Abstract
Background
To increase the number of hours available for cognitive rehabilitation, it may be an option to use the spouse or paid assistants to assist with computerized home training. However, the delegation of training responsibilities may affect the normal roles of the therapist, the spouse and the training assistants.
Objective
This article suggests a new model for understanding the impact of computerized home training on the therapeutic alliance between the therapist, the patient and training assistants. Aspects of this knowledge are relevant also for the development and use of computerized training systems in clinical settings.
Method
Qualitative Interpretative Phenomenological Analysis (IPA) of semi-structured interviews was used to analyse the experience gained during home-based computerized cognitive training.
Results
Home-based computerized training enforces the delegation of aspects of the therapeutic alliance established between the therapist and the patient. The perceived authority of assistants and computer training systems may differ from the authority established through the patient/therapist alliance. Information may be lost in transition impacting skills and expertise long-term.
Conclusion
Roles and responsibilities between the therapist, the assistants and the computerized training system need to be clearly defined. A Cognitive Training Alliance model is being proposed which takes into consideration the challenges of delegating training responsibility to computer systems and non-professional assistants.
Keywords: Psychology, Clinical psychology, Spousal impact, The cognitive training alliance model, Home training, Caretaker involvement, Computer-based cognitive rehabilitation
Psychology; Clinical psychology; Spousal impact; The cognitive training alliance model; Home training; Caretaker involvement; Computer-based cognitive rehabilitation.
1. Introduction
The use of computer technology and systems are ubiquitous in healthcare administration today including purchasing, inventory management, resource planning, patient journaling and so forth. With the introduction of telemedicine, technological solutions are being introduced for clinical reporting, patient monitoring and even diagnosing [1, 2]. Direct interaction with doctors and nurses are being replaced by monitored self-care and assistance being delegated to remote professional and non-professional assistants. However, the delegation of responsibility in telemedicine from in-clinic care to remote or even home-care introduces new challenges for patients as roles and responsibilities are delegated to systems and non-professionals. In the US, the American Medical Association have recently concluded a survey on rules and regulation regarding patient-physician relationship in telemedicine at state level [3] demonstrating the need for general guidelines to protect patients. In the EU, projects like ICT4Life and C-MMD have been initiated to build standard integrated remote healthcare platforms for patients living with cognitive impairments such as dementia [4]. However, for both platforms, the focus will be mainly on monitoring and daily care and less on rehabilitation. In telemedicine, the observations of the effects of delegation of triage, consultancy, long-term monitoring and self-monitoring was reported in a study from North Italy [1]. The overall conclusion is that delegation of tasks to both professional and non-professional caregivers using telemedicine systems reveals the complexity capturing the essence of onsite caregiving in scripts and computer systems. It also questions the long-term effect on learning and expertise in the health sector.
Improved survival rates for patients with acquired brain injury as well as improved cognitive training procedures have increased the demand for cognitive rehabilitation training [5]. Modern models of cognitive rehabilitation embrace the plastic processes of the brain involved in relearning or recovery of cognitive function following brain injury [6, 7] and with that follows that cognitive rehabilitation training needs to be delivered frequently, intensively and with appropriate level of difficulty to have an effect [6]. Training often consists of sessions of 20–30 min repeated 2 times a day for 2-5 weeks as seen in neglect training [8, 9, 10].
Increasingly, rehabilitation clinics are embracing computer-based training as a means to accommodate the flexibility in schedules demanded by patients [11, 12, 13] and as an alternative way of increasing the much needed intensity without increasing the demand for therapists and cost to health service e.g. [14]. By installing the computerized training system in the patient's home and engaging the assistance of the patient's family or paid assistants, the patient is able to train basic cognitive skills at a time and place suited to his or her needs.
It has been demonstrated that with proper support from the family and next of kin, the family involvement in rehabilitation may actually improve the outcome of the rehabilitation process [15, 16]. Several studies have investigated and found positive effect of cognitive training in a home environment e.g. [17, [18], [19], [20]] on cognitive skills.
As in other areas of healthcare, placing the cognitive training system from in-clinic environment to the patient's home may come at a cost to the therapeutic alliance between the patient and therapist as some of the implicit training responsibilities are being delegated to either the computer system itself and/or the home training assistants. It increases the demand for self-adapting training systems that are able to respond to individual changes and progress made by the patients. It also raises the question of how the delegation will affect the expertise of therapists.
This article attempts to take it a step further looking at requirements for home-based computer training which needs to be included in considerations and regulation of remote healthcare services. It offers a suggestion for a new model for understanding the impact of computerized home training on the therapeutic alliance between the therapist, the patient and training assistants. The proposal is based on the author's years of experience with computerized cognitive training as well as data from a new case study investigating the impact of the training on the spousal relationship. Aspects of the new model are relevant also for the use of computerized training in clinical settings.
Firstly, the study leading to the crystallization of the elements of the model will be presented and secondly the model itself will be presented.
2. The model
2.1. The therapeutic alliance
Most treatment and therapy in psychological terms requires an alliance between the patient and the therapist, the patients being the person with a problem and the therapist being the expert within a field of solutions [21]. The concept of the therapeutic alliance originates from the psychoanalytic literature in which the alliance is defined as the pact of a common goal based on the demands and wishes of the patients [19, 21] suggesting that in psychotherapy, an important skill of a therapist is to create a common ground for change and improvement. The difference in outcome of therapy may be related to: 1) the therapy or intervention used, 2) the experience level of the therapist, 3) the personal qualities and professional social skills demonstrated by the therapist [22]. It is important for the outcome to establish an alliance in which the patient feels comfortable with the therapist and trust the therapist's expertise [23]. Cognitive computerized training is a long way from psychotherapy but as pointed out by Bordin [21], many training relationships share features of the working alliance.
