Abstract
From May to November most romaine lettuce shipments in the United States come from California’s Central Coast region, whereas from December to April most come from the Yuma, Arizona, region. During 2017–2018, the 3 outbreaks of Shiga toxin–producing Escherichia coli (STEC) O157:H7 in US romaine lettuce all occurred at the tail end of a region’s production season. During the fall 2018 outbreak, the US Food and Drug Administration (FDA) recommended that suppliers begin labeling romaine packaging so that consumers can identify the product’s harvest region.
We used publicly available data to show that labels may not avert many illnesses in future outbreaks but may reduce suppliers’ financial losses and reduce food loss.
Market data available during both 2018 outbreak investigations showed that there was no romaine production from one of the 2 regions when the first illness onset occurred. That is, at the beginning of an outbreak investigation, market data may allow the FDA to quickly rule out an entire production region as a source of contamination.
Health and safety officials in the United States are charged with keeping consumers safe from foodborne pathogens. Most of the estimated 9.4 million foodborne illnesses from known pathogens that occur annually in the United States are sporadic and not associated with an outbreak. Generally in these cases, the food sources are unknown and there is no practical way to determine the cause behind an individual illness. Conversely, outbreaks are cases in which 2 or more people become sick from the same illness from the same food. Commonalities in food consumption among those who fall ill raise the possibility of finding the contaminated food. During the 2009 to 2015 period, there were approximately 800 foodborne illness outbreaks each year in the United States.1 These outbreaks accounted for approximately 15 000 illnesses, 800 hospitalizations, and 20 deaths.
Mitigating the effects of a foodborne illness outbreak is a challenging public health issue. Health and safety officials are expected to find the contaminated food within the supply chain and consumers’ homes as soon as possible, which requires that they solve a pair of practical problems: they must recognize that an outbreak is occurring and then must identify the food that is causing the outbreak. Both problems have to be solved before a single illness or death can be averted.
Speed and reliability are critical in preventing illness and death, especially when it comes to fresh produce. However, the information available to the US Food and Drug Administration (FDA) is usually old by the time an outbreak is identified because it takes 2 to 3 weeks from when a person consumes contaminated food to when the Centers for Disease Control and Prevention (CDC) identifies the person’s illness as part of a larger outbreak.2 This gap between when illnesses occur and when the FDA starts to gather information makes traceback—identifying the food vector—difficult because consumers have trouble recalling what they ate near the time of their illness onset.3
Often, the tradeoff for speed is reliability. Should officials identify a food as contaminated when epidemiological studies, laboratory results, and traceback are all complete and scientifically defensible? Or should they make recommendations to avoid a food when the information at hand plausibly points to a particular food, knowing that the recommendation may later be proven wrong?
Making a recommendation quickly could prevent some illnesses and deaths. If the recommendation turns out to be wrong, however, no illnesses will be averted and producers and marketing firms that are blameless may incur economic damage, as occurred in 1996 with strawberries or in 2008 with tomatoes.4–6 Between 2009 and 2015, investigators were able to identify the foods that caused outbreaks in only 42% of cases.1 That is, most outbreaks have not yielded enough information for investigators to determine the cause. Even in cases in which the FDA is able to identify the source of the outbreak and communicate details to the public, research suggests that not all consumers receive the public health warnings, nor do all of those who receive warnings act on them.7
In the United States, leafy greens are the fifth most commonly consumed vegetable and are commonly consumed raw.8 From 1988 to 2018, the amount of leafy greens consumed per capita quadrupled.9 Also, leafy greens have been identified as a source of foodborne illness outbreaks since 1988.10 In recent years, the number of studies examining how Shiga toxin–producing Escherichia coli (STEC) contaminates leafy greens have dramatically increased.11–17 The growing and intense interest regarding STEC and leafy greens is attributable in part to the disproportionate number of illnesses and outbreaks associated with leafy greens. After an unprecedentedly large STEC outbreak in 2006 linked to spinach, the leafy greens industry (collectively and without direct federal intervention) established the California and Arizona Leafy Greens Marketing Agreements to implement measures to address safety concerns. Even so, from 2007 to 2017, the CDC identified 40 outbreaks of STEC linked to leafy greens (including lettuce and spinach).18
During 2017 and 2018 in the United States and Canada, there were 3 multistate, multinational foodborne illness outbreaks of STEC O157:H7 associated with the consumption of romaine lettuce. These outbreaks, which occurred in fall 2017, spring 2018, and fall 2018, led to a total of 376 illnesses, 158 hospitalizations, and 7 deaths.19–24 In 2 of the 3 outbreaks, the contaminated production region was identified but the FDA and the CDC were unable to definitively trace the contamination back to a specific farm or harvest date. Members of the public were advised not to consume romaine lettuce, and in 2 cases the FDA requested that all romaine lettuce on the market (including in restaurants and other commercial establishments) be withdrawn and discarded.25
During the fall 2018 outbreak, the FDA recommended that suppliers and distributors label lettuce packages with a harvest location (e.g., Yuma, Arizona, or California’s Central Coast) and harvest date or indicate whether the lettuce was hydroponically or greenhouse grown. Retailers were directed to use in-store signage when labels were not an option (e.g., for unwrapped whole heads of romaine lettuce).
