Abstract
Purpose:
Seizures have a variety of significant physical, cognitive, and social effects upon the individual. Depression has been linked to an increase in seizure activity and Project UPLIFT was shown to reduce depressive symptoms. Project UPLIFT, based upon Mindfulness-Based Cognitive Therapy (MBCT), provides distance delivery of depression management skills to groups of people with epilepsy. Because Project UPLIFT reduces depression and depression is linked to seizure activity, the current analysis was designed to determine the impact of Project UPLIFT upon seizure frequency and severity.
Method:
Participants (n = 107) were adults ages 21-70 with epilepsy and mild-to-moderate depressive symptoms from the states of Georgia, Michigan, Texas, and Washington. The eight-session Project UPLIFT intervention was group-delivered weekly via the Web or telephone. Participants were randomly assigned to condition (i.e., Project UPLIFT or a treatment-as-usual [TAU] waitlist) and assessed at baseline, and after intervening in the Project UPLIFT group (~10 weeks). Assessments included valid self-report measures of seizure frequency and severity and depression.
Results:
Mediation analysis found that there was a significant negative direct relationship between condition and number of seizures at posttest; the mean number of seizures decreased by 3.2 in the Project UPLIFT group, but increased by 2.3 in the TAU group. The indirect path from condition to number of seizures through change in depression was not significant. Conversely, there was no significant negative direct relationship between condition and seizure severity at posttest, although the seizure severity decreased by 2.2 points in the UPLIFT group and increased by 2.7 points in the TAU group. The indirect path from condition to seizure severity through depression was significant, however, demonstrating that change in depression mediated the effect of Project UPLIFT on seizure severity.
Conclusions:
This study found that participating in Project UPLIFT directly reduced the number of seizures experienced by participants with epilepsy. This was not mediated by the change in depression. Participation in Project UPLIFT also reduced their perceived seizure severity indirectly, through reducing their depressive symptoms. This suggests Project UPLIFT may have the potential to impact the health, health care costs, and well-being of people with epilepsy.
Keywords: epilepsy, seizures, depression, cognitive behavioral therapy, mindfulness
Introduction
Seizures, a period of abnormal firing of a population of neurons, have varied symptoms including loss of awareness, confusion, body shaking, and visual or other sensory symptoms [1, 2] Seizures have a variety of significant physical, cognitive, and social effects upon the individual. Seizure frequency is associated with injuries, most commonly due to falls [3]. A review of studies found a small, but measurable decline in intellectual performance associated with seizures [4], and cognitive issues related to attention, memory, language, and information processing are of frequent concern [5–7]. Although another review reported that both children and adults were able to demonstrate plasticity and cognitive recovery after intervention to improve seizures [8], data from the Institute of Medicine indicate that cognitive, behavioral, and social problems may persist after epilepsy resolves [9]. Furthermore, increased seizures and poor seizure control increase the stigma associated with epilepsy [10] as the epilepsy, which may not have previously been apparent to others, becomes apparent when recreational and vocational activities are limited after a seizure occurs [9, 11]. The stigma, for many people with epilepsy, is among the most burdensome aspects of this disorder [12].
Depression, worldwide the second leading cause of years of life lost to disability [13], is common among people with epilepsy [14, 15]. A recent meta-analysis estimated the pooled prevalence of depressive disorders among people with epilepsy to be 23% [16]. Depression has predicted reduced quality of life in people with epilepsy more strongly than seizure frequency [17]. Individuals with epilepsy and depression also report increased levels of perceived seizure frequency and severity [18]. Such an increase in perceived frequency and severity could result from emotional reactivity, negative thinking, and/or stressors associated with depression. Research has shown that these factors influence both the way stressful events like having a seizure are interpreted and evaluated, as well as the actual occurrence of these events [19, 20], establishing a link between depression and seizures.
Furthermore, studies have suggested that having a history of depression increases the likelihood of developing epilepsy. The first such study, conducted in Sweden, matched newly diagnosed cases of epilepsy ages 17 to 74 to population-based controls by age and sex [21]. The odds of depression prior to onset were 17.2 times greater in cases than in controls. Another study of older adults found that cases with new-onset idiopathic/cryptogenic seizures had 3.7 times the odds of major depression prior to the onset of their first unprovoked seizure when compared to matched controls receiving medical evaluation during the same year as the case’s first unprovoked seizure [22]. In a population-based case-control study of Icelandic residents ages 10 years and older [23],cases were individuals with newly diagnosed, unprovoked seizures, each matched by age and gender to two controls. Cases had 1.7 times the odds of major depression preceding the onset of the unprovoked seizures. These studies establish depression as a risk factor for seizures. Subsequently, Hesdorffer et al. demonstrated that the relationship between depression and epilepsy is bidirectional: epilepsy can lead to depression, and depression can lead to epilepsy [24].
Recognizing the high rate of depression in people with epilepsy, combined with the transportation limitations of people with seizures, the Centers for Disease Control and Prevention (CDC) released a call for a home-based depression treatment program for people with epilepsy. With funding from the CDC, Project UPLIFT was developed to provide group delivery by telephone or Web of depression management skills to people with epilepsy [25]. The program was evaluated in two randomized, controlled studies. In the first study, conducted in one southeastern state, the Project UPLIFT intervention was found to increase depression-management knowledge and skills and reduce depressive symptoms among people with epilepsy who screened positive for depression [26]. Subsequently in the second study, funded by the National Institute for Minority Health and Health Disparities (NIMHD), the Project UPLIFT intervention demonstrated the same results among people with epilepsy from four geographically diverse states who had symptoms of depression, but did not screen positive for major depressive disorder [27]. In this study, Project UPLIFT also significantly reduced the incidence of Major Depressive Disorder compared to the treatment-as-usual waitlist.
