Abstract
Obesity is pandemic throughout the world, and there is concern that physicians are inadequately trained to treat their patients with obesity despite its prevalence. This review explores obesity education in medical students, resident, and fellow physicians throughout the world from 2005 to 2018. Previous reviews on obesity education were conducted before 2011, focused solely on medical students, and only explored obesity education in the United States. We systematically searched MEDLINE, EMBASE, PsycINFO, and ERIC databases for studies which included the search terms “obesity education” AND either “medical students”, “residency”, or “fellowship” that met PICOS (Population, Interventions, Comparators, Outcomes, Study Design) criteria for articles published in English for obesity education and evaluation of outcomes. Our initial search yielded 234 articles, and 27 studies met criteria for our review. We described and analyzed these studies for their study design and graded quality, quantity, and consistency for each measured outcome. We applied an evidence grading system that has been previously applied in the literature in which each outcome measure was graded on a scale from A to D. We evaluated obesity education programs for outcomes regarding implicit and explicit bias, changes in attitude towards obesity, weight change, obesity knowledge, counseling confidence, intent to counsel, and counseling quality. There was a significant degree of heterogeneity in the studies included. While obesity knowledge was most frequently studied, counseling confidence was the only outcome with an overall grade A. There is currently a paucity of obesity education programs for medical students, residents, and fellow physicians in training programs throughout the world despite high disease prevalence. However, these programs often improve outcomes when they are administered. Our review suggests that more obesity education should be administered in undergraduate and graduate medical education to ensure optimal treatment of patients with obesity.
Introduction
The prevalence of obesity remains high in both children and adults worldwide. Obesity affects 93.3 million adults >18 years of age in the USA, and 650 million adults worldwide [1]. Childhood obesity affects 24% of boys and 23% of girls in developed nations, while 13% of children (both boys and girls) in developing countries have obesity. There is evidence that patients with access to obesity care are more likely to attempt weight loss [2, 3]. Unfortunately, the majority of patients with obesity do not receive an obesity diagnosis and subsequent care [4]. There are several barriers thought to contribute to the under-recognition and undertreatment of obesity. Physicians’ negative attitudes towards patients with obesity and their view of themselves as not prepared to treat obesity are two such barriers [5]. There is evidence to suggest that these perceptions flourish in the absence of formal obesity education offered at all levels of training for medical students and physicians [6]. Obesity education can be distinguished from physical activity and nutrition education, which have also been studied as areas in which medical education is insufficient [7, 8]. Obesity education modules focus less on prevention and more on the mechanisms behind the chronic disease state and the complex care of patients with obesity. It is important to make this distinction since patients with obesity require a unique approach to treatment that incorporates components addressing societal stigma and the multitude of weight-related comorbidities (e.g., type 2 diabetes mellitus, hypertension, dyslipidemia, cardiovascular disease, non-alcoholic fatty liver disease, reproductive disorders, pulmonary dysfunction, psychiatric illnesses, some types of cancer) that must be addressed [9].
Numerous organizations have highlighted the need for standardized obesity care delivered by healthcare professionals trained in providing care to patients with obesity [6, 10, 11]. The US Preventive Services Task Force (USPSTF) recommends that patients with obesity receive intensive, multi-component behavioral interventions [10]. The American College of Physicians has developed guidelines to encourage physicians to provide counseling on weight loss, weight loss medication use, and bariatric surgery [11]. The Obesity Medicine Association (OMA) has developed continuing medical education modules to facilitate physicians to become board-certified in obesity medicine and to learn how to design an obesity treatment plan for an individual patients [12].
It has been suggested that physicians, particularly primary care providers (PCPs) play a vital role in steering patients towards obesity treatment by recognizing obesity in patients, and counseling patients on treatment options [13]. A systematic review found that physician weight loss counseling can have a significant impact on increasing patients’ weight reduction efforts [14]. Furthermore, a positive correlation between PCP-provided weight loss advice and actual weight loss of patients exists [14]. When queried, patients themselves have reported that they viewed physician-delivered advice on healthy eating and physical activity as useful [15]. It was also reported that patients saw less utility in a referral to a dietitian, highlighting the importance of general practice M.D.s and D.O. in counseling patients with obesity [15]. Because physicians have contact with patients at regular intervals, they are positioned to develop the long-term therapeutic relationship that is conducive to patients’ weight loss and weight loss maintenance.
Educational interventions focused on obesity diagnosis and treatment have demonstrated success in improving physicians’ and other healthcare providers’ attitudes and skills in caring for patients with obesity [16–19]. Obesity-focused education has been shown to improve physicians’ confidence level in their patients’ ability to lose weight [19]. Physicians who reported early exposure to obesity education were more likely to correctly answer bariatric surgery-related questions [20]. Obesity education has been shown to increase empathy of medical students towards patients with obesity, and increase their confidence in clinically interacting with such patients [21]. Conversely, medical educators can increase weight bias in their trainees if they model discriminatory behavior and express negativity concerning patients with obesity, highlighting the strong influence educators can exert over their trainees’ attitudes [22]. Unfortunately, only a small percentage of curricula in medical schools, residencies, and fellowship programs involve obesity-specific content.
There are few published articles from medical schools outlining a formal obesity curriculum. While we believe that preventive medicine curricula is important, we chose to focus our efforts on obesity-focused curricula that emphasizes a view of obesity as a chronic relapsing progressive disease and equips learners with practical tools to treat it [23]. The one previously published systematic review of obesity education in U.S. medical schools only covered the literature before 2011, did not explore curricula from countries outside of the U.S., and did not include healthcare providers other than medical students [24]. To understand the gaps in medical education with respect to obesity management, we searched the literature to find medical training programs that included obesity education, and analyzed their nature and qualities. We conducted a systematic review to identify the state of obesity education for medical students, residents, and fellows throughout the world.
