was excluded because it was not classifiable. The distribution of the meniscus injury patterns is presented in Figure 1.
Fig. 1.
Diagram illustrating the overall distribution of meniscus lesions. The different zones are based on the anatomic description of meniscus injury reported by Cooper et al.12.
Frequency of Meniscus Lesions
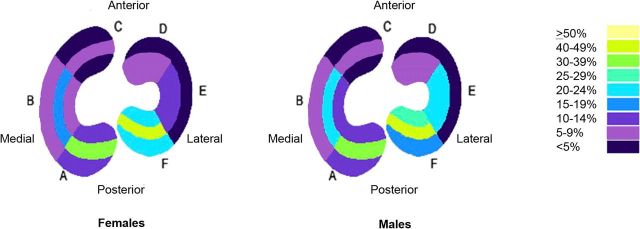
Sex was found to be associated with meniscus injury after adjusting for age (p < 0.0001). Female patients were more likely to have no injury than male patients were (44% compared with 29%; p = 0.0005), and male patients were more likely to have combined medial and lateral meniscus injuries than female patients were (20% compared with 11%; p = 0.002) (Fig. 2-A and Table I). No significant associations between age and the frequency of meniscus injury were found after adjusting for sex and surgical delay (Fig. 2-B). After adjusting for age, patients who had a surgical delay of less than three months were less likely to have a medial meniscus injury than were those who had a longer delay (8% compared with 19%; p = 0.0006) (Table I). After adjusting for age, patients for whom surgery was delayed for more than one year were less likely to have no injury (21% compared with 41%; p < 0.0001) and were more likely to have a combined medial and lateral meniscus injury (27% compared with 13%; p = 0.0001) than were patients for whom surgery was delayed for one year or less (Fig. 2-C and Table I).
Fig. 2-A Fig. 2-B Fig. 2-C.
Figs. 2-A, 2-B, and 2-C Diagrams illustrating the frequency of meniscus injury according to different factors, presented as a percentage of the total number of injuries involving the meniscus. The meniscus injury groupings are based on the anatomic description of meniscus injury as reported by Cooper et al.12. Fig. 2-A Diagram illustrating the frequency of meniscus injury according to sex. Fig. 2-B Diagram illustrating the frequency of meniscus injury according to age. Fig. 2-C Diagram illustrating the frequency of meniscus injury according to surgical delay.
TABLE I.
Associations Between Lesion Characteristics (Frequency, Location, and Type) and Independent Variables (Sex, Age, and Surgical Delay) in Patients of All Ages*
| Lesion Characteristics and Independent Variables | Overall Test (p value) | Post Hoc Tests |
| Frequency of meniscus injuries | ||
| Sex | <0.0001 | Male patients more likely to have combined medial and lateral injuries (20% compared with 11%), female patients more likely to have no injury (44% compared with 29%) |
| Surgical delay | <0.0001 | Patients with surgical delay of 0 to 2 months less likely to have medial injury (8% compared with 19%), patients with delay of >1 year less likely to have no injury (21% compared with 41%), patients with a delay of >1 year more likely to have combined medial and lateral injuries (27% compared with 13%) |
| Location of meniscus injuries (each side evaluated separately) | ||
| Sex | 0.04 (lateral side) | Trend: Female patients more likely to have injury of posterior horn, male patients more likely to have injuries involving anterior and middle thirds |
| Frequency of femoral cartilage lesions | ||
| Sex | 0.06 | |
| Age | <0.0001 | Patients with an age of ≥25 years more likely to have multiple lesions (8% compared with 1%), patients with an age of ≥25 years more likely to have isolated medial femoral condyle lesions (24% compared with 13%), patients with an age of 18 to 24 years more likely to have no lesions (67% compared with 47%) |
| Surgical delay | 0.006 | Patients with a delay of >1 year less likely to have no lesions (40% compared with 53%), patients with a delay of >1 year more likely to have combined lateral and medial condyle lesions (15% compared with 6%) |
| Location of femoral cartilage lesions (each side evaluated separately) | ||
| Age | 0.02 (medial side) | Trend: Patients with an age of ≥25 years more likely to have middle-central and middle-lateral injuries |
| Surgical delay | 0.005 (medial side) | Patients with a delay of >1 year less likely to have middle-lateral lesions (13% compared with 31%) |
