Abstract
Background
Kidney damage is associated with increased workload in high ambient temperatures, and may represent a pathway to chronic kidney disease of unknown origin in agricultural workers. We tested the associations of workload and heat with acute kidney dysfunction in California agricultural workers.
Methods
We recruited a convenience sample of 471 agricultural workers from 29 farms in California during two summer harvest seasons. Sustained 3-minute maximum workload was estimated using accelerometer data collected from Actical monitors and individual heat load through elevations in core body temperature. Acute kidney injury (AKI) was defined by a change in serum creatinine of ≥0.3mg/dL or ≥1.5 times the pre-shift creatinine over the course of the work shift. Associations between AKI and workload were modeled using logistic regression, controlling for demographic, physiologic, and occupational variables.
Results
357 workers (75.8%) had accelerometer readings in the moderate workload category, 93 (19.7%) had readings in the vigorous category. 177 (36%) had elevations of core body temperature ≥1°C. 72 workers (14.9%) demonstrated evidence of AKI after a single day of agricultural work. Workload category was associated with an increased adjusted odds of AKI (1.92, 95% confidence interval (CI) 1.05-3.51). Piece rate work was also associated with increased adjusted odds of AKI (3.02, 95% CI1.44-6.34).
Conclusions
Heavy occupational workload and piece-rate work were associated with acute effects on renal health of agricultural workers. This indicates that occupations requiring high physical effort put workers at risk for AKI, possibly independent of ambient and core body temperature. Changes to agricultural practices may reduce the risk for renal disorders for these workers.
Keywords: Acute Kidney Injury, Chronic Kidney Disease of Unknown Origin, Agricultural Workers, Metabolic Equivalents, Temperature, Occupational Risk Factors
INTRODUCTION
California employed over 829,000 farm workers in 2014, many of them undocumented immigrants from Mexico.1 The nature of the work, with its physical demands and exposure to extreme weather during harvest season, increases the potential for adverse health outcomes in this population.2–4 Recent evidence indicates an increased risk for acute kidney injury across a workshift.5 Acute kidney injury (AKI), defined as subclinical injury to the kidneys usually resulting from reduced renal blood flow, appears in as little as 8–12 hours and resolves in approximately 24–48 hours.6 It is possible that repeated episodes of AKI may lead to chronic kidney disease.7 Among agricultural workers, this is particularly concerning because of reports of chronic kidney disease of unknown origin (CKDu) principally affecting young male agricultural workers who do not have the traditional risk factors of diabetes, hypertension, or obesity.8,9 Studies of marathon runners and military recruits have documented cases of AKI resulting from periods of increased physical labor, especially when combined with heat exposure and volume depletion.10–12 These findings are echoed in studies of CKDu where a connection between kidney damage and heavy workload in high ambient temperatures is established.13,14 In wildland firefighters after prolonged physical exertion in extreme temperatures, elevations in creatine kinase, a marker of rhabdomyolysis has been noted.15 This muscle damage leads to elevations in renal injury biomarkers, indicating AKI.16 It is conceivable that similar damage induces AKI in agricultural workers. In previous work, we found an increased risk of AKI among workers who were paid by the piece, that is, by the amount they harvest.17 Workers who are paid by the piece tend to work harder and faster than those paid by the hour because they can make more money,18,19 suggesting that they experience higher work load and thus, a higher risk of AKI. We build upon our previous work and hypothesize that increased workload may result in a higher risk of AKI, a relationship that has not yet been examined in agricultural workers. Our purpose was to test associations of workload on AKI in a cohort of agricultural workers over the course of two harvest seasons.
METHODS
Participants were recruited as part of the California Heat Illness Prevention Study, and methods have been described elsewhere.17,20 Briefly, eligible participants for this study were adults age 18 or older, working in the fields for at least 6 hours per day, understood Spanish or English, and had no impediments to swallowing an ingestible sensor. All eligible participants were enrolled in the study for a single day of data collection and were given a small monetary incentive for their time. Participants were consented in their language of choice (English or Spanish) and signed written consent forms. We collected data at two time points. At pre-shift data collection, we weighed participants in a base layer of clothing, took a capillary blood sample, fitted participants with a heart rate monitor, and asked them to swallow a temperature probe. Actical accelerometers, calibrated at the manufacturer, were firmly attached to the waist belt at the iliac crest of the hip using both a Velcro band through the mounting tabs and zip ties to ensure it remained in place during rough fieldwork. The Actical measures activity in all directions and provides readings in counts per minute (cpm), which can be converted to METS.21,22 Accelerometers have been used in many studies for their convenience, negligible weight and size, and reliability. They are an objective way to measure physical activity.23 At post-shift data collection, approximately 7–10 hours after the pre-shift collection, we reweighed participants and collected another capillary blood sample. We took a seated blood pressure, measured height without shoes, and orally administered a health questionnaire in Spanish.
Outcome Variable: Acute kidney injury
We analyzed the capillary blood sample using the i-STAT point-of-care test to measure serum creatinine (Abbott Point of Care, Princeton, New Jersey, USA). The i-STAT measurements are traceable to isotope dilution mass spectrometry through the standard reference material SRM967.24 Baseline kidney function was estimated from the morning creatinine reading and categorized based on the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation:31 ≥90 mL/min/1.73m2, ≥60 to <90 mL/min/1.73 m2, or <60 mL/min/1.73 m2. We compared pre-and post-shift creatinine levels and classified AKI based on the recommended definition and stages of injury from the Kidney Disease: Improving Global Outcomes (KDIGO) group.25 AKI was defined as an increase of serum creatinine by ≥0.3mg/dL or ≥1.5 times the pre-shift creatinine. Staging was based on the following: stage 1 (≥0.3 mg/dL or 1.5-1.9 times pre-shift measure); stage 2 (2.0-2.9 times pre-shift measure); and stage 3 (≥3.0 times pre-shift measure).
