Abstract
Introduction:
Many individuals with stroke still have functional difficulties with their affected hand after going through a rehabilitation program. A 3D printed upper limb exoskeleton was designed for an individual who had a stroke. Functional and neuromuscular outcomes were measured using his affected hand with and without a 3D printed passive exoskeleton. The goal of this study was to determine the functional and neuromuscular changes induced by the 3D printed exoskeleton in a participant with stroke.
Materials and methods:
The functional ability of the exoskeleton was assessed using the Fugl-Meyer Assessment and the Box and Block Test. Strength testing and muscle activation of the participant’s forearms were measured during maximal voluntary contractions. Furthermore, EMG was measured during the Box and Block Test and satisfaction and usability of the 3D printed exoskeleton were assessed using standardized questionnaires.
Results:
The exoskeleton improved both the participant’s Fugl-Meyer Assessment scores and Box and Block test scores compared to not wearing the device. The subject had increased EMG activation in his extensor when wearing the exoskeleton.
Conclusion:
The inexpensive 3D printed exoskeleton was effective in assisting the participant with stroke during the functional assessments and has the potential to be used to help regain function of the hand in the home setting of an individual with stroke.
Keywords: hand, exoskeleton, additive manufacturing, computer-aided design, stroke, biomechanics
Introduction
Stroke leads to disability and loss of motor function[1,2]. When the cerebral cortex is injured, motor deficits are usually seen on the opposite side of where the stroke occurred[2]. Pathways from the brain, down the spine, and to the neuromuscular junction become damaged. These pathways may not be as regulated by the damaged portion of the brain as they were when the brain was healthy. Individuals with stroke have shown to have poor muscle activation in their paretic forearms compared to their non paretic forearms[3]. When recovering, individuals with stroke also tend to regain some flexor movement of their fingers more than extensor movement[4].
An additional impairment in many individuals with stroke is spasticity with a predominantly flexor tone. Due to this permanently flexed hand, the individual with stroke has reduced hand dexterity. Upper limb uni-manual movements and bi-manual movements lose speed and coordination compared to healthy controls[5]. Individuals with stroke may become limited to just using their unaffected hand[1] and this can reduce their performance of daily living, as well as their quality of life. This decline in quality of life has been addressed with sensorimotor arm therapy where participants with stroke have shown improvement in upper limb mobility[6,7]. However, many participants still lack function in their affected hand when rehabilitation is finished[8,9].
Wearable devices, such as exoskeletons are useful in that they offer the ability for individuals to regain mobility in their own environment[10]. Hand exoskeletons are designed to assist and promote movement of the user’s affected hand while being used without a health care professional present. The Saebo Flex is a current commercially available passive exoskeleton that has shown to improve patient’s hand function after therapy sessions in a clinical setting and on loan in a home setting[11,12]. Our inexpensive and simple passive exoskeleton design is produced on a low-cost 3D printer. When fully assembled, the hand exoskeleton is lightweight and mobile. The device can therefore be taken outside of the lab to be used in a home based environment which may be more convenient and practical to the user.
In addition to ease of availability, it is important for the exoskeleton to be effective and useful with participants with stroke. Traditional definitions of usability incorporate effectiveness, efficiency, and satisfaction of the user with the product[13]. In the context of individuals with stroke, the exoskeleton should be able to assist the user in extending their affected hand and allow for flexion to grasp an object. The elastic component of the hand exoskeleton will allow the user to keep the hand open overcoming increased hand flexor muscle tone allowing a functional grasp.
The objective of this case study was to determine the functional and neuromuscular changes induced by the 3D printed exoskeleton in a participant with stroke. It was hypothesized that our custom designed exoskeleton would increase the function of the affected hand by showing an improvement in functional test results.