The prior studies, reviewed above, establish a link between depression and an increase in perceived or actual seizure activity. Research has also demonstrated the effectiveness of participation in the Project UPLIFT intervention in reducing depressive symptoms. A question that remains is whether Project UPLIFT, in addition to its impact upon depression, has an impact upon seizures. The current analysis uses data from the NIMHD study to investigate two questions:
Did participation in the Project UPLIFT intervention decrease seizure frequency and severity?
If participation in the Project UPLIFT intervention decreased seizure frequency or severity, was this decrease mediated by a decrease in depressive symptoms?
Method
Design
This randomized, controlled trial used a cross-over design (see Figure 1). All groups were assessed at Baseline, Interim (after the intervention groups completed the program; at about 9-10 weeks), and Follow-up (after the treatment-as-usual [TAU] groups completed the program; at about 18-20 weeks). This analysis is based upon data from the first two assessments, at baseline and interim, before the cross-over occurred. Further details about the methodology are described elsewhere [27].
Figure 1.

Crossover Design
Intervention
Project UPLIFT is a psychoeducational program designed to teach mental health skills in 8-sessions delivered to groups by telephone or Web [25–27]. The content of the program is based upon Mindfulness-Based Cognitive Therapy (MBCT) [28] and is manualized, including a script for use by the telephone facilitators when leading activities and discussions. Because the delivery is not face-to-face, use of the script is feasible. The same script is used on the Web pages of the Internet version. The Project UPLIFT activities and discussions were designed to increase knowledge and skills related to mental health self-management. These include education about depression; monitoring, challenging, and changing of thoughts; coping and relaxing; attention and mindfulness; focusing on pleasure; the importance of reinforcement; and preventing relapse. Each session is planned to last one hour by telephone and includes a check-in period, educational material laid out in slides that covers the topic of that week’s session, group discussion, a skill-building exercise, and recommended material for practice between sessions.
Participants
Participants were recruited between 2010 and 2013 from the clinical populations to which the four participating university sites (located in Georgia, Michigan, Texas, and Washington) had access. Criteria for inclusion in the study were: 1) diagnosis of epilepsy; 2) at least three months post initial diagnosis of epilepsy and either on medication or physician-approved to participate; 3) symptoms of depression, but absence of moderate-to-severe depression on the Center for Epidemiologic Studies-Depression (CES-D) scale [29] (i.e., 8 < CES-D score < 27) or Major Depressive Disorder according to the Patient Health Questionnaire-9 (PHQ-9) [30]; 4) no active suicidal ideation; 5) 21 years of age and older; 6) English speaking; 7) access to a telephone; and 8) mentally stable, as determined by a score of > 23 on the telephone version of the Mini-Mental Status Examination (T-MMSE) [31].
A total of 367 adults were recruited from the four sites. Among those recruited, 183 did not meet inclusion criteria; 88 (24%) screened as too depressed, and 10 (3%) others expressed suicidal ideation. Random assignment and baseline assessment were performed on 128 people who met criteria and consented, but 10 of the 128 (7.8%) now met criteria for Major Depressive Disorder on the baseline assessment; these participants were excluded from the study. Subsequently, another participant scored as an extreme outlier for number of seizures and was also removed. Among the final 117 participants, 62 were in the intervention condition, and 55 were in the TAU group. Five (8.9%) intervention participants dropped out before attending any sessions and 5 others (8.9%) dropped out after attending at least one session, leaving 107 participants for the analyses. A CONSORT diagram is presented in Figure 2.
Figure 2.

CONSORT Flow Diagram
Measures
Measures of seizure severity, depressive symptoms, sleep, knowledge and skills, self-efficacy, self-compassion, satisfaction with life, and quality of life comprised the assessments at baseline and interim. The current study employed only the measures of seizure severity and depressive symptoms.
Seizure Frequency and Severity were assessed with the Liverpool Seizure Severity Scale (LSSS) [32]. The LSSS is a validated 12-item scale assessing the frequency and severity of seizures experienced using a 4-week reference period. This instrument quantifies seizure frequency by self-report, asking, “How many seizures have you experienced during the past 4 weeks?” Seizure severity assessed patients’ perceptions of the most severe seizure they had during the past 4 weeks.
Depressive Symptoms were assessed using the mBDI [33], a modified form of the BDI [34]. The 21-item BDI has demonstrated validity for assessing depression among people with epilepsy [35]. The mBDI assesses depression severity during the past 2 weeks. It is comprised of the original 21 items of the BDI, but it also includes a positive response category for each item. As a result, the responses are scaled from 0 (positive response) to 4 (severe). With the additional response category, the mBDI better detects differences in depression when depression scores are low [33].
Procedure
Assignment.
After being screened with the CES-D [29] and the T-MMSE [31] and giving consent, participants were stratified by whether or not they were on antidepressants and randomly assigned to the Project UPLIFT condition or the TAU waitlist condition. In the original study of Project UPLIFT, we found that Web and telephone delivery were equivalent in efficacy [26]. In the current study, therefore, within each condition, people who required a particular mode of delivery (Web or telephone) were placed in that group and the remainder (the majority of participants) were assigned to equalize the groups.
Assessment.
Baseline, interim, and follow-up assessments included the measures previously described. Assessment of participants from all sites was conducted by telephone by Master of Public Health students in Georgia. Participants were contacted in advance to schedule the timing of the assessment. They were paid $25 for each assessment completed, and $15 for each session attended.
Delivery.