2.2. The generic model of psychotherapy
In the generic model of psychotherapy (GMP) [24], a range of variables defines the process of change. Although the model is presented in a specific therapeutic context, the suggestion here is that the main construct variables may be said to be true for therapeutic processes in a broader perspective. The GMP defines input, process and output variables for change. The actors are the patient and the therapist and the social and cultural environment in which their meeting is set is defined as the input variables. The process variables define everything that occurs during the course of the treatment such as the type of therapy activities. The output variables define the consequences or effect of the therapeutic intervention, not only in the patient but also in the therapist and the environments.
2.3. The cognitive training alliance
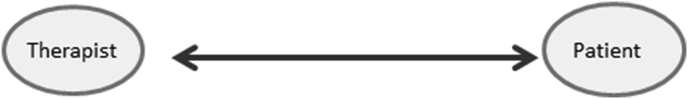
In cognitive rehabilitation training, the patient is joining a range of therapeutic relationships between different professionals involved in the rehabilitation and training of neuropsychological and physical deficit following brain injury. In each case, the patient forms a therapeutic relationship, teaming up with the professional to obtain improvements. The alliance between the therapist and the patient relies on trust in the therapist devising a sequence of activities and exercises which will improve the current state of patient ability. The patient has to perform the activities in the right manner following an appropriate schedule. The therapeutic alliance for cognitive training between a patient and a therapist may be illustrated simply by two entities joined by a to-way arrow indicating the elements in cognitive training alliance under normal circumstances (Figure 1).
Figure 1.
The basic cognitive training alliance (CTA). The therapist plans and executes the training and is in total control of all aspects of training. This is the most common clinical structure.
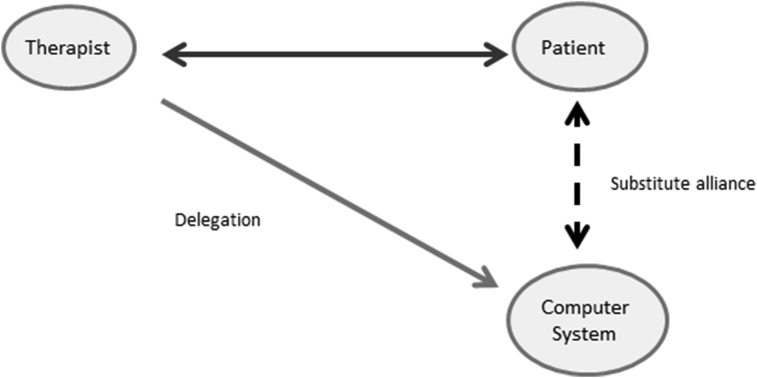
When a therapist chose to use computerized cognitive training, the CTA may be said to be extended to include the computer system (Figure 2) as an actor. The training expertise is now shared between the computer program and the therapist. The therapist is introducing the computer training into the alliance. The patient must keep faith in this shared alliance constituted by the two to provide adequate and timely training. The training programs need to provide appropriate progress and adequate feedback for the patient to stay motivated, understand progress and adjust behavior. Most computerized training systems available today are not able to adjust to the individual progress of a patient automatically. Even so, the patient must establish a substitute alliance (indicated by the stabled line between the patient and the computer system) with the computerized system and trust that the system will move forward in a suitable fashion.
Figure 2.
The computerized cognitive training alliance. The therapist plans the training but part of the execution is delegated to a computer program which may or may not be highly sophisticated in terms of control of progress, feedback and content of training. The patient has to form a temporary substitute alliance with the system. Training is still taking place at the clinic.
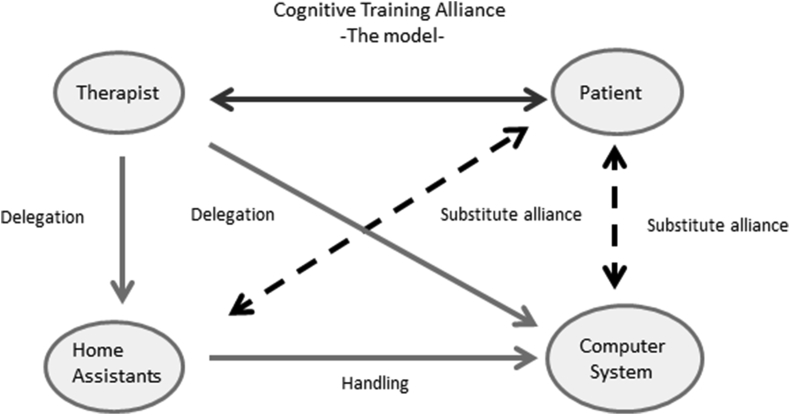
When the training system moves from the clinic into the home of the patient and non-therapist helpers assist with the control and execution of training, the therapeutic alliance may need to embrace human substitutes for further areas of the alliance. To embrace this complexity, the Cognitive Training Alliance model extends the therapeutic alliance further taking into consideration that the parts of the therapist's domain may be substituted by computer and helpers (Figure 3).
Figure 3.
The Home-based Computerized Cognitive Training Alliance model. The computer training system is now moved further away from the therapist. Daily supervision is delegated to the spouse or paid helpers who must have ways of providing feedback or seek assistance from the therapist.