Methods
Subject
A 67-year-old male more than six months post-stroke, with his right hand affected from the stroke participated in this study. The stroke occurred 17 years ago, and the subject was right hand dominant. The participant suffered a middle cerebral artery stroke that occurred in the left hemisphere of his brain. The frontal lobe, lateral regions in the parietal lobe and temporal lobe receive blood from the middle cerebral artery. The subject’s left frontal lobe, including the motor cortex, was damaged. After the stroke, the subject had spasticity in his right arm and hand. The subject had difficulty with movement of the right shoulder, right arm, and extending the fingers of his right hand. Performing a maximum voluntary contraction (MVC) with his affected hand, the subject’s flexor EMG measured an average of 13.61 μVrms and the flexor muscle averaged a force of 66.69 N. The subject’s extensors had an MVC EMG average value of 27.03 μVrms and an average force of 47.07 N. Prior to participating in the study, the participant regularly went for long walks and participated in a weight training exercise program. The subject was fitted for a 3D printed exoskeleton to assist with extension of his hand. The study was approved by the University of Nebraska Medical Center Institutional Review Board, IRB# 805–17-EP.
Passive Hand Exoskeleton
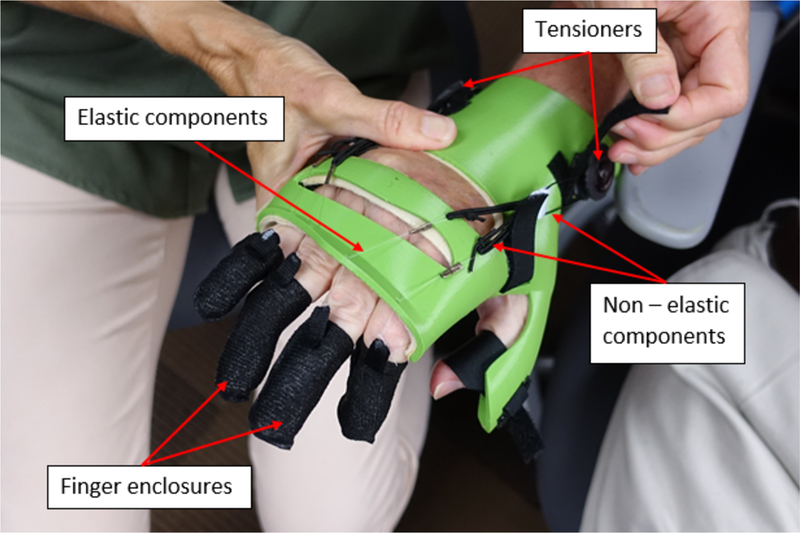
The exoskeleton developed incorporates elastic and tension control of the non-elastic components (Figure 1). The tensioners to control the non-elastic components are located on the dorsal side of the body of the exoskeleton. The body of the exoskeleton is attached to the forearm of the user through Velcro straps on the ventral side. The elastic cords connect with the non-elastic component midway between the tensioners and the wrist of the user. The elastic cords run through guides at the distal end of the body of the exoskeleton. These guides separate the elastic cord to direct them to a specific finger. The elastic cords attach on the dorsal side of each finger enclosure. Extension of the fingers occurs at this attachment point. Each finger has its own enclosure that fits snugly around the distal and intermediate phalanges of each finger. These finger enclosures are custom fit to each user in order to prevent slipping.
Figure 1.
The exoskeleton with elastics and tension control
The user was able to tighten the tensioner system to shorten the length of the elastic cords to control the tension and thus extending the user’s fingers. Due to the elastic properties of the cords, once the user’s fingers are extended the user is able to flex his fingers to stretch the elastic cords and grasp an object. The passive exoskeleton allows for an object to be grasped by utilizing the elasticity of the cords and active control of flexion by the user.
3D Printing Specifications
The exoskeleton device was designed on a desktop 3D printer (Ultimaker 2+ Extended, Ultimaker B.V., Geldermalsen, The Netherlands) with a building platform of at least 28.5 cm x 15.3 cm x 15.5 cm. The exoskeleton was manufactured using PLACTIVE™ (PLACTIVE™ 1% Antibacterial Copper-nanocomposite additive, Copper3D Inc, Nebraska, USA). The exoskeleton was printed at 35% - 40% infill (hexagon pattern), 60 – 100 mm/s print speed, 150 – 200 mm/s travel speed, 50° C heated bed, 0.15 – 0.25 mm layer height, and 0.8 mm shell thickness.