Telephone sessions were held weekly at a scheduled time. Before each telephone session, participants received reminder phone calls. The telephone groups used the telephone technology services of the university in Georgia. Participants were provided with a conference bridge for each call; this allowed them to call in using their own telephone. Those whose call incurred long-distance charges, were provided a calling card number to cover the cost.
The Web-based intervention used Blackboard Course Management System software, a secure online learning system that houses content and includes communication tools. Blackboard tools can be accessed using standard dial-up or higher Internet access. As with a protected website, Blackboard content is accessible by computer at any time to study participants who have the required password(s). It can be used in any location, at any hour. Within the Blackboard system, one develops “courses,” which include asynchronous discussion boards, areas for posting content, and other resources. The Web intervention was created as a Blackboard course. Only the course in which (s)he was enrolled was accessible to the user once (s)he logged into the system. Users’ communications and personal information within the course could be viewed only by the users and system administrators. A username, which did not include an actual name, and a password created by each participant were the only personal information that was entered into Blackboard. Participants were allowed to choose whether or not they wished to share their names with other members of the group. Web sessions were posted on Mondays, and the previous session was moved to an accessible archive when a new session was posted. If a Web participant had not logged into the session by Wednesday, (s)he received a reminder call or email.
Safety management of the participants is described in detail elsewhere [27].
Analysis.
Data input and management were performed using SPSS version 24.0. Descriptive analyses were run and data were prescreened for missing data and outliers. Mean values were used to replace missing data for any participant who was missing fewer than 10 percent of the items on a scale. One extreme outlier was removed from the data and variables were centered. All statistical tests were 2-sided and a p-value ≤ 0.05 was considered statistically significant.
Chi squares and t-tests were used to determine whether the randomization produced equal intervention and TAU groups at baseline with respect to the variables measured. According to Vickers [36], ANCOVA should be selected as the method for the analysis of randomized trials with baseline measures, except when the data have extreme skew. Thus, we assessed the skewness of the outcome measures to ensure the skew was not extreme before changes in seizure measures over time in the intervention and TAU groups were assessed using repeated-measures analyses of covariance (ANCOVAs). The analyses controlled for any variables that differed between groups at baseline. We also planned to explore the association between the number of Project UPLIFT sessions attended and change in the seizure variables using Pearson’s correlation coefficient.
Mediation was assessed using MPlus version 7.2 [37]. Data were pre-screened for missing data, outliers, and skewness. Bootstrapping (5000 replications) was added to the analysis command to account for asymmetry, particularly for the number of seizures. Model fit was determined by examining the X2 statistic, Standardized Root Mean Square Residual (SRMR), Root Mean Squared Error of Approximation (RMSEA), and the Comparative Fit Index (CFI) [38].
Results
Descriptive Results
Twenty-two groups of up to 7 people received the Project UPLIFT program. A total of 118 participants were randomized and met study criteria. Participants ranged in age from 21 to 70, with a mean of 41.2 years and a median of 40.0 years; almost one-third (32.4%) were on antidepressant medication. Beck Depression scores ranged from 0 to 30 with a mean of 7.1 and a median of 6.0. A total of 108 (91.5%) participants completed the intervention, and one was removed due to the number of seizures at baseline being an extreme outlier (>10 standard deviations from the mean). Among the remaining 107 participants, 52 were assigned to the UPLIFT group (23 telephone, 29 Web) and 55 were assigned to the TAU group (26 telephone, 29 Web). Descriptive data for the 107 participants by condition are summarized in Table 1. Two-thirds of the 107 participants were female (66.4%). Most (n = 63, 58.9%) were in the 31-59 year age range. Most participants reported being Caucasian (n = 66, 60.7%), with 10 (9.3%) African Americans, 2 (1.9%) people of Hispanic origin, and 6 (5.6%) people of other races; 24 (22.4%) participants did not provide their race/ethnicity. The greatest proportions of participants were married (46.7%), and not working or on disability (37.4%), had graduated college or more (n = 52, 48.6%), and were living with family (n = 70, 65.4%). There were no significant differences in characteristics between the intervention and TAU waitlist conditions at baseline. The difference in number of days in the past 30 on which health was not good closely approached significance (p = 0.058), however, so it was controlled in the analyses. Neither the number of seizures in the past 30 days (t54.833 = 1.430; p = 0.159) nor seizure severity (t105 = 0.381, p = 0.704) differed between groups at baseline.
Table 1.