In this case, the CTA is extended further to include equipment and helpers and it becomes even more important to clearly communicate which aspects are being delegated and roles and responsibilities clearly stated.
3. The home training study
3.1. The case
In 2013, NN (75 YO) falls down a flight of stairs and subsequent scanning of the brain revealed injury to the right hemisphere, particularly to the parietal and temporal lobes. Prior to the fall, NN had a history of several smaller cardiovascular incidents but was working full time at the time of the accident. After 4 months in hospital, NN was released with severe unilateral visual neglect, neglect dyslexia, prosopagnosia, achromatopsia, agnosia and other perceptual difficulties as well as left-sided hemiparesis. He was unable to walk but was able to communicate coherently and intelligently.
After an initial cognitive assessment, a plan was put together targeting the visual neglect and neglect dyslexia through intensive computerized training. To achieve the necessary intensity and flexibility, it was decided to conduct the cognitive training in NN's home using a tailored combination of computerized training system matching NN's deficits.
NN had no prior experience with the use of computers and was totally dependent on the assistance from others to start up the computer and to navigate through the software. The visual problems made it impossible for him to follow written instructions.
The therapist taught the spouse and the assistants how to operate the equipment and initiate the programs for training. The therapist also provided detailed written instructions for the tasks and all assistants were required to log and timestamp all activities and problems encountered.
Once a week, the therapist would visit NN and assess progression. The training would be adjusted and the therapist would demonstrate new activities and supervise NN and assistants in how to do the exercises properly.
The 4 months of training had a significant and positive effect on NN's ability to cope with the visual problems and the final and follow up assessments showed improvements in visuo-motor tasks such as line bisection and in perceptual processing speed. The results have been described in detail in Wilms [25].
3.2. The follow-up on the home training experience
As this was one of the longest periods of home training tested in a home study by the author, a follow up interview was conducted with the spouse, the assistants and NN to investigate how training at home for such a long period, had impacted the family relationship.
3.3. Data collection
NN and the spouse were interviewed independently at home a month after the completion of the 4 months training regimen. Using semi-structured interviews with a combination of closed and open questions, the interviews lasted for approx. 45 minutes each. This approach was selected to ensure that both interviews touched the same subjects while allowing for free commenting by NN and the spouse within the framework of the questions.
The semi-structured interview was divided into three parts, one investigating how NN and the spouse felt about computer-based home training, one where the spouse and NN were interrogated about training and assistance and finally one, where the training itself were rated. NN and the spouse were asked to rate level of difficulty, level of frustration and perceived training effect. Both interviews were taped on a digital recorder and later transcribed ad verbatim. An interpretive phenomenological analysis (IPA) was done on the transcribed data.
3.4. Ethical considerations
NN and the spouse gave full written and informed consent to the use and publication of the data in this study. Ethical approval was obtained from The Institutional Ethical Review Board, Department of Psychology, University of Copenhagen, has reviewed and approved the project, approval no IP-IRB/11112019.
3.5. IPA
IPA is a qualitative research method that is rooted in the phenomenological objective to understand the specific, the personal and the subjective experience of phenomena [26, 27]. The most common data source is the result from semi-structured interviews [28]. In IPA, the process of interpretation of data follows a methodological procedure which allows for a systematic approach to extracting the individual experience through interpretation of the transcribed text. The method is rooted in the hermeneutic tradition which is the study of interpretation of text [27, 28]. Kvale [28] explains the “hermeneutic circle” which requires the continuous back and forth between the parts and the whole of the text facilitating a deepened understanding of it until a “good gestalt” is reached. The good gestalt is described by Kvale [28] as “...an inner unity of the text free of logical contradictions”. In this study, the practical guidance for designing, conducting and analyzing the IPA part of the study was borrowed from Smith et al. [26] and Willig [27]. The method requires the reading and re-reading of text and the researcher to immerse in the text to get a deeper understanding of what is being said. Once the text is understood in its parts, the researcher is to identify patterns and recurring themes that when clustered describe the overall experience of the phenomena by the respondent during the process.
The IPA results have been structured into in a selection of superordinate themes each containing a number of subordinate themes emerging from the data available.
3.6. Preparation for training
A separate corner of NN's living room was screened off from the rest and white sheets were covering the nearby walls and windows to reduce the visual and attentional noise. A touch monitor was placed on a large table on an adjustable arm allowing optimal positioning for each of the different types of training systems. The table was wide and high enough to allow NN to sit comfortable in his wheelchair. A chin rest was borrowed from the department of Psychology and used to restrain head movements when required.
3.7. The training schedule
The cognitive training consisted of several different types of computer-based training including training on an iPad (see Table 1). Each type of training targeted different aspects of NN's visual and attentional impairments.
Table 1.
The test and training schedule.
| Type | Period | Intensity | Equipment |
|---|---|---|---|
| Test 1 | |||
| Prism Adaptation Training | 2 weeks | 2 × 30 min, daily | PC, Win7. Authors own software and equipment |
| Test 2 | |||
| Prism Adaptation Training | 1 week | 1 × 30 min, daily | PC, Win7. Authors own software and equipment |
| Optokinetic training 1 | 3 weeks | 45 min, daily | PC, Win7. EyeMove purchased from MedCom |
| Test 3 | |||
| Optokinetic training 2 | Ongoing | 45 min, daily | PC, Win7. EyeMove purchased from MedCom |
| Visual attention training | 4 weeks | 15 min, daily | iPad App “Visual Attention Therapy” available from iTunes |
| Afasi-assistant: object determination | 4 weeks | 20 min, daily | PC, Win7. Afasi-assistant customized. Purchased from COGNIsoft |
| Test 4 | |||
| 8 weeks | No training | ||
| Test 5 | The final follow-up test |
The Prism Adaptation Training was a computerized version of the standard adaptation to prism induced bias in visual input [29]. The prism training software was originally developed by the author and had been used for several years at the Center for Rehabilitation of Brain Injury. The Optokinetic training used the EyeMove [30] software from the company MedCom Verlag. EyeMove training targets the oculo-motoric system. The Visual Attention Therapy [31] app was purchased on iTunes from the company TactusTherapy. Afasi-assistant [32] was developed by the company COGNIsoft and a copy was borrowed from the author as part of the research project.