| Type (grade and size) of lateral femoral condyle lesions | ||
| Surgical delay | 0.005 (size) | Patients with a delay of >1 year more likely to have large lesions (21% compared with 5%) |
| Surgical delay | 0.05 (grade) | Patients with a delay of >1 yr more likely to have grade-3 and 4 lesions (24% compared with 9%) |
| Type (grade and size) of medial femoral condyle lesions | ||
| Sex (× age)† | 0.02 (grade) | Older patients only: males more likely to have grade-4 lesions, females more likely to have grade-1 lesions |
| Age (× sex)† | 0.003 (grade) | Males only: patients with an age of ≥25 years more likely to have higher-grade lesions |
| Surgical delay | 0.004 (size) | Patients with a delay of 0 to 2 months more likely to have small lesions, patients with a delay of >1 yr more likely to have large lesions |
For statistical analysis, the age of twenty-five years was based on the median age of the sample. Surgical delay was divided into three categories (within three months after the injury, between three and twelve months after the injury, and more than one year after the injury).
Interaction was found.
Location of Injury within the Medial or Lateral Meniscus
Lateral meniscus injuries and the sex of the patient were associated after adjusting for age (p = 0.04). There was a trend for female patients to have more injuries in the posterior horn of the lateral meniscus near the periphery in zones 1 and 2 (Table I). Male patients had more injuries in the anterior and middle horns of the lateral meniscus than did female patients. However, no association between sex and the location of injury within the medial meniscus was found after adjusting for age. No significant associations between age and the location of meniscus injury were found after adjusting for sex and surgical delay. Surgical delay was not associated with the location of medial or lateral meniscus injuries after adjusting for age.
Articular Cartilage Injury
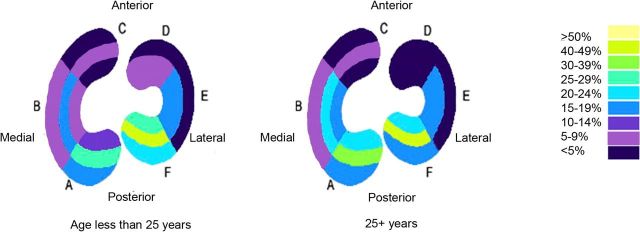
Femoral articular cartilage injuries were identified in 472 patients (43%). Specifically, medial femoral cartilage injuries were found in 205 patients (43%), lateral femoral cartilage injuries were found in ninety-three patients (20%), and trochlear injuries were found in thirty-five patients (7%). Multiple articular cartilage lesions were found in 139 patients (29%); ninety-one of these lesions occurred in the medial and lateral condyles. Five cases were unclassifiable and were dropped, reducing the overall sample size to 1099. The distribution of articular cartilage injury patterns is presented in Figure 3.
Fig. 3.
Diagram illustrating the overall distribution of cartilage injuries according to sex; it is possible for there to be multiple cartilage injuries per knee. The cartilage injury groupings are based on the anatomic description of cartilage injury as reported by the ICRS10.
Frequency of Femoral Cartilage Lesions
Although the sex of the patient did not have a significant relationship with the frequency of femoral cartilage lesions, a trend was apparent (p = 0.06) (Table I) and the difference was large enough to suggest that the results were clinically relevant (Fig. 4-A and Table I). This was evidenced by the fact that more male patients than female patients had a femoral injury (48% compared with 35%). Age was a significant factor after adjusting for sex and surgical delay (p < 0.0001). Older patients were more likely to have multiple femoral cartilage lesions (7.7% compared with 1.3%; p = 0.0001), and younger patients were more likely to have no lesions (67% compared with 47.1%; p = 0.002). Older patients were more likely to have isolated medial femoral condyle lesions than younger patients were (24.2% compared with 13.3%; p = 0.004) (Fig. 4-B and Table I). Surgical delay was a significant factor after adjusting for age (p = 0.006). Patients who had a surgical delay of more than one year were less likely to have no lesions (40% compared with 53%; p = 0.003) and were more likely to have combined lateral and medial condyle lesions (15.2% compared with 5.5%; p = 0.0006) (Fig. 4-C and Table I).
