Abstract
The occurrence of hyperpigmentation or hypopigmentation after inflammation is a common condition in dermatology and cosmetology. Since the exact mechanism of its occurrence is not yet known, prevention and treatment are troublesome. Previous studies have confirmed that α-melanocyte-stimulating hormone, stem cell factor and other factors can promote melanogenesis-related gene expression through the activation of signaling pathways. Recent studies have revealed that a variety of inflammatory mediators can also participate in the regulation of melanogenesis in melanocytes. In this review, we summarized that interleukin-18, interleukin-33, granulocyte-macrophage colony stimulating factor, interferon-γ, prostaglandin E2 have the effect of promoting melanogenesis, while interleukin-1, interleukin-4, interleukin-6, interleukin-17 and tumor necrosis factor can inhibit melanogenesis. Further studies have found that these inflammatory factors may activate or inhibit melanogenesis-related signaling pathways (such as protein kinase A and mitogen activated protein kinase) by binding to corresponding receptors, thereby promoting or inhibiting the expression of melanogenesis-related genes and regulating skin pigmentation processes. This suggests that the development of drugs or treatment methods from the perspective of regulating inflammation can provide new ideas and new targets for the treatment of pigmented dermatosis. This review outlines the current understanding of the inflammation factors' roles in melanogenesis.
Keywords: hypopigmentation, hyperpigmentation, inflammatory factor, melanogenesis, pigmented dermatosis
1. Introduction
A coordination system has been formed under the interaction of various cells in the skin. For instance, the cutaneous neuron-immune-endocrine system consists of interaction and coordination between keratinocytes, melanocytes and dendritic Langerhans cells in the epidermis and the components of the dermis such as mast cells, macrophages, fibroblasts and nerve cells (1–3). Allergens, pathogens, chemical stimuli, and physical damage can all lead to skin inflammation (4–7), which is a defense response to exogenous or endogenous stimuli (8). Skin inflammation plays a crucial role in the body, such as resisting the invasion of bacteria and other pathogens and promoting the repair of wounds. Recent studies have revealed that inflammatory cytokines are closely related to skin pigmentation (9,10).
Skin hyperpigmentation or hypopigmentation after inflammation is a clinically common symptom. Various acute or chronic inflammatory skin reactions may cause changes in skin pigmentation (11), such as psoriasis, eczema, or laser surgery. Recent studies have confirmed that interleukin (IL)-1, IL-4, IL-6 and other inflammatory mediators can regulate the proliferation and differentiation of human epidermal melanocytes directly or indirectly and participate in the regulation of melanogenesis in melanocytes (11–13). Treatments that modulate these inflammatory mediators may have great clinical utility in the treatment of some dyschromatosis (14). This review will focus on the role of inflammatory factors in melanogenesis and the mechanisms involved.
2. Process of melanogenesis
Melanocytes originate from the ectodermal neural crest, migrate to the mesenchyme as the embryo develops, and then further migrate to the skin, eye uveal, stria vascularis, vestibular organ, endolymphatic sac and pia mater (15,16). The migration, proliferation, and differentiation of melanoblasts are mainly regulated by regulatory factors secreted by the dorsal neural tube, ectoderm, and keratinocytes such as the fmily of Wingless-type protein (WNT), endothelin 3 (EDN3), and stem cell factor (SCF) (17). Melanogenesis in mature melanocytes occurs in melanosomes. Melanosomes are unique organelles located in the cytoplasm of melanocytes, which contain key enzymes regulating the production of pigments such as tyrosinase (TYR), tyrosinase-related protein-1 (TYRP-1) and tyrosinase-related protein-2 (TYRP-2) (17,18). Activation of the transcription factor microphthalmia-associated transcription factor (MITF) (19–21) results in the upregulation of the expression of key genes such as TYR, TYRP-1 and TYRP-2 (16,22,23), and promotes melanogenesis in melanocytes (17). Mature melanosomes can migrate from the perinuclear region to the dendrites of melanocyte under the regulation of tubulin (kinesin, dynein) (17). In the epidermis, melanocytes are associated with 30 to 40 keratinocytes through dendrites, transferring mature melanosomes into the cytoplasm of keratinocytes (15,24).