Procedure
Hand measurements were obtained from the subject during an orientation visit to produce the custom exoskeleton. Once the exoskeleton was printed and assembled, it was fitted for the subject. To assess hand function, the subject went through the Fugl-Meyer Assessment of Physical Performance, Upper Extremity, VIII. Hand (8a, 8b, 8d, 8e, 8f, 8g). The Fugl-Meyer Assessment (FMA) was performed by a trained hand therapist. The FMA was done with the participant’s paretic hand without the exoskeleton and with the exoskeleton. Once finished with the assessment, the subject moved on to strength testing.
Strength measurements were taken with a microFET3 manual muscle testing handheld dynamometer (Hoggan Scientific in Salt Lake City, Utah). The dynamometer was used to measure flexor and extensor strength during Maximal Voluntary Contractions (MVC). The applicator pad of the muscle testing dynamometer was stabilized at the distal end of the affected hand. The pad was placed on the anterior side for flexion and on the dorsal side for extension. The participant’s arm and wrist were stabilized in a neutral position using a customized arm rest and Velcro straps while seated in a chair. The subject was asked to flex and extend his wrist pushing on the pad of the muscle testing dynamometer as hard as possible for a period of 6 s. Time was given to rest between contractions. Each measure was repeated two times for each motion and the average of the two measures was used for the analysis.
Wireless Delsys Trigno Avanti EMG sensors (Delsys, Natick, Massachusetts, USA) were used to obtain the maximum EMG output from the flexor and extensor of the forearm during maximum voluntary contraction. The subject had separate surface EMG sensors placed on the flexor carpi ulnaris and the extensor digitorum muscles of his affected arm. The sensors have 4 silver bar contacts for acquiring the EMG signal. To obtain the highest possible signal, these bars were oriented perpendicular to the muscle fibre direction. The surface of the skin was cleaned with an alcohol wipe to ensure the best signal.
The wireless sensors relayed the signal back to the base which was in turn stored and saved with the EMGWorks Software (Version 4.5.4, Delsys, Natick, Massachusetts, USA). The amplitude (microvolts root-mean-square, μVrms) was calculated using the maximum 2.0 second time period of the 6 second isometric muscle action.
The Box and Block test (Figure 2) was carried out using previous methods described by Mathiowetz et al[14]. The Box and Block test[15] required the subject to move 1 inch blocks one at a time from one box, over a partition, and to drop the blocks in the adjacent box. The subject was seated comfortably and completed two trials of the box and block test with his affected hand both with and without the exoskeleton, for a total of four trials.
Figure 2.
Box and Block Test format
Exertion while using the exoskeleton during the box and block test was measured using the Delsys EMG wireless sensors and an RPE scale. The EMG sensors were placed on the flexor carpi ulnaris and the extensor digitorum of the subject during the maximal voluntary contraction and kept in the same place during the box and blocks trials. The signals were normalized by taking the submaximal values and dividing them by the maximal EMG signal values from the maximum voluntary contraction. After normalization the signals were averaged for each task.
After each trial of the box and blocks test the subject was shown the Borg RPE scale ranging from 0 – 10[16]. The subject gave a number based on the perceived exertion of that box and block trial where 0 meant no exertion and 10 meant maximal exertion. These values were averaged for each task.
The participant was given two usability questionnaires to fill out after completion of the trials, the first of which was the System Usability Scale[17] (SUS). The SUS[17] is quick, ten question survey with a five-point Likert scale to assess the usability of a device. The SUS is scored from 0 – 100 and has eight questions that focus on the usability aspect of the device and two questions that focus on the learnability of the device. The best score for each odd question is a five and the best score for each even question is one. The SUS is scored by subtracting one point from each odd question and subtracting from five with each score of the even questions. Therefore, the maximal value for each question becomes four. After performing the proper calculation for each question, the values for all ten questions are summed together and the sum is multiplied by 2.5. Since the best possible score for each question is four, adding all scores together can give a total of 40. Multiplying 40 by 2.5 gives the maximum score of 100.
