Abstract
Objective:
The overall goal of this study was to examine self-reported hearing quality of life (QoL) for pediatric cochlear implant (CI) recipients. Three questions were addressed: 1) How do children with CIs compare to age-mates with varying degrees of hearing loss (HL) 2) Are there differences among children with different bilateral CI device configurations? 3) Are audiological, demographic and spoken language factors related to hearing QoL?
Design:
One hundred four children (ages 7–11 years) using bimodal devices (CI and hearing aid) or bilateral CIs (BCIs) participated. The Hearing Environments and Reflection of Quality of Life (HEAR-QL) questionnaire, receptive language and speech perception tests were administered. HEAR-QL scores of CI recipients were compared to scores of age-mates with normal hearing (NH) and with mild to profound hearing loss HL.
Results:
HEAR-QL scores for CI participants were similar to those of children with varying degrees of HL, and did not differ based on device configuration. Emotion identification and word recognition in noise correlated significantly with HEAR-QL scores for the CI participants.
Discussion:
These CI recipients reported that HL poses an obstacle to social participation, though no greater than age-mates with lesser degrees of HL. Children with CIs who were better at understanding speech in noise and emotional content in speech reported fewer hearing-related difficulties on the HEAR-QL.
Conclusions:
Noisy situations encountered in everyday educational settings should be addressed for children with HL. The link between perception of emotion and hearing-related QoL for CI recipients should be further examined.
Introduction
The benefits of cochlear implants (CI) for children with severe to profound hearing loss (HL) are well documented, with several studies reporting that many pediatric CI recipients achieve age appropriate spoken language skills (Geers, Brenner, & Tobey, 2011; Niparko et al., 2010; Svirsky, Teoh, & Neuburger, 2004). These improvements in auditory and communicative skills have resulted in an increasing interest in CI recipients’ subjective perception of their social and emotional function, often globally referred to as quality of life (QoL) measures. According to the World Health Organization (WHO), QoL assessments encompass individuals’ perception of function across a number of physical, psychological and social domains (WHO, 1995). QoL assessments generally fall into two broad categories: condition specific, developed for specific clinical populations, and generic, developed for a broad range of conditions across different medical interventions. Generic health-related QoL measures allow for comparisons of different clinical interventions with typical populations and across clinical populations. Condition-specific assessments permit comparisons within a clinical population and provide nuanced information unique to a particular condition.
Two systematic literature reviews were undertaken to identify the main aspects of QoL that have been evaluated for pediatric CI recipients. Additionally, the various tools used to quantify QoL and the various factors contributing to QoL were examined (Lin and Niparko, 2006; Morettin et al., 2013). Assessment questions covered a variety of aspects of QoL, including physical and emotional well-being, communication abilities, social function and satisfaction with the CI. When using CI-specific questionnaires, parents of CI pediatric recipients generally report improvements in sound awareness, speech perception, communication skills, social skills and self-confidence (Archbold, Sach, O’neill, Lutman, & Gregory, 2008; Huttunen et al., 2009; Kelsay & Tyler, 1996; Nicholas & Geers, 2003). When using generic questionnaires, pediatric CI recipients and their parents, generally rate QoL on par with age-mates with normal hearing (NH) (Chmiel, Sutton, & Jenkins, 2000; Huber, 2005; Loy, Warner-Czyz, Tong, Tobey, & Roland, 2010; Meserole et al., 2014; Moog, Geers, Gustus & Brenner, 2011; Nicholas & Geers, 2003; Warner-Czyz, Loy, Roland, Tong, & Tobey, 2009).
Roland and colleagues (2016) conducted a meta-analysis of four studies utilizing the Pediatric Quality of Life Inventory (PedsQL). These studies included children with varying degrees of HL and devices. After pooling data across these studies, the authors found statistically and clinically significant decreases among school-aged children with HL compared to those with NH on domains of school and social functioning. These findings are particularly relevant given that education statistics show that the majority of children in the United States (US) who are deaf or hard of hearing spend some or all of their day attending general education classrooms (US Department of Education Report, 2017). Moreover, children with CIs increasingly attend schools in general education environments (as opposed to schools for the deaf) by the time they are in elementary school (Geers & Nicholas, 2013; Nittrouer, Muir, Tietgens, Moberly, & Lowenstein, 2018). The results by Roland and colleagues (2016) suggest that although a majority of children with HL attend general education classrooms, many may perceive difficulties functioning in school and social activities. Importantly, this review and the two aforementioned reviews focused exclusively on CI-users, highlight the need for well-validated hearing-specific tools that assess QoL within the population of children with HL (Lin & Niparko, 2006; Morettin et al., 2013; Roland et al., 2016).
Addressing the need for hearing-specific QoL measures, Umansky and colleagues (2011) validated a hearing-specific hearing QoL questionnaire on children ranging in age from 7–12 years old with NH and mild to profound HL. Participants completed two questionnaires; a validated pediatric generic quality of life (PedsQL) questionnaire and a hearing-specific questionnaire related to hearing environments and reflections on quality of life (HEAR-QL). Results from this study revealed that the scores for the HEAR-QL correlated moderately with scores for the PedsQL. While scores of children with HL were similar to those of age-mates with NH on the PedsQL (with the exception of school environments), children with HL scored below age-mates with NH on all subscales of the HEAR-QL. There were no significant differences in the total HEAR-QL scores for children with different levels of HL. Due to the small numbers of CI participants (N=8), their responses were not compared to other device groups in the study. Comparisons between children with CIs and other device groups may be beneficial since it has been suggested that pediatric CI recipients may have concerns related to QoL that are different from children with traditional hearing devices and less severe HL (Warner-Czyz, Loy, Tobey, Nakonezny, & Roland, 2011). Thus, having a validated hearing-specific QoL assessment may identify challenges children with HL face in day-to-day educational and social functioning and identify if there are challenges that are unique to children with a particular device or hearing level. Identifying factors associated with differences in QoL within a sample of children with HL may be valuable for implementing intervention practices that facilitate functioning in general educational environments.