Predictor Variable: Workload
Using the cpm from the Actical readings, we computed summary statistics and tallied the number of minutes at the maximum, mean, and median cpm. We used the values for the sustained 3-minute cpm for these statistics. Due to a lack of variability in the data for the mean cpm, we categorized the sustained 3-minute maximum readings based on previously published cut-off points: sedentary (<100 cpm), light activity (100 - <1,535 cpm), moderate activity (1,535 - <3,962 cpm), and vigorous activity (≥3,962 cpm).21
Covariates
We selected variables thought to be associated with AKI in occupational settings a priori based on current evidence and feasibility of collecting data in the field. Demographic variables included sex (male versus female); age (continuous); country of origin (US, Mexico, versus Central America); and primary language (English, Spanish, versus Indigenous). Occupational variables included years in farm work (≤ 5 years, 6 – 10 years, 11 – 20 years, > 20 years); method of payment (hourly/salary vs piece-rate); income (≤ $10,000, $10,001 – 30,000, >$30,000); how the participant was hired (by the farmer directly versus a labor contractor); and primary farm task during the day (picking/harvesting, hoeing/raking/shoveling/grounds-keeping, irrigation, packing/sorting, pruning, multi-tasking or other [e.g. supervising, repair, or fumigating]).26
Heat exposure during the work day was estimated using the 3-minute maximum ambient heat each day measured via a wet bulb globe thermometer (WBGT) placed in a central location at each of the sampling farms. We used a change in core body temperature over the course of the day to estimate a participant’s individual heat strain. We calculated the sustained 3-minute maximum core temperature reading during the day,20 and calculated a change in body temperature by subtracting the 3-minute maximum from the baseline reading. All participants had at least some increase in core body temperature over the course of the day, so we categorized the change as either ≥ 1 degree Celsius versus < 1 degree. Volume depletion was calculated by comparing the weight taken at post-shift to the pre-shift weight and classified as no body mass change, gained body mass, lost <1.5% body mass, or lost ≥1.5% body mass. The National Institute of Occupational Safety and Health (NIOSH), classifies workers as dehydrated if they lose more than 1.5% of their body mass during the day.27 Body mass index (BMI) was calculated from pre-shift weight and height measurements and classified according to WHO recommendations:28 normal weight (BMI<25 kg/m2), overweight (BMI 25.0-29.9 kg/m2) or obese (BMI >30 kg/m2). Diabetes status was estimated by HgA1c, via the capillary blood sample taken in the morning and self-report of diabetes or antidiabetic medicine:29 no diabetes (HbA1c<5.7% and no self-reported antidiabetic medications), pre-diabetes (HbA1c 5.7-6.4%) or diabetes (HbA1c≥6.5% or self-reported diabetes diagnosis or antidiabetic medications). We categorized blood pressure based on Joint Commission recommendations:30 normal (<120/80 and no self-reported antihypertensive medications), prehypertension (120-139/80-89) or hypertension (≥140/90 or self-reported hypertension diagnosis or antihypertension medications). We also asked about personal or family history of kidney disease (none, personal, versus family). Finally, we included two time variables in our analyses: one to account for the week of data collection to estimate if AKI occurred more frequently in workers who were sampled later in the summer or who had worked for a longer amount of time over the summer; and a second variable of year of data collection (year 1 versus year 2) to estimate differences by year that were not assessed by measured variables (e.g. shade availability, length of breaks, work team compositions, etc). Because we included participants who were part of our first analysis of AKI,17 we included the year variable to determine if there were differences between the workers in the two years.
Statistical Analysis
Participant characteristics were stratified as outlined above and frequencies and percentages calculated. Chi-square tests32 were used to compare variables frequencies between sexes. Fisher’s exact test33 was used to examine frequency differences in heat strain, volume depletion, and workload across KDIGO stage due to small sample sizes within some cells. Logistic regression36 was used to model the associations of AKI and workload as a continuous variable. We used a forward stepwise regression34 model selection technique with the Akaike value as criterion for the best fitting model.35 Analyses were then adjusted for age and sex (Model 2); followed by heat exposure variables including volume depletion (lost <1.5% body mass [reference] compared to lost ≥1.5% body mass), change in core body temperature (continuous), and 3-minute maximum WBGT (continuous) (Model 3). We added occupational variables to the next model and adjusted for the number of years in agriculture (continuous), farm task (picking compared to other [reference]), week of the harvest (continuous), and year (2014 [reference] compared to 2015). Finally, in Model 5 physiologic variables, including BMI (BMI<25 [reference], BMI 25-30, compared to BMI >30), diabetes status (A1c<5.7% [reference] compared to A1c≥5.7%), blood pressure (<120/80 [reference], compared to ≥120/80), history of kidney disease (none [reference] compared to personal or family history), and the eGFR (continuous) were added.
To examine the effect piece rate work may have on the relationship of workload with AKI, we tested an interaction of payment type with workload. However, due to model quasi-separation issues, we were unable to include the interaction term in our model. We did run models to test the interaction of sex and workload and sex and payment type. Those were not significant and did not change estimates appreciably.
All analyses were completed using SAS v 9.4 and Stata 12.
The study protocols and procedures were approved by the Institutional Review Board of the University of California, Davis, where the study was conducted.
RESULTS
Participant Characteristics
We collected results from 492 participants, but we only had complete results on 471, who were included in this analysis. There were 298 male and 173 female participants. Demographic and health data are shown in Table I. Our sample was mostly over age 25, and only 7.43% were born in the United States. The majority spoke Spanish as their primary language. The majority of participants reported working in farm work for more than 6 years, and men reported more years in farm work than women (p<0.01). Most participants were paid by the hour or salaried, versus piece-rate, and the median yearly income was between $10,001 and $30,000, though men reported earning more money than women (p<0.01). Men reported being hired by the farm directly more than women who tended to be hired by labor contractors (p<0.01). Women reported their main tasks as pruning or packing and sorting, while men were more often involved in picking or harvesting (p<0.01). Nearly half of the sample (44.4%) was overweight and over a third (35.5%) was obese, with women forming a higher proportion of each category than men (p=0.02). Very few participants had diabetes (4.7%), and 16.1% had pre-diabetes. Most participants were either pre-hypertensive (48.0%) or hypertensive (23.4%); men were more likely to be pre-hypertensive while women were more likely to have normal blood pressure (p<0.01). Most participants had normal eGFR, while 4.5% had eGFR between 60 and 89 ml/min/1.73m2, and most (91.0%) reported no personal or family history of kidney disease. We included 240 participants from 2014 and 231 participants from 2015.
Table I.