The second questionnaire given to the participant was the Quebec User Evaluation of Satisfaction with assistive Technology[18] (QUEST). The QUEST[18] is a reliable tool to evaluate the satisfaction of patients using assistive technology. The QUEST is made up of 12 questions, each on a five-point satisfaction scale. The questionnaire is divided into two parts, “device” and “service”, these two portions can be totalled together to obtain a total QUEST score. The “service” portion did not pertain to this study and therefore the “device” portion of the QUEST was the only portion assessed.
Results
Possible FMA scores for the hand ranged from 0 to 12. Without the exoskeleton, the subject received a score of 0. With the exoskeleton, the subject received a score of 10. Table 1 has a breakdown of the scoring of the FMA.
Table 1.
Fugl-Meyer Assessment
| Without Exoskeleton | With Exoskeleton | |
|---|---|---|
| Finger Mass Flexion | 0 | 2 |
| Finger Mass Extension | 0 | 2 |
| Grasp II (Note card) | 0 | 2 |
| Grasp III (Pencil) | 0 | 0 |
| Grasp IV (Cylinder) | 0 | 2 |
| Grasp V (Tennis ball) | 0 | 2 |
0 = the task could not be performed, 1 = the task was partially completed or the object can be held, but not against a slight tug, 2 = the task had full active flexion/extension or the object for the specific grasp was held firmly against a tug.
The Box and Blocks test resulted in the subject moving an average of five more blocks with the exoskeleton compared to not wearing the exoskeleton. The subject’s RPE while using the exoskeleton decreased compared to not wearing the exoskeleton. Table 2 has the results of the box and blocks trials along with the RPE for each trial. Table 3 has the normalized flexor and extensor activation during the box and blocks trials. The subject had greater extensor activation in his affected arm while using the exoskeleton compared to his affected hand without the exoskeleton and a less amount of flexor activation while using the exoskeleton compared to using his affected hand without the exoskeleton. Table 4 contains the survey results from the QUEST and Table 5 contains the results from the SUS. The subject gave the exoskeleton an overall average score of 4 with the QUEST survey and an overall score of 90 with the SUS.
Table 2.
Mean number of blocks moved and RPE of the affected hand during the box and blocks trials
| Number of Blocks Moved | Rate Perceived Exertion (RPE) | |||
|---|---|---|---|---|
| Trial Number | With Exoskeleton | Without Exoskeleton | With Exoskeleton | Without Exoskeleton |
| 1 | 10 | 4 | 4 | 8 |
| 2 | 10 | 6 | 5 | 8 |
| M | 10 | 5 | 4.5 | 8 |
Table 3.
Mean normalized EMG flexor and extensor activation of the affected hand during the box and block trials
| EMG Flexor (%) | EMG Extensor (%) | |||
|---|---|---|---|---|
| Trial Number | With Exoskeleton | Without Exoskeleton | With Exoskeleton | Without Exoskeleton |
| 1 | 26.62 | 35.54 | 21.37 | 19.07 |
| 2 | 31.92 | 29.98 | 56.81 | 21.40 |
| M | 29.27 | 32.76 | 39.09 | 20.24 |
Table 4.
Results from the Quebec User Evaluation of Satisfaction with assistive Technology (QUEST)
| Items How satisfied are you with: |
Score |
|---|---|
| Dimensions (size, height, length, width) | 4 |
| Weight | 4 |
| Adjustments (fixing, fastening) | 4 |
| Safety (secure) | 5 |
| Durability (endurance, resistance to wear) | 5 |
| Ease of Use | 4 |
| Comfort | 3 |
| Effectiveness (the degree to which your device meets your needs) | 3 |
| Average Device Satisfaction | 4 |
1 = not satisfied at all, 2 = not very satisfied,
3 = more or less satisfied, 4 = quite satisfied,
5 = very satisfied.
Table 5.