Demographic Characteristics of Participants
| Variable | Category | Intervention Group (n=52) | TAU Waitlist Group (n=55) | TOTAL (N=107) |
|---|---|---|---|---|
| n (%*) | n (%*) | |||
| Gender | Female | 35 (67.3) | 36 (65.5) | 71 (66.4) |
| Male | 17 (32.7) | 19 (34.5) | 36 (33.6) | |
| Age Group | <=30 | 17 (32.7) | 18 (32.7) | 35 (32.7) |
| 31-59 | 31 (59.6) | 32 (58.2) | 63 (58.9) | |
| 60+ | 4 (7.7) | 5 (9.1) | 9 (8.4) | |
| Race/Ethnicity | African American | 5 (9.6) | 5 (8.9) | 10 (9.3) |
| Hispanic | 1 (1.9) | 1 (1.8) | 2 (1.9) | |
| Caucasian | 31 (59.6) | 34 (61.8) | 66 (60.7) | |
| Other | 2 (3.8) | 4 (7.3) | 6 (5.6) | |
| No Response | 13 (25.0) | 11 (20.0) | 24 (22.4) | |
| Marital Status | Married | 27 (51.9) | 23 (41.8) | 50 (46.7) |
| Single, never married | 15 (28.8) | 24 (43.6) | 39 (36.4) | |
| Single, living with partner | 3 (5.8) | 3 (5.5) | 6 (5.6) | |
| Divorced | 6 (11.5) | 5 9.1) | 11( 10.3) | |
| Widowed | 1 (1.9) | 0 (0.0) | 1 (0.9) | |
| Employment | Working full-time | 17 (32.7) | 16 (29.1) | 33 (30.8) |
| Working part-time | 8 (15.4) | 6 (10.9) | 14 (13.1) | |
| Volunteer | 1 (1.9) | 1 (1.8) | 2 (1.9) | |
| Student | 5 (9.6) | 5 (9.1) | 10 (9.3) | |
| Retired | 2 (3.8) | 5 (9.1) | 7 (6.5) | |
| Do not work or on disability | 18 (34.6) | 22 (40.0) | 40 (37.4) | |
| Other | 1 (1.9) | 0 (0.0) | 1 (0.9) | |
| Education | High School or Less | 7 (13.5) | 12 (21.8) | 19 (17.8) |
| Some College | 11 (21.2) | 19 (34.5) | 30 (28.0) | |
| Graduated College or More | 30 (57.7) | 22 (40.0) | 52 (48.6) | |
| Other Program | 4 (7.7) | 2 (3.6) | 6 (5.6) | |
| Living Situation | Alone | 9 (17.3) | 14 (25.5) | 23 (21.5) |
| Family | 37 (71.2) | 33 (60.0) | 70 (65.4) | |
| Friend, Roommate, Partner | 5 (9.6) | 8 (14.5) | 13 (12.1) | |
| Homeless | 1 (1.9) | 0 (0.0) | 1 (0.9) |
Column percent
More than half of the participants (51.9%) had experienced seizures in the past 4 weeks. The average number of seizures in the last 4 weeks ranged from 0 to 100. The mean number of seizures (sd) was 4.2 (14.0) and the median was 1.0. The seizure severity score ranged from 0 to 85, with a mean (sd) of 20.3 (24.7) and a median of 1.25.
Table 2 presents the distribution properties of the seizure measures. The distributions for number of seizures were non-normal at both baseline and posttest. In this study, while the baseline and posttest distributions of number of seizures were somewhat skewed, the change in number of seizures was not. Thus, ANCOVA was used to analyze the changes in the seizure measures from baseline to posttest, as planned.
Table 2.
Distribution Properties of Seizure Variables
| Variable | Assessment | Mean | Skewness | Kurtosis |
|---|---|---|---|---|
| Number of Seizures | Baseline | 4.24 | 6.25 | 41.17 |
| Posttest | 3.82 | 6.77 | 54.74 | |
| Change | −0.42 | 0.377 | 33.75 | |
| Seizure Severity | Baseline | 20.16 | 0.74 | −0.95 |
| Posttest | 19.46 | 0.81 | −0.68 | |
| Change | −0.70 | −0.48 | 3.06 |
Analyses of Covariance (ANCOVAs)
Results of the repeated-measures ANCOVAs are presented in Table 3. While the average number of seizures increased by 2.3 in the TAU group, it was reduced by 3.2 in the UPLIFT group. The change in number of seizures differed significantly for the two groups (F1,104= 5.178; p = 0.025). Similarly, the seizure severity score increased by 2.7 in the TAU group but decreased by 2.2 in the UPLIFT group. This difference did not achieve statistical significance (F1,104=2.505, p = 0.117).
Table 3.
ANCOVA Results—Change in Seizure Variables by Condition
| Variable | Condition | Baseline | Posttest | Change | F-interaction | df | p-value |
|---|---|---|---|---|---|---|---|
| Number Seizures | UPLIFT | 6.6 | 3.4 | −3.2 | 5.178 | 1,104 | 0.025 |
| TAU | 2.0 | 4.3 | +2.3 | ||||
| Seizure Severity | UPLIFT | 20.8 | 16.6 | −2.2 | 2.505 | 1,104 | 0.117 |
| TAU | 19.5 | 22.2 | +2.7 |
The number of Project UPLIFT sessions attended was negatively skewed, with a mean of 6.56 and a median of 7.00 out of a possible 8 sessions to attend. Due to this skewness, we categorized the attendance variable; we elected to categorize into tertiles because assessing dose-response requires a minimum of three categories. The first tertile was comprised of those attending 5 or fewer sessions, the second tertile was those attending 6 or 7 sessions, and the third tertile was those attending all 8 sessions. After categorizing the variable, we used ANOVA rather than Pearson’s correlation to assess the association of tertile of attendance with changes in the seizure outcomes (Table 4). As attendance increased, change in number of seizures decreased. No similar dose relationship was found for seizure severity.
Table 4.
Change in Seizure Variables by Tertile of Attendance (n=52)
| UPLIFT Sessions Attended | n | Mean Change in Number of Seizures | Mean Change in Seizure Severity |
|---|---|---|---|
| 1-5 | 12 | 0.00 | −1.25 |
| 6-7 | 17 | −.94 | −1.18 |
| All 8 | 23 | −5.83 | −6.96 |
Mediation Analyses
The ANOVA analysis tests a total path from condition to the outcome. According to Kenny and Judd [39] there is higher power for testing an indirect path through a mediating variable, relative to the total path. For this reason, the mediation analysis was conducted if the ANCOVA achieved a p-vlaue less than 0.20. The mediation analyses tested whether the proposed mediating variable (Depression at posttest), mediated between treatment group (UPLIFT versus TAU waitlist) and each seizure measure at posttest, when controlling for Depression at baseline, that seizure measure at baseline, and the control variable (number of days in the past 30 on which health was not good). Suggested Hu and Bentler Criteria [38] are Standardized Root Square Mean Residual (SRMR) ≤ 0.08, Comparative Fit Index (CFI) ≥ 0.95, and Root Mean Square Error of Approximation (RMSEA) ≤ 0.06.
