Abstract
Purpose
The risk of posthepatectomy liver failure (PHLF) after right hepatectomy remains substantial. Additional parameters such as computed tomography volumetry, liver stiffness measurement by FibroScan, indocyanine green retention rate at 15 minutes, and platelet count used to properly assess future liver remnant volume quality and quantity are of the utmost importance. Thus, we compared the usefulness of these modalities for predicting PHLF among patients with hepatocellular carcinoma after right hepatectomy.
Methods
We retrospectively reviewed patients who underwent right hepatectomy for hepatocellular carcinoma between 2007 and 2013. PHLF was determined according to International Study Group of Liver Surgery consensus definition and severity grading. Grades B and C were defined as clinically relevant posthepatectomy liver failure (CRPHLF). The results were internally validated using a cohort of 97 patients.
Results
Among the 90 included patients, 15 (16.7%) had CRPHLF. Multivariate analysis confirmed that platelet count < 140 (109/L) (hazard ratio [HR], 24.231; 95% confidence interval [CI], 3.623–161.693; P = 0.001) and remnant liver volume-to-body weight (RVL/BW) ratio < 0.55 (HR, 25.600; 95% CI, 4.185–156.590; P < 0.001) were independent predictors of CRPHLF. Among the 12 patients with a platelet count < 140 (109/L) and RLV/BW ratio < 0.55, 9 (75%) had CRPHLF. Likewise, 5 of 38 (13.2%) with only one risk factor developed CRPHL versus 1 of 40 (2.5%) with no risk factors. These findings were confirmed by the validation cohort.
Conclusion
RLV/BW ratio and platelet count are more important than the conventional RLV/TFLV, indocyanine green retention rate at 15 minutes, and liver stiffness measurement in the preoperative risk assessment for CRPHLF.
Keywords: Hepatectomy, Hepatocellular carcinoma, Liver failure
INTRODUCTION
Liver resection remains the mainstay of treatment for hepatocellular carcinoma (HCC). Recent advances in surgical techniques and instrumentations have greatly improved liver surgery outcomes [1,2]. However, the risk of posthepatectomy liver failure (PHLF) remains substantial after major hepatectomy [3] with a considerable fatal outcome rate [4]. Thus, a proper preoperative evaluation and identification of patients at risk for PHLF is of paramount importance.
Consequently, defining oncologic resections to prevent PHLF warrants a thorough assessment of future liver remnant (FLR) quality and quantity [5]. This is particularly relevant among patients who will undergo right hepatectomy because of the relatively small FLR in such cases. It was found that the remnant liver volume-to-body weight ratio (RLV/BWR) was more specific than the remnant liver volume-to-total functional liver volume (RLV/TFLV) ratio in assessing FLR following major hepatectomy in cirrhotic and noncirrhotic patients [6,7]. In addition, various quantitative and qualitative tests to assess liver function such as indocyanine green (ICG) [8,9,10,11], platelet count determination [12], and liver stiffness measurement using a FibroScan [13] are presently being utilized as part of the standard protocol prior to liver resection. The clinical application of these modalities for identifying patients at risk of PHLF and selecting patients who will most likely benefit from upfront curative hepatic resection or portal vein embolization (PVE) prior to resection deserves consideration.
However, the standardization of which among these sophisticated methods should be used preoperatively varies among centers. Up to date, it is still unclear which among these preoperative parameters play the most important role in determining PHLF. This study was conducted to compare the usefulness of CT volumetry using the conventional RLV/TFLV and RLV/BW, ICG, liver stiffness measurement using a Fibroscan, and platelet count for predicting PHLF among patients with HCC after right hepatectomy according to the International Study Group of Liver Surgery (ISGLS) definition of PHLF. Using these modalities, we hope to identify patients at greatest and lowest risk for PHLF thereby identifying patients who might benefit from right hepatectomy or volume-preserving right hepatectomy or PVE.
METHODS
Study design
Here we retrospectively reviewed the cases of all patients who underwent right hepatectomy for HCC between 2007 and 2013. We only included those patients for whom preoperative FibroScan, CT volumetry, ICG retention rate at 15 minutes (ICG R15), complete blood count with differentials, and preoperative and postoperative liver function test data were available. Exclusion criteria were incomplete imaging and liver function test results and a lack of data to identify PHLF.
A cohort of patients who underwent right hepatectomy for HCC in the same period with incomplete laboratory results for ICG R 15% and liver stiffness measurement was retrospectively reviewed and formed the validation cohort of this study. The study protocol was approved by the Institutional Review Board (approval number 4-2018-0974), and the need for written informed consent was waived because of the retrospective nature of the study.
Data collection
The data were collected prospectively from the hospital's electronic medical records database. The patients' demographic characteristics, clinical presentations, preoperative comorbidities, perioperative outcomes, imaging studies, and laboratory results were reviewed and analyzed. The imaging and laboratory studies were obtained within 1 month prior to surgery, and the most recent preoperative laboratory results were recorded. The postoperative complications were categorized according to Clavien-Dindo classification [14].