Some reports have asserted that validated CI-specific QoL measures may be valuable for comparing unilateral CIs to BCIs (Hoffman, Cejas, & Quittner, 2019). One study found that BCI use, compared to unilateral CI use, is associated with higher (better) parent ratings on CI- specific QoL assessments (Sparreboom, Snik & Mylanus, 2012). Samuel et al. (2016) found that parent QoL ratings were similar for children receiving a second (2nd) CI either simultaneously or sequentially. Sarant and colleagues (2018) collected parent ratings of psychosocial QoL from a sample of 5 year olds and 8 year olds. BCI use was associated with fewer difficulties for psychosocial situations compared to unilateral CI use. These studies have not examined hearing-related QoL from the child’s perspective. Studies specifically related to how children might perceive their hearing function in daily listening environments using various bilateral CI device configurations [i.e. use of a CI and HA (bimodal devices) versus BCIs received either simultaneously or sequentially] have not been reported.
Predictors of QoL Ratings in children with CIs
Associations between QoL for pediatric CI recipients and various demographic and device variables have been inconsistent, with much of this variability likely attributable to the considerable heterogeneity across study characteristics. Reported QoL often varies with age of participants and across assessments (Huber, 2005; Stacey, Fortnum, Barton, & Summerfield, 2006; Warner-Czyz et al., 2009). Some have found that earlier age at CI or longer duration of CI use, are associated with positive QoL outcomes (Sach & Barton, 2007; Warner-Czyz et al., 2009). Several studies (Huber, 2005; Loy et al., 2010; Nicholas & Geers, 2003) have found that better speech recognition abilities, particularly when assessed in noise (Haukedal, Torkildsen, Lyxell, & Wie, 2018), are associated with better scores on QoL assessments. In a departure from using clinical word recognition measures, some studies have examined the association between perceived QoL and CI recipients’ ability to identify vocal emotions accurately. Schorr and colleagues (2009) found that the ability to identify vocal emotions (positive, neutral and negative) was positively associated with self-perceived QoL assessments in children with CIs ranging in age from 5–14 years. Geers et al. (2013) found that for a group of CI recipients ranging in age from 9–12 years old, well-developed social skills, were associated with the ability to recognize vocal emotion as well as discriminate among female talkers. More recently, investigators have found that the ability to recognize vocal emotion in speech is also positively associated with self-perceived QoL in adult CI recipients (Lou, Kern and Pulling, 2018). Since perception of emotion is fundamental to the development of social competence and social function in typically developing children (Wiefferink, Rieffe, Ketelaar, & Frijns, 2012), it may be a critical perceptional skill for optimizing QoL in CI recipients. Prosody differences found in emotional content are not preserved well in current CIs (Nakata, Trehub, & Kanda, 2012) and children with CIs have poorer perception of emotion than their age-mates with NH (Chatterjee et al., 2015; Geers et al., 2013).
Objectives:
The overall aim of this study was to examine self-reported hearing QoL for a group of pediatric CI recipients using a validated hearing-specific tool.
Three questions were addressed: 1) How do children with CIs compare to age-mates with varying degrees of HL? 2) Are there differences among children with different bilateral CI device configurations? 3) Are audiological, demographic and spoken language factors related to hearing QoL?
METHODS
Participants
HEAR-QL scores for the 104 CI recipients recruited for this study are compared with those obtained in the Umansky et al. (2011) validation study of children (N=115) with a broad range of HL. Table 1 summarizes demographic characteristics for both groups.
Table 1:
Validation and CI Group Demographics
| Age (Years) | Mean | SD | Minimum | Maximum | N |
| Validation Group | 9.65 | 1.58 | 7 | 12 | 115 |
| CI Group | 9.02* | 1.28 | 6.75 | 11.32 | 104 |
| Maternal Education | DNR | High School | College | Post-Graduate | |
| Validation Group | 3 | 15 | 49 | 27 | 94+ |
| CI Group | 0 | 18 | 47 | 39 | 104 |
| Gender | Male | Female | |||
| Validation Group | 52 | 62 | 114+ | ||
| CI Group | 54 | 50 | 104 |
CI; Cochlear Implant, SD; standard deviation, DNR; Did Not Respond,
CI group is significantly younger than the Validation group (p=.002),
some demographic data for the validation group was missing, N; Total Number of Participants.
CI Participants:
A total of 104 pediatric participants, ranging in age from 7 to 11 years, were recruited from multiple CI centers and private oral schools for the deaf across the United States. Participating CI centers and schools identified potential candidates for the study and sent letters inviting parents to consider their child’s participation in a study examining spoken language skills of children using BCIs or bimodal devices. When they brought their children to participate in testing for the study, parents completed case history forms detailing their child’s educational history, audiological and family demographics. All children had received some period of spoken language instruction in early intervention (EI) programs prior to age three. All children used spoken English as their primary language and HL as their primary diagnosis with no significant cognitive deficits reported. Approximately 71% (N=74) of these children attended private oral schools for pre-school. At the time of testing, however, a large percentage of the children (88%, N=91) attended school in a general education setting. Maternal education level was calculated in total years of education through college or beyond and was categorized into 3 groups: 1- high school (up to 12 years); 2- college (12–16 years); and 3- post graduate, (> 16 years). All children used two devices; bimodal devices or BCIs received sequentially or simultaneously. The average age at their first (1st) CI/s was 2 years (SD=1.0). The average age at the 2nd CI for children receiving BCIs was 2.9 years old (SD=1.7) and ranged from 0.7 years-7.7 years. All parents reported that their children wore their current devices (BCIs or bimodal) consistently.
Validation Study Participants:
A total of 115 children aged 7–12 years old participated (35 children with UHL, 45 with BHL and 35 siblings with NH. Parents report laterality (UHL vs. BHL) and level (normal hearing, mild to profound HL) of HL. Device use (hearing aids (HAs), bone conduction aids, CIs & remote microphone systems) was reported by the children, although not all of the children used a device (N= 39), and eight participants used CIs [6 unilateral CIs, 1 bimodal and 1BCI].