In a review of historically important outbreaks, Goodman et al. identified “the need for fostering collaborative efforts beyond those of traditional public health” and “enhancing diagnostic and technological tools” to allow better responses “to events when information is insufficient for initiating control measures.”26(p1080) Here we address that need by investigating whether the structured schedule of production of romaine lettuce in the United States can help outbreak investigators identify the source of contaminated lettuce more quickly and whether newly required labeling of production sources and harvest dates can be used to prevent illness and reduce economic loss.
METHODS
We obtained publicly available data on daily US romaine lettuce shipments at international and national ports between 2013 and 2018 from the US Department of Agriculture’s Agricultural Marketing Service Web site.27 Included were all shipments via rail, truck, and air reported by rail carriers as well as federal marketing orders, administrative committees, federal or state inspection services, and shippers.
Using the statistical software R (version 3.5.1),28 we calculated the daily average number of shipments during the 6-year period (2013–2018) for each region and then calculated the 7-day moving average of these 6-year daily averages as the mean of the period spanning 3 days before and 3 days after each date. We estimated a 95% confidence interval surrounding each daily average shipment using the standard deviation observed at that date over the 6 years of data. We placed a lower bound on the confidence interval at zero. For the period 2013–2018, we calculated the 7-day moving average share of shipments of romaine lettuce originating from California’s Central Coast; Yuma, Arizona; and other locations that were not implicated in the 3 most recent romaine outbreaks (i.e., other regions of California and Arizona as well as Florida and imports from Canada and Mexico).
We obtained information on 26 outbreaks and 644 illnesses associated with romaine lettuce between 1998 and 2017 by formally requesting National Outbreak Reporting System (NORS) data (maintained by the CDC) on foodborne outbreaks since 1998 in which romaine lettuce was the implicated food.18 Information provided in the reports on the 3 outbreaks and 376 illnesses associated with romaine lettuce in 2017–2018 published by the Public Health Agency of Canada (PHAC) and the CDC (and not included in NORS) was appended to the NORS data19–24 (Appendix Table A, available as a supplement to the online version of this article at http://www.ajph.org). We tabulated the total number of outbreaks by type of pathogen beginning in each month of each year between 1998 and 2018.
For the 3 most recent STEC O157:H7 outbreaks associated with romaine lettuce, we collected information on the dates of onset for the first and last illnesses from the publicly available incident reports provided by the CDC. Information on dates of when the FDA was first notified about the outbreak and when the agency made public health announcements was collected from FDA investigation reports.29–31 We used this information to summarize each event’s timeline, including the first illness onset, the outbreak investigation, and the end of each outbreak. We combined this information with the data on daily US romaine lettuce shipments reported by the Agricultural Marketing Service.
RESULTS
US romaine shipments display a consistent seasonal pattern. Combining shipment data with dates of illness onset can allow investigators to rule out major production regions as the source of illness during an outbreak.
Split and Seasonal Shipments
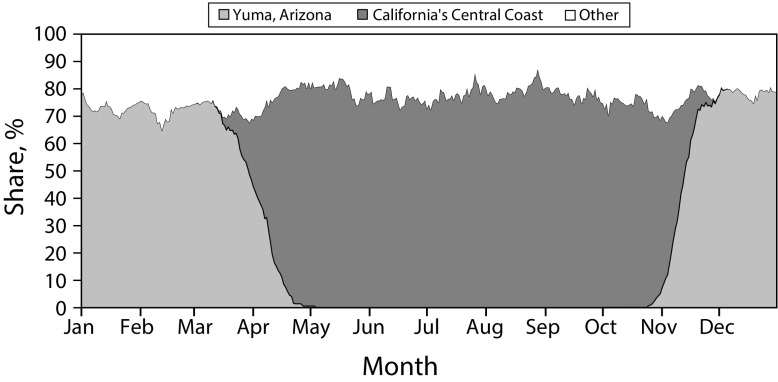
US romaine shipments have been split and seasonal between 2 production regions. During the past 6 years, from about May through November, romaine lettuce originated predominantly from California’s Central Coast (Figure 1). During that time, no production occurred in Yuma, Arizona. Production shifted quickly to Yuma, Arizona, each November, with Yuma production predominantly serving the market through March. Another rapid shift back to California’s Central Coast occurred each April. Outside of this pair of 1-month-long transition periods, the dominant region made up about 75% of shipments; the other 25% of shipments came from other areas in the United States, Mexico, or Canada.