There were 4 surgeons performing liver resections during this period. The decision to perform the right hepatectomy was determined according to the patients' general health condition, extent of tumor involvement, liver function (Child A), portal hypertension (presence of splenomegaly or esophageal varices), and liver volume. Generally, a right hepatectomy was performed in patients whose left liver volume was ≥30% of the total liver volume (TLV), Child A, and no signs of portal hypertension. Patients with <30% FLR usually underwent PVE or volume-preserving right hepatectomy. Moreover, patients with hepatitis B or C virus infection were treated preoperatively.
Right hepatectomy
The abdomen was accessed using a right subcostal incision with midline extension to the xiphoid. After liver mobilization, the hanging method was utilized. The right hepatic artery and right portal vein were individually then ligated and transected and the right hepatic duct was left divided during the parenchymal transection. The parenchymal transection followed the intrahepatic course of the middle hepatic vein using the Cavitron Ultrasonic Surgical Aspirator. After hemostasis was ensured, 2 drains were placed at the right subdiaphragmatic area and the abdomen was closed. The Pringle maneuver was not used in any case.
CT volumetry
TLV, total right liver volume, and tumor volume were measured manually by delineating the liver contour on every cut with a 3-mm slice thickness. The total surface area was then measured on each imaging cut and as well as the distance between slices for the volume calculation. The RLV to total functional liver volume (RLV/TFLV) and RLV to body weight (RLV/BW) ratios were calculated using the following formulas:
| TFLV (cm3) = TLV − total tumor volume |
| RLV (cm3) = TLV − right liver volume |
| RLV/TFLV (%) = RLV (cm3) /TFLV (cm3) × 100 |
| RLV/BW (%) = RLV (cm3) /actual body weight (g) × 100 |
For patients who underwent PVE, the liver volume after the PVE was measured and was used in the analysis. Only one surgeon prospectively reviewed and measured the liver volume in this cohort using the Voxelplus (Mevisys Co. Ltd., Daejeon, Korea) program.
ICG R15
For the ICG R15 test, ICG 0.5 mg/kg was administered through a peripheral vein and measured using pulse dye densitometry. The ICG R15 and plasma disappearance rate (ICG-k per minute) were recorded and calculated.
Liver stiffness
Liver stiffness in the right lobe of the liver was measured using a FibroScan (Echosens North America Inc., Waltham, MA, USA). A sonographic evaluation was used to properly identify the free-tumor liver parenchyma. Ten measurements were performed in all patients and the success rate was calculated as the number of validated measurements divided by the total number of measurements. For each patient, the liver stiffness values were accepted only if the success rate was at least 60%. The results are expressed in kilopascals (kPa). Liver stiffness was assessed by only one dedicated radiologist during this period.
Primary outcome
PHLF was determined according to the ISGLS consensus definition and severity grading [15]. Briefly, PHLF is characterized by increase in prothrombin time-international normalized ratio (PT-INR) and hyperbilibirubinemia (according to the normal cutoff levels defined by the local laboratory) on or after postoperative day 5. If PT-INR or serum bilirubin is increased preoperatively, PHLF is defined by an increasing PT-INR and serum bilirubin level on or before postoperative day 5 (compared with the values of the previous day). Patients with abnormal laboratory parameters not requiring a change in clinical management were categorized as grade A. However, patients who required further clinical management but did not need invasive treatment and patients who needed invasive treatment were categorized as grades B and C, respectively. In this study, grade A was defined as non-clinically relevant PHLF (CRPHLF), whereas grade B and C were defined as CRPHLF.
Statistical analysis
The data analysis was performed using IBM SPSS Statistics ver. 22 (SPSS Inc., Chicago, IL, USA). Categorical variables are expressed as frequency (%), whereas continuous variables are presented as mean with range or ± standard deviation. The association between variables and PHLF was tested as continued and categorical using logistic regression analysis and Fisher exact test, respectively. The optimal cutoff values for RLV/TFLV ratio, RLV/BW ratio, liver stiffness, ICG R15, and platelet count were determined using receiver operating characteristic (ROC) curve analysis. Statistically significant variables (P < 0.05) on univariate analysis were entered into a multivariate logistic regression model to identify the independent risk factors for CRPHLF. Two-sided P-values < 0.05 were used to define statistical significance.
RESULTS
Patient characteristics of the primary and validation cohorts
A total of 90 patients who met the inclusion criteria were included in the analysis in the primary cohort, comprising 12 women (13.3%) and 78 men (86.6%). We identified 24 patients (26.6%) who experienced PHLF according to the ISGLS criteria. Among them, 15 (16.7%) had CRPHLF (11 grade B and 4 grade C PHLF).
Among 4 patients with grade C PHLF, 3 died postoperatively. These patients were managed in the intensive care unit. Three required invasive mechanical ventilation. Hemodialysis was performed in 2 patients. Patients with grade B PHLF (n = 9) were managed conservatively in the intermediate care unit through administrations of FFP, albumin, and diuretics if appropriate. All patients with grade B recovered well. However, the average length of hospital stay among patients with CRPHLF was 23.7 ± 14.3 days.