Group Comparisons:
The CI group and validation study group (Umansky et al., 2011) were compared on several demographic variables including age at test, maternal education and distribution of gender. A chi-square test of goodness-of-fit revealed that there were no significant differences between the groups for maternal education (X2 (3, N = 198) = 5.00, p = .13) or gender (X2 (2, N = 218) = .867, p = .35. The average age of the validation group and the current CI group was 9.6 years and 9.2 years respectively. Results from Mann-Whitney test (U = 4538.5, p = .002) revealed a statistically significant effect of age (validation group older). While statistically significant, a group difference of ~ 5 months in age was not considered clinically meaningful.
Procedures
Children in the CI group attended a one-day test session, which included various speech perception and language measures. Testing was conducted by members of the research team along with certified audiologists and speech language pathologists at their local CI center or school for the deaf.
Hearing Quality of Life:
The HEAR-QL is a 26-item questionnaire for children ages 7–12 and is broken down into three subscales (Environments, Activities, and Feelings): Environments: e.g. “Do you have a hard time hearing your friends at recess?” Activities: e.g. “Do you play fewer sports or participate in fewer activities than your friends because of your hearing?” Feelings: e.g. “Does your hearing loss make you feel different from everyone else?” Response choices for each item use a 5-point scale ranging from Never (4) to Almost Always (0). Scores are then reverse transformed into a 0–100 scale where higher scores indicate a better hearing QoL. A total score is calculated along with scores for each individual subscale. Children were instructed to answer the questions as if they were wearing their everyday devices (BCIs or bimodal devices). All participants completed the HEAR-QL and received assistance from an audiologist if they needed help reading the questions.
Results on the following test battery served as predictors of hearing QoL for the CI-group only.
Speech perception test battery:
The Lexical Neighborhood Test (LNT) (Kirk, Pisoni, & Osberger, 1995) monosyllabic open-set word test was administered using pre-recorded stimuli presented from a computer to a loudspeaker placed at 0° azimuth and approximately 1 meter from the child. One fifty-word list was presented at 60 dBA in multi-talker background noise (0° azimuth) at a signal to noise ratio (SNR) of +8 dB. A percent- correct LNT word score was calculated.
The Emotion Identification task presented pre-recorded sentences spoken by a female talker to assess perception of four emotional intentions: Angry, Scared, Happy and Sad (Geers et al., 2013). Children listened to 36 semantically neutral sentences with simple vocabulary and chose among the four emotions pictured on the computer screen. A percent-correct score was calculated.
The Talker Discrimination task presented a subset of pre-recorded sentences from the Indiana multi-talker speech database (Bradlow, Torretta, & Pisoni, 1996; Karl & Pisoni, 1994) spoken by eight female talkers. The child heard two different sentence scripts and indicated whether the sentences were spoken by the same person or by different people. A total of 32 sentence pairs were presented. A percent-correct score was calculated.
Receptive language test battery
The Clinical Evaluation of Language Fundamentals, fourth edition (CELF-4) (Semel, Wiig, & Secord, 2004) was administered to calculate a Receptive Language total score by combining the following three subtests: 1) Concepts and Following Directions: evaluates the ability to interpret spoken directions of increasing length and complexity (containing concepts that require logical operations) and remember names, characteristics and order of objects; 2) Word Classes - Receptive: evaluates the ability to understand relationships between words that are related by semantic class feature; and 3) Sentence Structure: evaluates the ability to interpret spoken sentences of increasing length and syntactic complexity.
The Peabody Picture Vocabulary Test- IV (PPVT) (Dunn & Dunn, 2007) was administered live voice in an auditory + visual mode and was used as a measure of receptive vocabulary. The examiner produced words and asked the child to point to the correct picture in a set of four pictures.
Raw scores for the above two tests were converted to a standard score relative to the age-appropriate normative group, where the mean is set at 100 with a SD of 15.
Analysis
Total and subscale scores on the HEAR-QL were not normally distributed for some groups, therefore, nonparametric tests were used in all group comparisons. Due to multiple comparisons, a Bonferroni adjusted alpha level of .019 per test (.05/3) was used. Comparisons on speech perception and language measures were conducted for the three CI groups using Analysis of Variance (ANOVA). Correlation analyses were used to examine the association between the various demographic, audiologic and spoken language variables and HEAR-QL scores.
RESULTS
HEAR-QL scores for NH, UHL, BHL & CI Groups
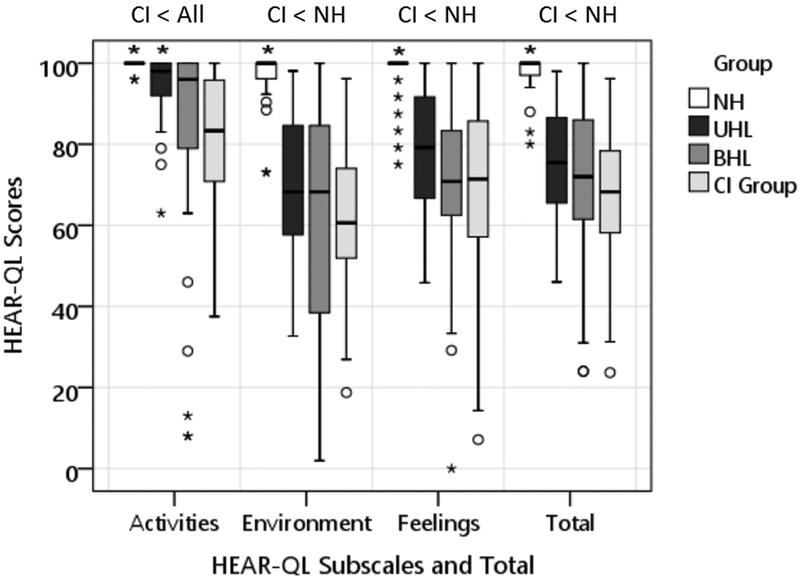
The boxplots in Figure 1 show HEAR-QL Total and subscale scores for the NH, UHL and BHL and CI groups respectively. Mean Total scores were 98, 75, 69 and 68 respectively. A Kruskal-Wallis test revealed a significant effect for group for the Total scores [(χ2(3)= 78.77, p<.001, with a mean rank score of 180.0 for the NH group, 102.3 for the UHL group, 88.9 for the BHL group and 79.4 for the CI group]. Post-hoc pairwise comparisons (Mann-Whitney U) revealed that the score for the NH group was significantly higher than the CI group (U = 63.00, p < 0.001). There were no significant differences in Total scores between the CI group and the BHL or UHL groups (U values: 1831 and 906 respectively; p values: .37 and .04 respectively).