3. Signaling pathways regulating melanogenesis
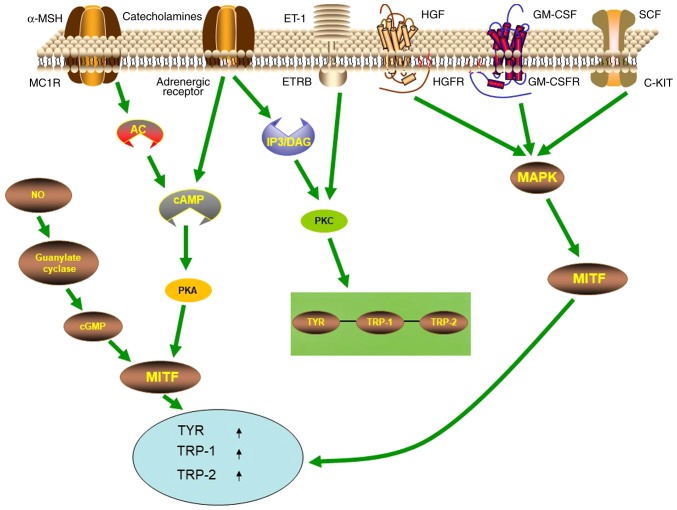
Multiple signaling pathways are involved in the regulation of melanogenesis, with the cyclic AMP (cAMP)/protein kinase A (PKA) signaling pathway being one of the most important signaling pathways (Fig. 1). The most well-known receptor on melanocytes that modulates their function is the melanocortin-1 receptor (MC1R). When α-melanocyte-stimulating hormone (α-MSH) binds to MC1-R on the membrane of melanocytes, it activates adenylate cyclase, increases intracellular cAMP, activates PKA-cAMP response element-binding protein (CREB) pathway, and then increases MITF, promoting melanogenesis (25–28). MC1R is also a major regulator of human pigmentation and is also a melanoma susceptibility gene (28). In addition, signaling pathways such as mitogen activated protein kinase (MAPK), inositol trisphosphate/diacylglycerol (IP3/DAG), WNT, and protein kinase C (PKC) have also been revealed to participate in melanogenesis. The α1 adrenergic receptor can activate the IP3/DAG pathway and increase the intracellular levels of PKC-β and activate tyrosinase (29). SCF, GM-SCF and hepatocyte growth factor (HGF) can activate signaling pathways mediated by the corresponding receptor c-KIT, GM-CSFR, and HGFR, leading to autophosphorylation and activation of MAP kinase, thereby phosphorylating MITF, upregulating the expression of melanogenesis-related enzymes (30–32). The WNT signaling pathway can activate MITF-M promoter (33–35), thereby resulting in upregulation of MITF expression to further regulate melanogenesis. Catecholamines can promote melanogenesis through the cAMP/PKA pathway, while catecholamines also mediate melanogenesis through the activation of PKC-β pathways by α1 and β2 adrenergic receptors (29,36).
Figure 1.
Different signaling pathways regulating melanogenesis. Upon binding to MCIR and adrenergic receptor respectively, α-MSH and catecholamines activate the PKA pathway by increasing cAMP. Then PKA promotes MITF expression, which controls the expression of melanogenesis-related genes TYR, TRP-1 and TRP-2. Upon binding to ETR and adrenergic receptor respectively, ET-1 and catecholamines activate the PKC pathway to promote the expression of TYR, TRP-1 and TRP-2. Upon binding to c-MET, GM-CSFR, and c-KIT and respectively, HGF, GM-CSF, and SCF activate the MAPK pathway to promote the expression of MITF, which in turn increases the expression of TYR, TRP-1 and TRP-2. In addition, NO in the cytoplasm regulates MITF-driven expression of TYR, TRP-1 and TRP-2 through the guanylate cyclase-cGMP pathway. α-MSH, α-melanocyte-stimulating hormone; MC1R, melanocortin-1 receptor; ET-1, endothelin-1; ETR, ET-receptor; HGF, hepatocyte growth factor; GM-CSF, granulocyte-macrophage colony-stimulating factor; GM-CSFR, granulocyte macrophage colony-stimulating factor receptor; SCF, stem cell factor; AC, adenylate cyclase; cAMP, 3′5′-cyclic adenosine monophosphate; PKA, protein kinase A; c-GMP, cyclic guanosine monophosphate; IP3/DAG, inositol trisphosphate/diacylglycerol; PKC, protein kinase C; MAPK, mitogen activated protein kinase; TYR, tyrosinase; TRP-1, tyrosinase-related protein-1; TRP-2, tyrosinase-related protein-2.