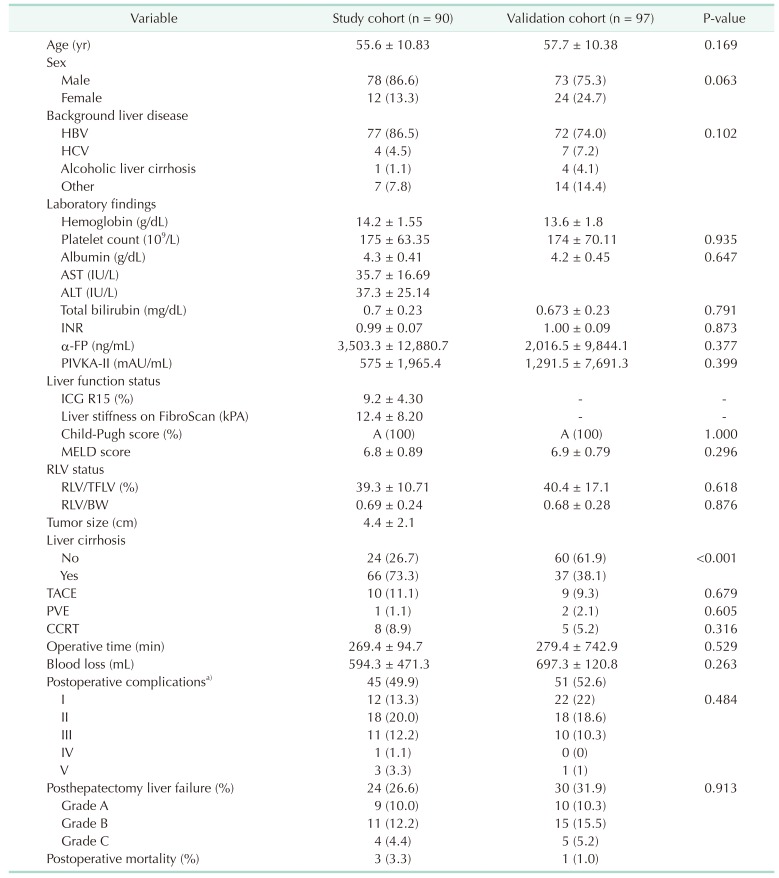
For the validation cohort, 97 patients were included. Notably, there were more patients with liver cirrhosis in the primary cohort compared to the validation cohort (73.3% vs. 38.1%, P < 0.001, respectively). Table 1 summarizes the clinicopathological characteristics of the patients who underwent right hepatectomy for HCC in the primary and validation cohorts.
Table 1. Clinical characteristics of patients in the primary study cohort and validation cohorts who underwent right hepatectomy for hepatocellular carcinoma.
Values are presented as mean ± standard deviation or number (%).
INR, international normalized ratio; PIVKA, protein induced by vitamin K absence/antagonist; ICG R15, indocyanine green retention rate at 15 minutes; MELD, model for end-stage liver disease; RLV, remnant liver volume; TFLV, total functional liver volume; BW, body weight; TACE, transarterial chemoembolization; PVE, portal vein embolization; CCRT, concurrent chemoradiotherapy.
a)Postoperative complication was assessed by Clavien-Dindo classification.
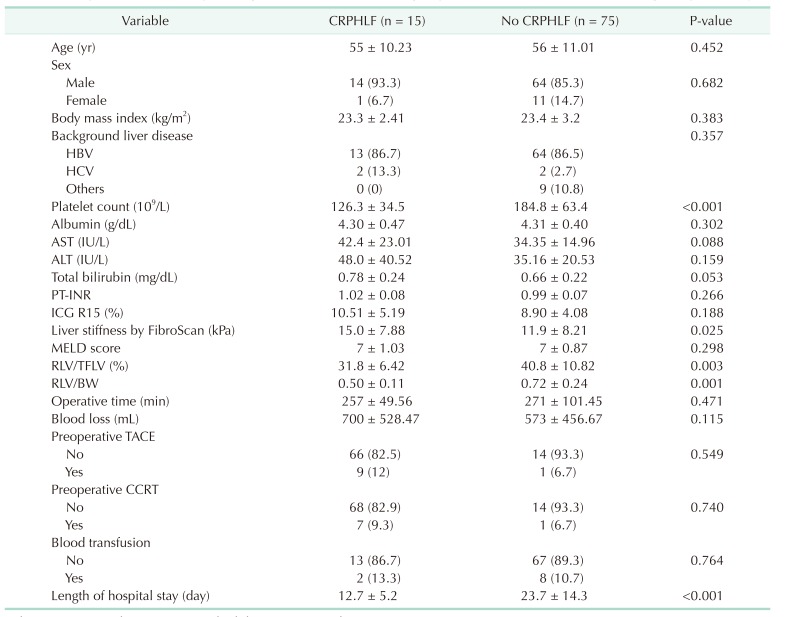
Analysis of factors predicting CRPHLF
In the primary cohort, we compared the preoperative clinical variables associated with no CRPHLF and CRPHLF (Table 2). Platelet count (P < 0.001), liver stiffness (P = 0.025), RLV/TFLV ratio (P = 0003), and RLV/BW ratio (P < 0.001) were significantly associated with CRPHLF.
Table 2. Comparisons of clinicopathologic variables between the groups with or without CRPHLF after right hepatectomy.
Values are presented as mean ± standard deviation or number (%).
CRPHLF, clinically relevant posthepatectomy liver failure; PT-INR, prothrombin time-international normalized ratio; ICG R15, indocyanine green retention rate at 15 minutes; RLV, remnant liver volume; TFLV, total functional liver volume; BW, body weight; TACE, transarterial chemoembolization; CCRT, concurrent chemoradiotherapy.