FIGURE 1—
6-Year, 7-Day Moving Average Romaine Lettuce Shipment Shares by Region: United States, 2013–2018
Source. Authors’ calculations using data from the US Department of Agriculture’s Agricultural Marketing Service.27
Note. Six-year daily averages of shipments were calculated for each region over the period 2013–2018, from which the 7-day moving average was calculated as the mean of the period spanning 3 days before and 3 days after each date. The share at each date was calculated for California’s Central Coast; Yuma, Arizona and other locations (other regions of California and Arizona as well as Florida and imports from Canada and Mexico).
Outbreaks Often Precede Transitions
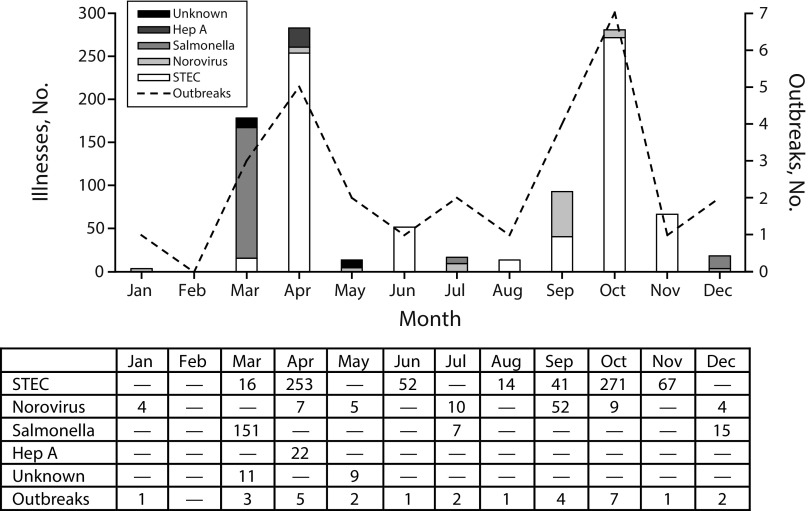
Historically, outbreaks linked to romaine have occurred disproportionately just before the transition from one production region to another. From 1998 to 2018, foodborne illnesses and outbreaks associated with romaine lettuce occurred most frequently during March, April, September, and October (Figure 2), the times of year when romaine production begins to shift from one region to another. STEC illness counts (STEC O157:H7 is included among other strains) peak in April and October.
FIGURE 2—
Total Foodborne Illness Outbreaks and Outbreak-Caused Illnesses Linked to Romaine Lettuce by Month: United States,1998–2018
Source. Authors’ calculations using National Outbreak Reporting System (NORS) data on 1998–2017 outbreaks in which romaine lettuce was the implicated ingredient.18 Additional information (not included in NORS) covering the 3 multistate outbreaks involving romaine during 2017 and 2018 was gathered from Public Health Agency of Canada and Centers for Disease Control and Prevention outbreak reports.19–24
Note. Hep A = hepatitis A; STEC = Shiga toxin–producing Escherichia coli.
Ruling Out Production Regions
Shipment and outbreak timeline analysis indicates how market data can be used to identify potential outbreak sources. During the week prior to the day the first reported illness began in the fall 2017 outbreak—November 5, 2017—15% of romaine shipments came from Yuma, Arizona, and 58% came from California’s Central Coast. By December 21, when PHAC announced that consumers should avoid romaine lettuce,19 no romaine was originating from California’s Central Coast, whereas 69% was originating from Yuma, Arizona. Consumer Reports followed PHAC’s lead on January 4, 2018, recommending that US consumers avoid romaine.32 By that point, romaine shipments from California’s Central Coast had ceased for more than a month.