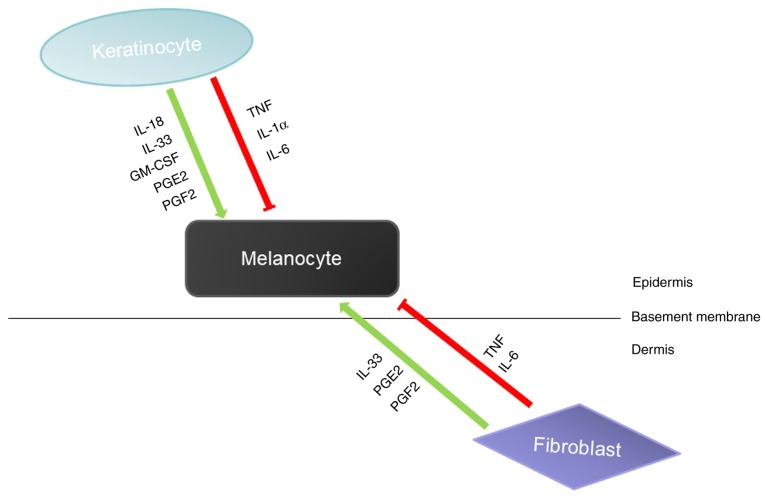
Skin melanogenesis is affected by the epidermal melanin unit, which is mainly composed of keratinocytes and melanocytes. Many of the paracrine factors secreted by keratinocytes can act on melanocytes to promote or inhibit melanogenesis. For example, IL-18, IL-33, GM-CSF can promote melanogenesis, and TNF, IL-1 and IL-6 can inhibit melanogenesis (37,38). In addition to keratinocytes, other types of cells in the skin, such as fibroblasts, also participate in the regulation of melanocytes by producing paracrine factors (Fig. 2). Melanocytes interact with these surrounding cells by expressing corresponding receptors on the cell surface (27). In addition, studies have revealed that paracrine factors can provide a variety of mechanisms to activate DNA repair mechanisms by activating different receptors and signaling pathways to maintain melanocyte homeostasis and prevent UV mutagenesis (28).
Figure 2.
Keratinocyte-derived factors and fibroblast-derived factors that affect melanogenesis in melanocytes through a paracrine effect. Various factors are identified to stimulate (green arrows) or inhibit (red arrows) melanogenesis in melanocytes. Keratinocytes secret factors such as IL-18, IL-33, GM-CSF, PGE2 and PGF2 to stimulate melanocyte melanogenesis as well as TNF, IL-1α and IL-6 to inhibit melanocyte melanogenesis. Fibroblast-derived factors such as IL-33, PGE2 and PGF2 stimulate melanocyte melanogenesis while TNF and IL-6 inhibit melanocyte melanogenesis. IL-18, interleukin-18; IL-33, interleukin-33; GM-CSF, granulocyte-macrophage colony stimulating factor; PGE2, prostaglandin E2; PGF2, prostaglandin F2; TNF, tumor necrosis factor; IL-1α, interleukin-1α; IL-6, interleukin-6.
4. Function and mechanism of inflammatory factors in regulating melanogenesis
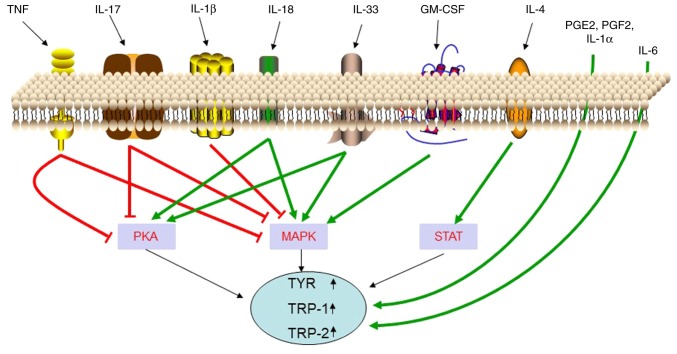
Inflammation is a basic pathological process mainly involving defensive reactions of living tissues with a vascular system in response to the stimulation of various damage factors. The chemical factors involved in mediating inflammatory reactions are called chemical mediators or inflammatory mediators. The inflammatory mediators in the skin are mainly secreted by Th cells, lymphocytes, monocytes-macrophages, dendritic cells, and the like. Th cells are mainly classified as Th1 and Th2 cells (39). Th1 cells play an important role in cellular immune responses, secreting cytokines such as interferon-γ (IFN-γ), tumor necrosis factor (TNF), IL-2, IL-3, GM-CSF; Th2 cells play a key part in humoral immune responses, secreting IL-4, IL-5, IL-10, IL-13, IL-3, GM-CSF as well as other cytokines (40,41). In a normal body, Th1 cytokines and Th2 cytokines are in equilibrium. When the body suffers from a certain disease, the balance between Th1 and Th2 is impaired, and there is a drift toward Th1 or Th2 (39). T helper cell 17 (Th17) is a newly discovered T cell subset that secretes IL-17, IL-6, IL-21 and IL-22 and participates in the occurrence of innate immunity and certain inflammations by secreting IL-17, IL-6 and TNF-α. Studies have revealed that keratinocytes can secrete IL-18, TNF, IL-1, GM-CSF, INF-γ, and IL-3, fibroblasts can secrete IL-33, TNF, IL-6, and IL-8, and melanocytes can secrete INF-β, IL-1, IL-8, IL-10 and TNF-α (37,38,42). The main inflammatory mediators that are secreted by various types of cells in the skin are presented in Table I. Recent studies have revealed that local inflammatory factors of the skin may be involved in the regulation of skin pigmentation (Fig. 3). The function and mechanisms of these inflammatory factors in regulating melanogenesis are presented in Table II.
Table I.