Fig. 4-A Fig. 4-B Fig. 4-C.
Figs. 4-A, 4-B, and 4-C Diagrams illustrating the frequency of articular cartilage injury according to different factors, presented as the percentage of the total number of injuries involving the femoral articular cartilage. The cartilage injury groupings are based on the anatomic description of cartilage injury as reported by the ICRS10. Fig. 4-A Diagram illustrating the frequency of articular cartilage injury according to sex. Fig. 4-B Diagram illustrating the frequency of cartilage injury according to age. Fig. 4-C Diagram illustrating the frequency of cartilage injury according to surgical delay.
Location of Femoral Cartilage Lesions
The log-linear analyses did not identify significant associations for the lateral femoral condyle lesions. On the medial side, significant associations were found for age (p = 0.02, adjusted for sex) and surgical delay (p = 0.005, adjusted for age), but not for sex (Table I). Patients who had a surgical delay of more than one year had fewer middle-lateral lesions than did those with shorter delays (13% compared with 31%, p = 0.01) (Table I). There was a trend for older patients to be more likely to have injuries in the middle-central (63%) or middle-lateral (25%) regions in comparison with patients who were younger than twenty-five years of age (55% and 19%, respectively).
Type (Grade and Size) of Femoral Condyle Lesion
Age was associated with the grade (p = 0.02) but not the size of articular cartilage lesions. Nearly all grade-2 and 3 lesions were found in the older group. No association was identified with regard to sex or surgical delay and lesion grade or size.
In analyses involving the lateral femoral condyle, sex and age at the time of surgery were not associated with the grade or size of articular cartilage lesions. However, surgical delay was associated with both the grade and size of injury (p = 0.05 and p = 0.005, respectively). The pattern was that a surgical delay of more than one year was associated with a greater proportion of large (>10-mm) and grade-3 lesions (Table I).
In analyses involving the medial femoral condyle, surgical delay was associated with the size (p = 0.004) but not the grade of the cartilage injury. There were more small lesions than expected for a surgical delay of less than three months (49% compared with 34% for all others) and more large lesions than expected for a surgical delay of more than one year (19% compared with 8%) (Table I). Both sex and age at the time of surgery were found to be significantly associated with the grade of the lesion. Combined analyses suggested that these associations were true only for certain subgroups. Sex was significantly associated with the grade of the lesion in older patients only (p = 0.02): female patients had a greater proportion of grade-1 lesions in comparison with male patients (29% compared with 16%), whereas male patients had a greater proportion of grade-3 and 4 lesions in comparison with female patients (49% compared with 35%) (Table I). Age at the time of surgery was found to be related to lesion grade only among male patients (p = 0.003): the pattern showed higher-grade (grade-3 and 4) lesions for the older male patients (49% compared with 29% for younger male patients) (Table I). When both age and sex were considered, none of the analyses identified significant associations for the size of the cartilage lesion.
All of the above comparisons of meniscus and cartilage lesions were repeated in an analysis in which patients with an age of thirty-five years or more (n = 186) were compared with those with an age of less than thirty-five years. Significant results are reported in Table II. Older patients more frequently injured the medial meniscus than the lateral meniscus and had more isolated medial femoral cartilage lesions in comparison with the younger patients. Other comparisons were not significant.
TABLE II.