3.8. The role of the assistants
The first session of a new exercise was always conducted by the therapist to ensure that NN was able to perform the tasks and that the level of difficulty was appropriate. This was determined through interviews, tests and observations. The therapist (the author) would adjust parameters in the training software accordingly. The home training assistants were then taught how to assist before and during the exercise. They conducted one training session with NN under the supervision of the therapist before passing on the responsibility for the exercise to assistants.
The role of the assistants would wary from exercise to exercise but essentially it was to turn on the equipment, load the software programs and select the appropriate exercise for the day. For the prism and oculo-motor exercises, assistants would ensure correct positioning in a chin rest as well as correct pointing speed.
3.9. Formal consent
Both NN and the spouse have consented in writing to the use of the data in this article.
4. The IPA analysis of the interview with NN and the spouse
The following analysis has been limited to focus on elements related to the interpersonal experience of home training. More specific technological issues will be addressed in a later article.
For this article, only the following three emerging superordinate themes will be analyzed in the following section:
-
•
Superordinate theme 1: The marital impact
-
•
Superordinate theme 2: The spouse and home assistants as teachers
-
•
Superordinate theme 3: Skills of a good assistant
4.1. Superordinate theme 1: the marital impact
This theme deals with how assisting in the home training influenced the spousal relationship. It is well known spousal relationship may suffer or change as a results of brain injury in one party [33]. The therapist observed that turning over the daily responsibility for the training to the spouse and paid assistants created a certain amount of conflicts and tension between patient and the assistants. Some of these problems were uniquely related to the relationship with the spouse and are therefore handled here separately.
In general, the spouse was very positive towards the daily schedule introduced by the training. She found that it introduced a structure of the day similar to that of a regular working day. It provided both of them a sense of purpose and a feeling of contributing to the recovery of NN.
In many brain injury cases, the spouse becomes the primary caretaker and is forced by circumstance to act as a nurse [34] which may lead to depression and burn-out. In this study, the spouse took great comfort in being an active part in activities aimed at improving the cognitive state of the husband rather than just being a “nurse”. She found the exercises fun and the role as an assistant gave her an opportunity to follow the progress of NN more closely than in a normal clinical setting.
It is well-known that brain injury affects not only the patient but also the relationship between to the spouses [35, 36, 37]. Both NN and the spouse were very positive towards computer-based training and for the opportunity boost training sessions.
Quite quickly after the initiation of the home training, NN himself began humorously to refer to the training equipment as the “divorce equipment”, a notion supported by the wife. Although they were both in full support of the home training and were satisfied with the results, they also recognized that conflicts occurred as a result of the changes in roles induced by the training responsibility. They both raised several issues that would be causing problems.
NN and his spouse were both very concerned about “wasting valuable time” or doing something wrong that would render the training inefficient. They both tried to follow the written and oral instructions to the letter. However, in brain injury training, the patient is not always able to do a task 100% correctly even at a slow pace. In a clinical setting, the therapist will make allowances for this based on the severity of the deficit and the show of progress.
In many cases the spouse had understood the exercises correctly but pride and lack of insight on the part of NN would make it hard for the spouse to convince him. The spouse felt that her role was not only to assist with the manipulation of the machinery and the software but also to supervise that training was done correctly. This was never explicitly stated by the therapist and was never intended either. Somehow it became implicitly implied in the way the instructions were provided to the spouse and helpers confusing the roles of delegation.
NN, however, did not accept this change in role. The spouse said:
“If I asked him to keep his head still (important for one of the exercises), he would be furious. He took every comment as being patronizing and I can fully relate to that… but it is not something that can be changed now I think…..”
NN stated his frustration this way:
“All discussions now ended with a feeling that she knew better. It is hard to control ones temper. If it is a nurse that asks you to do menial tasks, it is ok, but if the wife does it, then we get into trouble…Using the spouse as a trainer is risky business. It is terrible when you direct your frustration toward the spouse. I have a spouse that does a tremendous job assisting me, but it also gives me a feeling that she decides everything”.
At times, the spouse expressed concerns about feeling overwhelmed by the frustration and irritation exhibited by NN during training. They would be listening to instructions from the therapist together, but understand them differently.
On one hand, she understood his frustration but the role of assistant prevented her from just listening and soothing. She felt responsible for enforcing the training regimen the way she understood it to be:
“When you had explained something to me and NN, we sometimes understood your instructions differently. When I tried to guide him, he sometimes exploded in anger”.
The spouse acting as both eyes and hands were accepted by NN but the spouse acting as a trainer was not and was in conflict with the spousal role as comforter and supporter. Indirectly, this perceived lack of support may very well have been felt by NN as lack of understanding and empathy and even love at times.