Inflammatory mediators secreted by various types of cells in the skin.
| Cell type | Inflammatory factors |
|---|---|
| Mononuclear macrophages | INF-γ, TNF, IL-1, GM-CSF, IL-6, IL-8, IL-12, IL-18, IL-10 |
| Neutrophils | IL-1β, TNF, IL-6, IL-8, IL-15, IFN-γ |
| Th1 cells | IFN-γ, TNF, IL-2, IL-3, GM-CSF |
| Th2 cells | IL-4, IL-5, IL-6, IL-10, IL-13, IL-3, GM-CSF |
| Th17 cells | IL-17, IL-6, IL-21, IL-22, TNF-α |
| Mast cells | TNF, IL-1, IL-4, IL-6, IL-8, IL-10, IL-13, IFN-γ |
| Dendritic cells | IL-2, IL-4, IL-5, IL-12, INF-γ |
| Keratinocytes | IL-18, TNF, IL-1, GM-CSF, INF-γ, IL-33 |
| Melanocytes | INF-β, IL-1, IL-8, IL-10, TNF-α |
| Fibroblasts | IL-33, TNF, IL-6, IL-8 |
Th1, T helper 1; IFN-γ, interferon-γ; TNF, tumor necrosis factor; IL, interleukin; GM-CSF, granulocyte-macrophage colony stimulating factor.
Figure 3.
Cytokines that inhibit or stimulate melanogenesis. Cytokines such as TNF, IL-17 and IL-1β inhibit melanogenesis by suppressing the PKA or MAPK pathway. While cytokines such as IL-18, IL-33 and GM-CSF stimulate melanogenesis by stimulating the PKA or MAPK pathway. IL-4 stimulates melanogenesis by stimulating the STAT pathway. PGE2, PGF2, IL-1α and IL-6 stimulate melanogenesis through unidentified signaling pathways. TNF, tumor necrosis factor; IL-17, interleukin-17; IL-1β, interleukin-1β; IL-18, interleukin-18; IL-33, interleukin-33; GM-CSF, granulocyte-macrophage colony stimulating factor; IL-4, interleukin-4; PGE2, prostaglandin E2; PGF2, prostaglandin F2; IL-1α, interleukin-1α; IL-6, interleukin-6; PKA, protein kinase A; MAPK, mitogen activated protein kinase; STAT, signal transducer and activator of transcription; TYR, tyrosinase; TRP-1, tyrosinase-related protein-1; TRP-2, tyrosinase-related protein-2.
Table II.
Function and mechanisms of inflammatory factors in the regulation of melanogenesis.
| Factor | Experimental cells | Effect on melanogenesis | Mechanisms | (Refs.) |
|---|---|---|---|---|
| IL-18 | Keratinocyte | Promotion | Increasing tyrosinase activity and upregulating TYRP-1 and TYRP-2 expression | (43) |
| IL-33 | Melanocytes | Promotion | Promoting MITF, TYR, TYRP-1, TYRP-2 expression by activating the p38/MAPK and PKA pathways | (14) |
| GM-CSF | Melanocytes | Promotion | Promoting melanocyte proliferation and melanin synthesis | (17) |
| PGE2 and PGF2α | Keratinocytes | Promotion | Stimulating melanocyte dendrite formation through a cAMP-dependent pathway | (62) |
| IFN-γ | B16F10 | Inhibition | Blocking maturation of melanosome and upregulating STAT1 phosphorylation | (46,72) |
| TNF | Melanocytes, primary pooled human keratinocytes | Inhibition | Inhibiting melanin formation through PKA and MAPK signaling pathways in combination with IL-17 | (10) |
| IL-1α | Primary melanocytes, swine skin | Promotion | Combination of KGF increases melanin deposition | (79) |
| IL-1β | Melanoma cell lines (LB2259-MEL and CP50-MEL) | Inhibition | Downregulating MITF-M expression through NF-κB and JNK pathways | (74) |
| IL-4 | Melanocytes | Inhibition | Downregulating the expression of MITF, TYRP-1, TYRP-2 through the JAK2-STAT6 signaling pathway | (13) |
| IL-6 | Melanocytes | Inhibition | Decreasing tyrosinase activity | (12) |
| IL-17 | Melanocytes, primary pooled human keratinocytes | Inhibition | Inhibiting melanin formation through PKA and MAPK signaling pathways in combination with TNF | (10) |
TYRP-1, tyrosinase-related protein-1; TYRP-2, tyrosinase-related protein-2; MITF, microphthalmia-associated transcription factor; TYR, tyrosinase; PKA, protein kinase A; MAPK, mitogen activated protein kinase; JNK, c-Jun N-terminal kinase; JAK-STAT, Janus kinase-signal transducer and activator of transcription.