Ultimately, in the United States, the outbreak sickened 25 individuals, with 9 hospitalizations, 2 cases of hemolytic uremic syndrome—a condition that affects the blood and blood vessels, resulting in the destruction of blood platelets (cells involved in clotting), a low red blood cell count (anemia), and kidney failure—and 1 death.29 In Canada, the outbreak sickened 42 individuals, with 17 hospitalizations and 1 death.19 The FDA never linked this outbreak directly to romaine lettuce (it was directly linked only to leafy greens).29
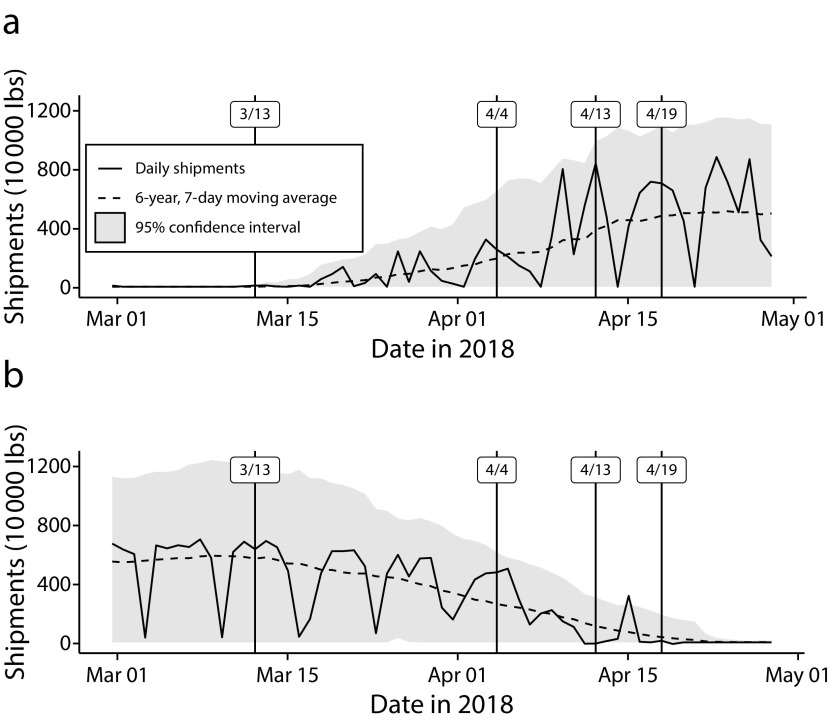
An analysis of the timeline of the 2018 outbreaks revealed that nearly no romaine in the market came from California’s Central Coast at the start of the spring 2018 outbreak or from Yuma, Arizona, at the start of the fall 2018 outbreak. The spring 2018 outbreak was the largest outbreak of STEC O157:H7 since August 2006, when fresh spinach from California’s Central Coast proved to be the source. Beginning on March 13, 2018, and ending in May, there were 210 reported illnesses across 36 states along with 96 hospitalizations, 27 cases of hemolytic uremic syndrome, and 5 deaths.30 The FDA was first notified by the CDC of 2 clusters of foodborne illness on April 4. In Canada, there were 8 reported illnesses, 1 hospitalization, and no deaths.20 During the week before the date of the first illness onset, no romaine was shipped from California’s Central Coast and 71% was shipped from Yuma, Arizona (Figure 3). During the week prior to the April 13 FDA announcement that consumers should avoid chopped romaine from Yuma, Arizona, 50% of romaine came from California’s Central Coast and 26% from Yuma.
FIGURE 3—
Daily Shipments and Notable Outbreak Dates in (a) California’s Central Coast and (b) Yuma, Arizona: Spring 2018
Source. Authors’ calculations using data from the Centers for Disease Control and Prevention, the Agricultural Marketing Service, and the US Food and Drug Administration (FDA).23,27,30
Note. The first illness onset occurred on March 13. The FDA investigation began on April 4. On April 13, the FDA advised consumers to avoid chopped romaine from Yuma, Arizona. On April 19, the FDA advised consumers to avoid all romaine from Yuma. Six-year daily averages of shipments were calculated for each region over the period 2013–2018, from which the 7-day moving average was calculated as the mean of the period spanning 3 days before and 3 days after each date. The confidence interval was estimated via the standard deviation from the 6-year, 7-day moving average observed at that date over the 6 years of data.