Characteristic of Study Participants
| Total Sample (n=471) | Male (n=298) | Female (n=173) | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p-valuea | |
| Age Group | 0.19 | ||||||
| 18-25 years | 72 | 15.29 | 52 | 17.44 | 20 | 11.56 | |
| 26-40 years | 211 | 44.80 | 127 | 42.61 | 84 | 48.55 | |
| 41-54 years | 126 | 26.75 | 76 | 25.50 | 50 | 28.90 | |
| Over 55 years | 62 | 13.16 | 43 | 14.43 | 19 | 10.98 | |
| Country of Origin | <0.01 | ||||||
| United States | 35 | 7.43 | 31 | 10.40 | 4 | 2.31 | |
| Mexico | 420 | 89.17 | 259 | 86.91 | 161 | 93.06 | |
| Central America | 16 | 3.40 | 8 | 2.68 | 8 | 4.62 | |
| Primary Language | 0.40 | ||||||
| English | 25 | 5.31 | 19 | 6.37 | 6 | 3.47 | |
| Spanish | 427 | 90.66 | 267 | 89.59 | 160 | 92.49 | |
| Indigenous | 19 | 4.03 | 12 | 4.02 | 7 | 4.04 | |
| Years in Farmwork | <0.01 | ||||||
| 5 or less | 139 | 29.64 | 82 | 27.70 | 57 | 32.95 | |
| 6-10 | 86 | 18.34 | 45 | 15.20 | 41 | 23.70 | |
| 11-20 | 141 | 30.06 | 87 | 29.39 | 54 | 31.21 | |
| More than 20 | 103 | 21.96 | 82 | 27.70 | 21 | 12.14 | |
| Payment Type | 0.20 | ||||||
| Hourly/Salary | 366 | 77.71 | 226 | 75.84 | 140 | 80.92 | |
| Piece-rate | 105 | 22.29 | 72 | 24.16 | 33 | 19.07 | |
| Income | 0.01 | ||||||
| $10,000 or less | 107 | 23.57 | 55 | 19.16 | 52 | 31.14 | |
| $10,001-30,000 | 241 | 53.08 | 157 | 54.70 | 84 | 50.30 | |
| $30,001 or more | 106 | 23.35 | 75 | 26.13 | 31 | 18.56 | |
| Hired by | <0.01 | ||||||
| Farm directly | 220 | 46.71 | 161 | 54.03 | 59 | 34.10 | |
| Labor contractor | 251 | 53.29 | 137 | 45.97 | 114 | 65.90 | |
| Farm Task | <0.01 | ||||||
| Picking/Harvesting | 140 | 29.72 | 97 | 32.55 | 43 | 24.86 | |
| Hoeing/Raking/Shoveling/Groundskeeping | 37 | 7.86 | 21 | 7.05 | 16 | 9.25 | |
| Irrigation | 47 | 9.98 | 47 | 15.77 | 0 | 0.00 | |
| Packing/Sorting | 68 | 14.44 | 20 | 6.71 | 48 | 27.75 | |
| Pruning | 94 | 19.96 | 34 | 11.41 | 60 | 34.68 | |
| Multi-task | 61 | 12.95 | 58 | 19.46 | 3 | 1.73 | |
| Otherb | 24 | 5.10 | 21 | 7.05 | 3 | 1.73 | |
| BMIc | 0.03 | ||||||
| Normal Weight (<25 kg/m2) | 95 | 20.17 | 71 | 23.83 | 24 | 13.87 | |
| Overweight (25-30 kg/m2) | 209 | 44.37 | 127 | 42.62 | 82 | 47.40 | |
| Obese (>30 kg/m2) | 167 | 35.46 | 100 | 33.56 | 67 | 38.73 | |
| HgA1cd | 0.20 | ||||||
| HgA1c <5.7% (No diabetes) | 368 | 79.14 | 239 | 81.57 | 129 | 75.00 | |
| HgA1c 5.7-6.4% (Pre-diabetes ) | 75 | 16.13 | 43 | 14.68 | 32 | 18.60 | |
| HgA1c ≥6.5% (Diabetes ) | 22 | 4.73 | 11 | 3.75 | 11 | 6.40 | |
| Blood Pressuree | <0.01 | ||||||
| Normal blood pressure (<120/80) | 135 | 28.66 | 54 | 18.12 | 81 | 46.82 | |
| Pre-hypertensive (120-139/80-89) | 226 | 47.98 | 162 | 54.36 | 64 | 36.99 | |
| Hypertension (≥140/90) | 110 | 23.35 | 82 | 27.52 | 28 | 16.18 | |
| eGFR at morning samplef | 0.21 | ||||||
| ≥90ml/min/1.73m2 | 450 | 95.54 | 282 | 94.63 | 168 | 97.11 | |
| 60-89ml/min/1.73m2 | 21 | 4.46 | 16 | 5.37 | 5 | 2.89 | |
| >60ml/min/1.73m2 | 0 | 0.00 | |||||
| History of Kidney Disease | 0.31 | ||||||
| None | 426 | 91.03 | 272 | 92.20 | 154 | 89.01 | |
| Personal History | 42 | 8.97 | 23 | 7.80 | 19 | 10.98 | |
| Family History | 92 | 19.80 | 54 | 18.40 | 38 | 22.20 | |
| Year of Data Collection | 0.35 | ||||||
| 2014 | 240 | 50.96 | 147 | 49.32 | 93 | 53.75 | |
| 2015 | 231 | 49.04 | 151 | 50.67 | 80 | 46.24 | |
Differences based on chi-square tests between males and females
“Other” includes supervising staff, machinery repair, shoveling dirt, or fumigating
BMI=Body Mass Index (kg/m2)
HgA1c=Hemoglobin A1c, from capillary blood sample
Blood pressure based on JNC7 categories
Categorized based on KDIGO guidelines
Acute Kidney Injury and Occupational Risks
Among 471 participants, 70 (14.9%) had cross-shift elevations in serum creatinine high enough to classify them as incurring AKI. A total of 59 participants (12.5%) had stage 1 AKI and 11 (2.3%) had stage 2. No participant was classified as stage 3 AKI. There were no statistically significant differences between males and females, so we conducted subsequent analyses on pooled data for both sexes. The average 3-minute maximum WBGT during data collection was 30.3° Celsius/86.5° Fahrenheit (95% confidence interval [CI] 27.11° - 33.4°C/80.8° - 92.1°F). None of the participants had a 3-minute maximum workload in the sedentary category, and 21 (4.5%) had 3-minute maximum values in the light work category. The majority of the sample (357 participants, 75.8%) had 3-minute maximum workload measurements in the moderate category, and 93 participants (19.7%) had 3-minute maximum measurements in the vigorous category. There were no statistically significant differences in workload categories based on sex, change in core body temperature, payment method, or year of data collection. There were differences in volume depletion and acute kidney injury. Relatively few people in the vigorous category had no body mass change (16.7%) or gained body mass (14.8%), which suggests that few of these hardest-working participants were adequately hydrated across their shift (p=0.02). 60% of those who lost more than 1.5% of their body mass during the shift were in the moderate category, and 38% were in the vigorous category (p=0.02). For participants in the vigorous workload category, 17.2% had no AKI, 33.9% had stage 1 injury, and 36.4% had stage 2 injury (p=0.03). Results shown in Table II.