Figure 3 illustrates the relationships of Treatment Group, Depression, and Number of Seizures, when baseline depression and number of seizures are controlled, as well as number of days when health was not good. The model fit was adequate, χ2 = 7.59, df(3), p = .06. The SRMR (0.045) and CFI (0.966) met the suggested fit criteria. The RMSEA (0.120) did not, but Kenney, Kaniskan, and Mccoach [40] found that this measure too often incorrectly indicates a model is a poor fit when degrees of freedom are low (i.e., N is less than 200) and recommend against its use in this circumstance. The total effect for the model was significant (Estimate = - 0.260, 95% CI = −0.740, −0.009). The confidence interval for direct effect of condition to number of seizures demonstrated significance (Estimate = −0.224; 95% CI = −0.625, −0.007). The indirect (mediation) effect from treatment through depression at posttest to number of seizures at posttest was not significant (Estimate = −0.036; 95% CI = −0.217, 0.005).
Figure 3.

Longitudinal Path Analysis for Number of Seizures at Posttest, controlling for baseline depression, baseline number of seizures, and days health was not good (n = 107)
Figure 4 illustrates the relationships of Treatment Group, Depression, and Seizure Severity when baseline depression and seizure severity are controlled, along with number of days when health was not good. The model fit was adequate, χ2 = 7.01, df(3), p = .07. The SRMR (0.044) and CFI (0.974) met the suggested fit criteria. Once again, the RMSEA (0.112) did not. The total effect was not significant (Estimate = −.255, 95% CI = −0.555, 0.052). The confidence interval for direct effect of condition to number of seizures was not significant (Estimate = −0.162; 95% CI = −0.460, 0.150). The indirect (mediation) effect from treatment through depression-at-posttest to seizure severity-at-posttest was significant (Estimate = −0.092, CI = −0.239, −0.015).
Figure 4.
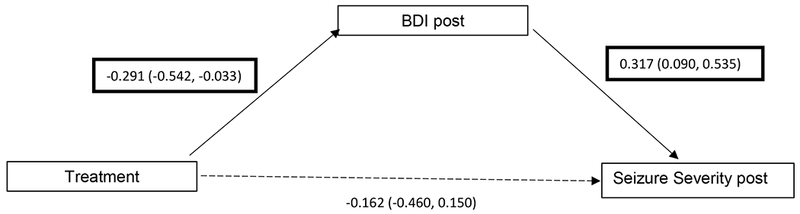
Longitudinal Path analysis for Seizure Severity, controlling for baseline depression, baseline seizure severity, and days health was not good (n = 107)
Discussion
Summary of Findings
As noted in the Introduction, seizures are costly in terms of both financial resources and their physical, cognitive, and social effects [3, 4, 8, 12, 15, 41]. In this study of the effect of Project UPLIFT on seizures, we found that participation in the program significantly reduced the number of seizures, but not seizure severity. On average, the number of seizures in the past 30 days decreased by more than 3 in the intervention group, while increasing by more than 2 in the TAU waitlist group. As participants attended more sessions, the decrease in number of seizures was greater, but no similar dose-effect was found for seizure severity. Through path analysis, we further found that the impact of Project UPLIFT participation on number of seizures was not mediated by the decrease in depressive symptoms resulting from the program. In contrast, Project UPLIFT did have an indirect impact on perceived seizure severity that operated through depressive symptoms.
The finding that participation in Project UPLIFT reduced the reported number of seizures, but that the effect did not operate through the reduction in depressive symptoms suggests the reduction is not due to cognitive or other factors associated with improved mood state [19, 20], or to the reduced level of depression, a potential precipitant of seizures. Based in MBCT, Project UPLIFT has the potential to impact factors other than depression such as anxiety [42], stress [43], insomnia [44], or general self-management skills, which may have, in turn, affected seizure frequency. In other analyses, we did not see a change in reported sleep quality as a result of participating in Project UPLIFT, but we did not have measures of anxiety, stress, or general self-management to explore.
The finding that there was a significant mediation effect of depressive symptoms on the relationship between Project UPLIFT participation and perceived seizure severity, but negative findings for the ANCOVA, and the total effect in the model is not surprising. Kenny and Judd [39] have described the higher power associated with testing an indirect path relative to the total path, which is also tested by the ANCOVA. The significant mediation effect of the path from Project UPLIFT to perceived seizure severity by depressive symptoms is consistent with prior findings. Project UPLIFT significantly reduces depressive symptoms in people with epilepsy [26, 27], and people with epilepsy and depression report higher levels of perceived seizure severity than those without depression [17].
Implications for Health and Cost Saving
We found that participation in Project UPLIFT, a distance-delivered self-management program, reduced seizures among participants by an average of 3, while seizures in the TAU waitlist condition increased by an average of 2. Thus, program participation reduced the seizures per person by somewhere between 3 and 5 in the 30-day period assessed. This represents about 18 to 30 seizures per month in a group of six Project UPLIFT program participants.
Reducing seizures is critical for a variety of physical and mental health reasons. Research shows a mild cognitive decline, particularly related to memory, in adults with a longstanding history of seizures [4]. In addition, patients with epilepsy experience deficits in attention and concentration [45], and fatigue is more severe among epilepsy patients than controls, especially among those with epilepsy whose seizures are uncontrolled [46]. Not surprisingly, then, seizures and their cognitive effects can result in an increased risk of injury from falls, motor vehicle crashes, burns or submersion (drowning), as well [47]. Moreover, seizure frequency is associated with depression [48], anxiety [49], and quality of life [50].