The results from the System Usability Scale (SUS)
| Items | Score |
|---|---|
| 1. I think that I would like to use this device frequently | 4 |
| 2. I found the device unnecessarily complex | 1 |
| 3. I thought the device was easy to use | 4 |
| 4. I think that I would need the support of a technical person to be able to use this device | 1 |
| 5. I found the various functions in this device were well integrated | 5 |
| 6. I thought there was too much inconsistency in this device | 1 |
| 7. I would imagine that most people learn to use this device very quickly | 5 |
| 8. I found the device very awkward to use | 1 |
| 9. I felt very confident using the device | 3 |
| 10. I needed to learn a lot of things before I could get going with this device | 1 |
Five-point Likert scale with 1 = Strongly Disagree and 5 = Strongly Agree
Discussion
The goal of this study was to evaluate the functional and neuromuscular effects of the 3D printed exoskeleton. The 3D printed exoskeleton was tested on a 67-year-old participant with stroke. During the first functionality test, the FMA, the subject was unable to perform any of the tasks without the exoskeleton. While wearing the exoskeleton, the subject improved in flexion, extension, and successfully performed three out of the four different grasps. Based on these results, the subject would increase the number of activities of daily living he could perform with his affected right hand if he wore the exoskeleton.
The subject successfully moved blocks with his affected right hand while wearing the exoskeleton and when not wearing the exoskeleton. During the two trials, the subject doubled the number of average blocks moved with the exoskeleton compared to not wearing it. While using the exoskeleton the subject successfully pinched the blocks between his index finger and thumb. Without the exoskeleton, the subject used a different mechanism to move the blocks. The subject was unable to extend his index finger to pinch the block with his thumb. Instead, the participant wedged each block between his thumb and index finger.
While using the exoskeleton the subject successfully pinched the blocks between his index finger and thumb resembling a normal pincer grasp. Without the exoskeleton, the subject used two compensatory grasping strategies including ulnar grasping and wedging the blocks between fingers. The subject was unable to extend his index finger to pinch the block with his index and thumb. Thus, the use of ulnar grasping and wedging blocks between his thumb and index fingers allowed the participant to grab several blocks. The subject was unsuccessful at using these grasping strategies for the specific tasks of the FMA due to the different object dimensions.
The passive exoskeleton had finger enclosures that did not allow the user to have any proprioceptive feedback when picking up the blocks. This may have inhibited the ability to feel where the blocks were and require the user to see where he placed his hand to pick up a block. In a test that requires speed, this can slow down and diminish the number of blocks moved in a minute. A future design alteration would be to create slits or holes in the finger enclosures of the exoskeleton to allow for feeling when reaching for items.
A finger splint may be able to improve the patient’s dexterity allowing a pincer grasp during the box and block test, however some activities of daily living may require dexterity of all fingers to perform different gasping patterns. The hand exoskeleton was able to assist the user in a variety of grasps during the FMA, something a simple finger splint may not have been able to accomplish.
During the Box and Blocks test, the subject’s normalized EMG extensor activation was larger while using the exoskeleton compared to not using the exoskeleton. This could be interpreted as the subject attempting to open his hand while wearing the exoskeleton. The assistance from the tension in the cables may have countered the spasticity enough to allow for the subject to use his extensors and attain some extension with his fingers.
The reported RPE scores were lower when using the exoskeleton compared to not using the exoskeleton. The participant with stroke was more inefficient without the exoskeleton and was able to redirect that exertion to a more beneficial outcome when using the exoskeleton. While a higher amount of normalized activation was seen in the extensor with the exoskeleton, the exertion may have been perceived as less due to the more positive outcome in the Box and Blocks test while wearing the exoskeleton.
Lowering the amount of exertion required to grasp objects can allow for more hand movements throughout the day for individuals who wear the exoskeleton without becoming fatigued. This increase in movements throughout the day could improve function. In addition to increasing the amount of repetitions, an exoskeleton that can increase function and be used in a home environment creates opportunities for the practice of activities of daily living (ADL). It has been suggested that activities incorporating variable movement, such as practicing grasping throughout the day, may be more beneficial than practicing single movements in a clinical setting[19].