IL-18 is produced by inflammatory stimuli in Langerhans cells (LC), dendritic cells (DC), Kupffer cells, activated monocytes/macrophages, and keratinocytes in the epidermis (43–45). IL-18 has been revealed to increase the cascade expression of MITF and downstream enzymes by activating the p38/MAPK and PKA pathways, and thus promote melanogenesis and upregulate TYRP-1 and TYRP-2 expression (43,46). These results suggest that IL-18 may participate in the regulation of pigmentation by regulating melanocytes.
IL-33 can induce mast cells to produce pro-inflammatory cytokines and chemokines (47–51), thereby activating macrophages (52–54), CD4+T cells, basophils, dendritic cells and neutrophils (47,55–58), and promoting skin inflammation. It has been revealed that IL-33 mRNA is expressed in multiple organs in humans (including the skin), and in particular, relatively abundant IL-33 mRNA is found in keratinocytes and fibroblasts (59,60). Research has revealed that IL-33 can improve melanin biosynthesis in NHEM and promote the expression of MITF and its downstream-regulated tyrosine, TYRP-1, and TYRP-2 through the activation of MAPK and PKA pathways (14), thereby promoting melanogenesis.
In addition, granulocyte-macrophage colony-stimulating factor (GM-CSF) which is produced by mononuclear macrophages, keratinocytes and Th cells, has been revealed to promote melanocyte proliferation and melanin synthesis (17). Wu et al revealed that increased serum levels of GM-CSF may be used as the serum biomarkers to predict the prognosis of TCAM (transplantation of cultured autologous melanocytes) when vitiligo patients are treated (61).
Prostaglandin E2 (PGE2) and PGF2α which are produced by fibroblasts and keratinocytes have been revealed to stimulate dendritic cell formation and activate tyrosinase in melanocytes through their dependence on the cAMP signaling pathway and phospholipase C (PLC) (62,63). Ma et al revealed that PGE2 is important in melanosome transfer by promoting filopodia delivery (including miniaturization of melanosome, filopodia formation, and broadening diameter of filopodia) and the number of shedding spheroid granules in primary melanocytes (MCs), but has no effects on morphological observation of KCs (64).
As one of the most important endogenous mediators of immunity and inflammation, IFN-γ is also a common secretory cytokine in the skin (46). As a pro-inflammatory cytokine, IFN-γ is mainly secreted by Th1 lymphocytes, CD8+ cytotoxic T lymphocytes and NK cells (65). Other cells, including antigen-presenting cells, B cells and NKT cells, can also secrete IFN-γ (66–68). Recent studies have demonstrated that the local accumulation of IFN-γ through melanocyte-specific CD8+ T cells plays an important role in skin discoloration spots in various mouse models of vitiligo (69,70). Yang et al reported that increased IFN-γ is essential for the pathogenesis of vitiligo by inducing apoptosis of melanocytes (71). Natarajan et al revealed that IFN-γ signaling blocks maturation of melanosomes by regulating pigmentation genes (72). Moreover, IFN-γ has been revealed to regulate melanogenesis by upregulating STAT1 phosphorylation, and its inhibiting effect can be restrained by JAK1 inhibitors. Studies have also revealed that IFN-γ inhibits IL-18-induced melanogenesis (46).
TNF is a homotrimeric cytokine, secreted mainly by monocytes and macrophages, and also by keratinocytes, dendritic cells, Th1, Th17 and Th22. It functions by binding to two different receptors: TNFR1/p55 and TNFR2/p75 (9). TNF not only induces inflammation through the activation of vascular endothelial cells and immune cells, but also acts as an important regulator of lymphoid tissue development by controlling apoptosis (9). Elevated levels of TNF have been revealed at sites of inflammation in several autoimmune diseases, and inflammatory symptoms have generally decreased after neutralization of TNF. For instance, higher expression levels of TNF, TNFR1 and TNFR2 are observed in psoriasis (73). Studies have revealed that after treatment of melanocytes with both IL-17 and TNF for 24–48 h, the levels of c-KIT, MC1-R, MITF, and TYRP-2 were on the decrease, and the levels of tyrosinase and melanin were significantly reduced (10). It has been revealed that, through the combination with IL-17, TNF can inhibit melanogenesis by PKA and MAPK signaling pathways (9,10). Blocking TNF can lead to rapid restoration of pigmentation gene expression in psoriatic lesions. This suggests that anti-TNF has the potential of treating pigmented dermatosis (10).