Figure 1.
Box-plots for HEAR-QL scores for the Activities, Environments, Feelings and Total Score for NH; Normal Hearing, UHL; Unilateral Hearing Loss, BHL; Bilateral Hearing Loss; BHL and CI; Cochlear Implant groups. The limits of the box represent the lower and upper quartile of the distribution and the horizontal line through the box represents the median. Whiskers represent the minimum and maximum scores in the distribution, excluding outliers. Open-circle outliers are values between 1.5 and 3 interquartile ranges (IQR) from the end of a box; asterisk outliers are values more than 3 IQRs from the end of a box. Significant differences (p<.019) between the CI group and the HL groups are shown above each plot.
The pattern of results on the subscales were the same as on the Total scores with the CI group scoring lower than the NH group for the Environments (U = 77.5, p < 0.001) Feelings (U = 253.5, p < 0.001) and Activities subscales (U = 432.0, p < 0.001). There were no significant differences scores between the CI group and BHL or UHL group for the Environments (U values: 2156.5 and 1413 respectively; p values: .58 and .08) nor the Feelings subscales (U values: 1948 and 969 respectively; p values: .58 and .04). There were significant differences, however, in the Activities scores between the CI group and the BHL and UHL groups (U values: 1626 and 888 respectively; p values: .01 and .001).
The mean scores for the CI, BHL and UHL groups ranged from 81–94 for the Activities subscale. Higher scores on the Activities subscales indicate children reported that their HL is less likely to prevent them from participating in sports and social activities. Scores for all 3 groups for the Environments and Feelings subscales were overall lower (62–78). Lower scores on the Environments subscale indicate more difficulty listening in various challenging listening environments and lower scores on the Feelings subscale indicate more negative emotions such as anxiety and nervousness related to HL.
Within-CI Group Comparisons
Table 2 summarizes the audiologic variables for the three CI groups tested in the current study (bimodal, sequential and simultaneous BCIs). The groups did not differ significantly for age at 1st HA or unaided pre-implant PTA (F values 1.18 and 1.3 respectively; p values .27 and .31 respectively). They did differ, however, in age at 1st CI; the simultaneous BCI group received their 1st CI significantly earlier than the bimodal and sequential BCI groups (F=10.63, p<.001).
Table 2.
Hearing variables for the CI group
| Age 1st HA (months) | N | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Bimodal | 21 | 12.7 | 10.2 | 1 | 29 |
| Sequential CIs | 64 | 10.0 | 7.9 | 1 | 27 |
| Simultaneous CIs | 18 | 8.6 | 6.7 | 2 | 22 |
| Total | 103* | 10.3 | 8.3 | 1 | 29 |
| Age 1st CI (years)** | |||||
| Bimodal | 21 | 2.77 | 1.05 | 1.03 | 4.54 |
| Sequential CIs | 64 | 2.07 | 1.08 | 0.67 | 4.50 |
| Simultaneous CIs | 19 | 1.32 | 0.48 | 0.70 | 2.23 |
| Total | 104 | 2.08 | 1.08 | .67 | 4.54 |
| Unaided PTA pre-CI | |||||
| Bimodal | 21 | 91.2 | 19.9 | 37 | 125 |
| Sequential CIs | 64 | 99.7 | 14.4 | 65 | 125 |
| Simultaneous CIs | 19 | 104.8 | 15.0 | 72 | 125 |
| Total | 104 | 92.4 | 18.3 | 45 | 125 |
| Age 2nd CI (years) | |||||
| Sequential CIs | 64 | 3.39 | 1.69 | 0.69 | 7.72 |
| Simultaneous CIs | 19 | 1.32 | 0.48 | 0.70 | 2.23 |
| Total | 83 | 2.91 | 1.73 | 0.69 | 7.72 |
CI; Cochlear Implant, HA; Hearing Aid, SD; standard deviation,
one child was never fit with a HA, PTA; pure-tone average .5, 1, 2 kHz (dB HL) for the first implant ear,
; significantly different p< .05, BE; Better Ear’ N; Total Number of Participants
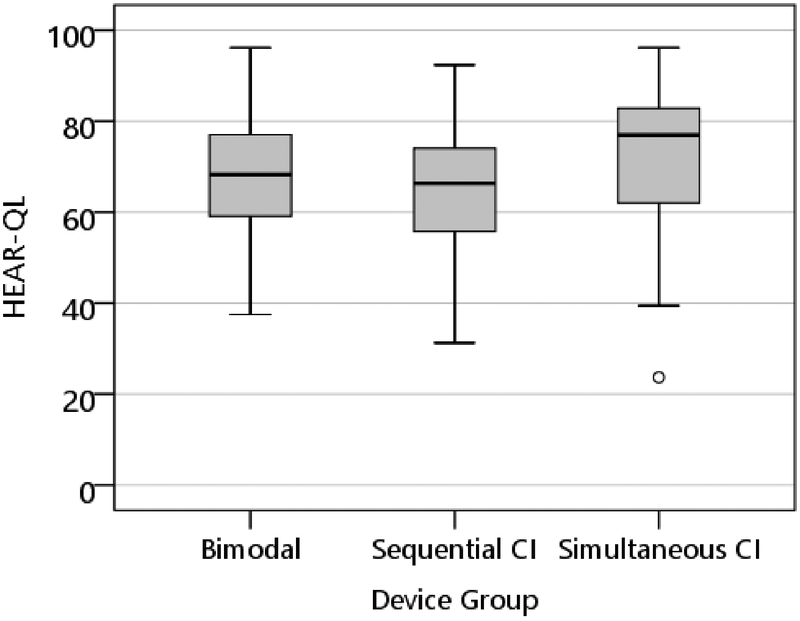
The boxplots in Figure 2 show the Total HEAR-QL scores for the bimodal group, sequential and simultaneous BCI groups (mean scores 67–71). A Kruskal-Wallis test revealed that there was not a statistically significant difference in HEAR-QL Total scores among the device groups, [(χ2(2)= 2.34, p = .310], with a mean rank score of 52.3 for the Bimodal group, 49.8 for the Sequential CI group and 61.8 for the Simultaneous CI group. Mean group scores on the three subscales for the bimodal, sequential and simultaneous BCI groups respectively were as follows: Activities, 80, 79 & 88; Feelings, 68, 67 & 75; Environment, 61, 61, & 69. Results for the three subscales revealed no statistically significant differences among groups (p values: .15, .21 & .07 respectively).