Not only did the exoskeleton improve the functional outcomes of the stroke patient, it also received high scores from the QUEST and SUS survey. The QUEST survey resulted in an average score of 4 for the exoskeleton, which can be interpreted as “quite satisfied.” The SUS resulted in a score of 90, which can be interpreted as a letter grade of A or excellent[20]. The scores from the usability questionnaires show that the passive exoskeleton has the potential to be effective with additional individuals with stroke. Specifically, the exoskeleton scored well on dimensions, weight, and adjusting in the QUEST survey. This shows that the process of 3D printing an exoskeleton can be successful. Also, the design and production of the passive exoskeleton can be replicated for other subjects with stroke. The exoskeleton scored well in the QUEST on ease of use. Additionally, the exoskeleton scored well in the SUS on the exoskeleton’s ability to not need a technician present to assist the user. These scores show promise that the passive exoskeleton could be used in a home environment by the user on their own.
While the exoskeleton improved the function of the stroke subject in this study, there are large differences and variation seen in impairment and recovery after stroke. It is unclear if additional stroke survivors will improve in function with the 3D printed passive exoskeleton. For the future, we hope to continue to test the 3D printed exoskeleton on more subjects with chronic stroke. Additionally, bringing the subjects back in for a follow-up will be important for addressing possible increases in hand function after using the hand exoskeleton in their home environment.
Conclusion
The 3D printed passive hand exoskeleton improved the functionality of the affected hand of a participant with stroke. The extensor activation of the participant’s affected hand increased in activation during the Box and Block test, possibly showing the subject was attempting to extend his fingers. With the ability to be inexpensively 3D printed, the passive hand exoskeleton can be easily accessible to individuals with stroke. The usability questionnaires showed the 3D printed exoskeleton fit properly and has the potential to be used in the home setting of an individual with stroke. Future studies are needed to evaluate if the 3D printed passive hand exoskeleton can improve hand function in additional subjects with stroke.
Acknowledgements
We would like to thank the subject for participating in our study. We would like to thank all of the students who helped with the data collection at the Biomechanics Research Building at the University of Nebraska at Omaha. Additionally, we would like to thank Dr. Jim Brown for his support. Finally, thank you to Copper3D Inc. for donating the antimicrobial 3D printing filament for the construction of the hand exoskeleton.
Funding
This study was supported by the National Institutes of Health under grants (R15HD094194) and (P20GM109090), the GRACA/The Office of Research and Creative Activity at the University of Nebraska at Omaha, and the NASA Nebraska Space Grant.
Footnotes
Disclosure Statement
The authors report no conflict of interest.
References
- [1].Michielsen ME, Selles RW, Stam HJ, Ribbers GM, Bussmann JB. Quantifying nonuse in chronic stroke patients: a study into paretic, nonparetic, and bimanual upper-limb use in daily life. Arch Phys Med Rehabil 2012;93:1975–81. doi: 10.1016/j.apmr.2012.03.016. [DOI] [PubMed] [Google Scholar]
- [2].Nudo RJ. Recovery after brain injury: mechanisms and principles. Front Hum Neurosci 2013;7:1–14. doi: 10.3389/fnhum.2013.00887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Kamper DG, Fischer HC, Cruz EG, Rymer WZ. Weakness Is the Primary Contributor to Finger Impairment in Chronic Stroke. Arch Phys Med Rehabil 2006;87:1262–9. doi: 10.1016/j.apmr.2006.05.013. [DOI] [PubMed] [Google Scholar]