Table II.
Maximum Workload, Occupational Risk Factors, and Acute Kidney Injury (n=471)
| Light (100 - 1,534 cpm) | Moderate (1,535-3,691 cpm) | Vigorous (≥3,692 cpm) | p-valueg | Row Total | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Total Sample (n=471) | 21 | 4.5 | 357 | 75.8 | 93 | 19.7 | ||
| Sex | 0.10 | |||||||
| Male | 11 | 3.7 | 220 | 73.8 | 67 | 22.5 | 298 | |
| Female | 10 | 5.8 | 137 | 79.2 | 26 | 15.0 | 173 | |
| Volume Depletionb | 0.02 | |||||||
| No body mass change | 2 | 11.1 | 13 | 72.2 | 3 | 16.7 | 18 | |
| Gained any body mass | 3 | 2.8 | 89 | 82.4 | 16 | 14.8 | 108 | |
| Lost <1.5% body mass | 15 | 5.1 | 224 | 76.2 | 55 | 18.7 | 294 | |
| Lost ≥1.5% body mass | 1 | 2.0 | 30 | 60.0 | 19 | 38.0 | 50 | |
| Change in Core Body Temperaturec | 0.59 | |||||||
| < 1°C | 14 | 4.8 | 226 | 76.9 | 54 | 18.4 | 294 | |
| ≥ 1°C | 7 | 4.0 | 131 | 74.0 | 39 | 22.0 | 177 | |
| Payment Method | 0.23 | |||||||
| Piece-Rate | 19 | 5.2 | 279 | 76.2 | 68 | 18.6 | 366 | |
| Hourly/Salary | 2 | 1.9 | 78 | 74.3 | 25 | 23.8 | 105 | |
| Acute Kidney Injury | 0.03 | |||||||
| No injury | 19 | 4.7 | 313 | 78.1 | 69 | 17.2 | 401 | |
| Stage 1 | 2 | 3.4 | 37 | 62.7 | 20 | 33.9 | 59 | |
| Stage 2 | 0 | 0.0 | 7 | 63.6 | 4 | 36.4 | 11 | |
| Year of Data Collection | 0.13 | |||||||
| 2014 | 10 | 4.2 | 191 | 79.6 | 39 | 16.3 | 240 | |
| 2015 | 11 | 4.8 | 166 | 71.9 | 54 | 23.4 | 231 | |
Workload categorized by sustained 3-minute maximum counts per minute from accelerometer data
Volume depletion estimated by percent change in body mass (post-shift weight - pre-shift weight ) x 100%/Pre-shift weight
Estimated from elevation from baseline reading from ingested sensor
Estimated from serum creatinine measurements and classified per Kidney Disease Improving Global Outcomes
Stage 1 classified based on meeting at least one of the criteria
p-value based onFisher’s exact tests
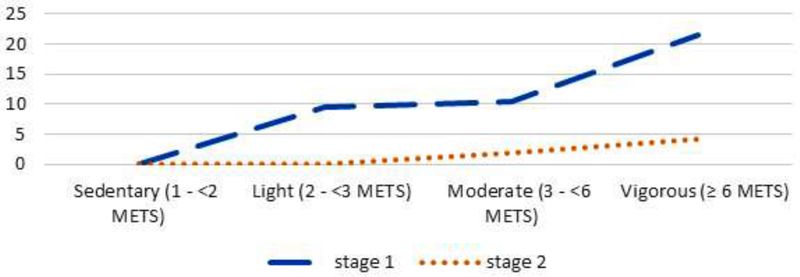
When we looked at AKI as a binary variable ( AKI ≥ stage 1 v. not), we found that of those with vigorous workload measurements, 25.8% had AKI contrasted with 12.3% of those with moderate workload, and only 9.5% with light workload (p<0.01). These results are illustrated in Figure 1, which shows the dose-response relationship of workload to AKI and demonstrates that as workload increased, participants with cross-shift AKI increased.
Figure 1.
Percent of workers with AKI in workload categories
Results from the logistic regression models are shown in Table III. In the unadjusted model, the 3-minute maximum workload was significantly associated with AKI with an odds ratio (OR) 2.28, (95% confidence interval [CI] 1.36-3.85). This association changed little with the addition of age and sex variables. Variables related to heat exposure (volume depletion, change in core body temperature, and maximum daily WGBT) similarly did not change the estimates for workload (adjusted odds ratio [AOR] 2.21, 95% CI 1.28-3.82). Addition of occupational variables (Model 4) resulted in a small decline in the AOR for workload to 2.17 (95% CI 1.23-3.81) while piece-rate work was associated with an AOR for AKI of 2.75 (95% CI 1.39-5.47). Year of data collection was also statistically significantly associated with higher odds of AKI: those sampled in 2015 had AOR 2.17 of AKI (95% CI 1.21-3.91). In the final model, after adding physiologic characteristics that may increase the risk for AKI, workload remained statistically significantly associated with AKI, though the AOR reduced to 1.92 (95% CI 1.05-3.51). Piece rate work remained significant with increased adjusted odds of AKI (AOR 3.02, 95% CI 1.44-6.34). The association with the year of data collection was no longer statistically significant in this model. Maximum daily temperature, independent of workload, showed a small association with AKI in the final model (AOR 1.09; 95% CI 1.00-1.20). Using the Akaike criteria for model selection, the Model 5 (AIC 358.56) was the best fit for the data.
Table III.