Figure 2.
Box-plots for the Total HEAR-QL scores for the Bimodal, Sequential and Simultaneous BCIs. The limits of the box represent the lower and upper quartile of the distribution and the horizontal line through the box represents the median. Open-circle outliers are values between 1.5 and 3 interquartile ranges from the end of a box.
Variables associated with HEAR-QL scores for CI recipients
Correlational analyses were conducted to examine associations between HEAR-QL Total scores and various demographic, audiologic, speech perception and spoken language measures. Table 3 shows the scores for the total group and the three CI device groups for the language and speech perception measures. Standard scores on the CELF and PPVT range from 93–103 and are within one SD of the normative mean for typically-hearing age-mates (i.e., 85–115) for the total and individual groups. No significant differences were found among the three groups for either language measure (F values: 1.53 and 1.35; p values: .22 and .26 for the CELF and PPVT respectively). As with the language measures there were no significant differences among groups for speech perception measures (F values: 1.53–2.0; p values: .13-.15). The mean LNT in noise score for the total and individual groups ranged from 61–68% and the scores for the emotion and talker discrimination ranged from 67–85%.
Table 3.
Speech Perception and Language Scores for the CI Groups
| CELF-SS | N | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Bimodal | 21 | 100.9 | 16.2 | 64 | 134 |
| Sequential CIs | 64 | 93.4 | 17.4 | 52 | 122 |
| Simultaneous CIs | 19 | 96.7 | 18.3 | 60 | 122 |
| Total | 104 | 95.5 | 17.4 | 52 | 134 |
| PPVT-SS | |||||
| Bimodal | 21 | 103.0 | 19.3 | 71 | 146 |
| Sequential CIs | 64 | 96.5 | 17.0 | 56 | 151 |
| Simultaneous CIs | 19 | 102.6 | 24.9 | 71 | 160 |
| Total | 104 | 98.9 | 19.2 | 56 | 160 |
| LNT in Noise | |||||
| Bimodal | 21 | 61.4 | 15.5 | 26 | 86 |
| Sequential CIs | 64 | 67.9 | 13.2 | 30 | 92 |
| Simultaneous CIs | 19 | 68.3 | 10.7 | 48 | 82 |
| Total | 104 | 66.7 | 13.4 | 26 | 92 |
| Emotion Identification | |||||
| Bimodal | 21 | 84.7 | 12.6 | 47.2 | 100 |
| Sequential CIs | 64 | 75.1 | 20.7 | 22.2 | 100 |
| Simultaneous CIs | 19 | 76.6 | 20.6 | 19.4 | 100 |
| Total | 104 | 77.3 | 19.5 | 19.4 | 100 |
| Talker Discrimination | |||||
| Bimodal | 21 | 70.1 | 10.9 | 40.6 | 90.6 |
| Sequential CIs | 64 | 69.5 | 11.5 | 43.8 | 87.5 |
| Simultaneous CIs | 19 | 67.1 | 11.8 | 46.9 | 84.4 |
| Total | 104 | 69.2 | 11.4 | 40.6 | 90.6 |
CI; Cochlear Implant, SD; standard deviation, SS; standard score, CELF; Clinical Evaluation of Language Fundamentals, PPVT; Peabody Picture Vocabulary Test, LNT; Lexical Neighborhood Test
None of the demographic/audiologic variables (age at test, maternal education, age at 1st HA, age at 1st CI) are significantly correlated with the Total HEAR-QL score (r values: .07 - .07; p values: .42 - .49). Table 4 shows correlations between the speech perception/language scores and the Total HEAR-QL score. The LNT in noise and the emotion identification scores show significant correlations (r values: .24 and .25; p = .011) with the Total HEAR-QL score. No other correlations are significant (r values: .05 - .17; p values: .08-.56).
Table 4.
Correlations between HEAR-QL and spoken language outcomes for CI participants.
| HEAR-QL | ||
|---|---|---|
| HEAR-QL | Pearson r | 1 |
| Sig. (2-tailed) | ||
| N | 104 | |
| PPVT SS | Pearson r | 0.056 |
| Sig. (2-tailed) | 0.575 | |
| N | 104 | |
| CELF SS | Pearson r | 0.167 |
| Sig. (2-tailed) | 0.090 | |
| N | 104 | |
| LNT in Noise | Pearson r | .241* |
| Sig. (2-tailed) | 0.014 | |
| N | 104 | |
| Talker Discrim | Pearson r | 0.143 |
| Sig. (2-tailed) | 0.147 | |
| N | 104 | |
| Emotion ID | Pearson r | .248* |
| Sig. (2-tailed) | 0.011 | |
| N | 104 | |
HEAR-QL; Hearing Environments and Reflections on Quality of Life, PPVT;
Peabody Picture Vocabulary Test, CELF; Clinical Evaluation of Functional Language,
LNT; Lexical Neighborhood Test, Discrim; Discrimination,
ID; Identification, Sig.; Significance,
N; Total Number of Particpants,
Significant at the 0.05 level (2-tailed).
DISCUSSION
The overall aim of this study was to examine self-reported hearing QoL of pediatric CI recipients using a validated hearing-specific questionnaire on children with a wide range of HL and devices.
1. HEAR-QL scores from children with HL compared to children with NH.
Previous research using generic QoL questionnaires have found that results for children with CIs are generally on par with age-mates with NH (Chmiel, Sutton, & Jenkins, 2000; Geers et al, 2003; Huber, 2005; Loy et al., 2010; Meserole et al., 2014; Warner-Czyz et al., 2009). Similarly, Umansky et al., (2011) showed that scores for the generic PedsQL did not differ significantly for children with HL and age-mates with NH. There were significant group differences, however, on the HEAR-QL. Administering the HEAR-QL to the current group of pediatric CI recipients enabled us to examine how these children rate various aspects of hearing related to participation, function and feelings in everyday situations compared to children with a range of HL.