- [4].Cruz EG, Waldinger HC, Kamper DG. Kinetic and kinematic workspaces of the index finger following stroke. Brain 2005;128:1112–21. doi: 10.1093/brain/awh432. [DOI] [PubMed] [Google Scholar]
- [5].Kilbreath SL, Crosbie J, Canning CG, Lee MJ. Inter-limb coordination in bimanual reach-to-grasp following stroke. Disabil Rehabil 2006;28:1435–43. doi: 10.1080/09638280600638307. [DOI] [PubMed] [Google Scholar]
- [6].Jørgensen HS, Nakayama H, Raaschou HO, Vive-Larsen J, Støier M, Olsen TS. Outcome and time-course of recovery in stroke. Part I: Outcome. The Copenhagen Stroke Study. Arch Phys Med Rehabil 1995;76:399–405. doi: 10.1016/S0003-9993(95)80567-2. [DOI] [PubMed] [Google Scholar]
- [7].Oujamaa L, Relave I, Froger J, Mottet D, Pelissier JY. Rehabilitation of arm function after stroke. Literature review. Ann Phys Rehabil Med 2009;52:269–93. doi: 10.1016/j.rehab.2008.10.003. [DOI] [PubMed] [Google Scholar]
- [8].Duncan PW, Studenski S, Richards L, Gollub S, Lai SM, Reker D, et al. Randomized clinical trial of therapeutic exercise in subacute stroke. Stroke 2003;34:2173–80. doi: 10.1161/01.STR.0000083699.95351.F2. [DOI] [PubMed] [Google Scholar]
- [9].Paolucci S, Grasso MG, Antonucci G, Bragoni M, Troisi E, Morelli D, et al. Mobility status after inpatient stroke rehabilitation: 1-Year follow-up and prognostic factors. Arch Phys Med Rehabil 2001;82:2–8. doi: 10.1053/apmr.2001.18585. [DOI] [PubMed] [Google Scholar]
- [10].McConnell AC, Moioli RC, Brasil FL, Vallejo M, Corne DW, Vargas PA, et al. Robotic devices and brain-machine interfaces for hand rehabilitation post-stroke. J Rehabil Med 2017. doi: 10.2340/16501977-2229. [DOI] [PubMed] [Google Scholar]
- [11].Andriske L, Verikios D, Hitch D. Patient and therapist experiences of the saeboFlex: A pilot study. Occup Ther Int 2017;2017. doi: 10.1155/2017/5462078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Barry JG, Ross SA, Woehrle J. Therapy incorporating a dynamic wrist-hand orthosis versus manual assistance in chronic stroke: A pilot study. J Neurol Phys Ther 2012;36:17–24. doi: 10.1097/NPT.0b013e318246203e. [DOI] [PubMed] [Google Scholar]
- [13].Resnik L Development and testing of new upper-limb prosthetic devices: research designs for usability testing. J Rehabil Res Dev 2011;48:697–706. doi: 10.1682/JRRD.2010.03.0050. [DOI] [PubMed] [Google Scholar]
- [14].Mathiowetz V, Volland G, Kashman N, Weber K. Adult Norms for the Box and Block Test of Manual Dexterity. Am J Occup Ther 1985;39:386–91. doi: 10.5014/ajot.39.6.386. [DOI] [PubMed] [Google Scholar]
- [15].Desrosiers J, Bravo G, Hébert R, Dutil E, Mercier L. Validation of the Box and Block Test as a measure of dexterity of elderly people: reliability, validity, and norms studies. Arch Phys Med Rehabil 1994;75:751–5. [PubMed] [Google Scholar]
- [16].Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982;14:377–81. doi: 10.1249/00005768-198205000-00012. [DOI] [PubMed] [Google Scholar]
- [17].Brooke J SUS - A quick and dirty usability scale. Usability Eval Ind 1996;189:4–7. [Google Scholar]
- [18].Demers L, Weiss-Lambrouand R, Ska B. The Quebec User Evaluation of Satisfaction with Assistive Technology (Quest 2.0): An overview of recent progress. Technol Disabil 2002;14:101–5. doi: 10.13072/midss.298. [DOI] [Google Scholar]
- [19].Krakauer JW. Motor learning: its relevance to stroke recovery and neurorehabilitation. Curr Opin Neurol 2006;19:84–90. doi: 10.1097/01.wco.0000200544.29915.cc. [DOI] [PubMed] [Google Scholar]
- [20].Bangor A, Kortum PT, Miller JT. Determining What Individual SUS Scores Mean: Adding an Adjective Rating Scale. J Usability Stud 2009;4:114–23. [Google Scholar]