Clearly, NN felt bothered by the shift in role and his frustration may be interpreted as well from the standpoint that the temporary role of the spouse as teacher shifted the balance of respect and perhaps dominance between the spouses.
When asked how this might be ameliorated in the future, NN said:
“There is no easy way to resolve it. It can only be done with tolerance and communication and a common feeling that we are doing this together”.
Using the CTA model (Figure 3), the therapist delegated the responsibility of operating the computer system to the spouse and assistants but failed to assist the patient in forming a new substitute alliance with the assistants. The training system itself was not programmed to actively correct the patients speed or posture directly. The substitute alliance between patient and computer was for this reason weak. One way to avoid an inter-role conflict would have been may be to firmly state the roles of the spouse as assistant rather than as a therapist firmly stated. If the spouse and patient see the training as a joint effort rather than a therapist-pupil effort, it may promote less conflict and more shared encouragement and support.
NN and the spouse felt comforted by the fact that we met once a week and over time, the spouse would learn to be less concerned about minor details and correct only when really necessary. That way the amount of grievance and pressure on the relationship decreased. The spouse said:
“Overall, home training worked well. Initially, we had some difficulties and adjustments to do, but over time I learned to ignore the irritation and be more sensitive to how he wanted to be instructed when he did something wrong”.
The spouse fully supported the activities that she and her husband endured throughout the training months. She provided additional and valuable insight into the difficulties facing NN during the training and felt grateful of the opportunity for active participation in activities improving the NN's abilities. She stayed empathetic to the annoyance and frustration of NN whenever he failed to achieve his goal as fast as he had hoped.
In summary, the first theme indicates that engaging the spouse as an assistant in cognitive training of deficits works. However, it briefly changes the role of the spouse from being a caretaker and unconditional supporter to being actively involved in the correct execution of training and the recovery of the patient. NN was well aware of his dependency on the spouse in activities of daily living at a rational level and grateful for her support but he felt annoyed about this dependency and this annoyance was exacerbated by her role in the training. For both NN and her, the best solution would probably have been to rely on paid assistants solely but this is also very expensive even short-term.
To avoid conflicts, it is important to ensure that the role and obligations of the spouse is clearly defined in relation to how training should be executed. Also, the spouse needs to know what to expect in terms of training progress when dealing with brain injury and should be encouraged to call for support if in any doubt. It should be clearly stated that the responsible teacher is the therapist.
4.2. Superordinate theme 2: the spouse and home assistants as teachers
NN had employed paid assistants to assist home with work and daily activities unrelated to the training. On his suggestion, the assistants were taught to initiate the different steps of the training when the spouse was unavailable. However, NN would respond very negatively to comments, adjustments and even help from assistants even though he understood that they were substituting for the therapist and the spouse during the week. He felt patronized when offered assistance and encouragement and was generally annoyed if the assistants did anything apart from operating the equipment. This was true when the spouse assisted but even more so when the paid assistants were assisting with the exercises. NN said:
“I was more annoyed with the assistants and especially when they stood and looked over my shoulder to follow what I did. It felt like a child watching Dad play. I hated that”.
NN pointed out several times that he felt that it would have improved the relationship between helpers and him if they had known their role to be instructors not helpers.
“Assistants and the wife must be instructed to be more invisible and not meddle or interfere and not comment…() Good assistants are somebody who only controls the technical functions such as starting the equipment and adjusting your chair”.
When asked to elaborate, NN said:
“In my view help is annoying. Fundamentally, help is annoying..() You get sensitive to peoples interference when you are forced to do things (and cannot do them) that you previously did without thinking”.
“There is a difference between instruction and help. I get furious when they help…()..As an example, when a guy sets up a radio, he is responsible for making sure the radio is set correctly to produce the best sound. He should not comment on my hearing ability”
NN and the spouse were asked to identify what in their view qualifies a good assistant. NN himself said the following:
“I feel that it is important that assistants are told not to help unless asked. Preferably, they are my hands and eyes but not my brain”.
Another area of contention which was more difficult to handle for the helpers was the fluctuations between hope and despair in NN. Initially, helpers were encouraged to commend NN when he did the tasks correctly or reached a target set for the day. We had to change that practice when it turned out that NN felt patronized.
Sometimes NN did not seem to have full insight into own ability and would lie about them. The spouse said:
“He lied about his abilities in the beginning. When he was browsing in book, I would ask him if he recognized any of the objects and he would say yes. When asked to name one, he would refuse”.
A therapist may interpret this behavior in at least two different ways. One might be the anosognosia accompanying neglect that prevents patients from realizing the full extent of their injury afflicted difficulties [38]. Another possibility might be that the patient is trying to cover up the lack of ability to retain the respect of the spouse and helpers or even his own self-respect. In either case, it is important for assistants to react respectfully and just report what they observe to the therapist.
NN was always courteous and polite and able to see things from a humorous angle when he failed when together with the therapist. One explanation might be that NN referred to an implicit hierarchy of validity and knowledge with the therapist at top, NN himself second and helpers at the bottom. Corrections and supervision would then be regarded as undermining his authority. Differences in explicit and implicit structures of authority is known to create tension and conflicts [39]. Another more sensitive aspect is the perceived loss of dignity from failing in simple tasks in front of family and assistants. In a therapeutic environment, this loss of dignity is part of the work to get better and you are with peers. When training moves into the home of the patient, the impact of the injury becomes apparent at a basic level to all around you.
Although all instructions were accompanied by detailed scripts and an introduction to the purpose of the training, it was clear that training aiming at improving basic cognitive components of attention can be very difficult to understand and self-adjust to. In the future, it is important also to discuss the level and type of feedback provided to the patient from helpers.