Odds of Acute Kidney Injurya based on Logistic Regression (n=471)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | AOR | 95% CI | p-value | AOR | 95% CI | p-value | AOR | 95% CI | p-value | AOR | 95% CI | p-value | ||||||
| 3-Minute Maximum Workloadb | 2.28 | 1.36 - 3.85 | <0.01 | * | 2.23 | 1.31 - 3.79 | <0.01 | * | 2.21 | 1.28 - 3.82 | 0.01 | * | 2.17 | 1.23 - 3.81 | 0.01 | * | 1.92 | 1.05 - 3.51 | 0.03 | * |
| Age in years | 1.00 | 0.98 - 1.02 | 0.77 | 1.00 | 0.97 - 1.02 | 0.70 | 0.99 | 0.96 - 1.02 | 0.56 | 1.05 | 1.01 - 1.09 | 0.04 | * | |||||||
| Sex | ||||||||||||||||||||
| Male (reference) | ||||||||||||||||||||
| Female | 0.89 | 0.51 - 1.53 | 0.67 | 0.94 | 0.53 - 1.66 | 0.83 | 1.11 | 0.61 - 2.05 | 0.73 | 0.61 | 0.29 - 1.30 | 0.20 | ||||||||
| Volume Depletionc | ||||||||||||||||||||
| Lost <1.5% body mass (reference) | ||||||||||||||||||||
| Lost ≥1.5% body mass | 0.65 | 0.27 - 1.57 | 0.34 | 0.52 | 0.21 - 1.29 | 0.16 | 0.55 | 0.21 - 1.40 | 0.21 | |||||||||||
| Change in Core Body Temperature | 1.76 | 0.83 - 3.74 | 0.14 | 1.8 | 0.81 - 4.04 | 0.15 | 2.00 | 0.85 - 4.72 | 0.11 | |||||||||||
| Max daily WBGT | 1.01 | 0.93 - 1.10 | 0.80 | 1.06 | 0.97 - 1.15 | 0.81 | 1.09 | 1.00 - 1.20 | 0.05 | |||||||||||
| Piece Rate Workd | 2.75 | 1.39 - 5.47 | <0.01 | * | 3.02 | 1.44 - 6.34 | <0.01 | * | ||||||||||||
| Years in Agricultural Work | 1.02 | 0.99 - 1.05 | 0.23 | 1.02 | 0.99 - 1.06 | 0.23 | ||||||||||||||
| Farm Task | ||||||||||||||||||||
| Picking | 1.40 | 0.75 - 2.61 | 0.30 | 1.57 | 0.81 - 3.04 | 0.18 | ||||||||||||||
| Other (reference) | ||||||||||||||||||||
| Week | 1.02 | 0.95 - 1.09 | 0.66 | 1.04 | 0.97 - 1.12 | 0.30 | ||||||||||||||
| Year | 2.17 | 1.21 - 3.91 | 0.01 | * | 1.18 | 0.61 - 2.30 | 0.62 | |||||||||||||
| BMIe | ||||||||||||||||||||
| Normal Weight (BMI<25) (reference) | ||||||||||||||||||||
| Overweight (BMI 25-30) | 0.69 | 0.32 - 1.51 | 0.35 | |||||||||||||||||
| Obese (BMI >30) | 1.20 | 0.54 - 2.68 | 0.65 | |||||||||||||||||
| Diabetesf | ||||||||||||||||||||
| A1c <5.7% (reference) | ||||||||||||||||||||
| A1c ≥5.7% | 0.66 | 0.31 - 1.42 | 0.29 | |||||||||||||||||
| Blood Pressureg | ||||||||||||||||||||
| Normal blood pressure (<120/80) (reference) | ||||||||||||||||||||
| Elevated blood pressure (≤120/80) | 1.05 | 0.51 - 2.18 | 0.90 | |||||||||||||||||
| History of Kidney Disease | ||||||||||||||||||||
| None (reference) | ||||||||||||||||||||
| Personal or Family History | 1.20 | 0.63 - 2.29 | 0.58 | |||||||||||||||||
| Baseline eGFR | 1.07 | 1.04 - 1.10 | <0.01 | * | ||||||||||||||||
| AIC | 390.47 | 394.20 | 394.53 | 378.42 | 355.07 | |||||||||||||||
Acute kidney injury based on KDIGO classification of elevations in serum creatinine
Workload as continuous data from Actical counts per minute
Percent body mass lost based on comparing pre-shift weight in kilograms and post-shift weight in kilograms
Payment by the piece compared to by the hour or salaried
BMI=Body Mass Index (kg/m2) categorized based on WHO recommendations
HgbA1c=Hemoglobin A1c, from capillary blood sample
Blood pressure based on JNC7 categories
significant at α<0.05
DISCUSSION
In a sample of 471 agricultural workers, we found evidence for AKI across a work shift in 70 (14.9%) participants. Payment type (piece work) and workload were significantly associated with higher odds of AKI. Our estimates of AKI in two years of data collection are slightly higher than we previously estimated in a single year of data collection (12.4%).5 The current work builds on our previous estimates by investigating the potential role of workload on the incidence of AKI during a work shift. We find that increased workload is associated with a nearly two-fold increase in the odds of developing AKI at work. Studies in Central America of agricultural workers with CKDu suggest that increased workload contributes to decreased renal function and potentially leads to chronic kidney disease.37,38 Interventions designed to encourage workers to rest and hydrate throughout the workday target this assumption, and are successful in reducing the number of persons with kidney damage.39 In California, occupational regulations seek to protect workers by promoting rest breaks, regular hydration, and the provision of shade (Cal-OSHA Heat Illness Regulation 3395). It is unclear whether these regulations are sufficient to protect the health of the kidneys, but these findings suggest that the importance of rest cannot be overstated.
The link between high physical exertion and renal disorders is well-documented. For example, workers who are chronically dehydrated and who have high levels of exertion in high ambient temperatures have a higher risk of kidney stones.40,41 Associations between high levels of physical activity and kidney function have been shown in studies of athletes who experience AKI after intense physical exertion.10,42 When the body’s workload increases, muscle injury may result, with release of myoglobin, which lodges in kidney tubules. This process of rhabdomyolysis, which is usually benign, can be aggravated by external factors such as heat and dehydration.43 Additionally, if previous instances of muscle damage are combined with strenuous exercise, the risk of AKI increases, independent of hydration status.44 While the majority of our sample had activity readings in the moderate workload category, the association between higher workload and AKI suggests that workers who work multiple days in a row may incur injuries that compound across a working period. On the other hand, one study of AKI conducted in the lab during exercise in the heat showed that as participants were acclimated to exertion in the heat, subsequent elevations in serum creatinine were not as severe, due to the capacity of the kidneys for autoregulation.45 The importance of acclimatization cannot be understated in agricultural workers and is part of the NIOSH recommendations to prevent heat related illness in workers. We did not have enough variability in our data to assess acclimatization, but we attempted to estimate this using the week of the harvest as a variable. As this estimate proved non-significant in our analyses, we cannot make a clear statement about the acclimatization of our sample and the effect this has on the development of AKI.