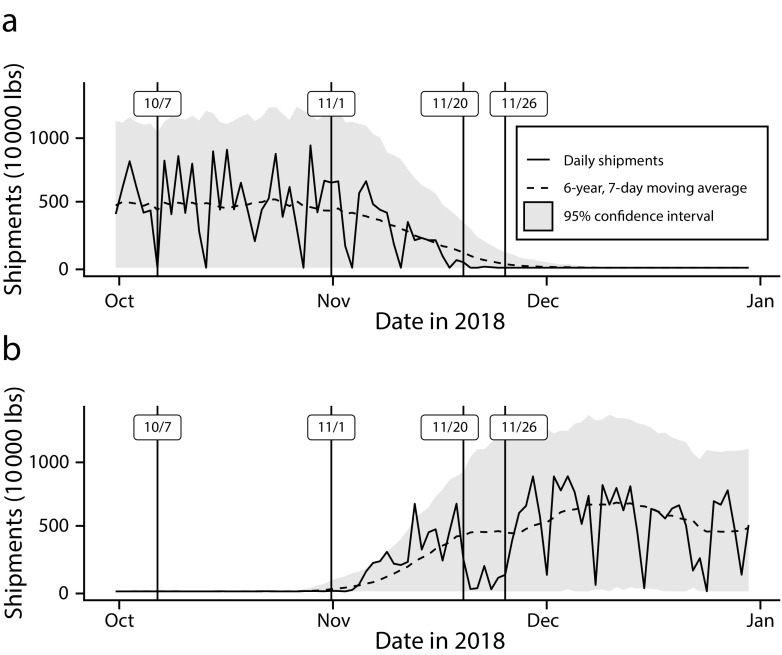
The fall 2018 outbreak resulted in fewer illnesses than the spring 2018 outbreak. Between October and December 2018, there were 62 reported illnesses across 16 states and the District of Columbia, with 25 hospitalizations and 2 cases of hemolytic uremic syndrome associated with STEC O157:H7 in romaine.31 In Canada there were 29 reported illnesses, 10 hospitalizations, and 2 cases of hemolytic uremic syndrome.21 On average, for the week up to the date of the first illness onset—October 7, 2018—75% of romaine shipments came from California’s Central Coast (Figure 4). No romaine was shipped from Yuma, Arizona, until weeks later.
FIGURE 4—
Daily Shipments and Notable Outbreak Dates in (a) California’s Central Coast and (b) Yuma, Arizona: Fall 2018
Note. The first illness onset occurred on October 7. The FDA investigation began on November 1. On November 20, the FDA advised consumers to avoid romaine. On November 26, the FDA advised consumers to avoid romaine from California’s Central Coast. Six-year daily averages of shipments were calculated for each region over the period 2013–2018, from which the 7-day moving average was calculated as the mean of the period spanning 3 days before and 3 days after each date. The confidence interval was estimated via the standard deviation from the 6-year, 7-day moving average observed at that date over the 6 years of data.
Source. Authors’ calculations using data from the Centers for Disease Control and Prevention, the Agricultural Marketing Service, and the US Food and Drug Administration (FDA).24,27,31
By the time the FDA made its first public health announcement advising consumers to avoid all romaine lettuce—November 20, 2018—63% of all romaine was shipped from Yuma, Arizona, during the week prior and 17% was shipped from California’s Central Coast. Subsequent FDA announcements restricted the warning to avoid lettuce from California’s Central Coast on November 26 and from Monterey, San Benito, and Santa Barbara counties on December 13. The last reported illness began on December 4, 2018. Shipments from Yuma, Arizona, dropped immediately after the general romaine warning (November 20) and returned to normal after the region-specific warning (November 26). The FDA and CDC announced that the strain of STEC O157:H7 in the fall 2018 outbreak was similar to that of the 2017 leafy green outbreak and dissimilar to that of the April 2018 outbreak involving Yuma romaine.31
DISCUSSION
Our study established or confirmed 3 facts. The first is that recent multistate STEC outbreaks involving romaine lettuce generally occurred at the tail end of the production seasons in each of the 2 main production areas in the United States: California’s Central Coast region (primarily Monterey County33) and the region surrounding Yuma, Arizona. The seasonality that we identified in these 3 recent outbreaks fits a 2-decade-long seasonal pattern in romaine outbreaks and has implications both for public health monitoring and outbreak response and for further investigation into the source of STEC outbreaks involving romaine.34
We are unable to offer definitive answers as to why this seasonality in romaine outbreaks exists. However, the biophysical and operations management characteristics that affect the likelihood of contamination provide a set of hypotheses to examine. Seasonality in the movement of both domestic and wild animals may affect the level of contamination reaching romaine in the field. E. coli O157:H7 is one of many STEC serogroups that colonize the intestinal tracts of ruminant animals. The organisms are present in manure, and thus domesticated livestock such as cows and wild animals such as deer have the potential to contaminate nearby produce fields or nearby water sources used in produce fields.35
Changes in farm management as production slows down may affect how food safety activities are carried out. Although production shifts from one region to another, many times a single firm operates fields in both regions. Firms have diversified the geography of their production to keep their buyers supplied throughout the year and their machinery and employees productively employed. Many leafy green growers move farm workers, supervisors, trucks and equipment, and even processing facilities back and forth twice a year.36 Preparing for and carrying out this large-scale relocation of personnel and equipment may change how food safety activities are implemented on farms.