4.3. Superordinate theme 3: skills of a good assistant
In this theme, the analysis touches upon the skills and characterization of a good training assistant in relation to computerized training. Therapy has traditionally been carried out by trained clinicians in a clinical environment. In a clinical environment, assistants are under constant supervision to conduct the training in an adequate pace and level of difficulty to fit the patient's progress and endurance. When introducing computerized training, the therapist loses the knowledge resulting from close interaction with the patient. Good training software will monitor the progress of the patient and provide adequate tools for reporting and adjusting the training as the patient improves. Excellent training software will recognize that responsibility has been delegated on the part of the therapist and will automatically adjust training and provide neutral feedback to the patient during training e.g. [40, 41].
Introducing computer-based systems in cognitive training changes the role of the therapist and to some extent reduces the need for constant supervision of the patients’ progress as this in theory is done by the computer system. This frees up senior therapy resources but it also introduces the problem of recruiting and organizing alternative training assistants. Professionals from different professions may have to share the task of conducting training and less skilled professionals may be called upon to watch and supervise the training as the systems become more and more advanced and self-reliant. It is therefore important to understand the skills required by the personnel used in the clinics or at home.
The spouse was asked whether it would have been an advantage that the therapist more specifically had stated the roles and responsibility of the assistants. In her view, that could easily have come across as patronizing too. She would have felt uncomfortable. To her, it is important to prepare the assistants for the emotional state of the patient and how corrections and assistance may be regarded as patronizing or demoralizing.
She felt strongly that brain injury affects the family and that as a couple you need to work together to adjust to the new situation. She felt less sure that the wife is the ideal assistant as she is too emotionally involved. Again this reflects on the change in marital relationship that brain injury often entails. From being equal partners, the spouse also becomes the primary caretaker. When introducing home training, it introduces the third role as teacher/instructor as well. The three-way inter-role state as a wife, a nurse and teacher stretched the resources of the wife and makes the relationship vulnerable to conflicts.
When asked about the qualifications needed by a good assistant, the spouse said:
“The assistant has to be patient….you have to be able to cope with anger and frustration without feeling personally attacked…. And be able to discuss with the patient the best way to providing encouragement and corrections to avoid conflict”.
The role of the assistant in motivating the patient was not discussed directly as NN was highly motivated and insistent in following the daily schedule. However, the assistants need to know when to encourage the patient to follow the instructions and when to let go. One said:
“You told me at one point that it was a difficult task and that I could not expect him to do it correctly. The point was to do the best he could”.
“Over time, I came to realize that the training had an effect even though it was not done perfectly every time and to give him some slack….I need to be there if he needs help and to correct a thing or two and let it go if he gets upset”.
NN expressed his view on the qualifications of a good assistant like this:
“Good basic chemistry is important. Young people (referring to the assistants) tend to be condescending in their way to speak and that annoys me….. It is important to feel that we have a common goal”.
When asked about the difference between the spouse and the paid assistants he described it like this:
“I was more annoyed with the assistants than the spouse, especially when they stood next to me and observed”.
When asked how assistants needed to be instructed, NN said:
“They have to be told to instruct [in the use of the system] not help. When doing a cognitive task, they would say ‘Can't you see it has horns?’ because it was a cow or something. Then I would tell them to shut up….. Help is annoying when not asked for!”
“Good assistants are someone who controls the system, starts it up, adjusts your chair and ensure the thing works [the PC]…. It requires much psychological insight to intervene so when they change from instruction to assistance it becomes lethal”.
In summary, the assistants need to know about the variability in performance and moods that is normal to brain injury rehabilitation. The more the patient relies on assistance to operate the equipment and software, the more the assistants have to be skilled in how to deal with the psychological issues arising from suffering from brain injury.
Computerized training systems to be used in a home environment need to be able to monitor progress, provide ample feedback to the patient and the therapists and self-adjust to progress or lack of it.
5. Discussion
5.1. CTA in the current case
In the case described in this article, a substitute alliance was established between the spouse and NN, but this alliance was unclear in the definition of goals, activities and roles. NN did not trust the expertise of the spouse and helpers and reacted against their attempts to assist with and guide the training.
The CTA continued to exist between the therapist and NN who had complete trust in her instructions and selections. However, it was also clear that it was difficult to establish a teaching or training alliance between NN and the home assistants. NN never accepted the shift in roles. He sought out his wife for comfort, planning and assistance in many other aspects of his life due to the injury and fully accepted her role as a nurse but he never accepted her role as instructor. The therapist might have been able to alleviate some of the tension with clearly stated roles and responsibilities.
In retrospect, both the spouse and NN pointed out that it was important to prepare home assistants to this difference in role. They were not regarded as therapists but as subordinate to NN's actions. Originally, the therapist had thought that encouragement and positive acknowledgement of progress from home assistants would be valuable but it turned out to the one of the major grounds for conflict and irritation. Another point of conflict was the difference in perception of the instructions provided. The training was planned and initiated each week with a demonstration for the NN and if needed, training for the home assistants. However, after the therapist had left there would be difference of opinion as how the exercises needed to be conducted despite scripts and instructions. In hindsight, the instruction and level of attention to detail should have been even more clearly defined.
It becomes important that the therapist is very clear and specific about the roles played by the assistants and to what extent, they substitute the therapist. In this case, the roles became unclear much to the frustration of NN and the home assistants.