Consistent with other CI studies, (Geers & Nicholas, 2013; Nittrouer, Muir, Tietgens, Moberly, & Lowenstein, 2018) the majority (88%) of these CI participants reported attending elementary school in a general education setting. Thus, these CI recipients listen and learn in environments with age-mates with NH, as well as those with less severe HLs. Children with CIs reported that their HL interfered with listening in certain environments (e.g., recess or sports), interfered with their participation in some activities (e.g., parties) and made them feel shy when meeting new people. They rated their hearing QoL similarly to children with varying degrees of HL regardless of degree, configuration, or devices used with the exception of lower ratings on the Activities subscale. Compared to the children with less severe HL, the majority of these children with CIs spent their early pre-school years in oral schools for the deaf and likely entered general education later. Nevertheless, the children with less severe HL reported feeling socially affected by HL, even though they presumably had better residual hearing and more time to acclimate to general education environments.
All groups of children with HL reported that their HL made them less likely to participate in school activities such as recess or sports. The children with CIs reported these difficulties even though most of them achieved spoken language skills on par with their age-mates with NH. This finding suggests that considering normal language levels sufficient for successful placement in general education classrooms does not mean that continued accommodation to HL is no longer necessary. Thus, new approaches should be implemented which address the needs of children with HL and their ability to function in daily activities.
2. HEAR-QL scores among children with different CI device configurations
Binaural hearing abilities are thought to facilitate effective communication and socialization in complex listening environments. Since children with severe to profound HL are often candidates for BCI, there has been a growing interest in examining QoL in BCI recipients.
For this group of CI recipients, bilateral input, through BCIs or bimodal devices, resulted in similar self-perceived hearing-related QoL. These comparisons were not between unilateral and bilateral device use, but instead they were between different bilateral devices. Consistent with parent ratings from the Samuels et al. (2016) study, results from the current study suggest that children rate their hearing QoL similarly, regardless of the configuration or timing of BCI.
3. Variables associated with HEAR-QL scores in children with CIs.
A number of variables were explored as potential factors contributing to HEAR-QL ratings. Age at test, maternal education, age at HA and age at CI were not related to hearing QoL. One might assume that a greater proficiency with understanding spoken language would allow for improved communication and possibly higher perceived functional benefits for a variety of school and social activities. Notably, neither receptive language nor vocabulary were associated with HEAR-QL scores for this group of CI recipients. Only two of the speech perception measures, word recognition in noise and emotion identification, correlated significantly with HEAR-QL scores. Many of the questions on the HEAR-QL are related to listening in noisy environments so the relationship to word recognition in noise may be expected. The current study, along with two studies conducted on pediatric CI recipients (Schorr et al. 2009; Geers et al. 2013), and one on adults CI recipients (Lou et al. 2018), suggest that the ability to perceive the nuances of speaker emotions may be related to positive social outcomes for CI recipients. These results are consistent with a body of literature asserting that emotional understanding has significance for communication skills and social development later on in childhood (Cutting & Dunn, 1999; Dunn, Brown, &Beardsall, 1991; Dunn, Brown, & Maguire, 1995). In addition to clinical word recognition tests, tests of emotion perception may be helpful in identifying children who are more likely to struggle in certain school and social activities. More recently, music training was found to result in improved perception of vocal emotion for pediatric CI recipients (Good et al. 2017). Thus, the possibility of rehabilitation targeting improvement in emotion perception should be explored.
CONCLUSION
The results of this study show that these children with BCIs and bimodal devices rate their overall hearing QoL similarly to children with a wide range of HL. All HL groups reported more difficulty in hearing-related situations than their age mates with NH. There were no differences in ratings among bilateral device groups (BCIs received simultaneously or sequentially, or bimodal devices). The ability to listen in noise and to recognize vocal emotion were associated with higher HEAR-QL scores. School environments need to accommodate children with HL by reducing ambient noise wherever possible. The link between emotion perception and QoL deserves further study along with methods for improving the extent to which CIs convey cues to spoken emotional content. Future directions should include an exploration of additional factors that may be associated with QoL, such as fatigue, ability to self-advocate and personality. These areas may offer guidance for facilitating function in everyday social and educational settings.
ACKNOWLEDGMENTS :
This project was supported by NIDCD T35DC008765 and NIDCD R01 DC012778 (PI: Davidson). Appreciation is expressed to Ann Geers for comments and editing of this manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Deafness and Other Communication Disorders of the National Institutes of Health. Appreciation is expressed to the 104 students and their parents who graciously gave their time and effort to participate in this study. Appreciation is expressed to speech language pathologists, audiologists and deaf educators who conducted testing at the follow sites: Arkansas Children’s Hospital, Central Institute for the Deaf-St. Louis, Child’s Voice-Chicago, Children’s Hospital of Philadelphia, Children’s Choice for Hearing and Talking-Sacramento, Hearts for Hearing, Listen and Talk-Seattle, Memphis Oral School for the Deaf, Moog Center for Deaf Education, St. Louis, Ohio Valley Voices, Presbyterian Ear Institute-Albuquerque, University of Miami, University of Minnesota Children’s Hospital, University of Texas at Dallas, Vanderbilt University Medical Center-Nashville, Weingarten Children’s Center-Redwood City.
This research was approved by the Human Studies Committee at Washington University School of Medicine (IRB#-201305136).
Footnotes
JL and DS report no relevant conflicts of interest related to this work. LSD is a member of the Knowledge Implementation in Pediatric Audiology (KIPA) group, Oticon.