In addition, seasonal temperatures may affect both romaine production and bacterial growth. Lettuces such as romaine are very sensitive to heat and cold, as are many bacteria. The temperate climate of California’s Central Coast region, which includes the Salinas valley in Monterey County, is amenable to growing delicate lettuces during the summer and fall. Yuma, Arizona, is generally hot and dry, but in the winter and spring temperatures are favorable for lettuce production, and irrigation is available via rights to Colorado River water. In both regions, lettuce production decreases as temperatures approach a threshold. Maximum temperature in the 3 days preceding sampling has been found to be the most important variable in explaining E. coli contamination levels in leafy greens.37
The second fact is that there is a lag between when illnesses in an outbreak begin and when the FDA becomes aware and begins to investigate the cause of the outbreak. The 3 outbreaks we examined were nearly half over by the time the FDA became aware of them: on average, the FDA began its investigation 28 days after the date of the first illness onset, whereas the last illness onset occurred 60 days later. The outbreak investigations lasted an average of 159 days, more than twice as long as the actual outbreaks. Given that the CDC and FDA have not had evidence indicating that an outbreak is over until weeks after the last illness onset and given that romaine outbreaks tend to occur at the end of the production season, it is unlikely that the new harvest region labeling information would avert many illnesses. By the time public health scientists identify an outbreak and outbreak investigators can reliably point to romaine from one of the 2 major domestic production regions, nearly everything produced for the year from the region in question has been sold.
The third fact is that in spite of the lag between the onset of illnesses from contaminated romaine and FDA awareness of those illnesses, publicly available market data can inform outbreak investigations and public health announcements. Publicly available Agricultural Marketing Service data on shipments can provide the FDA with up-to-date information about the origin of romaine lettuce in the market so that the source of the outbreak can be more quickly identified. Using these market data, the FDA may be able to rule out the region with negligible or no production at the time of the first illness onset, facilitate trace-back investigations, maintain public health with announcements to avoid region-specific romaine, and avoid negative economic outcomes for producers in the regions that are not associated with the outbreak.
Specifically, we found that if an outbreak were to begin between May and November, market data could confirm that no romaine was shipped from Yuma, Arizona, and that Yuma could not be the source. Similarly, market data could confirm that an outbreak beginning between December and April could not have originated in the Central Coast because no romaine was shipped from that region at that time.
On the basis of these 3 facts, we conclude that the FDA’s new requirement for romaine lettuce packages to carry source and harvest date information may reduce financial losses for romaine lettuce suppliers and reduce food loss but that it is unlikely to substantially change public health outcomes. If regional labels had been in use on romaine in the fall 2018 outbreak, and if market data had informed the FDA’s first announcement, it may have mitigated a drop in consumer demand without leading to additional illnesses. Recent outbreaks involving romaine suggest that assessments of the biophysical and operations management characteristics unique to the end of the production season can guide the development of new contamination prevention measures.
ACKNOWLEDGMENTS
This work was part of the US Department of Agriculture’s Economic Research Service intramural research program.
We thank the anonymous reviewers, along with Jean Buzby and Suzanne Thornsbury, for their constructive comments on this article.
Note. The findings and conclusions in this article are those of the authors and should not be construed to represent any official US Department of Agriculture or US government determination or policy.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
No protocol approval was needed for this analysis because publicly available data were used.
Footnotes
See also Majowicz, p. 278.
REFERENCES
- 1.Dewey-Mattia D, Manikonda K, Hall AJ, Wise ME, Crowe SJ. Surveillance for foodborne disease outbreaks—United States, 2009–2015. MMWR Surveill Summ. 2018;67(10):1–11. doi: 10.15585/mmwr.ss6710a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Timeline for reporting cases of E. coli O157 infection. Available at: https://www.cdc.gov/ecoli/reporting-timeline.html. Accessed December 5, 2019.
- 3.Mann JM. A prospective study of response error in food history questionnaires: implications for foodborne outbreak investigation. Am J Public Health. 1981;71(12):1362–1366. doi: 10.2105/ajph.71.12.1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calvin L, Foster W, Solorzano L, Mooney JD, Flores L, Barrios V. Response to a food safety problem in produce. In: Krissoff B, Bohman M, Caswell JA, editors. Global Food Trade and Consumer Demand for Quality. Boston, MA: Springer; 2002. pp. 101–127. [Google Scholar]
- 5.Richards TJ, Patterson PM. The economic value of public relations expenditures: food safety and the strawberry case. J Agric Resour Econ. 1999;24(2):440–462. [Google Scholar]
- 6.Florida Tomato Committee. The recent salmonella outbreak: lessons learned and consequences to industry and public health. 2008. Available at: https://www.govinfo.gov/content/pkg/CHRG-110hhrg61557/pdf/CHRG-110hhrg61557.pdf. Accessed December 5, 2019.