Independent of the effect of workload on kidney function, we found that workers paid by the piece had higher odds of AKI. This finding is surprising, given the assumption that those piece-rate payment incentivizes the worker to work faster and harder to earn more money.46 This is especially true when work is seasonal and irregular,47 though we found no statistically significant differences in the workload categories between those who were paid by the piece and those who were paid hourly or on salary. Studies of workers who are paid by the piece continuously cite increased risks from this method of compensation, even though this is a popular method of payment because workers can make more money for less time working.46 Our previous work found that workers paid by the piece were at increased risk of AKI when we examined piece-rate work independently.17 This work builds upon that report with the finding that piece-rate work exerts its own effect on AKI, independent of workload; however because we did not find a significant interaction between piece-rate work and workload, these two variables need to be considered independent risk factors for AKI. Piece-rate work may capture other working conditions, which we did not include in our data collection. It is possible that workers paid by the piece take shorter breaks than those paid by the hour. It is also conceivable that piece-rate workers have more peer pressure than hourly workers do, especially if they are paid piece-rate as a team. Piece-rate work increases the likelihood that a worker will experience heat-related illness and even death,3,48 and while piece-rate work was not associated with heat strain in our work, nor was heat strain associated with AKI, other studies document the association of heat strain and AKI. A meta-analysis by Flouris and colleagues found that 15% of workers who experience heat stress also experience AKI or kidney disease.49 Workers paid by the piece tend to be unauthorized immigrants with lower levels of education and English-language skills.46 We did not assess immigration status or education level, but other work points to external factors that may contribute to increased risk of AKI for piece-rate workers that we did not capture and are external to the payment mechanism alone.
We found that baseline kidney function, as estimated by the eGFR, was associated with slightly higher odds of developing AKI over the shift, as did age. We hypothesize that workers who experience the occupational risks of agricultural work that may cause harm to the kidneys are largely unaware of their injury and can repeatedly damage their kidneys with each day of work. In common with other studies of CKDu which find that kidney disease is related to occupational or environmental exposures,50 we found no association between kidney function and traditional risk factors of diabetes, hypertension, and overweight/obesity. While the demonstrable cause(s) of CKDu are as yet unknown, researchers hypothesize that CKDu could be a result of heat exposure and dehydration during the work day, as most agricultural workers affected by the disease work in extreme temperatures without adequate hydration.51 However, our findings suggest that workload and payment method appear to be stronger risks than heat exposure nor hydration in their contribution to a decrease in kidney function.
The overwhelming majority of the workers we sampled had 3-minute maximum activity levels in the moderate stage, suggesting that the agricultural work that we measured in this study may have been less physically demanding than we might have originally surmised. There are few data on the workload of agricultural workers in the literature, although most assessments of physical demand levels (e.g. O*NET, DOT) put farmworkers at the high end of workload. A pilot study of ten hand planters working in reforestation revealed that workers spend most of their day in moderate and vigorous activity,52 and another study of brush cutters reported that workers have high levels of physical activity as estimated by heart rates.19 Finally, an analysis of cane cutters (the primary occupation of those affected by CKDu) found that workers spent more than half of the day at 50% of their maximum heart rate, indicating extremely physically demanding labor.37 Workers in our sample did not log these high activity levels, perhaps because of the nature of the work which included hand sorting or pruning.26 It is difficult to compare our findings to those of cane cutters, therefore, because of the variations between the activities. Additionally, no one in our sample had eGFR<60ml/min/1.732, which further differentiates our sample from those in Central America.
Some limitations of this work should be noted. The first is the sampling method of recruiting participants at their sites of employment. This convenience sample may be biased if employers who allowed us to collect data on their farms were more likely to follow occupational regulations to protect workers. Therefore, our estimates may be low. An additional limitation is the lack of variability in the mean workload measurement. We suspected that AKI would be associated with higher workload over the course of the day, as captured by a mean workload, but we were unable to estimate this in our analysis. Our estimate of the 3-minute moving maximum workload ensured that we did not measure only one single moment of intense workload. Knowing how the maximum workload affects AKI is important because it suggests potential mechanisms inherent in hard physical labor that may affect the kidneys. Due to the design of our study, we were unable to collect data, including measures of rhabdomyolysis, to further estimate these effects. In addition, despite the potential risks of pesticide exposure on the health of the kidneys, we did not collect information on pesticide exposure in our study and are unable to include this in our analysis.53,54 A final limitation is the potential for error in our estimates of AKI based on a point-of-care test of serum creatinine. A recently published study reported that point-of-care testing may overestimate creatinine levels.55 While this is a significant potential limitation in our data, other studies of AKI in agricultural workers find similar results using different assessment methods. Strengths of this study include the large sample size collected over two summer harvest seasons and the physiologic measurements of AKI, workload, and heat strain. In particular, we use an objective measure of workload via accelerometers in a sample whose work tasks are varied.26
Our study is the first to estimate the effect of workload on measures of acute kidney injury in a sample of agricultural workers in the United States. Given the establishment of these factors as risks to kidney function in other populations, these findings have implications for occupational standards in the agricultural sector. Continued attention to NIOSH recommendations that encourage workers to rest in the shade during the workday may have effects beyond those of preventing heat-related illness, and may help protect the kidneys. Understanding potential modifications to existing work structures is important not only for the protection of workers in the United States, but also to elucidate the potential etiology of CKDu, which affects workers globally.
Acknowledgements:
The authors acknowledge the editorial assistance of Dawnette Henderson, Montana State University.
Funding: This manuscript was supported by Grant/Cooperative Agreement Numbers R01OH010243 and U54OH007550 from CDC-NIOSH. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of CDC-NIOSH.
Footnotes
Institution and Ethics approval and informed consent: The study protocols were approved by the Institutional Review Board at the University of California, Davis, where the study was conducted. All participants were consented in their preferred language (English or Spanish) via a signed paper consent form.