Associations Between Lesion Characteristics (Frequency and Location) and Patient Age in Older Patients*
| Lesion Characteristics | Overall Test (p value) | Post Hoc Tests |
| Meniscus injuries | ||
| Frequency | 0.0004 | Patients with an age of 18 to 35 years more likely to have lateral injuries (37% compared with 23%), patients with an age of >35 years more likely to have medial injuries (22% compared with 13%) |
| Location (each side evaluated separately) | 0.0007 (medial side) | Trend: Patients with an age of >35 years more likely to have A23 and AB23 injuries, patients with an age of 18 to 35 years more likely to have A1 and ABC injuries |
| Femoral cartilage injuries | ||
| Frequency | <0.0001 | Patients with an age of 18 to 35 years more likely to have no lesions (61% compared with 37%; p < 0.0001, binomial test), patients with an age of >35 years more likely to have isolated medial lesions (27% compared with 17%; p = 0.01, binomial test) |
| Location (each side evaluated separately) | 0.05 (medial side) |
The table presents the results of the comparisons when the patients were divided into two age groups (eighteen to thirty-five years and more than thirty-five years); 186 patients were more than thirty-five years old. For statistical analysis, the age of thirty-five years was selected to explore how advancing age affects meniscus and articular cartilage injury patterns after anterior cruciate ligament injury. Surgical delay was divided into three categories (less than three months after the injury, three to twelve months after the injury, and more than one year after the injury). The categories of A23, AB23, and ABC are based on the meniscus classification system of Cooper et al.12.
Discussion
The present study demonstrates that, following an anterior cruciate ligament injury, increased age, male sex, and increased surgical delay are all associated with an increase in both the frequency and the severity of injuries to the menisci and the articular cartilage. These three factors must be considered when designing studies, and they must be considered in the statistical analysis. In addition, the present study provides baseline information to help us to understand the location of cartilage and meniscus injury in the knee at the time of anterior cruciate ligament reconstruction.
Two important associations were found among the three independent variables that were studied. First, the female patients tended to be younger (64% of female patients were less than twenty-five years of age, compared with 42% of male patients). Second, older patients were more likely to have a delay in surgery (36% of patients who were older than twenty-five years had a delay of more than one year, compared with 25% of younger patients). Therefore, the distributions of age and surgical delay for the female patients relative to the male patients were not evenly (proportionately) distributed in our sample. Consequently, log-linear analyses were used to adjust for these associations in the data analysis.
In our review of the literature, we identified six reports that described intra-articular injuries that were observed at the time of anterior cruciate ligament reconstruction1-6. The present study was most similar to the reports by Tandogan et al.6, Maffulli et al.2, and O'Connor et al.4 in that we carefully mapped the intra-articular injuries and explored associations between cartilage and meniscus injury and surgical delay and age. However, the present study included a significantly higher number of female patients and a more in-depth description of the injuries to the menisci and the articular cartilage. Our findings regarding the factors associated with meniscus injury were similar to the findings reported by Tandogan et al.6, Maffulli et al.2, O'Connor et al.4, and Piasecki et al.5; however, they were different from those reported by Murrell et al.3. We found that female patients were less likely to have a meniscus injury and that male patients were more likely to have combined medial and lateral meniscus injuries. Patients who had a surgical delay of more than one year were more likely to have a meniscus injury of any type. The studies by Tandogan et al.6 and Maffulli et al.2 both demonstrated that the likelihood of observing a meniscus injury at the time of anterior cruciate ligament reconstruction increased with surgical delay, but neither group of investigators studied the relationship of this finding to the sex of the patient. Similar to us, Piasecki et al.5 reported that female patients had fewer meniscus injuries than male patients did; however, in that study, the observations for female basketball players were compared with those for male basketball players. O'Connor et al.4 reported that male patients had a higher rate of meniscus injury than female patients and that all patients had an increased risk of meniscus injury with an increased surgical delay.
Our observations regarding cartilage have several similarities to those reported by Maffulli et al.2, Tandogan et al.6, and O'Connor et al.4; however, there were also differences. In the present study, a surgical delay of more than one year was more likely to be associated with an articular cartilage lesion and to be associated with combined lateral and medial condyle lesions. For the lateral femoral cartilage, surgical delay was associated with a greater proportion of large and grade-3 lesions, whereas for the medial femoral cartilage, surgical delay was associated with larger-sized lesions. Female patients had a greater proportion of grade-1 lesions, whereas male patients had a greater proportion of grade-3 and 4 lesions. Higher-grade lesions were observed for older male patients as compared with younger male patients. Maffulli et al.2 reported that surgical delay resulted in a greater number of observed cartilage injuries. Tandogan et al.6 reported that patient age and surgical delay were associated with the presence of grade-3 or 4 chondral lesions but fewer medial femoral condyle injuries in female patients. O'Connor et al.4 reported that the risk of cartilage injury was increased with surgical delay in men but not in women. The differences reported here are likely explained by the population differences among the studies.