- 7.Mahon BE, Slutsker L, Hutwagner L et al. Consequences in Georgia of a nationwide outbreak of Salmonella infections: what you don’t know might hurt you. Am J Public Health. 1999;89(1):31–35. doi: 10.2105/ajph.89.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Department of Agriculture, Economic Research Service. Food availability (per capita) data system. Available at: https://www.ers.usda.gov/data-products/food-availability-per-capita-data-system/interactive-charts-and-highlights/#fruit. Accessed December 5, 2019.
- 9.US Department of Agriculture, Economic Research Service. Commodity highlights. Available at: https://www.ers.usda.gov/topics/crops/vegetables-pulses/commodity-highlights. Accessed December 5, 2019.
- 10.Rosenblum LS, Mirkin IR, Allen DT, Safford S, Hadler SC. A multifocal outbreak of hepatitis A traced to commercially distributed lettuce. Am J Public Health. 1990;80(9):1075–1079. doi: 10.2105/ajph.80.9.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chase JA, Partyka ML, Bond RF, Atwill ER. Environmental inactivation and irrigation-mediated regrowth of Escherichia coli O157:H7 on romaine lettuce when inoculated in a fecal slurry matrix. PeerJ. 2019;7:e6591. doi: 10.7717/peerj.6591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Erickson MC, Liao J-Y, Payton AS et al. Pre-harvest internalization and surface survival of Salmonella and Escherichia coli O157:H7 sprayed onto different lettuce cultivars under field and growth chamber conditions. Int J Food Microbiol. 2019;291:197–204. doi: 10.1016/j.ijfoodmicro.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Gutiérrez-Rodríguez E, Gundersen A, Sbodio A, Koike S, Suslow TV. Evaluation of post-contamination survival and persistence of applied attenuated E. coli O157:H7 and naturally-contaminating E. coli O157:H7 on spinach under field conditions and following postharvest handling. Food Microbiol. 2019;77:173–184. doi: 10.1016/j.fm.2018.08.013. [DOI] [PubMed] [Google Scholar]
- 14.Kearns EA, Gustafson RE, Castillo SM, Alnughaymishi H, Lim DV, Ryser ET. Rapid large-volume concentration for increased detection of Escherichia coli O157:H7 and Listeria monocytogenes in lettuce wash water generated at commercial facilities. Food Control. 2019;98:481–488. [Google Scholar]
- 15.Kumar GD, Zhu L, Siemens MC et al. Modified coring tool designs reduce iceberg lettuce cross-contamination. J Food Prot. 2019;82(3):454–462. doi: 10.4315/0362-028X.JFP-18-317. [DOI] [PubMed] [Google Scholar]
- 16.O’Flaherty E, Solimini AG, Pantanella F, De Giusti M, Cummins E. Human exposure to antibiotic resistant Escherichia coli through irrigated lettuce. Environ Int. 2019;122:270–280. doi: 10.1016/j.envint.2018.11.022. [DOI] [PubMed] [Google Scholar]
- 17.Söderqvist K, Rosberg AK, Boqvist S, Alsanius B, Mogren L, Vågsholm I. Season and species: two possible hurdles for reducing the food safety risk of Escherichia coli O157 contamination of leafy vegetables. J Food Prot. 2019;82(2):247–255. doi: 10.4315/0362-028X.JFP-18-292. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. National Outbreak Reporting System. Available at: https://wwwn.cdc.gov/norsdashboard. Accessed December 5, 2019.
- 19.Public Health Agency of Canada. Outbreak of E. coli infections linked to romaine lettuce: February 9, 2018, final update. Available at: https://www.canada.ca/en/public-health/services/public-health-notices/2017/public-health-notice-outbreak-e-coli-infections-linked-romaine-lettuce.html. Accessed December 5, 2019.
- 20.Public Health Agency of Canada. Outbreak of E. coli infections linked to romaine lettuce: June 22, 2018, final update. Available at: https://www.canada.ca/en/public-health/services/public-health-notices/2018/public-health-notice-outbreak-e-coli-infections-linked-romaine-lettuce.html. Accessed December 5, 2019.