Methods
Search strategy
Following the recommendations of the Center for Reviews and Dissemination for performing reviews in healthcare, we determined our inclusion criteria based off of the PICOS (Population, Interventions, Comparators, Outcomes, Study Design) format. Our search included medical student, resident physician, and fellow physician programs throughout the world. Studies were limited to those written in English. Studies were required to have at least one outcome measure that addressed future obesity counseling. Since this field of interest is recently evolving, our search was limited to studies published between 2005 and 2018. (Table 1).
Table 1.
Inclusion and exclusion criteria for systematic review of the literature
| Category | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Population | Medical school students of any year from any medical school in the world Resident and Fellow physicians in any training program in the world |
Qualified healthcare professional students of other healthcare professions (e.g., physician assistants, nurse practitioners, dietitians, nurses) |
| Interventions | Educational interventions that have components that address obesity education, including (but not restricted to): | Educational interventions that do not have a component that addresses obesity education |
| • Obesity knowledge | ||
| • Weight bias and stigma | ||
| • Counseling strategies for obesity | ||
| May be in any academic-sponsored program that is delivered in any academic, clinical, or community setting Use any kind of educational methodology | ||
| Instructed by any teacher including, but not restricted to: | ||
| • Physician | ||
| • Psychology | ||
| • Physician assistant | ||
| • Nurse practitioner | ||
| Comparators | Studies with or without control/comparison groups | |
| Outcome | Studies with at least one outcome measure that addresses future obesity counseling | |
| Study design (and study feature) | Any design (except studies without outcome measures) | |
| English language only | ||
| Published between 2005 and 2018 |
Authors systematically searched the MEDLINE, EMBASE, PsycINFO, and ERIC databases for relevant studies. Search terms included “obesity education AND medical students,” “obesity education AND residency,” and “obesity education AND fellowship”. A full list of inclusion search terms can be found in Fig. 1. Our search resulted in 234 articles. All articles were imported into the Covidence® software, which was used throughout the review process. Abstract titles were independently reviewed by two study investigators (MRM, FCS). Titles that did not meet our PICOS criteria were excluded. We compared independent results and discussed any conflicts to reach 95 initial studies of inclusion. In a final review, MRM, FCS, SR independently reviewed full-text articles to determine those that met full PICOS inclusion (N = 27). The remainder of the studies were excluded for lacking an intervention or measured outcome (N = 39) or for involving attending physicians rather than trainees (N = 22). Systematic reviews were also excluded (N = 7) (Fig. 2).
Fig. 1.
Inclusion search terms
Fig. 2.
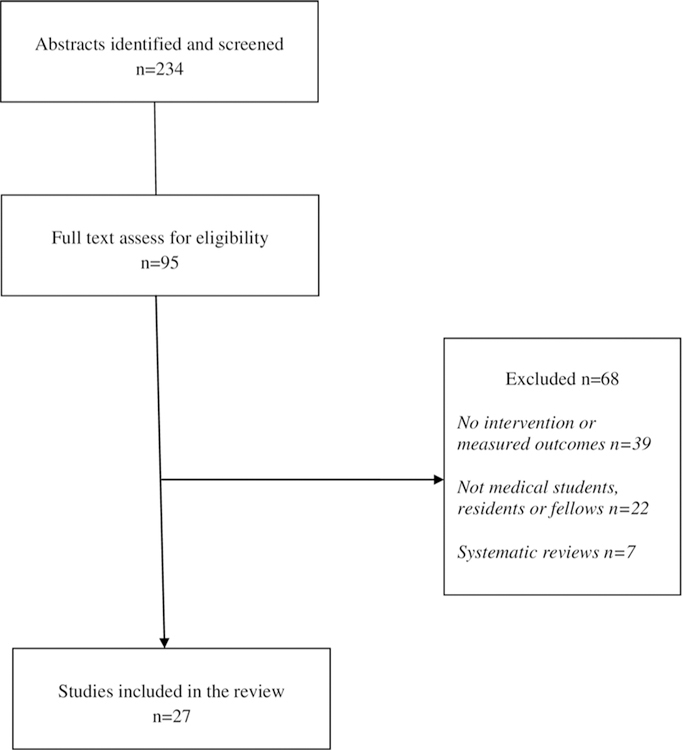
Study selection process for systematic review
Data synthesis
Data were extracted from each of the 27 studies, utilizing a tool developed by the researchers. We gathered features of each study including study site, design, aim, participants, intervention, outcomes, and results. We also extracted data regarding components of obesity education including bias attitudes, personal or patient weight change, obesity knowledge, and obesity counseling. All researchers mutually discussed and resolved any inconsistencies in data extracted.
Strength of study designs and measured outcomes
To evaluate the educational interventions of each study, we first assessed the design of each study (Table 2). A previously developed approach [25] was applied to evaluate interventional transparency and control for bias risk in each study. For a study to have interventional transparency, the intervention and evaluation methods must have been described in enough detail for future replication. Control of bias risk was determined if the study included baseline measurements and a control or comparison group. We then evaluated the strength of evidence for the measured outcomes in each of the studies. We first determined which outcomes were consistently measured throughout the studies. We then objectively graded the quality, quantity and consistency for each measured outcome. This was done using a grading system that has been applied previously [26].
Table 2.