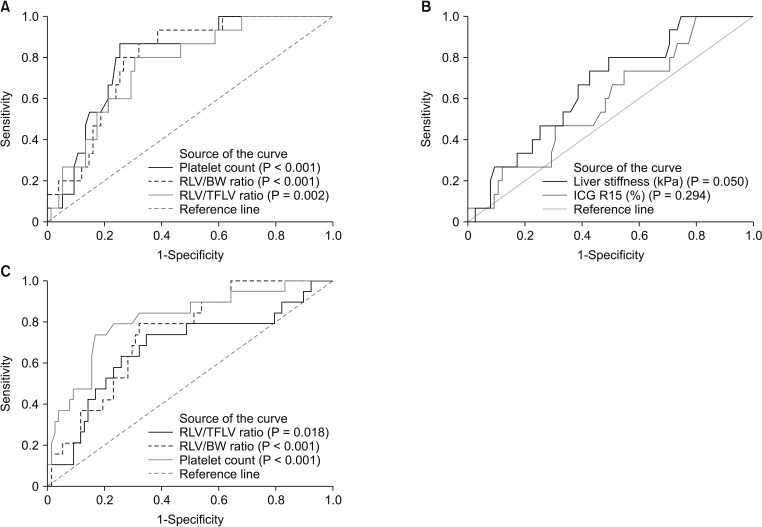
To determine optimal cutoff values for each variable, an ROC curve analysis was performed (Fig. 1A). In the primary cohort, the optimal cutoff values for platelet, RLV/BW ratio, RLV/TFLV ratio, liver stiffness, and ICG R15 were 140 (109/L), 0.55, 35%, 11 kPa, and 11%, respectively. Platelet count had the widest area under the curve (AUC, 0.796; 95% confidence interval [CI], 0.689–0.902, P < 0.001). The RVL/BW ratio had a wider AUC (0.793, 95% CI, 0.641–0.877; P < 0.001) compared to RLV/TFLV ratio (0.759; 95% CI, 0.352–0.679; P = 0.002). This result was also confirmed by the validation cohort with AUC values of 813 (95% CI, 0.701–0.925; P < 0.001), 0.742 (95% CI, 0.632–0.851; P < 0.001), and 0.676 (0.530–0.822; P = 0.018) for platelet count, RLV/BW, and RLV/TFLV ratio, respectively (Fig. 1B). Liver stiffness and ICG 15R had AUC values of, 0.661 (95% CI, 0.524–0.798; P = 0.050), and 0.586 (95% CI, 438–0.735; P = 0.294), respectively.
Fig. 1. Receiver operating characteristic curve of clinically relevant posthepatectomy liver failure (International Study Group of Liver Surgery grades B and C). (A) At a cutoff value of <140 (109/L), platelet count had a sensitivity of 86.7%, and specificity of 74.7% for predicting clinically relevant posthepatectomy liver failure. The optimal cutoff value for remnant liver volume-to-body weight (RLV/BW) ratio was 0.55 (sensitivity, 80%; specificity, 73.3%), while remnant liver volume/total functional liver volume (RLV/TFLV) ratio was 35 (sensitivity, 80%; specificity, 57.3%) of the primary cohort. (B) Optimal value of liver stiffness is 11.1 kPa (sensitivity, 66.7%; specificity, 57.3%), while indocyanine green retention rate at 15 minutes has an optimal cutoff value of 11.1 (sensitivity, 26.7%; specificity, 76%) of the primary cohort. (C) In the validation cohort, the optimal cutoff values for platelet count, RLV/BW ratio, and RLV/TFLV ratio were the same as the primary cohort.
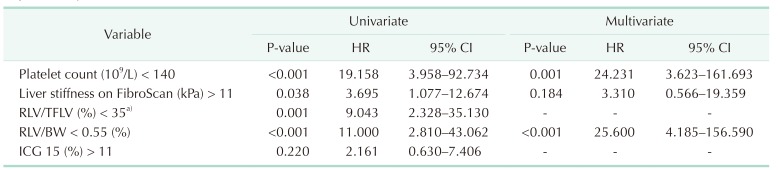
A univariate logistic regression analysis was performed for each optimal cutoff value. A platelet count <140 (109/L), liver stiffness at kPA > 11, RLV/TFLV ratio of <35%, and RLV/BW ratio of <0.55 were significantly associated with CRPHLF (P < 0.05). On multivariate analysis, only a platelet count <140 (109/L) (hazard ratio [HR], 24.231; 95% CI, 3.623–161.693; P = 0.001) and RVL/BW ratio < 0.55 (HR, 25.600; 95% CI, 4.185–156.590; P < 0.001) were independently associated with CRPHLF. Since RLV/BW ratio had higher AUC compared to RLV/FTLV ratio, the RLV/BW was the variable selected to be entered in the multivariable analysis model (Table 3).
Table 3. Logistic regression analysis of risk factors for clinically relevant posthepatectomy liver failure after right hepatectomy.
HR, hazard ratio; CI, confidence interval; RLV, remnant liver volume; TFLV, total functional liver volume; BW, body weight; ICG R15, indocyanine green retention rate at 15 minutes.
a)Not included in multivariate analysis.