IL-1 is an important pro-inflammatory cytokine in innate immunity that stimulates the differentiation and function of immune surveillance cells and contributes to increased tumor invasiveness, metastasis, and angiogenesis under chronic inflammatory conditions (74). IL-1α is an inflammatory mediator mainly produced by Langerhans cells, and is also secreted by melanocytes and keratinocytes. Its signal transduction is initiated by binding to IL-1 receptor type I (IL-1Rα chain) (75), which can inhibit tyrosinase activity and melanogenesis (12,74). Of its many activities, IL-1α also stimulates human fibroblasts to produce keratinocyte growth factor (KGF) (76). Keratinocytes store a large amount of active IL-1α, express IL-1 receptors (77) and produce more IL-1α upon ultraviolet B (UVB) exposure (78). KGF is thought to induce TYR expression in primary melanocytes (79). The combination of KGF and IL-1α increases melanin deposition and they may be involved in the initial stage of human Solar lentigines lesion formation (79). Although they share only 24% identity in protein sequence, IL-1β and IL-1α fold in a highly similar manner and recognize the same receptor, the type I IL-1 receptor (IL-1RI) (80). After treatment of a panel of melanoma cell lines with IL-1β, it was observed that most of the MITF-M was inhibited and was NF-κB- and JNK-dependent. The inactivation of these two pathways could eliminate the inhibitory effects of IL-1β on melanin, which indicated that IL-1β could downregulate MITF-M through NF-kB and JNK pathways, thereby inhibiting melanogenesis (74).
IL-4 is a cytokine mainly secreted by Th2 cells and can also be produced by CD8-positive cytotoxic T cells, basophils, eosinophils, and mast cells in chronic inflammation (81,82). IL-4 plays a key role in the generation of the major mediator IgE in hypersensitivity as well as in the induction of inflammation, contributing to the autoimmunity of the body (83). IL-4 is involved in the maintenance of Th2 lymphocytes and acts as an autocrine growth factor of differentiated Th2 cells (84). It is hypothesized that vitiligo development is directly affected by the imbalance of the Th1/Th2 response (85). Nouri-Koupaee et al revealed the Th1 and Th2 response profiles in vitiligo by assessing IFN-γ and IL-4. This study revealed significant increases in IFN-γ and marked decreases of IL-4 in patients when compared to controls (86). It has also been revealed that IL-4 downregulates the expression of MITF, TYRP-1, and TYRP-2 through the JAK2/STAT6 signaling pathway and thus inhibits melanogenesis (13).
IL-6 is secreted by keratinocytes, epidermal cells, fibroblasts and dermal endothelial cells and is involved in the regulation of various biological responses including immune response, inflammation, hematopoiesis, and tumorigenesis by regulating cell growth, survival, and differentiation (87). Research has revealed that IL-6 decreases tyrosinase activity and melanogenesis (12).
IL-17 is a pro-inflammatory cytokine produced mainly by Th17 cells, and also by other immune cells, including neutrophils, natural killer cells, mast cells, αβ and γδT cells (88). The most well-known function of IL-17 is to prevent bacterial and fungal infections (88). IL-17 has a variety of inflammatory effects, resulting in the release of large amounts of cytokines from a variety of cells, such as epithelial cells, endothelial cells, and fibroblasts (89). Studies have revealed that IL-17 can bind to TNF to inhibit the signaling pathway for melanogenesis, thereby inhibiting melanogenesis (10). The function and mechanisms of these inflammatory factors in regulating melanogenesis are presented in Table II.
It should be noted that the IFN-γ-related data were acquired from a murine melanoma model (B16F10) and IL-1α-related data were based on observations from porcine skin. Therefore, whether their effects on melanogenesis in human melanocytes are the same still requires confirmation by subsequent experiments.
5. Post-inflammatory hyperpigmentations and hypopigmentations can be treated by regulating local inflammatory factors
In clinical practice, various treatments can be effective for post-inflammatory hyperpigmentations and hypopigmentations by influencing inflammatory factors. For example, chloasma is a postinflammatory hyperpigmented disease caused by many factors such as heredity, ultraviolet radiation, pregnancy, hormone therapy, cosmetics, and phototoxic drugs (90). Kojic acid, hydroquinone, and tranexamic acid are commonly used to treat melasma (91). It is well-known that their inhibitory effect on tyrosine activity or melanocyte-specific cytotoxicity is the decolorization mechanism (92,93). In recent years, it has been revealed that kojic acid also inhibits the melanogenesis of melanocytes by promoting the expression of IL-6 in keratinocytes. Resveratrol was revealed to play an important role in ameliorating inflammation, including skin inflammation and reducing inflammatory injury in HaCaT cells (94). Studies have also reported that resveratrol inhibits melanin synthesis to treat hyperpigmented diseases (95). Therefore, resveratrol may also affect melanogenesis by regulating inflammatory factors.