Study design and quality of programs included in systematic review
| Intervention transparency |
Control for risk of bias |
||||
|---|---|---|---|---|---|
| Source | Study design | Program | Evaluation | Baseline measures | Comparison group |
| Acosta et al. | Pre- and post-survey Chart review | ✓ | ✓ | ✓ | |
| Brown et al. | Before and after | ✓ | ✓ | ✓ | ✓ |
| Burton et al. | Pre- and post-survey | ✓ | ✓ | ✓ | |
| Campbell et al. | Post survey only | ✓ | |||
| Chisholm et al. | Pre- and post-survey | ✓ | ✓ | ✓ | |
| Gayer et al. | Pre- and post-survey | ✓ | ✓ | ✓ | |
| Geller et al. | Pre- and post-survey | ✓ | ✓ | ✓ | |
| Gonzalez et al. | Pre- and post-survey | ✓ | ✓ | ✓ | ✓ |
| Huang et al. | Focus group | ✓ | |||
| Ip et al. | Pre- and post-survey | ✓ | ✓ | ✓ | ✓ |
| Iyer et al. | Pre- and post-survey | ✓ | ✓ | ✓ | |
| Jay et al. | Post survey | ✓ | ✓ | ✓ | |
| Jay et al. | Chart review | ✓ | ✓ | ||
| Kushner et al. | Pre- and post-survey | ✓ | ✓ | ✓ | |
| Laiteerapong et al. | Chart review | ✓ | ✓ | ✓ | |
| Matharu et al. | RCT | ✓ | ✓ | ✓ | ✓ |
| McAndrews et al. | Post survey only | ✓ | |||
| Ockene et al. | RCT | ✓ | ✓ | ✓ | ✓ |
| Perrin et al. | Pre- and post-survey | ✓ | ✓ | ✓ | |
| Poustchi et al. | Pre- and post-survey | ✓ | ✓ | ✓ | |
| Ren et al. | Chart review | ✓ | ✓ | ✓ | |
| Roberts et al. | Pre- and post-survey | ✓ | ✓ | ✓ | ✓ |
| Rodriguez et al. | Post survey only | ✓ | |||
| Schmidt et al. | Before and after | ✓ | ✓ | ✓ | |
| Stahl et al. | Pre- and post-survey | ✓ | ✓ | ✓ | ✓ |
| Swift et al. | RCT | ✓ | ✓ | ✓ | ✓ |
| Wislo et al. | Pre- and post-survey | ✓ | ✓ | ✓ | |
Two factors were evaluated to determine the quality of each primary outcome. The first was the utilization of objective assessments. An assessment was considered objective if it was quantifiable. These include, quantifiable survey data with features, such as self-report Likert scales and use of other evidence-based survey tools. Any observable outcome, such as knowledge base or behavior change required another tool, such as a checklist or skills test to be considered objective. Both results from focus groups and self-reports of any improvements in knowledge, skills or behavior were considered nonobjective. The second factor considered for quality of each outcome was use of a control or comparison group.
In order to grade the quality of evidence, we applied an evidence grading system that has been applied previously in the literature. Each outcome measure was graded on a scale from A to D. For quality of evidence to receive a grade A, there must have been one study utilizing a randomized control trial design and 75% of studies using objective assessment methods. To receive a grade B, there must have been at least one study using a control or comparison group (not required to be randomized) and at least 50% of studies with objective assessments. To meet criteria for grade C, there was at least one control or comparison group OR objective assessments. Lastly, for a grade D, neither of the grade C criteria were met.
Quantity of the studies was also evaluated on a grading scale. Quantity was determined by the number of studies investigating each measured outcome. Grade A was granted if at least four studies measured the outcome. Grade B was applied if there were three studies and grade C was conferred if there were two studies.
Lastly, consistency of results for each measured outcome was determined by the percent of studies that consistently reported results in the same direction. Studies results were deemed to be beneficial, harmful, or no change. Grade A was assigned if at least 75% of studies had an effect in the same direction. Grade B was applied if 51–74% results were in the same direction and grade C was granted at 25–50%.
Taking all of the grades into consideration, each measured outcome received an overall grade. The overall rating is the lowest grade for quality, quantity and consistency (Table 3).
Table 3.
Evidence of effectiveness for measured outcomes
| Measured outcomes | Overall evidence rating | Quality | Quantity | Consistency |
|---|---|---|---|---|
| Implicit bias | B | A | B | B |
| Explicit bias | C | A | C | A |
| Change in attitude toward obesity | B | B | A | A |
| Weight change | B | B | A | A |
| Obesity knowledge | B | B | A | A |
| Counseling confidence | A | A | A | A |
| Intent to counsel | B | B | A | A |
| Counseling quality | B | B | B | A |
Quality: grade A = at least one study utilizing a randomized control trial design and 75% of studies using objective assessment methods; grade B = at least one study using a control or comparison group) and at least 50% of studies with objective assessments. Grade C = at least one control or comparison group OR objective assessments. Grade D, neither of the grade C criteria were met
Quantity: grade A = at least four studies measured the outcome; grade B = three studies measure the outcome; grade C = two studies measured the outcome
Consistency: grade A = at least 75% of studies reported results in the same direction (beneficial, harmful, or no change); grade B = 51–74% results in the same direction; grade C = 25–50% results in the same direction.
The overall rating is the lowest grade for quality, quantity and consistency
Results
Twenty-seven educational programs with specific interventions and outcomes regarding obesity education were identified. Characteristics of each of these 27 programs are provided in Supplemental Table 1.
Curriculum design
Participants and timing
Of the 27 programs, 24 (89%) were piloted in the United States. The three remaining programs were performed in Manchester, United Kingdom [27], Nottingham, United Kingdom [28] and Edmonton, Alberta, Canada [29]. While Chisholm and Swift studied medical student education, Campbell et al. discussed a new obesity curriculum in internal medicine residents.
Twelve programs (44%) involved resident education and 1 program educated fellows and residents [30]. Resident education targeted internal medicine, pediatric, or family medicine programs. Burton et al. studied a curriculum piloted to internal medicine and pediatric residents simultaneously [31] and Huang et al. tested a new curriculum for both pediatric and preventive medicine residents [32].
The remaining programs (56%) focused on medical student education. Medical student programs varied in which year of. The majority of studies targeted third year medical students in their clinical years (33%). Four programs occurred during first year of medical school. The remainder of programs were for medical students in multiple years of study. There were no studies that targeted second year or fourth year students only.