References
- Archbold S, Sach T, O’neill C, Lutman M, & Gregory S (2008). Outcomes from cochlear implantation for child and family: parental perspectives. Deafness & Education International, 10(3), 120–142. doi:doi: 10.1002/dei.243 [DOI] [Google Scholar]
- Bradlow AR, Torretta GM, & Pisoni DB (1996). Intelligibility of normal speech I: Global and fine-grained acoustic-phonetic talker characteristics. Speech Communication, 20(3), 255–272. doi: 10.1016/S0167-6393(96)00063-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee M, Zion DJ, Deroche ML, Burianek BA, Limb CJ, Goren AP, … Christensen JA (2015). Voice emotion recognition by cochlear-implanted children and their normally-hearing peers. Hearing Research, 322, 151–162. doi: 10.1016/j.heares.2014.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chmiel R, Sutton L, & Jenkins H (2000). Quality of life in children with cochlear implants. Annals of Otology, Rhinology and Laryngology Supplement, 185, 103–105. [DOI] [PubMed] [Google Scholar]
- Cutting AL, & Dunn J (1999). Theory of Mind, Emotion Understanding, Language, and Family Background: Individual Differences and Interrelations. Child Development, 70(4), 853–865. doi: 10.1111/1467-8624.00061 [DOI] [PubMed] [Google Scholar]
- Dunn J, Brown JR, & Maguire M (1995). The development of children’s moral sensibility: Individual differences and emotion understanding. Developmental Psychology, 31(4), 649–659. doi: 10.1037/0012-1649.31.4.649 [DOI] [Google Scholar]
- Dunn J, Brown J, & Beardsall L (1991). Family talk about feeling states and children’s later understanding of others’ emotions. Developmental Psychology, 27(3), 448–455. doi: 10.1037/0012-1649.27.3.448 [DOI] [Google Scholar]
- Dunn LM, & Dunn DM (2007). Peabody Picture Vocabulary Test, Fourth Edition: PPVT-4. Bloomington, MN: NCS Pearson. [Google Scholar]
- Geers A, Davidson L, Uchanski R, & Nicholas J (2013). Interdependence of linguistic and indexical speech perception skills in school-aged children with early cochlear implantation. Ear and Hearing, 34(5), 562–574. doi: 10.1097/AUD.0b013e31828d2bd6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geers AE, Brenner CA, & Tobey EA (2011). Long-term outcomes of cochlear implantation in early childhood: Sample characteristics and data collection methods. Ear and Hearing, 32(1). doi: 10.1097/AUD.0b013e3181ffd5dc [DOI] [PubMed] [Google Scholar]
- Geers AE, & Nicholas JG (2013). Enduring advantages of early cochlear implantation for spoken language development. Journal of Speech, Language and Hearing Research, 56(2), 643–655. doi: 10.1044/1092-4388(2012/11-0347) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Good A, Gordon KA, Papsin BC, Nespoli G, Hopyan T, Peretz I, & Russo FA (2017). Benefits of music training for perception of emotional speech prosody in deaf children with cochlear implants. Ear and Hearing, 38(4), 455–464. doi: 10.1097/aud.0000000000000402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haukedal C, Torkildsen J, Lyxell B, & Wie O (2018). Parents’ Perception of Health-Related Quality of Life in Children With Cochlear Implants: The Impact of Language Skills and Hearing (Vol. 61). [DOI] [PubMed] [Google Scholar]
- Hoffman MF, Cejas I, & Quittner AL (2019). Health-Related Quality of Life Instruments for Children With Cochlear Implants: Development of Child and Parent-Proxy Measures. Ear and Hearing, 40(3), 592–604. doi: 10.1097/aud.0000000000000631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber M (2005). Health-related quality of life of Austrian children and adolescents with cochlear implants. International Journal of Pediatric Otorhinolaryngology, 69(8), 1089–1101. [DOI] [PubMed] [Google Scholar]
- Huttunen K, Rimmanen S, Vikman S, Virokannas N, Sorri M, Archbold S, & Lutman ME (2009). Parents’ views on the quality of life of their children 2–3 years after cochlear implantation. International Journal of Pediatric Otorhinolaryngology, 73(12), 1786–1794. doi: 10.1016/j.ijporl.2009.09.038 [DOI] [PubMed] [Google Scholar]
- Karl JR, & Pisoni DB (1994). Effects of stimulus variability on recall of spoken sentences: A first report. Retrieved from http://www.iu.edu/~srlweb/publications/progress-report-19/
- Kelsay DM, & Tyler RS (1996). Advantages and disadvantages expected and realized by pediatric cochlear implant recipients as reported by their parents. American Journal of Otology, 17(6), 866–873. [PubMed] [Google Scholar]
- Kirk KI, Pisoni DB, & Osberger MJ (1995). Lexical effects on spoken word recognition by pediatric cochlear implant users. Ear and Hearing, 16(5), 470–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR, & Niparko JK (2006). Measuring health-related quality of life after pediatric cochlear implantation: a systematic review. International Journal of Pediatric Otorhinolaryngology, 70(10), 1695–1706. doi: 10.1016/j.ijporl.2006.05.009 [DOI] [PubMed] [Google Scholar]
- Luo X, Kern A, & Pulling KR (2018). Vocal emotion recognition performance predicts the quality of life in adult cochlear implant users. The Journal of the Acoustical Society of America, 144(5), EL429–EL435. doi: 10.1121/1.5079575 [DOI] [PubMed] [Google Scholar]