Disclosure (Authors): The authors declare no conflicts of interest.
Disclaimer: None
REFERENCES
- 1.Martin P, Hooker B, Akhtar M, Stockton M. How many workers are employed in California agriculture? Calif Agric. 2016;71(1):30–34. [Google Scholar]
- 2.Villarejo D, McCurdy SA, Bade B, Samuels S, Lighthall D, Williams D. The health of California’s immigrant hired farmworkers. Am J Ind Med. 2010;53(4):387–397. [DOI] [PubMed] [Google Scholar]
- 3.Arbury S, Jacklitsch B, Farquah O, et al. Heat Illness and Death Among Workers — United States, 2012–2013. 2014;63(31):20. [PMC free article] [PubMed] [Google Scholar]
- 4.Moyce SC, Schenker M. Occupational Exposures and Health Outcomes Among Immigrants in the USA. Curr Environ Health Rep. 2017;4(3):349–354. [DOI] [PubMed] [Google Scholar]
- 5.Moyce S, Joseph J, Tancredi D, Mitchell D, Schenker M. Cumulative Incidence of Acute Kidney Injury in California’s Agricultural Workers. J Occup Environ Med. 2016;58(4):391–397. [DOI] [PubMed] [Google Scholar]
- 6.Bellomo R, Kellum JA, Ronco C. Acute kidney injury. The Lancet. 2012;380(9843):756–766. [DOI] [PubMed] [Google Scholar]
- 7.Hsu RK, Hsu C- Y. The role of acute kidney injury in chronic kidney disease In: Seminars in Nephrology. Vol 36 Elsevier; 2016:283–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weiner DE, McClean MD, Kaufman JS, Brooks DR. The Central American Epidemic of CKD. Clin J Am Soc Nephrol. 2013;8(3):504–511. [DOI] [PubMed] [Google Scholar]
- 9.Nanayakkara S, Komiya T, Ratnatunga N, et al. Tubulointerstitial damage as the major pathological lesion in endemic chronic kidney disease among farmers in North Central Province of Sri Lanka. Environ Health Prev Med. 2012;17(3):213–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clarkson PM. Exertional rhabdomyolysis and acute renal failure in marathon runners. Sports Med. 2007;37(4-5):361–363. [DOI] [PubMed] [Google Scholar]
- 11.Schrier RW, Hano J, Keller HI, et al. Renal, metabolic, and circulatory responses to heat and exercise - studies in military recruits during summer training, with implications for acute renal failure. Ann Intern Med. 1970;73(2):213-. [DOI] [PubMed] [Google Scholar]
- 12.Ribeiro G, Rodrigues L, Moreira M, Silami-Garcia E, Páscoa M, Camargos F. Thermoregulation in hypertensive men exercising in the heat with water ingestion. Braz J Med Biol Res. 2004;37(3):409–417. [DOI] [PubMed] [Google Scholar]
- 13.Glaser J, Lemery J, Rajagopalan B, et al. Climate change and the emergent epidemic of CKD from heat stress in rural communities: the case for heat stress nephropathy. Clin J Am Soc Nephrol. 2016;11(8):1472–1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.García-Trabanino R, Jarquín E, Wesseling C, et al. Heat stress, dehydration, and kidney function in sugarcane cutters in El Salvador–A cross-shift study of workers at risk of Mesoamerican nephropathy. Environ Res. 2015. http://www.sciencedirect.com/science/article/pii/S0013935115300281. Accessed July 29, 2015. [DOI] [PubMed]
- 15.Eisenberg J, Methner M, Dowell CH, Mueller C. Evaluation of heat stress, heat strain, and rhabdomyolysis during structural fire fighter training. 2015.
- 16.Schlader ZJ, Chapman CL, Sarker S, et al. Firefighter Work Duration Influences the Extent of Acute Kidney Injury. Med Sci Sports Exerc. 2017;49(8):1745–1753. doi: 10.1249/MSS.0000000000001254 [DOI] [PubMed] [Google Scholar]
- 17.Moyce S, Mitchell D, Armitage T, Tancredi D, Joseph J, Schenker M. Heat strain, volume depletion and kidney function in California agricultural workers. Occup Env Med. 2017:oemed–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rubin DK, Perloff JM. Who works for piece rates and why. Am J Agric Econ. 1993;75(4):1036–1043. [Google Scholar]
- 19.Toupin D, LeBel L, Dubeau D, Imbeau D, Bouthillier L. Measuring the productivity and physical workload of brushcutters within the context of a production-based pay system. For Policy Econ. 2007;9(8):1046–1055. [Google Scholar]
- 20.Mitchell DC, Castro J, Armitage TL, et al. Recruitment, methods, and descriptive results of a physiologic assessment of Latino farmworkers: the California Heat Illness Prevention Study. J Occup Environ Med. 2017;59(7):649–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Colley RC, Tremblay MS. Moderate and vigorous physical activity intensity cut-points for the Actical accelerometer. J Sports Sci. 2011;29(8):783–789. [DOI] [PubMed] [Google Scholar]
- 22.Heil DP, Brage S, Rothney MP. Modeling physical activity outcomes from wearable monitors. Med Sci Sports Exerc. 2012;44(1S):S50–S60. [DOI] [PubMed] [Google Scholar]
- 23.Wong SL, Colley R, Gorber SC, Tremblay M. Actical accelerometer sedentary activity thresholds for adults. J Phys Act Health. 2011;8(4):587–591. [DOI] [PubMed] [Google Scholar]
- 24.Shephard MD. Point-of-Care Testing and Creatinine Measurement. Clin Biochem Rev. 2011;32(2):109–114. [PMC free article] [PubMed] [Google Scholar]
- 25.Kidney Disease Improving Global Health Outcomes (KDIGO) Working Group. Definition and classification of acute kidney injury. Kidney Int. 2012;suppl 2:19–36. [Google Scholar]
- 26.Mitchell DC, Castro J, Armitage TL, Tancredi DJ, Bennett DH, Schenker MB. Physical activity and common tasks of California farm workers: California Heat Illness Prevention Study (CHIPS). J Occup Environ Hyg. 2018;(just-accepted):1–32. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. Occupational Safety and Health Guidance Manual for Hazardous Waste Site Activities. US Department of Health and Human Services; 1985. [Google Scholar]
- 28.Organization WH, others. Global database on body mass index: an interactive surveillance tool for monitoring nutrition transition. World Health Organ; Geneva: 2012. [Google Scholar]
- 29.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Supplement 1):S62–S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. Jama. 2003;289(19):2560–2571. [DOI] [PubMed] [Google Scholar]
- 31.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sharpe DE. Your Chi-Square Test Is Statistically Significant: Now What?. In: ; 2015.