Study design
The majority of studies (59%) used pre and post surveys as their primary study design. There were only three randomized control trials [28, 33, 34]. Two of these studies examined implicit and explicit bias in medical students [28, 33], while the other examined obesity counseling confidence in medical students during an objective structured clinical examination (OSCE) [34]. Four studies involved a chart review [19, 35–37]. All four of these programs studied resident education. Chart review examined the rates of obesity documentation [19, 37] and body mass index (BMI) documentation [35, 36] before and after intervention. Two studies tracked participant weight loss pre- and post-intervention in a before and after design [38, 39]. Brown et al. studied patient weight loss [38] while Schmidt et al. tracked student weight loss [39]. In both studies, participants lost or maintained their weight. Three studies utilized standardized patient encounters with two of these studies involving residents [30, 40] and one involving medical students [41].
Interventions
Fifteen studies used lecture-based format as their educational intervention. Of those studies, eight used additional educational interventions. In both 2010 and 2013, Jay et al. [35] studied the combination of lectures, resident role-playing and standardized patient encounters. Standardized patients and real patient encounters combined with lecture were utilized by Campbell et al. [29] as well. Lectures were also coupled with creation of patient education material [36, 38] personal weight loss tracking [39] and case-study readings [42]. Gonzalez et al. developed a curriculum that began with a lecture and continued with assigned readings, observational sessions with pediatric nutritionists, and culminated with resident patient encounters with pediatric patients with obesity [43]. Other studies utilized standardized patients in their interventions [41] along with readings about obesity [21]. Three studies developed a web-based training [32, 34, 44]. The web-based curriculum utilized by Ockene et al. was coupled with role playing, a Web Patient encounter, and enhancement of internal medicine and family medicine clerkship obesity curriculum [34]. Other interventions included obesity educational videos [28, 45], a bariatric surgery elective course [46], ethics sessions [47], and patient counseling [38, 48, 49]. Interventions ranged from 3 h [31] to 3 years [42] in length.
Outcomes
Throughout the examined studies, eight main outcomes were measured: change in attitude about obesity, implicit bias, explicit bias, weight change, obesity knowledge, counseling confidence, counseling quality, and intent to counsel about obesity.
Thirty-two percent of studies reported an increase in medical knowledge about obesity, while another 15% reported a change in attitude about obesity after intervention. Multiple studies examined obesity counseling in both medical students and residents. Of those studies, 26% examined confidence in discussing obesity with patients, 22% reported a change in intent to counsel patients about obesity and 11% assessed counseling quality after interention. Other outcomes included change in implicit (11%) and explicit (7%) bias and an increase in participant weight loss (15%). Two studies studied implicit and explicit bias simultaneously [28, 33].
The majority of studies (81%) reported positive findings from their educational interventions. One study is still in process and does not have results [34]. The remaining five studies found no change or negative change after intervention. Geller et al. reported 53% of students did not change their attitudes towards obesity 4 months after an ethics session and 10% had more negative attitudes [47]. Kushner et al. stated that at 1-year post intervention, negative obesity stereotyping had regressed to baseline levels and the modest decrease in stereotyping at the immediate follow-up survey had disappeared [21]. Ren et al. reported their intervention had no effect on obesity documentation or counseling [37], while Jay et al. found that residents who received an obesity counseling curriculum were not more likely to counsel patients with obesity than residents who did not [35]. One study, showed that even after an improvement to explicit bias towards patients with obesity, there was still no improvement in anti-fat bias amongst the participants [28].
Strength of study designs
All study designs are listed in Table 2. There were only three studies in which participants were randomized to intervention or control. Twenty of the studies (74%) provided interventional transparency in that they described both the curriculum and evaluation procedures well enough to be replicated. In contrast, control for bias was lacking. Only 10 studies (37%) provided baseline measures or a comparison group. There were only eight studies that met all criteria for interventional transparency and control for risk of bias. Three of these studies used a randomized control trial design, increasing their relative strength [28, 33, 34]. Six studies did not utilize objective outcomes. [27, 32, 35, 47–49]. These studies employed self-reported outcomes or subjective feedback from medical students, residents, or patients.
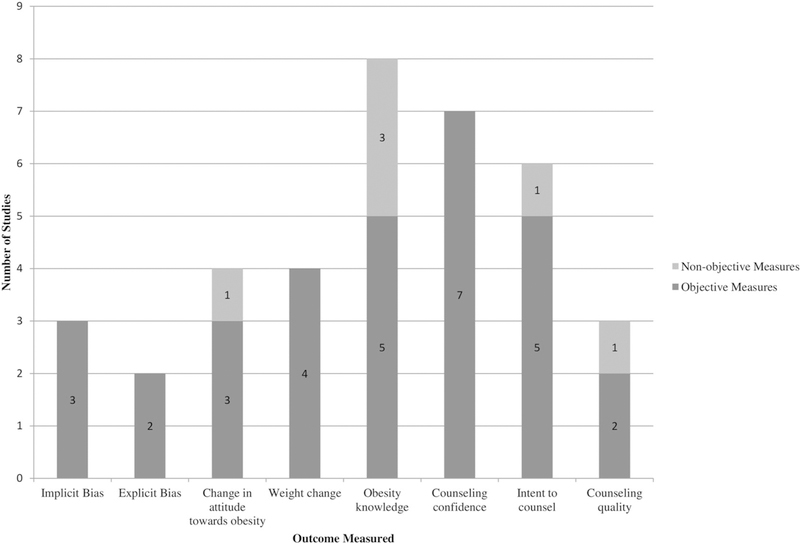
Strength of measured outcomes
There were eight measured outcomes that we found most often evaluated (Fig. 3 and Table 3). These outcomes are change in attitude about obesity, implicit bias, explicit bias, weight change, obesity knowledge, counseling confidence, counseling quality, and intent to counsel about obesity.
Fig. 3.