In addition to these health benefits, the reduction in seizures resulting from participation in Project UPLIFT has important implications for saving health care costs. In 2014, the total cost burden of epilepsy (medical cost and lost or reduced earnings and productivity) was estimated at $36.8 billion for 2.8 million Americans with epilepsy [51]. More recent figures estimate there were 3.4 million people with active epilepsy in 2015 [52], leading to an increase in costs.
Using claims data from 2007-2009 for 8,571 adult patients with controlled epilepsy, the average cost of a visit to the emergency department (ED) was $316 [53]. In 2008, the average cost per admission to a U.S. hospital for a person with epilepsy/convulsion was $18, 739 [54]. These costs are significantly higher today simply on the basis of the 2-3% annual medical cost inflation [55]. In contrast, the cost of conducting an 8-session UPLIFT program ranges from $1150-$2525, depending on the salary and credentials of the facilitator. Thus, if the 18-30 seizures that were averted during the 30-day period assessed resulted in the elimination of 5 ED visits, 1 hospitalization, or some combination of the two, the program would pay for itself in one month. This is likely, since depression [56] and anxiety [57] are associated with increased use of the ED for seizures, and participation in mindfulness-based cognitive therapy programs like Project UPLIFT has been shown to reduce depression, anxiety, and other psychiatric disorders [26, 27, 58, 59].
Study Limitations and Strengths
One main limitation of this study is the insufficient power to detect the main effect of Project UPLIFT upon perceived seizure severity. There was, however, sufficient power to detect the indirect pathway from participation in Project UPLIFT through depressive symptoms to decreased seizure severity. Another limitation was the representation of racial and ethnic minorities among the participants. To address this issue, studies are currently underway to assess the effectiveness of Project UPLIFT among Blacks [60] and Hispanics [61]. These studies can also explore the impact of Project UPLIFT upon stress; the study among Blacks includes a measure of post-traumatic stress disorder, and the study among Hispanics includes a measure of the perception of stress.
The strengths of this study include the randomized, controlled design; the use of validated seizure and depression measures; the assessment of dose-response; and the path analysis test of mediation. These features of the study contribute to the strength of the findings of an impact of Project UPLIFT upon seizure frequency and severity.
Conclusion
Participation in Project UPLIFT, an evidence-based, distance-delivered intervention based upon mindfulness-based cognitive therapy, directly reduced the number of seizures experienced by participants with epilepsy. It also reduced perceived seizure severity indirectly, by reducing depressive symptoms. Providing this low-cost, self-management intervention to people with epilepsy has the potential to impact the health and well-being of people with epilepsy, as well as their significant seizure-related health care costs.
Highlights.
Depression and seizures are linked
Participation in Project UPLIFT, a depression self-management intervention, directly reduced seizure frequency
Participation in Project UPLIFT indirectly reduced and perceived seizure severity through reduction in depression
Participation in the Project UPLIFT self-management intervention may improve seizure control and reduce seizure-related costs
Acknowledgments
FUNDING:
This research was supported by the National Center for Minority Health and Health Disparities NIH Grant #5RC1 MD004563]
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Johnson EL. Seizures and epilepsy. Medical Clinics of North America 2019;103: 309–324. [DOI] [PubMed] [Google Scholar]
- [2].Scharfman HE. The neurobiology of epilepsy. Current Neurology and Neuroscience Reports 2007;7: 348–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Lawn ND, Bamlet WR, Radhakrishnan K, O’Brien PC, So EL. Injuries due to seizures in persons with epilepsy. Neurology 2004;63: 1565–1570. [DOI] [PubMed] [Google Scholar]
- [4].Vingerhoets G Cognitive effects of seizures. Seizure 2006;15: 221–6. [DOI] [PubMed] [Google Scholar]
- [5].Hermann BP, Seidenberg M, Dow C, Jones J, Rutecki P, Bhattacharya A, Bell B. Cognitive prognosis in chronic temporal lobe epilepsy. Ann Neurol 2006;60: 80–7. [DOI] [PubMed] [Google Scholar]
- [6].Hermann B, Meador KJ, Gaillard WD, Cramer JA. Cognition across the life span: Antiepileptic drugs, epilepsy, or both? Epilepsy & Behavior 2010;17: 1–5. [DOI] [PubMed] [Google Scholar]
- [7].Berg AT, Langfitt JT, Testa FM, Levy SR, DiMario F, Westerveld M, Kulas J. Global cognitive function in children with epilepsy: a community-based study. Epilepsia 2008;49: 608–14. [DOI] [PubMed] [Google Scholar]
- [8].Elger CE, Helmstaedter C, Kurthen M. Chronic epilepsy and cognition. Lancet Neurol 2004;3: 663–72. [DOI] [PubMed] [Google Scholar]
- [9].IOM (Institute of Medicine). Epilepsy across the spectrum : Promoting health and understanding. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- [10].Stigma Jacoby A., epilepsy, and quality of life. Epilepsy & Behavior 2002;6: 10–20. [DOI] [PubMed] [Google Scholar]