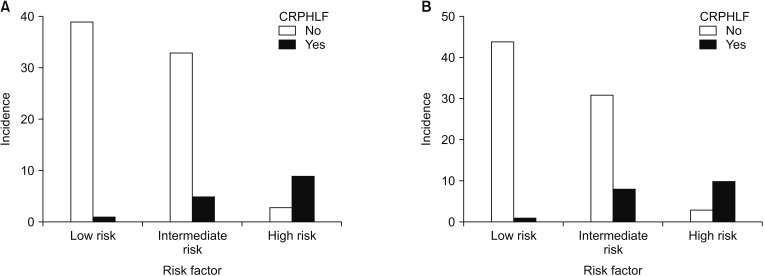
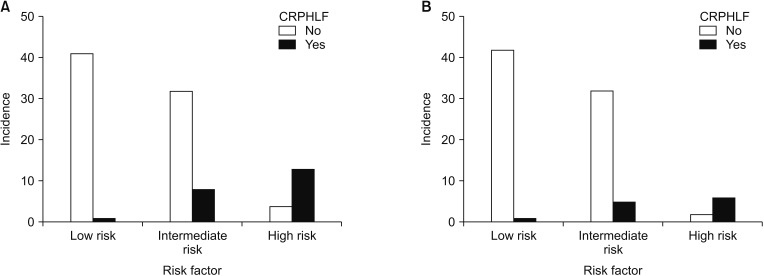
Consequently, we identified 3 risk subsets for predicting CRPHLF after right hepatectomy in the primary cohort (low, intermediate, high risk). Among the 12 patients who had both a platelet count <140 (109/L) and RLV/BW ratio < 0.55 (high-risk group), 9 (75%) had CRPHLF. Likewise, 5 of 38 patients (13.2%) with either of the risk factors (intermediate-risk group) had CRPHLF, while 1 of 40 patients (2.5%) had no risk factors (low-risk group). These results were confirmed by the validation cohort (Fig. 2). Using the same cut off values for platelet count and RLV/BW ratio, 10 out of 13 high-risk patients (76.9%) had CRPHLF. In addition, 8 out of 39 patients (20.5%) and 1 out of 44 patients (2.2%) had CRPHLF in the intermediate- and low-risk groups, respectively.
Fig. 2. Percentage risk of patients with hepatocellular carcinoma who underwent right hepatectomy according to the number of risk factors (platelet count < 140 [109/L] and remnant liver volume-to-body weight ratio < 0.55). (A) Primary cohort and (B) validation cohort. High risk, platelet count < 140 (109/L), and RLV/BW ratio < 0.55; intermediate risk, either platelet count < 140 (109/L) or RLV/BW ratio < 0.55; low risk, platelet count > 140 (109/L) and RLV/BW ratio > 0.55. CRPHLF, clinically relevant posthepatectomy liver failure; RLV/BW, remnant liver volume-to-body weight.
A subgroup analysis combining the primary and validation cohort was made among patients with no liver cirrhosis and with liver cirrhosis. Among 187 patients, 84 (44.9%) had liver cirrhosis while 103 (55.1%) had no liver cirrhosis. Compared to the RLV/BW ratio, the RLV/TLFV ratio had a smaller AUC in patients with liver cirrhosis and no liver cirrhosis (AUC, 0.762; 95% CI, 0.649–0.874; P < 0.001 vs. AUC, 0.785; 95% CI, 0.694–0.876; P < 0.001; and, AUC, 0.626; 95% CI, 0.438–0.814; P = 0.164 vs. AUC, 0.748; 95% CI, 0.611–0.855; P=0.007, respectively). The platelet count had the highest AUC among the 3 parameters in patients with liver cirrhosis (AUC, 0.794; 95% CI, 0.693–0.896; P < 0.001) and no liver cirrhosis (AUC, 0.814; 95% CI, 0.683–0.944; P = 0.001). The optimal cutoff value of the RLV/BW ratio and RLV/TFLV ratio for predicting CRPHLF among patients with liver cirrhosis and no liver cirrhosis where the same as the results of the primary cohort (0.55 and 35%, respectively). However, platelet count had a lower cutoff value in patients with liver cirrhosis compared to patients with no liver cirrhosis (138 [109/L] and 140 [109/L], respectively). Nevertheless, among 84 patients with no liver cirrhosis, 6 out of 8 high-risk patients (75%) (platelet count < 140 [109/L] and RLV/BW ratio < 0.55) had CLPHLF while 1 out of 40 low-risk patients (2.5%) (platelet count > 140 [109/L] and RLV/BW ratio > 0.55) had a CRPHLF. Likewise, among 103 patients with liver cirrhosis, 13 out of 17 patients (76.5%) had CLPHLF while 1 out of 45 low-risk patients (2.2%) had CRPHLF (Fig. 3).