- 33.Upton GJ. Fisher’s exact test. J R Stat Soc Ser A Stat Soc. 1992;155(3):395–402. [Google Scholar]
- 34.Henderson DA, Denison DR. Stepwise regression in social and psychological research. Psychol Rep. 1989;64(1):251–257. [Google Scholar]
- 35.Sakamoto Y, Ishiguro M, Kitagawa G. Akaike information criterion statistics. Dordr Neth Reidel. 1986;81. [Google Scholar]
- 36.Peng C- YJ, Lee KL, Ingersoll GM. An introduction to logistic regression analysis and reporting. J Educ Res. 2002;96(1):3–14. [Google Scholar]
- 37.Lucas RA, Bodin T, García-Trabanino R, et al. Heat stress and workload associated with sugarcane cutting - an excessively strenuous occupation! Extreme Physiol Med. 2015;4(Suppl 1):A23. doi: 10.1186/2046-7648-4-S1-A23 [DOI] [Google Scholar]
- 38.Wegman D Heat stress intervention to prevent Chronic Kidney Disease (CKD) in El Salvador. In: 143rd APHA Annual Meeting and Exposition (October 31-November 4, 2015). APHA; 2015. https://apha.confex.com/apha/143am/webprogram/Paper321577.html. Accessed July 29, 2015. [Google Scholar]
- 39.Bodin T, García-Trabanino R, Weiss I, et al. Intervention to reduce heat stress and improve efficiency among sugarcane workers in El Salvador: Phase 1. Occup Environ Med. 2016;73(6):409–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Atan L, Andreoni C, Ortiz V, et al. High kidney stone risk in men working in steel industry at hot temperatures. Urology. 2005;65(5):858–861. [DOI] [PubMed] [Google Scholar]
- 41.Fakheri RJ, Goldfarb DS. Ambient temperature as a contributor to kidney stone formation: implications of global warming. Kidney Int. 2011;79(11):1178–1185. [DOI] [PubMed] [Google Scholar]
- 42.Lipman GS, Krabak BJ, Waite BL, Logan SB, Menon A, Chan GK. A Prospective Cohort Study of Acute Kidney Injury in Multi-stage Ultramarathon Runners: The Biochemistry in Endurance Runner Study (BIERS). Res Sports Med. 2014;22(2):185–192. doi: 10.1080/15438627.2014.881824 [DOI] [PubMed] [Google Scholar]
- 43.Patel DR, Gyamfi R, Torres A. Exertional Rhabdomyolysis and Acute Kidney Injury. Phys Sportsmed. 2009;37(1):71–79. doi: 10.3810/PSM.2009.04.1685 [DOI] [PubMed] [Google Scholar]
- 44.Junglee NA, Di Felice U, Dolci A, et al. Exercising in a hot environment with muscle damage: effects on acute kidney injury biomarkers and kidney function. Am J Physiol-Ren Physiol. 2013;305(6):F813–F820. [DOI] [PubMed] [Google Scholar]
- 45.Omassoli J, Hill NE, Woods DR, et al. Variation in renal responses to exercise in the heat with progressive acclimatisation. J Sci Med Sport. 2019;22(9):1004–1009. doi: 10.1016/j.jsams.2019.04.010 [DOI] [PubMed] [Google Scholar]
- 46.Pena AA. Poverty, Legal Status, and Pay Basis: The Case of U.S. Agriculture: Poverty, Legal Status, and Pay Basis. Ind Relat J Econ Soc. 2010;49(3):429–456. doi: 10.1111/j.1468-232X.2010.00608.x [DOI] [Google Scholar]
- 47.Flocks J, Tovar JA, Economos E, et al. Lessons Learned from Data Collection as Health Screening in Underserved Farmworker Communities. Prog Community Health Partnersh Res Educ Action. 2018;12(1S):93–100. doi: 10.1353/cpr.2018.0024 [DOI] [PubMed] [Google Scholar]
- 48.Spector JT, Krenz J, Blank KN. Risk Factors for Heat-Related Illness in Washington Crop Workers. J Agromedicine. 2015;20(3):349–359. doi: 10.1080/1059924X.2015.1047107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Flouris AD, Dinas PC, Ioannou LG, et al. Workers’ health and productivity under occupational heat strain: a systematic review and meta-analysis. Lancet Planet Health. 2018;2(12):e521–e531. [DOI] [PubMed] [Google Scholar]
- 50.Wijkstrom J, Leiva R, Elinder CG, et al. Clinical and Pathological Characterization of Mesoamerican Nephropathy: A New Kidney Disease in Central America. Am J Kidney Dis. July 2013. doi: 10.1053/j.ajkd.2013.05.019 [DOI] [PubMed] [Google Scholar]
- 51.Wesseling C, Crowe J, Hogstedt C, Jakobsson K, Lucas R, Wegman D. Mesoamerican nephropathy: report from the first international research workshop on men. 2013. http://repositorio.una.ac.cr/handle/11056/8584. Accessed March 6, 2015.
- 52.Granzow R, Schall MC, Smidt M. Full Shift Physical Activity among Reforestation Hand Planters: A Feasibility Study. Proc Hum Factors Ergon Soc Annu Meet. 2016;60(1):1018–1021. doi: 10.1177/1541931213601236 [DOI] [Google Scholar]
- 53.Ghosh R, Siddarth M, Singh N, et al. Organochlorine pesticide level in patients with chronic kidney disease of unknown etiology and its association with renal function. Environ Health Prev Med. 2017;22(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Morgan DP, Roan CC. Renal functions in persons occupationally exposed to pesticides. Arch Environ Health. 1969;19(5):633–636. [DOI] [PubMed] [Google Scholar]
- 55.Griffin BR, Butler-Dawson J, Dally M, et al. Unadjusted point of care creatinine results overestimate acute kidney injury incidence during field testing in Guatemala. PLOS ONE. 2018;13(9):e0204614. doi: 10.1371/journal.pone.0204614 [DOI] [PMC free article] [PubMed] [Google Scholar]