6. Conclusion
Therapists working with cognitive rehabilitation training form a cognitive training alliance with their patients. The alliance is the mutual agreement to work together to improve quality of life including the ability to handle activities of daily living. Roles and responsibilities are implicitly and explicitly defined through direct conversation and a plan set for activities to achieve predefined goals.
Moving the computer equipment into the home of a patient expands the actors in the therapeutic alliance to include family member, friends or paid assistants and the computer system. The therapist must ensure that the alliance stays intact. Even when the patient is familiar with the computer system from the clinic, the use and roles of supporting family members and paid assistants need to be clearly defined to avoid conflict and maintain knowledge across actors.
Previously, the therapist would be the primary supervisor and controller of the training progress and would adjust training according to the patient's ability and progress. With the introduction of computerized cognitive rehabilitation training systems, part of the responsibility for monitoring and adjustments are being delegated to computer systems or to people with no prior knowledge in cognitive rehabilitation.
With the delegation, the therapist loose access to direct information and feedback from interacting with the patient. It befalls assistants or the computer system itself to monitor and control the training and provide adequate feedback to the therapist. Even when the patient is familiar with the system from the clinic, the use and roles of supporting family members, paid assistants and the computer system need to be clearly defined to ensure proper patients care and avoid conflict.
To do so, the therapist has to be aware what aspects of the alliance is being delegated and be able to explicate knowledge that in many cases would be considered implicit expert knowledge. Monitoring and control activities have to be carefully scripted and the training systems have to be sensitive to change and progress in patient ability. It will be important to convey to software developers of cognitive training aimed for home training, that remote use require adaptation and feedback mechanisms for the patient as well as the responsible therapist.
The proposed Cognitive Training Alliance model (Figure 3) can be used to understand how the introduction of computerized home-based training may affect the alliance and to what extend procedures have to be implemented remotely either through instruction to care givers or by the use of advanced algorithmic control of the software systems. It may share similar traits to telemedicine but the actions and impact may differ.
Declarations
Author contribution statement
I. Wilms: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This work was supported by The Danish Council for Independent Research, Communication and Culture, Denmark (Grant # 12-132029).
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Nicolini D. The work to make telemedicine work: a social and articulative view. Soc. Sci. Med. 2006;62(11):2754–2767. doi: 10.1016/j.socscimed.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Sneha S., Varshney U. Enabling ubiquitous patient monitoring: model, decision protocols, opportunities and challenges. Decis. Support Syst. 2009;46(3):606–619. [Google Scholar]
- 3.Association A.M. 50-state survey: establishment of a patient-physician relationship via telemedicine. 2018. https://www.ama-assn.org/system/files/2018-10/ama-chart-telemedicine-patient-physician-relationship.pdf Available from:
- 4.Solachidis V. Proceedings of the 11th PErvasive Technologies Related to Assistive Environments Conference. ACM; 2018. Two examples of online eHealth platforms for supporting people living with cognitive impairments and their caregivers. [Google Scholar]
- 5.Cicerone K.D. Evidence-based cognitive rehabilitation: updated review of the literature from 2003 through 2008. Arch. Phys. Med. Rehabil. 2011:92. doi: 10.1016/j.apmr.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 6.Kleim J.A., Jones T.A. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J. Speech Lang. Hear. Res. 2008;51(1):S225–S239. doi: 10.1044/1092-4388(2008/018). [DOI] [PubMed] [Google Scholar]
- 7.Mogensen J. Reorganization of the injured brain: implications for studies of the neural substrate of cognition. Front. Psychol. 2011;2 doi: 10.3389/fpsyg.2011.00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kerkhoff G. Repetitive optokinetic stimulation induces lasting recovery from visual neglect. Restor. Neurol. Neurosci. 2006;24(4-6):357–369. [PubMed] [Google Scholar]
- 9.Kerkhoff G., Rossetti Y. Plasticity in spatial neglect - recovery and rehabilitation. Restor. Neurol. Neurosci. 2006;24(4-6):201–206. [PubMed] [Google Scholar]
- 10.Kerkhoff G., Schenk T. Rehabilitation of neglect: an update. Neuropsychologia. 2012;50(6):1072–1079. doi: 10.1016/j.neuropsychologia.2012.01.024. [DOI] [PubMed] [Google Scholar]