The importance and uniqueness of the present report lie in the overall presentation of the data from a single observer's practice. The data were collected over a long period of time during which the surgeon maintained meticulous records describing the condition of the meniscus and cartilage structures on anatomic maps. The severity and location of all injuries were recorded in a consistent manner, making data interpretation over the length of study possible. The data are generalizable to a similarly aged population of individuals who participate in skiing and outdoor activities. An important strength of the present study is the fact that the data were carefully collected at the time of surgery and were immediately recorded on anatomic maps by the same investigator, eliminating the inconsistency that could have been produced by multiple observers. However, we recognize the limitation that the accuracy and reliability of the individual who recorded the data were not evaluated. Another limitation is that the observations made at a sports medicine practice that caters to active individuals participating in outdoor activities in the northeastern United States may not reflect other geographic locations where patients participate in different outdoor activities. Last, the meniscus classification system described by Cooper et al.12 has not undergone reliability testing. However, the IKDC system is a reliable knee-specific test14 and has been adapted for use in several specific knee injury15 and meniscus injury studies16. The ICRS mapping system is a validated instrument for assessing outcomes after arthroscopic evaluation of cartilage injury and repair17-19.
In summary, the present study demonstrates that increased age, male sex, and increased surgical delay are associated with an increase in the frequency and severity of injuries of the meniscus and cartilage following an isolated anterior cruciate ligament injury. In addition, the present study provides baseline information describing the location of cartilage and meniscus injury in the knee after anterior cruciate ligament tears. Age, sex, and surgical delay all must be considered in the statistical analysis in future studies and when designing investigations that study knee articular and meniscus damage. Finally, the present study shows where the intra-articular injuries occur as well as their severity, and this information will help with the design of prospective studies that determine specifically which injury combination predisposes patients to the posttraumatic onset of osteoarthritis.
Appendix
Figures depicting the Cooper meniscus injury classification system and the ICRS cartilage injury mapping system are available with the electronic versions of this article, on our web site at jbjs.org (go to the article citation and click on “Supplementary Material”) and on our quarterly CD/DVD (call our subscription department, at 781-449-9780, to order the CD or DVD). 
Footnotes
Disclosure: In support of their research for or preparation of this work, one or more of the authors received, in any one year, outside funding or grants of less than $10,000 from the Academy of Finland and of more than $10,000 from the Orthopaedic Research and Education Foundation (Clinician Scientist Award). Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which the authors, or a member of their immediate families, are affiliated or associated.
A commentary is available with the electronic versions of this article, on our web site (www.jbjs.org) and on our quarterly CD-ROM/DVD (call our subscription department, at 781-449-9780, to order the CD-ROM or DVD).