Fig. 3. Percentage risk of patients with hepatocellular carcinoma who underwent right hepatectomy according to the (platelet count < 140 [109/L] and remnant liver volume-to-body weight ratio < 0.55). (A) Patients with liver cirrhosis and (B) patients with no liver cirrhosis. High risk, platelet count < 140 (109/L) and RLV/BW ratio < 0.55; intermediate risk, either platelet count < 140 (109/L) or RLV/BW ratio < 0.55; low risk, platelet count > 140 (109/L) and RLV/BW ratio > 0.55. CRPHLF, clinically relevant posthepatectomy liver failure; RLV/BW, remnant liver volume-to-body weight.
DISCUSSION
It is well recognized that FLR is the most reliable determinant of hepatic dysfunction after major hepatectomy [16,17]. The FLR is usually expressed as the RLV/TLV ratio [18]. Truant et al. [7] reported that RLV/BW ratio was more specific than RLV/TLV in predicting liver failure after extended hepatectomy. At a cutoff value of 0.50%, RLV/BW ratio was associated with significantly higher 3-month morbidity and mortality rates as well as PHLF-associated mortality. The same cutoff value that was used by Schnitzbauer et al. [19] to classify patients undergoing portal vein ligation and in situ splitting achieved adequate FLR. Nonetheless, the present study demonstrated that RLV/BW ratio was independently associated with CRPHLF at a cutoff value of <0.55%. Although RLV/TFLV ratio was associated with CRPHLF at a cutoff value of 35%, it was shown in this cohort that RLV/BW ratio was more sensitive and specific than RLV/BW ratio for predicting CRPHLF.
Although a CT volumetric study preoperatively assesses FLR, it does not determine the associated liver disease or functional liver derangement. In the present study, we carefully evaluated liver function using child and model for end-stage liver disease (MELD) scores and properly selected patients to undergo liver resection. Hence, all of our patients had a Child class of A and a mean MELD score of 6.8 ± 0.89. However, in this present cohort, ICG R15 was not entirely adopted in our institution to assess liver function. As such, only in selected patients the ICG R15 was performed. The cutoff value of ICG R15 for major hepatectomy for HCC was reportedly safe at <10% [20]. Although reports of the safety of major hepatectomy used an ICG R15 cutoff value of <14% [21], our study found that ICG R15 as a continuous and categorical variable with an optimal cutoff value of 11% was not significantly associated with CRPHLF.
Furthermore, the use of transient elastography to evaluate the underlying liver fibrosis or cirrhosis was also not well adopted during this period in our institution; hence, it was not performed in all patients. Our present study showed a significant association between liver stiffness and CRPHLF at a cutoff value of 11 kPa on univariate analysis. Although it was reported that liver stiffness is a good determinant for liver cirrhosis [22,23], it was not found to be an independent predictor of CRPHLF.
As an indirect determinant for portal hypertension, low platelet count is known to be associated with liver dysfunction following major hepatectomy [12,24]. Although the optimal cutoff value for platelet count to predict PHLF varies among studies [25], here we found that a platelet count < 140 (109/L) was a significant independent predictor for CRPHLF.
However, it is noteworthy that the ability of the FLR to sustain the body's metabolic demand after hepatectomy not only depends on its functional reserve but also on its regenerative capacity. Notwithstanding that liver regenerative capacity is influenced by underlying diseases, in particular the presence of cirrhosis, the effect of low platelet count on liver regeneration has also been established in several studies. As such, low platelet count, as a surrogate for portal hypertension, may also influence the development of CRPHLF through its negative effect of liver regenerative capacity following hepatectomy.
Interestingly, we found that the presence of both an RLV/BW ratio < 0.55% and a platelet count < 140 (109/L) was associated with a 75% risk of CRPHLF after right hepatectomy. Nevertheless, if one of these parameters is present, only 13.2% are at risk of CRPHLF. Most importantly, if none of these are present, there is a 2.5% risk of CRPHLF. As such, when planning for right hepatectomy for HCC, it should be emphasized that patients with these 2 risk factors may benefit from PVE or volume-preserving right hepatectomy. In particular, the ventral segment-preserving right hepatectomy was found to be very useful for patients with small left liver volume. This procedure could preserve an adequate remnant liver volume to sustain the patient's metabolic demand [26]. However, for patients in the low-risk group, a right hepatectomy can be performed.
The present study was a retrospective design, which creates an unavoidable limitation. First, the accuracy of the CT volumetry software (Voxelplus) was not fully evaluated, mainly because of the retrospective nature of the study. Although our previous data showed a small discrepancy between preoperative CT liver volume and the actual specimen weight (714.9 ± 251.21 vs. 711.9 ± 252.45, respectively) [26], the actual weights, however, were based on the pathologic report which could to lead overestimation or underestimation of the result [27]. We believe that to fully assess its predictive value for the actual resected specimen, a well-design study is needed; such as a timely specimen-weight assessment right after resection – a scenario which can possibly be attained during living donor liver transplantation [28]. Secondly, it was also a singleinstitution study with a relatively small sample. Nevertheless, to the best of our knowledge, this is the first study which included the data on preoperative CT volumetry studies (RLV/BW and RLV/TFLV), ICG R 15%, liver stiffness, and traditional laboratory values such as platelet count for predicting CRPHLF. Furthermore, we validated our results. Although there was a significant difference in terms of the number of patients with liver cirrhosis between the 2 groups, and this maybe the reason why the ICG R15 or Fibroscan was requested on this group of patients, this difference may further expand the clinical application of this finding in noncirrhotic and cirrhotic patients. In fact, a subgroup analysis showed the same results as the primary and validation cohort. In clinical practice, utilizing RLV/BW ratio and platelet count can provide simple and useful information regarding decision-making and risk-stratification strategies for managing hepatocellular cancer, especially in centers where sophisticated parameters such as ICG R15 or liver stiffness measurement are not available. It is very easy to perform and provides a reliable cutoff value that could prevent PHLF. Although the emerging role of new modalities such as 99mTc-mebrofenin hepatobiliary scintigraphy [29] and gadoxetic acid-enhanced MRI [30] in predicting PHLF has been reported in the literature, its propagation is still limited only to selected centers. However, a larger prospective or multicenter study is required to validate our findings.