- 11.Tedim Cruz V. Web-based cognitive training: patient adherence and intensity of treatment in an outpatient memory clinic. J. Med. Internet Res. 2014;16(5):e122. doi: 10.2196/jmir.3377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cogollor J.M. Evolution of cognitive rehabilitation after stroke from traditional techniques to smart and personalized home-based information and communication technology systems: literature review. JMIR Rehabil. Assist. Technol. 2018;5(1):e4. doi: 10.2196/rehab.8548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van de Ven R.M. Computer-based cognitive training for executive functions after stroke: a systematic review. Front. Hum. Neurosci. 2016;10:150. doi: 10.3389/fnhum.2016.00150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stuifbergen A. Home-based computer-assisted cognitive training: feasibility and perceptions of people with multiple sclerosis. Int. J. MS Care. 2011;13(4):189–198. doi: 10.7224/1537-2073-13.4.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Foster A.M. Encouraging family engagement in the rehabilitation process: a rehabilitation provider's development of support strategies for family members of people with traumatic brain injury. Disabil. Rehabil. 2012;34(22):1855–1862. doi: 10.3109/09638288.2012.670028. [DOI] [PubMed] [Google Scholar]
- 16.Rosenthal M., Young T. Effective family intervention after traumatic brain injury: theory and practice. J. Head Trauma Rehabil. 1988;3(4):42–50. [Google Scholar]
- 17.Amir N., Taylor C.T. Combining computerized home-based treatments for generalized anxiety disorder: an attention modification program and cognitive behavioral therapy. Behav. Ther. 2012;43(3):546–559. doi: 10.1016/j.beth.2010.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boman I.L. Cognitive training in home environment. Brain Inj. 2004;18(10):985–995. doi: 10.1080/02699050410001672396. [DOI] [PubMed] [Google Scholar]
- 19.Margrett J.A., Willis S.L. In-home cognitive training with older married couples: individual versus collaborative learning. Neuropsychol. Dev. Cogn. B Aging Neuropsychol. Cogn. 2006;13(2):173–195. doi: 10.1080/138255890969285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shatil E. Home-based personalized cognitive training in MS patients: a study of adherence and cognitive performance. NeuroRehabilitation. 2010;26(2):143–153. doi: 10.3233/NRE-2010-0546. [DOI] [PubMed] [Google Scholar]
- 21.Bordin E.S. 1994. Theory and Research on the Therapeutic Working Alliance: New Directions. The Working Alliance: Theory, Research, and Practice; pp. 13–37. [Google Scholar]
- 22.Schaffer N.D. Multidimensional measures of therapist behavior as predictors of outcome. Psychol. Bull. 1982;92(3):670–681. [PubMed] [Google Scholar]
- 23.Lacrosse M.B. Perceived counselor social-influence and counseling outcomes - validity of the counselor rating form. J. Counsel. Psychol. 1980;27(4):320–327. [Google Scholar]
- 24.Orlinsky D.E. Varieties of psychotherapies and psychotherapists. In: Lippe A., Nissen H., Oddli H.W., editors. Psykoterapeuten - en antologi om terapeutens rolle i psykoterapi. Gyldendal Norsk Forlag a/S; Oslo: 2014. [Google Scholar]
- 25.Wilms I.L. In: Severe Neglect and Computer-Based Home Training in Virtual, Augmented and Mixed Reality. Applications of Virtual and Augmented Reality: 6th International Conference, VAMR 2014. Shumaker R., Lackey S., editors. Springer International Publishing; Germany: 2014. pp. 329–339. (Held as Part of HCI International 2014, Heraklion, Crete, Greece, June 22-27, 2014, Proceedings, Part II). [Google Scholar]
- 26.Smith J.A., Flowers P., Larkin M. Sage Publications Ltd; London, UK: 2009. Interpretive Phenomenological Analysis; p. 225. [Google Scholar]
- 27.Willig C. Interpretive phenomenology. In: Willig C., editor. Introducing Qualitative Research in Psychology. Open University Press; Philadelphia: 2008. [Google Scholar]
- 28.Kvale S. Sage; Thousand Oaks, CA: 1996. InterViews: an Introduction to Qualitative Research. [Google Scholar]
- 29.Frassinetti F. Long-lasting amelioration of visuospatial neglect by prism adaptation. Brain. 2002;125:608–623. doi: 10.1093/brain/awf056. [DOI] [PubMed] [Google Scholar]
- 30.MedComMedical Software E. https://www.medicalcomputing.de/eyemove/
- 31.Tactus Therapy . TactusTherapy; 2013. Visual Attention Therapy.https://tactustherapy.com/app/vat/ [Google Scholar]
- 32.Pedersen P.M. CogniSoft; 2007. Afasiassistent.https://www.cognisoft.dk/afasi.html [Google Scholar]
- 33.Levine C. Bridging troubled waters: family caregivers, transitions, and long-term care. Health Aff. 2010;29(1):116–124. doi: 10.1377/hlthaff.2009.0520. [DOI] [PubMed] [Google Scholar]
- 34.Sherwin E.D. Negotiating the reality of caregiving: hope, burnout and nursing. J. Soc. Clin. Psychol. 1992;11(2):129–139. [Google Scholar]
- 35.Webster G., Daisley A., King N. Relationship and family breakdown following acquired brain injury: the role of the rehabilitation team. Brain Inj. 1999;13(8):593–603. doi: 10.1080/026990599121331. [DOI] [PubMed] [Google Scholar]
- 36.Peters L.C. Psychosocial sequelae of closed head injury: effects on the marital relationship. Brain Inj. 1990;4(1):39–47. doi: 10.3109/02699059009026147. [DOI] [PubMed] [Google Scholar]
- 37.Burridge A.C. Spousal relationship satisfaction following acquired brain injury: the role of insight and socio-emotional skill. Neuropsychol. Rehabil. 2007;17(1):95–105. doi: 10.1080/09602010500505070. [DOI] [PubMed] [Google Scholar]
- 38.Appelros P. Prognosis for patients with neglect and anosognosia with special reference to cognitive impairment. J. Rehabil. Med. 2003;35(6):254–258. doi: 10.1080/16501970310012455. [DOI] [PubMed] [Google Scholar]
- 39.Wall J.A., Callister R.R. Conflict and its management. J. Manag. 1995;21(3):515–558. [Google Scholar]
- 40.Wilms I. Using artificial intelligence to control and adapt level of difficulty in computer-based, cognitive therapy – an explorative study. J. Cyberther. Rehabil. 2011;4(3):387–396. [Google Scholar]
- 41.Wilms I. Adaptive cognitive rehabilitation. In: Book A.L., editor. Technologies of Inclusive Well-Being. Springer Verlag; Heidelberg: 2014. pp. 75–93. [Google Scholar]