- [11].Lopez de Souza J, Faiola AS, Miziara CSMG, & Giraldes de Manreza ML. The perceived social stigma of people with epilepsy with regard to the question of employability. Neurology Research International 2018;2018: 4140508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Fisher RS. Epilepsy from the Patient’s Perspective: Review of Results of a Community-Based Survey. Epilepsy Behav 2000;1: S9–S14. [DOI] [PubMed] [Google Scholar]
- [13].Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJL, Vos T, & Whiteford HA. Burden of Depressive Disorders by Country, Sex, Age, and Year: Findings from the Global Burden of Disease Study 2010. PLOS Medicine 2013;10: e1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].CDC. Epilepsy: One of the nation’s most common disabling neurological disorders. . In. http://www.cdc.gov/epilepsy: United States Department of Health and Human Services, Centers for Disease Control and Prevention; 2006. [Google Scholar]
- [15].Peterson CL, Walker C, Shears G. The social context of anxiety and depression: exploring the role of anxiety and depression in the lives of Australian adults with epilepsy. Epilepsy Behav 2014;34: 29–33. [DOI] [PubMed] [Google Scholar]
- [16].Scott AJ, Sharpe L, Hunt C, & Gandy M. Anxiety and depressive disorders in people with epilepsy: A meta-analysis. Epilepsia 2017;58: 973–982. [DOI] [PubMed] [Google Scholar]
- [17].Boylan LS, Flint LA, Labovitz DL, Jackson SC, Starner K, Devinsky O. Depression but not seizure frequency predicts quality of life in treatment resistant epilepsy. Neurology 2004;62: 258–261. [DOI] [PubMed] [Google Scholar]
- [18].Cramer JA, Blum D, Reed M, Fanning K, Epilepsy Impact Project G. The influence of comorbid depression on seizure severity. Epilepsia 2003;44: 1578–84. [DOI] [PubMed] [Google Scholar]
- [19].Simons AD, Angell KL, Monroe SM, Thase ME. Cognition and life stress in depression: cognitive factors and the definition, rating, and generation of negative life events. J Abnorm Psychol 1993;102: 584–91. [PubMed] [Google Scholar]
- [20].Safford SM, Alloy LB, Abramson LY, Crossfield AG. Negative Cognitive Style as a Predictor of Negative Life Events in Depression-Prone Individuals: A Test of the Stress Generation Hypothesis. Journal of Affective Disorders 2007;99: 147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Forsgren L, Nystrom L. An incident case-referent study of epileptic seizures in adults. Epilepsy Res 1990;6: 66–81. [DOI] [PubMed] [Google Scholar]
- [22].Hesdorffer DC, Hauser WA, Annegers JF, Cascina G. Major depression is a risk factor for seizures in older adults. Annals of Neurology 2001;47: 246–249. [PubMed] [Google Scholar]
- [23].Hesdorffer DC, Hauser WA, Olafsson E, Ludvigsson P, Kjartansson O. Depression and suidical attempt as risk factors for incidental unprovoked seizures. Annals of Neurology 2006;59: 35–41. [DOI] [PubMed] [Google Scholar]
- [24].Hesdorffer DC, Ishihara L, Mynepalli L, Webb DJ, Weil J, & Hauser WA. Epilepsy, suicidality, and psychiatric disorders: A bidirectional association. . Annals of Neurology 2012; 72: 184–191. [DOI] [PubMed] [Google Scholar]
- [25].Walker ER, Obolensky N, Dini S, Thompson NJ. Formative and process evaluations of a cognitive-behavioral therapy and mindfulness intervention for people with epilepsy and depression. Epilepsy Behav 2010;19: 239–46. [DOI] [PubMed] [Google Scholar]
- [26].Thompson NJ, Walker ER, Obolensky N, Winning A, Barmon C, Diiorio C, Compton MT. Distance delivery of mindfulness-based cognitive therapy for depression: project UPLIFT. Epilepsy Behav 2010; 19: 247–54. [DOI] [PubMed] [Google Scholar]
- [27].Thompson NJ, Patel AH, Selwa LM, Stoll SC, Begley CE, Johnson EK, Fraser RT. Expanding the efficacy of Project UPLIFT: Distance delivery of mindfulness-based depression prevention to people with epilepsy. J Consult Clin Psychol 2015;83: 304–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Segal ZV, Williams JMG, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. New York: Guilford; 2002. [Google Scholar]
- [29].Devins G, Orme C. Center for Epidemiologic Studies Depression Scale In: Kaiser D, Sweetland R, editors. Test Critiques. Kansas City, MO: Test Corporation of America; 1985. [Google Scholar]
- [30].Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16: 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Newkirk LA, Kim JM, Thompson JM, Tinklenberg JR, Yesavage JA, Taylor JL. Validation of a 26-point telephone version of the Mini-Mental State Examination. J Geriatr Psychiatry Neurol 2004;17: 81–7. [DOI] [PubMed] [Google Scholar]
- [32].Scott-Lennox J, Bryant-Comstock L, Lennox R, Baker GA. Reliability, validity and responsiveness of a revised scoring system for the Liverpool Seizure Severity Scale. Epilepsy Res 2001;44: 53–63. [DOI] [PubMed] [Google Scholar]
- [33].Dori GA, Overholser JC. Evaluating depression severity and remission with a modified Beck Depression Inventory. Personality and Individual Differences 2000;28: 1045–1061. [Google Scholar]
- [34].Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford Press; 1979. [Google Scholar]
- [35].Jones JE, Hermann BP, Woodard JL, Barry JJ, Gilliam F, Kanner AM, Meador KJ. Screening for major depression in epilepsy with common self-report depression inventories. Epilepsia 2005;46: 731–5. [DOI] [PubMed] [Google Scholar]