- Loy B, Warner-Czyz AD, Tong L, Tobey EA, & Roland PS (2010). The children speak: an examination of the quality of life of pediatric cochlear implant users. Otolaryngology - Head and Neck Surgery, 142(2), 247–253. doi: 10.1016/j.otohns.2009.10.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meserole RL, Carson CM, Riley AW, Wang N-Y, Quittner AL, Eisenberg LS, … Niparko JK (2014). Assessment of health-related quality of life 6 years after childhood cochlear implantation. Quality of Life Research, 23(2), 719–731. doi: 10.1007/s11136-013-0509-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moog JS, Geers AE, Gustus CH, & Brenner CA (2011). Psychosocial adjustment in adolescents who have used cochlear implants since preschool. Ear and hearing, 32(1 Suppl), 75S–83S. doi: 10.1097/AUD.0b013e3182014c76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morettin M, dos Santos MJD, Stefanini MR, de Lourdes Antonio F, Bevilacqua MC, & Cardoso MRA (2013). Measures of quality of life in children with cochlear implant: systematic review. Brazilian Journal of Otorhinolaryngology, 79(3), 382–390. doi: 10.5935/1808-8694.20130066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morettin M, Santos M. J. D. d., Stefanini MR, Antonio F. d. L., Bevilacqua MC, & Cardoso MRA (2013). Avaliação da qualidade de vida em crianças com implante coclear: revisão sistemática. Brazilian Journal of Otorhinolaryngology, 79, 375–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakata T, Trehub SE, & Kanda Y (2012). Effect of cochlear implants on children’s perception and production of speech prosody. Journal of the Acoustical Society of America, 131(2), 1307–1314. doi: 10.1121/1.3672697 [DOI] [PubMed] [Google Scholar]
- Nicholas JG, & Geers AE (2003). Personal, social, and family adjustment in school-aged children with a cochlear implant. Ear and Hearing, 24(1 Suppl), 69S–81S. doi: 10.1097/01.AUD.0000051750.31186.7A [DOI] [PubMed] [Google Scholar]
- Niparko JK, Tobey EA, Thal DJ, Eisenberg LS, Wang NY, Quittner AL, & Fink NE (2010). Spoken language development in children following cochlear implantation. Journal of the American Medical Association, 303(15), 1498–1506. doi: 10.1001/jama.2010.451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nittrouer S, Muir M, Tietgens K, Moberly AC, & Lowenstein JH (2018). Development of Phonological, Lexical, and Syntactic Abilities in Children With Cochlear Implants Across the Elementary Grades. Journal of Speech, Language and Hearing Research, 61(10), 2561–2577. doi: 10.1044/2018_JSLHR-H-18-0047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roland L, Fischer C, Tran K, Rachakonda T, Kallogjeri D, & Lieu JE (2016). Quality of Life in Children with Hearing Impairment: Systematic Review and Meta-analysis. Otolaryngology - Head and Neck Surgery, 155(2), 208–219. doi: 10.1177/0194599816640485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sach TH, & Barton GR (2007). Interpreting parental proxy reports of (health-related) quality of life for children with unilateral cochlear implants. International Journal of Pediatric Otorhinolaryngology, 71(3), 435–445. doi: 10.1016/j.ijporl.2006.11.011 [DOI] [PubMed] [Google Scholar]
- Samuel V, Gamble C, Cullington H, Bathgate F, Bennett E, Coop N, … Edwards L (2016). Brief Assessment of Parental Perception (BAPP): Development and validation of a new measure for assessing paediatric outcomes after bilateral cochlear implantation. International Journal of Audiology, 55(11), 699–705. doi: 10.1080/14992027.2016.1204669 [DOI] [PubMed] [Google Scholar]
- Sarant JZ, Harris DC, Galvin KL, Bennet LA, Canagasabey M, & Busby PA (2018). Social Development in Children With Early Cochlear Implants: Normative Comparisons and Predictive Factors, Including Bilateral Implantation. Ear and Hearing, 39(4), 770–782. doi: 10.1097/aud.0000000000000533 [DOI] [PubMed] [Google Scholar]
- Schorr EA, Roth FP, & Fox NA (2009). Quality of life for children with cochlear implants: perceived benefits and problems and the perception of single words and emotional sounds. Journal of Speech, Language and Hearing Research, 52(1), 141–152. doi: 10.1044/1092-4388(2008/07-0213) [DOI] [PubMed] [Google Scholar]
- Semel EM, Wiig EH, & Secord W (2004). CELF-4 Screening: Clinical Evaluation of Language Fundamentals Screening Test - Fourth Edition: Pearson, PsychCorp. [Google Scholar]
- Sparreboom M, Snik AM, & Mylanus EM (2012). Sequential bilateral cochlear implantation in children: Quality of life. Archives of Otolaryngology-Head & Neck Surgery, 138(2), 134–141. doi: 10.1001/archoto.2011.229 [DOI] [PubMed] [Google Scholar]
- Stacey PC, Fortnum HM, Barton GR, & Summerfield AQ (2006). Hearing-impaired children in the United Kingdom, I: Auditory performance, communication skills, educational achievements, quality of life, and cochlear implantation. Ear and Hearing, 27(2), 161–186. doi: 10.1097/01.aud.0000202353.37567.b4 [DOI] [PubMed] [Google Scholar]
- Svirsky MA, Teoh SW, & Neuburger H (2004). Development of language and speech perception in congenitally, profoundly deaf children as a function of age at cochlear implantation. Audiology and Neurotology, 9(4), 224–233. doi: 10.1159/000078392 [DOI] [PubMed] [Google Scholar]
- Umansky AM, Jeffe DB, & Lieu JEC (2011). The HEAR-QL: Quality of Life Questionnaire for Children with Hearing Loss. Journal of the American Academy of Audiology, 22(10), 644–653. doi: 10.3766/jaaa.22.10.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Education, Office of Special Education and Rehabilitative Services, Office of Special Education Programs, 39th Annual Report to Congress on the Implementation of the Individuals with Disabilities Education Act, 2017, Washington, D.C. 2017. http://www.ed.gov/about/reports/annual/osep [Google Scholar]
- Warner-Czyz AD, Loy B, Roland PS, Tong L, & Tobey EA (2009). Parent versus child assessment of quality of life in children using cochlear implants. International Journal of Pediatric Otorhinolaryngology, 73(10), 1423–1429. doi: 10.1016/j.ijporl.2009.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner-Czyz AD, Loy B, Tobey EA, Nakonezny P, & Roland PS (2011). Health-related quality of life in children and adolescents who use cochlear implants. International Journal of Pediatric Otorhinolaryngology, 75(1), 95–105. doi: 10.1016/j.ijporl.2010.10.018 [DOI] [PubMed] [Google Scholar]
- WHO. (1995). The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine, 41(10), 1403–1409. [DOI] [PubMed] [Google Scholar]
- Wiefferink CH, Rieffe C, Ketelaar L, & Frijns JHM (2012). Predicting social functioning in children with a cochlear implant and in normal-hearing children: The role of emotion regulation. International Journal of Pediatric Otorhinolaryngology, 76(6), 883–889. doi: 10.1016/j.ijporl.2012.02.065 [DOI] [PubMed] [Google Scholar]