Number of programs using objective vs nonobjective measures
Change in attitude about obesity was studied in four papers and received an overall B rating [15, 19, 39, 41]. Of the four studies examining this outcome, only one had a comparison group [41] but all four used baseline measurements and objective outcomes. Three studies showed positive outcomes related to attitude about obesity after intervention [15, 19, 41], while one showed no change [21].
Implicit bias received an overall B rating and was examined in three studies [21, 26, 35]. Two of the studies examining implicit bias were randomized control trials [28, 33] and one utilized a comparison group [42]. All three of these studies had objective outcomes. Gayer et al. showed a positive change in implicit bias after intervention while the other two studies did not show a change [28, 33, 42].
Explicit bias was given a grade C. Only two studies examined explicit bias and both were randomized control trial design [28, 33]. These studies researched the effect of the intervention on implicit and explicit bias concomitantly. Both studies showed a positive change in explicit bias after intervention.
Weight change was examined in four studies and earned an overall B rating [14, 29, 32, 33]. Only two of these studies used a control or comparison group [35, 38]. However, all four used objective outcome measurements. In addition, all four consistently showed positive results post intervention.
Obesity knowledge was most frequently studied. It received a B rating overall. Three of these studies had a strong control of bias using baseline measures and comparison groups [42, 43, 46]. Three studies did not utilize objective outcomes measurements [32, 48, 49]. All eight studies had positive results [22, 25, 35, 36, 40, 42–44].
Counseling confidence was the only outcome with an overall grade A. One study examining this outcome was a randomized controlled trial [34], while another had both baseline measurements and comparison groups [30]. All of the studies utilized objective outcomes. All studies [14, 22, 23, 34, 37, 44] but the one conducted by Ockene and colleagues [27], which does not have result yet, reported a positive change in counseling confidence among participants.
Counseling quality received an overall grade C. Two studies examining this outcome used objective outcomes [44, 50], while the other used patient interviews and thus, did not [35]. Two studies had comparison groups [35, 44], while two had baseline measures [44, 50]. All three had positive results [35, 44, 50].
Intent to counsel was examined in six of the studies and was given an overall grade B. Only one of the studies did not use comparison or control groups or have baseline measurements [35]. Five of the studies had objective outcomes [27, 36, 37, 40, 46], while one did not [35]. Five studies showed positive results [27, 35, 36, 40, 46], and one reported no change in intent to counsel after intervention [37].
Discussion
We performed a systematic review on obesity education of medical trainees which featured 27 studies of medical student, resident physician, and fellow physician programs published between 2005 and 2018 throughout the world. The studies featured obesity curricula in three countries with at least one outcome measure that addressed medical trainees’ knowledge or skills in treating obesity. Our analysis of these studies showed heterogeneity, with variations on how curricula were structured and delivered (Supplemental Table 1). Our findings agree with the literature showing that behavioral change coursework addressing specific health issues (i.e., obesity) for medical students is not standardized in terms of educational content or how much time is spent delivering the lessons [25, 51]. Study interventions and outcomes were not always described to the extent that would be needed to replicate and assess efficacy of the educational program.
Most educational interventions we studied (22/27, 81%) reported positive findings. The exposure time to the educational interventions varied widely, from 34 min in a single session as performed by Swift et al. to an unspecified number of hours broken into multiple sessions over a period of 10 weeks [52]. Many authors did not explicitly state how many total hours their educational intervention involved. Similar to the findings of Vitolin et al. [24], the studies we reviewed did not include any interventions that spanned the full 4 years of medical school, although one study had educational components integrated into the 1st, 2nd, and 3rd year of medical school [42] and found that the positive effects in medical students lasted through the 4th year of medical school. There were only two studies that measured outcomes 1 year after the end of the intervention [21, 42]. An important consideration for future educational interventions is to test the longevity of the outcomes in medical trainees post intervention.
The studies we reviewed demonstrated a range of methodological rigor and heterogeneity in program content, duration, and frequency of exposure of the medical trainees to the obesity-related content. Only 3 of the 27 programs reviewed were randomized controlled trials [33, 52] with one [34] not reporting results. A previous review of obesity education in medical schools found that only one study addressed the bias of medical students against patients with obesity [24]. We reviewed three studies with this focus [33, 42, 52], two of which demonstrated that students showed increased empathy and decreased bias towards patients with obesity [33, 42]. The outcomes investigated were bias against people with obesity and counseling confidence, with one showing no effect on implicit anti-fat bias [52] and the other decreased explicit anti-fat bias [33]. Although the types of bias compared are different, the students who engaged interactively with obesity-related storytelling in the form of a play [33] showed a change in bias compared with the patients who attended a lecture [33] or watched a film [52].
These findings echo an intervention carried out with medical students by Wiese et al. [53], who designed an curriculum for medical students featuring active engagement with obesity-related material which successfully decreased explicit bias against patients with obesity [53]. The efficacy of active learning vs passive learning is further supported by our findings that the didactic and reading-based interventions were less effective [21, 37, 52]; however, one lecture-based intervention given to residents increased their confidence in counseling patients with obesity [19], which could be attributed to the increased length of lecture content hours or the multidisciplinary group of lecturers. The majority of our studies featured a quasi-experimental design, with 57% of the studies featuring a pre- and post-survey or a before-and-after. Such studies make it difficult to determine which components of the educational interventions, if any, caused the changes observed in outcomes. Only 10/28 (36%) of the studies we evaluated controlled for risk of bias, which makes it unclear whether other factors at work during the intervention influenced the findings of the studies.