Although the causes of vitiligo are not completely clear, inflammation has been revealed to play a role in its pathogenesis (96). Certain studies revealed that higher expression of pro-inflammatory cytokines had an inhibitory effect on pigmentation in vitiligo lesions (97,98). For example, Kim et al (99) revealed that increased expression of TNF-α in keratinocytes of the lesion area in vitiligo patients inhibited the secretion of melanocyte growth factor from KCs. Barygina et al suggested that low-dose IL-4, β-endorphin, bFGF and IL-10 may be considered as new therapeutic tools for vitiligo treatment (100). Studies have revealed that 308 nm excimer laser can significantly reduce the level of TNF-α in lesions (101), thereby promoting MC function. Various studies reported that the expression of IL-4, TNF-α and other inflammatory cytokines was downregulated after topical application of tacrolimus in lesions of vitiligo (102,103). Methotrexate (MTX) is used in the treatment of autoimmune diseases to decrease T cells that produce TNF-α, which is a key step in the development of vitiligo (104). A study by Alghamdi and Khurrum revealed that oral MTX was a safe and effective therapeutic approach for vitiligo, however, due to the fact that this was a small uncontrolled pilot study, further research needs to be carried out (105). Afamelanotide is a potent and longer-lasting synthetic analogue of naturally occurring α-MSH, which is decreased in vitiligo. Grimes et al (106) found that NB-UVB combined with afamelanotide is safe and effective and that afamelanotide represents a potentially effective treatment for vitiligo, however this still requires further studies. The aforementioned findings indicated that the external use of medications, light therapy and other treatments may serve to treat inflammation related-hyperpigmentations or hypopigmentations by regulating the expression of inflammatory factors associated with melanin production.
6. Conclusion and outlook
Studies have revealed that a variety of inflammatory factors can promote or inhibit the melanogenesis of melanocytes through different mechanisms, suggesting that the development of medicine or therapies from the perspective of inflammation regulation can provide new ideas and new targets for the treatment of pigmented dermatosis. It is widely considered that the regulatory network of inflammation is very complex, since all types of inflammatory cells are involved in the activation and release of inflammatory mediators. The imbalance of inflammatory factors related to T-cell subsets plays an important role in the development of various skin diseases, however, the relationship between imbalance or changes of T-cell subsets and melanogenesis has yet to be confirmed by further experiments.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Fundamental Research Funds for the Central Universities of Central South University (no. 2017zzts890), the National Natural Science Foundation of China (no. 81703101) and the Natural Science Foundation of Hunan Province (nos. 2018JJ3788 and 2018JJ3793).
Availability of data and materials
The datasets used during the present study are available from the corresponding author upon reasonable request.
Authors' contributions
CF and JC designed and wrote the paper. JH and QZ designed and supervised the study. JL, LY, XT, LK, SP, YO, LJ, YD, XZ, SL and YY analyzed and interpreted the data. All authors have read and approved the final manuscript and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no interests.
References
- 1.Gröne A. Keratinocytes and cytokines. Vet Immunol Immunopathol. 2002;88:1–12. doi: 10.1016/S0165-2427(02)00136-8. [DOI] [PubMed] [Google Scholar]
- 2.Skobowiat C, Dowdy JC, Sayre RM, Tuckey RC, Slominski A. Cutaneous hypothalamic-pituitary-adrenal axis homolog: Regulation by ultraviolet radiation. Am J Physiol Endocrinol Metab. 2011;301:E484–E493. doi: 10.1152/ajpendo.00217.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weiss E, Mamelak AJ, La Morgia S, Wang B, Feliciani C, Tulli A, Sauder DN. The role of interleukin 10 in the pathogenesis and potential treatment of skin diseases. J Am Acad Dermatol. 2004;50:657–678. doi: 10.1016/j.jaad.2003.11.075. [DOI] [PubMed] [Google Scholar]
- 4.Martin SF. Contact dermatitis: From pathomechanisms to immunotoxicology. Exp Dermatol. 2012;21:382–389. doi: 10.1111/j.1600-0625.2012.01471.x. [DOI] [PubMed] [Google Scholar]
- 5.Miller LS, Cho JS. Immunity against Staphylococcus aureus cutaneous infections. Nat Rev Immunol. 2011;11:505–518. doi: 10.1038/nri3010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Behrends U, Peter RU, Hintermeier-Knabe R, Eissner G, Holler E, Bornkamm GW, Caughman SW, Degitz K. Ionizing radiation induces human intercellular adhesion molecule-1 in vitro. J Invest Dermatol. 1994;103:726–730. doi: 10.1111/1523-1747.ep12398607. [DOI] [PubMed] [Google Scholar]