Investigation performed at the Department of Orthopaedics and Rehabilitation, University of Vermont College of Medicine, Burlington, Vermont
References
- 1.Kaeding CC, Pedroza AD, Parker RD, Spindler KP, McCarthy EC, Andrish JT. Intra-articular findings in the reconstructed multiligament-injured knee. Arthroscopy. 2005;21:424-30. [DOI] [PubMed] [Google Scholar]
- 2.Maffulli N, Binfield PM, King JB. Articular cartilage lesions in the symptomatic anterior cruciate ligament-deficient knee. Arthroscopy. 2003;19:685-90. [DOI] [PubMed] [Google Scholar]
- 3.Murrell GA, Maddali S, Horovitz L, Oakley SP, Warren RF. The effects of time course after anterior cruciate ligament injury in correlation with meniscal and cartilage loss. Am J Sports Med. 2001;29:9-14. [DOI] [PubMed] [Google Scholar]
- 4.O'Connor DP, Laughlin MS, Woods GW. Factors related to additional knee injures after anterior cruciate ligament injury. Arthroscopy. 2005;21:431-8. [DOI] [PubMed] [Google Scholar]
- 5.Piasecki DP, Spindler KP, Warren TA, Andrish JT, Parker RD. Intraarticular injuries associated with anterior cruciate ligament tear: findings at ligament reconstruction in high school and recreational athletes. An analysis of sex-based differences. Am J Sports Med. 2003;31:601-5. [DOI] [PubMed] [Google Scholar]
- 6.Tandogan RN, Taser O, Kayaalp A, Taskiran E, Pinar H, Alparslan B, Alturfan A. Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surg Sports Traumatol Arthrosc. 2004;12:262-70. [DOI] [PubMed] [Google Scholar]
- 7.Crawford K, Briggs KK, Rodkey WG, Steadman JR. Reliability, validity, and responsiveness of the IKDC score for meniscus injuries of the knee. Arthroscopy. 2007;23:839-44. [DOI] [PubMed] [Google Scholar]
- 8.Hefti F, Müller W, Jakob RP, Stäubli H. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226-34. [DOI] [PubMed] [Google Scholar]
- 9.Irrgang JJ, Ho H, Harner CD, Fu FH. Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6:107-14. [DOI] [PubMed] [Google Scholar]
- 10.Smith GD, Taylor J, Almqvist KF, Erggelet C, Knutsen G, Portabella M, Smith T, Richardson JB. Arthroscopic assessment of cartilage repair: a validation study of two scoring systems. Arthroscopy. 2005;21:1462-7. [DOI] [PubMed] [Google Scholar]
- 11.Metcalf RW, Burks RT, Metcalf MS, McGinty JB. Arthroscopic meniscectomy. In: McGinty JB, Caspari RB, Jackson RW, Poehling GG, editors. Operative arthroscopy. 2nd ed. Philadelphia: Lippincott-Raven; 1996. p 263-97. [Google Scholar]
- 12.Cooper DE, Arnoczky SP, Warren RF. Arthroscopic meniscal repair. Clin Sports Med. 1990;9:589-607. [PubMed] [Google Scholar]
- 13.Greis PE, Bardana DD, Holmstrom MC, Burks RT. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg. 2002;10:168-76. [DOI] [PubMed] [Google Scholar]
- 14.Higgins LD, Taylor MK, Park D, Ghodadra N, Marchant M, Pietrobon R, Cook C; International Knee Documentation Committee. Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Joint Bone Spine. 2007;74:594-9. [DOI] [PubMed] [Google Scholar]
- 15.Smith GD, Taylor J, Almqvist KF, Erggelet C, Knutsen G, Garcia Portabella M, Smith T, Richardson JB. Arthroscopic assessment of cartilage repair: a validation study of 2 scoring systems. Arthroscopy. 2005;21:1462-7. [DOI] [PubMed] [Google Scholar]
- 16.Crawford K, Briggs KK, Rodkey WG, Steadman JR. Reliability, validity and responsiveness of the IKDC score for meniscus injuries of the knee. Arthroscopy. 2007;23:839-44. [DOI] [PubMed] [Google Scholar]
- 17.Ossendorf C, Kreuz PC, Steinwachs MR, Erggelet C. Autologous chondrocyte implantation for the treatment of large full-thickness cartilage lesions of the knee. Saudi Med J. 2007;28:1251-6. [PubMed] [Google Scholar]
- 18.van den Borne MP, Raijmakers NJ, Vanlauwe J, Victor J, de Jong SN, Bellemans J, Saris DB; International Cartilage Repair Society. International Cartilage Repair Society (ICRS) and Oswestry macroscopic cartilage evaluation scores validated for use in Autologous Chondrocyte Implantation (ACI) and microfracture. Osteoarthritis Cartilage. 2007;15:1397-402. [DOI] [PubMed] [Google Scholar]
- 19.Smith TO, Davies L, O'Driscoll ML, Donell ST. An evaluation of the clinical tests and outcome measures used to assess patellar instability. Knee. 2008;15:255-62. [DOI] [PubMed] [Google Scholar]