Some major medical organizations have recently moved to promote obesity education for medical students, demonstrating the relevance of our review to influence medical education. In 2016, the Obesity Medicine Education Collaboration, or OMEC (a collaboration between educators from the Obesity Society (TOS), the OMA), and the American Society for Metabolic and Bariatric Surgery formed with the purpose of developing core competencies and professional activities for undergraduate medical schools and residency programs [54]. The medical education competencies created by OMEC cover domains such as: (1) patient care and procedural skills, (2) medical knowledge, (3) practice-based learning and improvement, (4) interpersonal and communication skills, professionalism, and (5) systems-based practice related to obesity. Some of the studies in our review incorporate these competencies, including students demonstrating knowledge of etiology, mechanisms, and biology of obesity [27, 32, 42, 43, 45, 46, 48, 49], educating patients and health professionals on the disease of obesity [39], and communicating in a nonbiased, nonjudgmental, respectful, and empathetic manner with patients with obesity [33, 35, 41, 42, 44, 47, 50]. In 2017, the American Medical Association, the largest physician advocacy organization in the United States, co-authored a resolution with the OMA to “promote the inclusion of education on obesity prevention and the medical complications of obesity in medical school and appropriate residency curricula” [55]. The findings of our review provide evidence to support the competencies delineated above.
Unfortunately, the state of obesity education in the world is inadequate. There are a modest number of educational efforts to teach obesity to medical students and trainees throughout the world. In addition, many of these programs are of short duration, and there is a concern that this does not allow this limited education to translate to the clinical practice of physicians as they care for a growing population with obesity. There should be more vigor in the breadth and depth of education provided to medical students, residents, and fellows to align with the education of other important chronic disease processes, such as diabetes mellitus and heart disease. These disease processes receive adequate time and attention in the medical curricula while obesity is grossly neglected.
We recommend that obesity-related curricula for medical trainees incorporate elements from the studies with outcomes that were strongly supported by the grading criteria, such as patient counseling skills, changing physicians’ attitudes towards patients with obesity, increasing physicians’ intent to counsel, and increasing general knowledge about obesity. We also recommend the use of tools suitable to assess not only subjective changes like attitude and confidence of the medical trainee, but also measurable skills such as empathy-related behaviors and key questions to consider when counseling patients with obesity. Tools such as surveys were used in 18/28 (64%) of the studies we reviewed. It was unclear from the descriptions of the interventions whether checklists and logs to record objective behaviors were used. Clinical outcomes (e.g., weight change) were only measured in four interventions [19, 38, 39, 50], with one of the interventions [39] evaluating the weight change of medical trainees. Most of the outcomes we graded focused on proximal outcomes (e.g., trainees’ knowledge of obesity, attitudes towards patients with obesity, intent to counsel, counseling confidence), which ultimately might impact patient outcomes since healthcare professionals who have more positive attitudes towards the patients potentially provide better care to them [56]. It would, however, be prudent for interventions to not only assess physician knowledge and skills, but to measure patient-centered outcomes, such as patient satisfaction, patients’ behavioral change, and changes in patients’ weight. Using such information, we could make better predictions about how obesity education interventions for trainees could impact patients’ health.
The strengths and weaknesses of our review give context to the findings. Our search criteria for inclusion and exclusion were in line with PICOS criteria, which makes our extraction for the review [7]. A limitation to this review includes the fact that the studies were heterogeneous in nature, with various outcomes evaluated, using a variety of study designs. Similar to a previous review of obesity counseling education geared toward medical students which did not include any interventions that compare multiple teaching modalities (e.g., didactic vs interactive, short and intensive vs long and split into sessions) within the same intervention [27], we only reviewed one study that compared teaching methods [33]. Therefore, the advantages and disadvantages of one teaching approach vs another remain unclear. Furthermore, because our study team did the coding for the review, there is the possibility of coder bias. We had two coders doing independent evaluations of each study to minimize this factor. In addition, the criteria used to grade strength of evidence was replicated from a review addressing physical activity counseling [7], which was based on criteria used to evaluate clinical interventions. The grading system therefore could be less suitable for grading strength of obesity-specific health outcomes (e.g., implicit bias, explicit bias, change in attitude toward obesity, weight change). Because we only included English-language articles and published studies, the studies we reviewed could have outcomes that are biased toward favorable results. Finally, there could also be obesity-related curricula in use at medical schools and residency and fellowship programs not been formally published, which are not included in our analysis.
Our findings support the inclusion of obesity-focused curricula in the education of medical trainees. Our recommendations for curriculum development based on previous literature, our own results, and recommendations by groups of organized physicians are to (a) incorporate both short, intensive educational sessions, and training over a longer period of time broken up into multiple sessions into medical education programs, (b) utilize an interactive learning format, with graded standardized patient encounters, interaction with patients with obesity, and group discussions, and (c) provide meticulous descriptions of the curricula and evaluation procedures of obesity-related educational interventions so that they may be scrutinized and replicated, perhaps with the creation and validation of a rubric as a standardized metric to evaluate educational programs on their efficacy in addressing knowledge and skill gaps related to obesity. Since many of these studies had multiple components to the intervention, further research needs to be done on obesity curricula to determine which individual components are most beneficial in developing the competence of medical trainees’ in treating patients with obesity. Based on our review, increasing obesity-related educational content at all levels of medical education will equip students with the tools and the confidence to effectively and compassionately treat patients with obesity.
Supplementary Material
Acknowledgments
Funding National Institutes of Health NIDDK P30 DK040561 and L30 DK118710.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Ethical approval This research was considered IRB exempt.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information The online version of this article (https://doi.org/10.1038/s41366-019-0453-6) contains supplementary material, which is available to authorized users.