- [36].Vickers AJ. Parametric versus non-parametric statistics in the analysis of randomized trials with non-normally distributed data. BMC Med Res Methodol 2005;5: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Muthen LK, Muthen B. MPlus. Los Angeles, CA.: Muthen & Muthen; 2010. [Google Scholar]
- [38].Hu L-t, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. . Structural Equation Modeling 1999;6: 1–55. [Google Scholar]
- [39].Kenny DA, Judd CM. Power anomalies in testing mediation. Psychol Sci 2014;25: 334–9. [DOI] [PubMed] [Google Scholar]
- [40].Kenny DA, Kaniskan B, McCoach DB. The Performance of RMSEA in Models With Small Degrees of Freedom. Sociological Methods & Research 2014;44: 486–507. [Google Scholar]
- [41].Begley CE, Famulari M, Annegers JF, Lairson DR, Reynolds TF, Coan S, Dubinsky S, Newmark ME, Leibson C, So EL, Rocca WA. The cost of epilepsy in the United States: an estimate from population-based clinical and survey data. Epilepsia 2000;41: 342–51. [DOI] [PubMed] [Google Scholar]
- [42].Noordali F, Cumming J, Thompson JL. Effectiveness of Mindfulness-based interventions on physiological and psychological complications in adults with diabetes: A systematic review. J Health Psychol 2017;22: 965–983. [DOI] [PubMed] [Google Scholar]
- [43].Phang CK, Chiang KC, Ng LO, Keng S-L, Oei TPS. Effects of brief group Mindfulness-based Cognitive Therapy for stress reduction among medical students in a Malaysian university Mindfulness 2016;7: 189–197. [Google Scholar]
- [44].Wong SY, Zhang DX, Li CC, Yip BH, Chan DC, Ling YM, Lo CS, Woo DM, Sun YY, Ma H, Mak WW, Gao T, Lee TM, Wing YK. Comparing the Effects of Mindfulness-Based Cognitive Therapy and Sleep Psycho-Education with Exercise on Chronic Insomnia: A Randomised Controlled Trial. Psychother Psychosom 2017;86: 241–253. [DOI] [PubMed] [Google Scholar]
- [45].Perrine K, Kiolbasa T. Cognitive deficits in epilepsy and contribution to psychopathology. Neurology 1999;53: S39–48. [PubMed] [Google Scholar]
- [46].Kwon OY, Park SP. Interictal fatigue and its predictors in epilepsy patients: A case-control study. Seizure 2016;34: 48–53. [DOI] [PubMed] [Google Scholar]
- [47].Nguyen R, Tellez Zenteno JF. Injuries in epilepsy: a review of its prevalence, risk factors, type of injuries and prevention. Neurol Int 2009;1: e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Thapar A, Roland M, Harold G. Do depression symptoms predict seizure frequency—or vice-versa? . Journal of Psychosomatic Research 2005;59: 269–274. [DOI] [PubMed] [Google Scholar]
- [49].Smith DF, Baker GA, Dewey M, Jacoby A, Chadwick DW. Seizure frequency, patient-perceived seizure severity and the psychosocial consequences of intractable epilepsy. Epilepsy Res 1991;9: 231–41. [DOI] [PubMed] [Google Scholar]
- [50].McLaughlin DP, Pachana NA, McFarland K. Stigma, seizure frequency and quality of life: the impact of epilepsy in late adulthood. Seizure 2008;17: 281–7. [DOI] [PubMed] [Google Scholar]
- [51].Gooch CL, Pracht E, Borenstein AR. The burden of neurological disease in the United States: A summary report and call to action. Ann Neurol 2017;81: 479–484. [DOI] [PubMed] [Google Scholar]
- [52].Zack MM, Kobau R. National and State Estimates of the Numbers of Adults and Children with Active Epilepsy - United States, 2015. MMWR Morb Mortal Wkly Rep 2017;66: 821–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Cramer JA, Wang ZJ, Chang E, Powers A, Copher R, Cherepanov D, Broder MS. Healthcare utilization and costs in adults with stable and uncontrolled epilepsy. Epilepsy Behav 2014;31: 356–62. [DOI] [PubMed] [Google Scholar]
- [54].Holmquist L, Russo CA, Elishauser A. Hospitalizations for Epilepsy and Convulsions, 2005 In: HCUP Statistical Brief #46. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [PubMed] [Google Scholar]
- [55].United States Department of Labor BoLS. Consumer Price Index. 2018.
- [56].Grinspan ZM, Shapiro JS, Abramson EL, Hooker G, Kaushal R, Kern LM. Predicting frequent ED use by people with epilepsy with health information exchange data. Neurology 2015;85: 1031–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Noble AJ, Goldstein LH, Seed P, Glucksman E, Ridsdale L. Characteristics of people with epilepsy who attend emergency departments: prospective study of metropolitan hospital attendees. Epilepsia 2012;53: 1820–8. [DOI] [PubMed] [Google Scholar]
- [58].Evans S, Ferrando S, Findler M, Stowell C, Smart C, Haglin D. Mindfulness-based cognitive therapy for generalized anxiety disorder. J Anxiety Disord 2008;22: 716–21. [DOI] [PubMed] [Google Scholar]
- [59].Chiesa A, Serretti A. Mindfulness based cognitive therapy for psychiatric disorders: a systematic review and meta-analysis. Psychiatry Res 2011;187: 441–53. [DOI] [PubMed] [Google Scholar]
- [60].Hunter-Jones JJ, Nellum AL, Olorundare El, McCloud CC, McCurdy MD, McGee RE, Davis CM, Thompson NJ, Quarells RC. Assessing the cultural appropriateness of UPLIFT for African Americans with epilepsy: A community engaged approach. Journal of the Georgia Public Health Association 2016;6. [Google Scholar]
- [61].Diaz L, Payano L, Montesdeoca J, Friedman D, Singh A, Devinsky O, Spruill T. Intervention targets to reduce depression in Hispanic adults with epilepsy: the role of mindfulness and rumination. . In: American Epilepsy Society Annual Meeting. New Orleans, LA; 2018. [Google Scholar]