- 21.Public Health Agency of Canada. Outbreak of E. coli infections linked to romaine lettuce: January 11, 2019, final update. Available at: https://www.canada.ca/en/public-health/services/public-health-notices/2018/outbreak-ecoli-infections-linked-romaine-lettuce.html. Accessed December 5, 2019.
- 22.Centers for Disease Control and Prevention. Multistate outbreak of Shiga toxin-producing Escherichia coli O157:H7 infections linked to leafy greens (January 25, 2018, final update) Available at: https://www.cdc.gov/ecoli/2017/o157h7-12-17/index.html. Accessed December 5, 2019.
- 23.Centers for Disease Control and Prevention. Multistate outbreak of E. coli O157:H7 infections linked to romaine lettuce (June 28, 2018, final update) Available at: https://www.cdc.gov/ecoli/2018/o157h7-04-18/index.html. Accessed December 5, 2019.
- 24.Centers for Disease Control and Prevention. Outbreak of E. coli infections linked to romaine lettuce (January 9, 2019, final update) Available at: https://www.cdc.gov/ecoli/2018/o157h7-11-18/index.html. Accessed December 5, 2019.
- 25.US Food and Drug Administration. Statement from FDA commissioner Scott Gottlieb, MD, on the current romaine lettuce E. coli O157:H7 outbreak investigation. Available at: https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm626716.htm. Accessed December 5, 2019.
- 26.Goodman RA, Posid JM, Popovic T. Investigations of selected historically important syndromic outbreaks: impact and lessons learned for public health preparedness and response. Am J Public Health. 2012;102(6):1079–1090. doi: 10.2105/AJPH.2011.300426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.US Department of Agriculture, Agricultural Marketing Service. Specialty crops market news. Available at: https://www.marketnews.usda.gov/mnp/fv-report-config-step1?type=shipPrice. Accessed December 5, 2019.
- 28.R Core Team. R: a language and environment for statistical computing. Available at: https://www.R-project.org. Accessed December 5, 2019.
- 29.US Food and Drug Administration. FDA ends investigation of E. coli O157:H7 outbreak likely linked to leafy greens. Available at: https://web.archive.org/web/20190422151512/www.fda.gov/Food/RecallsOutbreaksEmergencies/Outbreaks/ucm593896.htm. Accessed December 5, 2019.
- 30.US Food and Drug Administration. FDA investigated multistate outbreak of E. coli O157:H7 infections linked to romaine lettuce from Yuma growing region. Available at: https://www.fda.gov/food/outbreaks-foodborne-illness/fda-investigated-multistate-outbreak-e-coli-o157h7-infections-linked-romaine-lettuce-yuma-growing. Accessed December 5, 2019.
- 31.US Food and Drug Administration. Outbreak investigation of E. coli O157:H7 linked to romaine lettuce grown in California. Available at: https://www.fda.gov/food/outbreaks-foodborne-illness/outbreak-investigation-e-coli-o157h7-linked-romaine-lettuce-grown-ca. Accessed December 5, 2019.
- 32.Calvo T. Avoid romaine lettuce for now, Consumer Reports says. Available at: https://www.consumerreports.org/food-safety/avoid-romaine-lettuce-for-now. Accessed December 5, 2019.
- 33.US Department of Agriculture. 2017 census of agriculture. Available at: https://www.nass.usda.gov/Publications/AgCensus/2017/Full_Report/Volume_1,_Chapter_2_County_Level. Accessed December 5, 2019.
- 34.Turner K, Moua CN, Hajmeer M, Barnes A, Needham M. Overview of leafy greens–related food safety incidents with a California link: 1996 to 2016. J Food Prot. 2019;82(3):405–414. doi: 10.4315/0362-028X.JFP-18-316. [DOI] [PubMed] [Google Scholar]
- 35.Gyles CL. Shiga toxin-producing Escherichia coli: an overview. J Anim Sci. 2007;85(suppl 13):E45–E62. doi: 10.2527/jas.2006-508. [DOI] [PubMed] [Google Scholar]
- 36.Mathews J. Salinas and Yuma are 500 miles apart—but agribusiness is growing them closer. Available at: http://www.publicceo.com/2018/10/salinas-and-yuma-are-500-miles-apart-but-agribusiness-is-growing-them-closer. Accessed December 5, 2019.
- 37.Liu C, Hofstra N, Franz E. Impacts of climate and management variables on the contamination of preharvest leafy greens with Escherichia coli. J Food Prot. 2016;79(1):17–29. doi: 10.4315/0362-028X.JFP-15-255. [DOI] [PubMed] [Google Scholar]