References
- 1.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015–2016.: Hyattsville, MD, 2017. NCHS Data Brief. [PubMed] [Google Scholar]
- 2.Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282:1576–8. [DOI] [PubMed] [Google Scholar]
- 3.Jackson SE, Wardle J, Johnson F, Finer N, Beeken RJ. The impact of a health professional recommendation on weight loss attempts in overweight and obese British adults: a cross-sectional analysis. BMJ Open. 2013;3:e003693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thapa R, Friderici J, Kleppel R, Fitzgerald J, Rothberg MB. Do physicians underrecognize obesity? South Med J. 2014;107:356–60. [DOI] [PubMed] [Google Scholar]
- 5.Sebiany AM. Primary care physicians’ knowledge and perceived barriers in the management of overweight and obesity. J Fam Community Med. 2013;20:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goff SL, Holmboe ES, Curry L. Barriers to obesity training for pediatric residents: a qualitative exploration of residency director perspectives. Teach Learn Med. 2006;18:348–55. [DOI] [PubMed] [Google Scholar]
- 7.Dacey ML, Kennedy MA, Polak R, Phillips EM. Physical activity counseling in medical school education: a systematic review. Med Educ Online. 2014;19:24325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dang TM, Maggio LA. Supporting the call to action: a review of nutrition educational interventions in the health professions literature and MedEdPORTAL. Acad Med. 2017;92:403–16. [DOI] [PubMed] [Google Scholar]
- 9.Kyrou IRH, Tsigos C, et al. Endotext, MDText.com: South Dartmouth (MA), 2010. [Google Scholar]
- 10.Force USPST. Behavioral weight loss interventions to prevent obesity-related morbidity and mortality in adults: Us preventive services task force recommendation statement. JAMA. 2018;320:1163–71. [DOI] [PubMed] [Google Scholar]
- 11.Snow V, Barry P, Fitterman N, Qaseem A, Weiss K. for the Clinical Efficacy Assessment Subcommittee of the American College of P et al. Pharmacologic and Surgical Management of Obesity in Primary Care: A Clinical Practice Guideline from the American College of Physicians. Ann Inter Med. 2005;142:525–31. [DOI] [PubMed] [Google Scholar]
- 12.O.M.A. Obesity Medicine Academy. In: ObesityMedicine Association: CME, 2018. [Google Scholar]
- 13.Rutledge T, Groesz LM, Linke SE, Woods G, Herbst KL. Behavioural weight management for the primary careprovider. Obes Rev. 2011;12:e290–e297. [DOI] [PubMed] [Google Scholar]
- 14.Rose SA, Poynter PS, Anderson JW, Noar SM, Conigliaro J. Physician weight loss advice and patient weight loss behavior change: a literature review and meta-analysis of survey data. Int J O. 2005;37:118–28. 2013 [DOI] [PubMed] [Google Scholar]
- 15.Tan D, Zwar NA, Dennis SM, Vagholkar S. Weight management in general practice: what do patients want? Med J Aust. 2006;185:73–75. [DOI] [PubMed] [Google Scholar]
- 16.Sanchez-Ramirez DC, Long H, Mowat S, Hein C. Obesity education for front-line healthcare providers. BMC Med Educ. 2018;18:278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iwamoto S, Saxon D, Tsai A, Leister E, Speer R, Heyn H, et al. Effects of education and experience on primary care providers’ perspectives of obesity treatments during a pragmatic trial: PCPs’ perspectives on obesity treatments changed. Obesity. 2018;26:1532–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davila N, Vess J, Johnson EE. Identification and management of obese patients in a pediatric orthopaedic clinic. Orthop Nurs. 2017;36:194–200. [DOI] [PubMed] [Google Scholar]
- 19.Acosta A, Azzalin A, Emmons CJ, Shuster JJ, Jay M, Lo MC. Improving residents’ clinical approach to obesity: impact of a multidisciplinary didactic curriculum. Postgrad Med J. 2014;90:630–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stanford FC, Johnson ED, Claridy MD, Earle RL, Kaplan LM. The role of obesity training in medical school and residency on bariatric surgery knowledge in primary care physicians. Int J Fam Med. 2015;2015:841249–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kushner RF, Zeiss DM, Feinglass JM, Yelen M. An obesity educational intervention for medical students addressing weight bias and communication skills using standardized patients. BMC Med Educ. 2014;14:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Phelan SM, Puhl RM, Burke SE, Hardeman R, Dovidio JF, Nelson DB, et al. The mixed impact of medical school on medical students’ implicit and explicit weight bias. Med Educ. 2015;49:983–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bray GA, Kim KK, Wilding JPH, on behalf of the World Obesity F. Obesity: a chronic relapsing progressive disease process. a position statement of the world obesity federation: position paper. Obes Rev. 2017;18:715–23. [DOI] [PubMed] [Google Scholar]
- 24.Vitolins MZ, Crandall S, Miller D, Ip E, Marion G, Spangler JG. Obesity educational interventions in U.S. Medical Schools: a systematic review and identified gaps. Teach Learn Med. 2012;24:267–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chisholm A, Hart J, Mann KV, Harkness E, Peters S. Preparing medical students to facilitate lifestyle changes with obese patients: a systematic review of the literature. Acad Med. 2012;87:912–23. [DOI] [PubMed] [Google Scholar]
- 26.Beach MC, Price EG, Gary TL, Robinson KA, Gozu A, Palacio A, et al. Cultural competence: a systematic review of health care provider educational interventions. Med Care. 2005;43:356–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chisholm A, Hart J, Mann K, Perry M, Duthie H, Rezvani L, et al. Investigating the feasibility and acceptability of health psychology-informed obesity training for medical students. Psychol Health Med. 2016;21:368–76. [DOI] [PubMed] [Google Scholar]
- 28.Swift JA, Tischler V, Markham S, Gunning I, Glazebrook C, Beer C, et al. Are anti-stigma films a useful strategy for reducing weight bias among trainee healthcare professionals? Results of a pilot randomized control trial. Obes Facts. 2013;6:91–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Campbell-Scherer DL, Luig T, Wicklum S, Klein D, Lafrance R, Heatherington M et al. Improving Obesity Management Education and Training for Medical Residents. Can J Diabetes 2017; 41:S22. [Google Scholar]
- 30.Wislo VMP, McGaffey A, Scopaz KA, D’Amico FJ, Jewell IK, Bridges MW, et al. Fitwits. Clinical Pediatrics. 2013;52:1107–17. [DOI] [PubMed] [Google Scholar]
- 31.M. Burton A, Cherrington A, Agne A, Lehr S, Brezausek C. Implementing an obesity counseling curriculum in residency training, 2010;387.