In summary, RLV/BW ratio of <0.55 and platelet count < 140 (109/L) are the only independent predictors of CRPHLF after right hepatectomy in Child A patients in this cohort. CRPHLF will develop in 75% of patients with 2 of these risk factors, and in 2.5% of patients with none of these risk factors. High-risk patients may benefit from preoperative PVE and parenchymal preserving right hepatectomy, while low-risk patients may undergo right hepatectomy. Caution should be observed in doing right hepatectomy on intermediate-risk patients due to the associated 13.2% risk of CRPHLF. However, these findings should be validated in a prospective and a well-designed randomized study.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Allen PJ, Jarnagin WR. Current status of hepatic resection. Adv Surg. 2003;37:29–49. [PubMed] [Google Scholar]
- 2.Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, et al. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg. 2002;236:397–406. doi: 10.1097/01.SLA.0000029003.66466.B3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van den Broek MA, Olde Damink SW, Dejong CH, Lang H, Malago M, Jalan R, et al. Liver failure after partial hepatic resection: definition, pathophysiology, risk factors and treatment. Liver Int. 2008;28:767–780. doi: 10.1111/j.1478-3231.2008.01777.x. [DOI] [PubMed] [Google Scholar]
- 4.Mullen JT, Ribero D, Reddy SK, Donadon M, Zorzi D, Gautam S, et al. Hepatic insufficiency and mortality in 1,059 noncirrhotic patients undergoing major hepatectomy. J Am Coll Surg. 2007;204:854–862. doi: 10.1016/j.jamcollsurg.2006.12.032. [DOI] [PubMed] [Google Scholar]
- 5.Cauchy F, Soubrane O, Belghiti J. Liver resection for HCC: patient’s selection and controversial scenarios. Best Pract Res Clin Gastroenterol. 2014;28:881–896. doi: 10.1016/j.bpg.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 6.Lin XJ, Yang J, Chen XB, Zhang M, Xu MQ. The critical value of remnant liver volume-to-body weight ratio to estimate posthepatectomy liver failure in cirrhotic patients. J Surg Res. 2014;188:489–495. doi: 10.1016/j.jss.2014.01.023. [DOI] [PubMed] [Google Scholar]
- 7.Truant S, Oberlin O, Sergent G, Lebuffe G, Gambiez L, Ernst O, et al. Remnant liver volume to body weight ratio > or =0.5%: a new cut-off to estimate postoperative risks after extended resection in noncirrhotic liver. J Am Coll Surg. 2007;204:22–33. doi: 10.1016/j.jamcollsurg.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 8.Manizate F, Hiotis SP, Labow D, Roayaie S, Schwartz M. Liver functional reserve estimation: state of the art and relevance for local treatments: the Western perspective. J Hepatobiliary Pancreat Sci. 2010;17:385–388. doi: 10.1007/s00534-009-0228-x. [DOI] [PubMed] [Google Scholar]
- 9.Yokoyama Y, Nishio H, Ebata T, Igami T, Sugawara G, Nagino M. Value of indocyanine green clearance of the future liver remnant in predicting outcome after resection for biliary cancer. Br J Surg. 2010;97:1260–1268. doi: 10.1002/bjs.7084. [DOI] [PubMed] [Google Scholar]
- 10.Yokoyama Y, Ebata T, Igami T, Sugawara G, Mizuno T, Yamaguchi J, et al. The Predictive value of indocyanine green clearance in future liver remnant for posthepatectomy liver failure following hepatectomy with extrahepatic bile duct resection. World J Surg. 2016;40:1440–1447. doi: 10.1007/s00268-016-3441-1. [DOI] [PubMed] [Google Scholar]
- 11.Kim JM, Kwon CH, Joh JW, Park JB, Lee JH, Kim GS, et al. Can the model for end-stage liver disease score replace the indocyanine green clearance test in the selection of right hemihepatectomy in Child-Pugh class A? Ann Surg Treat Res. 2014;86:122–129. doi: 10.4174/astr.2014.86.3.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Venkat R, Hannallah JR, Krouse RS, Maegawa FB. Preoperative thrombocytopenia and outcomes of hepatectomy for hepatocellular carcinoma. J Surg Res. 2016;201:498–505. doi: 10.1016/j.jss.2015.08.038. [DOI] [PubMed] [Google Scholar]
- 13.Pavlov CS, Casazza G, Nikolova D, Tsochatzis E, Burroughs AK, Ivashkin VT, et al. Transient elastography for diagnosis of stages of hepatic fibrosis and cirrhosis in people with alcoholic liver disease. Cochrane Database Syst Rev. 2015;1:CD010542. doi: 10.1002/14651858.CD010542.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS) Surgery. 2011;149:713–724. doi: 10.1016/j.surg.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 16.Shirabe K, Shimada M, Gion T, Hasegawa H, Takenaka K, Utsunomiya T, et al. Postoperative liver failure after major hepatic resection for hepatocellular carcinoma in the modern era with special reference to remnant liver volume. J Am Coll Surg. 1999;188:304–309. doi: 10.1016/s1072-7515(98)00301-9. [DOI] [PubMed] [Google Scholar]
- 17.Schindl MJ, Redhead DN, Fearon KC, Garden OJ, Wigmore SJ Edinburgh Liver Surgery and Transplantation Experimental Research Group (eLISTER) The value of residual liver volume as a predictor of hepatic dysfunction and infection after major liver resection. Gut. 2005;54:289–296. doi: 10.1136/gut.2004.046524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abdalla EK, Denys A, Chevalier P, Nemr RA, Vauthey JN. Total and segmental liver volume variations: implications for liver surgery. Surgery. 2004;135:404–410. doi: 10.1016/j.surg.2003.08.024. [DOI] [PubMed] [Google Scholar]
- 19.Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012;255:405–414. doi: 10.1097/SLA.0b013e31824856f5. [DOI] [PubMed] [Google Scholar]
- 20.Torzilli G, Makuuchi M, Inoue K, Takayama T, Sakamoto Y, Sugawara Y, et al. No-mortality liver resection for hepatocellular carcinoma in cirrhotic and noncirrhotic patients: is there a way? A prospective analysis of our approach. Arch Surg. 1999;134:984–992. doi: 10.1001/archsurg.134.9.984. [DOI] [PubMed] [Google Scholar]
- 21.Fan ST, Lai EC, Lo CM, Ng IO, Wong J. Hospital mortality of major hepatectomy for hepatocellular carcinoma associated with cirrhosis. Arch Surg. 1995;130:198–203. doi: 10.1001/archsurg.1995.01430020088017. [DOI] [PubMed] [Google Scholar]
- 22.Cescon M, Colecchia A, Cucchetti A, Peri E, Montrone L, Ercolani G, et al. Value of transient elastography measured with FibroScan in predicting the outcome of hepatic resection for hepatocellular carcinoma. Ann Surg. 2012;256:706–712. doi: 10.1097/SLA.0b013e3182724ce8. [DOI] [PubMed] [Google Scholar]
- 23.Kim SU, Ahn SH, Park JY, Kim DY, Chon CY, Choi JS, et al. Prediction of postoperative hepatic insufficiency by liver stiffness measurement (FibroScan((R))) before curative resection of hepatocellular carcinoma: a pilot study. Hepatol Int. 2008;2:471–477. doi: 10.1007/s12072-008-9091-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang Z, Zhang Y, Wang W, Hua Y, Liu L, Shen S, et al. Thrombocytopenia and the outcomes of hepatectomy for hepatocellular carcinoma: a meta-analysis. J Surg Res. 2017;210:99–107. doi: 10.1016/j.jss.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Mehrabi A, Golriz M, Khajeh E, Ghamarnejad O, Probst P, Fonouni H, et al. Meta-analysis of the prognostic role of perioperative platelet count in posthepatectomy liver failure and mortality. Br J Surg. 2018;105:1254–1261. doi: 10.1002/bjs.10906. [DOI] [PubMed] [Google Scholar]
- 26.Lim JH, Choi GH, Choi SH, Lee HS, Kim KS, Choi JS. Ventral segment-preserving right hepatectomy in patients with hepatocellular carcinoma. World J Surg. 2015;39:1034–1043. doi: 10.1007/s00268-014-2894-3. [DOI] [PubMed] [Google Scholar]
- 27.Satou S, Sugawara Y, Tamura S, Yamashiki N, Kaneko J, Aoki T, et al. Discrepancy between estimated and actual weight of partial liver graft from living donors. J Hepatobiliary Pancreat Sci. 2011;18:586–591. doi: 10.1007/s00534-011-0374-9. [DOI] [PubMed] [Google Scholar]
- 28.Mussin N, Sumo M, Lee KW, Choi Y, Choi JY, Ahn SW, et al. The correlation between preoperative volumetry and real graft weight: comparison of two volumetry programs. Ann Surg Treat Res. 2017;92:214–220. doi: 10.4174/astr.2017.92.4.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chapelle T, Op De Beeck B, Huyghe I, Francque S, Driessen A, Roeyen G, et al. Future remnant liver function estimated by combining liver volumetry on magnetic resonance imaging with total liver function on (99m)Tc-mebrofenin hepatobiliary scintigraphy: can this tool predict post-hepatectomy liver failure? HPB (Oxford) 2016;18:494–503. doi: 10.1016/j.hpb.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim DK, Choi JI, Choi MH, Park MY, Lee YJ, Rha SE, et al. Prediction of posthepatectomy liver failure: MRI with hepatocyte-specific contrast agent versus indocyanine green clearance test. AJR Am J Roentgenol. 2018;211:580–587. doi: 10.2214/AJR.17.19206. [DOI] [PubMed] [Google Scholar]