- 32.Huang J, Pokala P, Hill L, Boutelle KN, Wood C, Becerra K, et al. The Health and Obesity: Prevention and Education (HOPE) Curriculum Project-Curriculum Development. Pediatrics. 2009;124:1438–46. [DOI] [PubMed] [Google Scholar]
- 33.Matharu K, Shapiro J, Hammer R, Kravitz RL, Wilson M, Fitzgerald F. Reducing obesity prejudice in medical education. Educ Health 2014; 27:231–37. [DOI] [PubMed] [Google Scholar]
- 34.Ockene JK, Ashe KM, Hayes RB, Churchill LC, Crawford SL, Geller AC, et al. Design and rationale of the medical students learning weight management counseling skills (MSWeight) group randomized controlled trial. Contemp Clin Trials. 2018;64:58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jay MR, Gillespie CC, Schlair SL, Savarimuthu SM, Sherman SE, Zabar SR, et al. The impact of primary care resident physician training on patient weight loss at 12 months. Obesity. 2013;21:45–50. [DOI] [PubMed] [Google Scholar]
- 36.Laiteerapong N, Keh CE, Naylor KB, Yang VL, Vinci LM, Oyler JL, et al. A resident-led quality improvement initiative to improve obesity screening. Am J Med Qual. 2011;26:315–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ren V, Ellison K, Miller J, Busireddy K, Vickery E, Panda M, et al. Effect of didactic lectures on obesity documentation and counseling among internal medicine residents. J Community Hosp Intern Med Perspect. 2016;6:30931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brown J, Lydecker JA, Turner T, Knackstedt RW, O’Neil PM. A novel approach to training students in delivering evidence-based obesity treatment. Fam Med. 2015;47:378–82. [PubMed] [Google Scholar]
- 39.Schmidt S, Rice A, Kolasa K. Teaching by example: educating medical students through a weight management experience. Fam Med. 2013;45:572–5. [PubMed] [Google Scholar]
- 40.Burton AM, Brezausek CM, Agne AA, Hankins SL, Willett LL, Cherrington AL. Evaluation of a workshop to improve residents’ patient-centred obesity counselling skills. Postgrad Med J. 2016;92:455–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ip EH, Marshall S, Vitolins M, Crandall SJ, Davis S, Miller D, et al. Measuring medical student attitudes and beliefs regarding patients who are obese. Acad Med. 2013;88:282–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gayer GG, Weiss J, Clearfield M. Fundamentals for an Osteopathic Obesity Designed Study: The Effects of Education on Osteopathic Medical Students’ Attitudes Regarding Obesity. J Am Osteopath Assoc. 2017;117:495–502. [DOI] [PubMed] [Google Scholar]
- 43.Gonzalez JL, Gilmer L. Obesity prevention in pediatrics: A pilot pediatric resident curriculum intervention on nutrition and obesity education and counseling. J Natl Med Assoc. 2006;98:1483–8. [PMC free article] [PubMed] [Google Scholar]
- 44.Stahl CE, Necheles JW, Mayefsky JH, Wright LK, Rankin KM. 5-4-3-2-1 go! Coordinating pediatric resident education and community health promotion to address the obesity epidemic in children and youth. Clin Pediatr. 2011;50:215–24. [DOI] [PubMed] [Google Scholar]
- 45.Poustchi Y, Saks NS, Piasecki AK, Hahn KA, Ferrante JM. Brief intervention effective in reducing weight bias in medical students. Fam Med. 2013;45:345–8. [PMC free article] [PubMed] [Google Scholar]
- 46.Roberts DH, Kane EM, Jones DB, Almeida JM, Bell SK, Weinstein AR, et al. Teaching medical students about obesity: a pilot program to address an unmet need through longitudinal relationships with bariatric surgery patients. Surg Innov. 2011;18:176–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Geller G, Watkins PA. Addressing medical students’ negative bias toward patients with obesity through ethics education. AMA J Ethics. 2018;20:E948–959. [DOI] [PubMed] [Google Scholar]
- 48.McAndrew S, Jackman C, Sisto PP. Medical student-developed obesity education program uses modified team-based learning to motivate adolescents. Med Teach. 2012;34:414–6. [DOI] [PubMed] [Google Scholar]
- 49.Rodriguez JE, Painter K. ‘Health Not Cosmetics’: a medical student obesity treatment project. Med Educ. 2006;40:1133–4. [DOI] [PubMed] [Google Scholar]
- 50.Iyer S, Jay M, Southern W, Schlair S. Assessing and counseling the obese patient: improving resident obesity counseling competence. Obes Res Clin Pract. 2018;12:242–5. [DOI] [PubMed] [Google Scholar]
- 51.Bell K, Cole BA. Improving medical students’ success in promoting health behavior change: a curriculum evaluation. J Gen Intern Med. 2008;23:1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Swift JA, Hanlon S, El-Redy L, Puhl RM, Glazebrook C. Weight bias among UK trainee dietitians, doctors, nurses and nutritionists. J Hum Nutr Diet. 2013;26:395–402. [DOI] [PubMed] [Google Scholar]
- 53.Wiese HJ, Wilson JF, Jones RA, Neises M. Obesity stigma reduction in medical students. Int J Obes Relat Metab disord. 1992;16:859. [PubMed] [Google Scholar]
- 54.Association OM. Obesity Medicine Education Collaborative Competencies. In, 2019.
- 55.Recognizing and Taking Action in Response to the Obesity Crisis D-440.980. American Medical Association Annual Meeting; Chicago, Illinois, 2017. [Google Scholar]
- 56.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.