- 7.Fuchs J, Kern H. Modulation of UV-light-induced skin inflammation by D-alpha-tocopherol and L-ascorbic acid: A clinical study using solar simulated radiation. Free Radic Biol Med. 1998;25:1006–1012. doi: 10.1016/S0891-5849(98)00132-4. [DOI] [PubMed] [Google Scholar]
- 8.Basler K, Brandner JM. Tight junctions in skin inflammation. Pflugers Arch. 2017;469:3–14. doi: 10.1007/s00424-016-1903-9. [DOI] [PubMed] [Google Scholar]
- 9.Grine L, Dejager L, Libert C, Vandenbroucke RE. An inflammatory triangle in psoriasis: TNF, type I IFNs and IL-17. Cytokine Growth Factor Rev. 2015;26:25–33. doi: 10.1016/j.cytogfr.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 10.Wang CQF, Akalu YT, Suarez-Farinas M, Gonzalez J, Mitsui H, Lowes MA, Orlow SJ, Manga P, Krueger JG. IL-17 and TNF synergistically modulate cytokine expression while suppressing melanogenesis: Potential relevance to psoriasis. J Invest Dermatol. 2013;133:2741–2752. doi: 10.1038/jid.2013.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Slominski A, Tobin DJ, Shibahara S, Wortsman J. Melanin pigmentation in mammalian skin and its hormonal regulation. Physiol Rev. 2004;84:1155–1228. doi: 10.1152/physrev.00044.2003. [DOI] [PubMed] [Google Scholar]
- 12.Swope VB, Abdel-Malek Z, Kassem LM, Nordlund JJ. Interleukins 1 alpha and 6 and tumor necrosis factor-alpha are paracrine inhibitors of human melanocyte proliferation and melanogenesis. J Invest Dermatol. 1991;96:180–185. doi: 10.1111/1523-1747.ep12460991. [DOI] [PubMed] [Google Scholar]
- 13.Choi H, Choi H, Han J, Jin SH, Park JY, Shin DW, Lee TR, Kim K, Lee AY, Noh M. IL-4 inhibits the melanogenesis of normal human melanocytes through the JAK2-STAT6 signaling pathway. J Invest Dermatol. 2013;133:528–536. doi: 10.1038/jid.2012.331. [DOI] [PubMed] [Google Scholar]
- 14.Zhou J, Song J, Ping F, Shang J. Enhancement of the p38 MAPK and PKA signaling pathways is associated with the pro-melanogenic activity of Interleukin 33 in primary melanocytes. J Dermatol Sci. 2014;73:110–116. doi: 10.1016/j.jdermsci.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 15.Tsatmali M, Ancans J, Thody AJ. Melanocyte function and its control by melanocortin peptides. J Histochem Cytochem. 2002;50:125–133. doi: 10.1177/002215540205000201. [DOI] [PubMed] [Google Scholar]
- 16.Costin GE, Hearing VJ. Human skin pigmentation: Melanocytes modulate skin color in response to stress. FASEB J. 2007;21:976–994. doi: 10.1096/fj.06-6649rev. [DOI] [PubMed] [Google Scholar]
- 17.Videira IF, Moura DF, Magina S. Mechanisms regulating melanogenesis. An Bras Dermatol. 2013;88:76–83. doi: 10.1590/S0365-05962013000100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yamaguchi Y, Brenner M, Hearing VJ. The regulation of skin pigmentation. J Biol Chem. 2007;282:27557–27561. doi: 10.1074/jbc.R700026200. [DOI] [PubMed] [Google Scholar]
- 19.Seong ZK, Lee SY, Poudel A, Oh SR, Lee HK. Constituents of cryptotaenia japonica inhibit melanogenesis via CREB- and MAPK-associated signaling pathways in murine B16 melanoma cells. Molecules. 2016;21(pii):E1296. doi: 10.3390/molecules21101296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Campos PM, Prudente AS, Horinouchi CD, Cechinel-Filho V, Fávero GM, Cabrini DA, Otuki MF. Inhibitory effect of GB-2a (I3-naringenin-II8-eriodictyol) on melanogenesis. J Ethnopharmacol. 2015;174:224–229. doi: 10.1016/j.jep.2015.08.015. [DOI] [PubMed] [Google Scholar]
- 21.Tsao YT, Huang YF, Kuo CY, Lin YC, Chiang WC, Wang WK, Hsu CW, Lee CH. Hinokitiol inhibits melanogenesis via AKT/mTOR signaling in B16F10 mouse melanoma cells. Int J Mol Sci. 2016;17:248. doi: 10.3390/ijms17020248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hirobe T. Role of keratinocyte-derived factors involved in regulating the proliferation and differentiation of mammalian epidermal melanocytes. Pigment Cell Res. 2005;18:2–12. doi: 10.1111/j.1600-0749.2004.00198.x. [DOI] [PubMed] [Google Scholar]
- 23.Schallreuter KU, Kothari S, Chavan B, Spencer JD. Regulation of melanogenesis-controversies and new concepts. Exp Dermatol. 2008;17:395–404. doi: 10.1111/j.1600-0625.2007.00675.x. [DOI] [PubMed] [Google Scholar]
- 24.Lin JY, Fisher DE. Melanocyte biology and skin pigmentation. Nature. 2007;445:843–850. doi: 10.1038/nature05660. [DOI] [PubMed] [Google Scholar]
- 25.Park HY, Kosmadaki M, Yaar M, Gilchrest BA. Cellular mechanisms regulating human melanogenesis. Cell Mol Life Sci. 2009;66:1493–1506. doi: 10.1007/s00018-009-8703-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schiaffino MV. Signaling pathways in melanosome biogenesis and pathology. Int J Biochem Cell Biol. 2010;42:1094–1104. doi: 10.1016/j.biocel.2010.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yuan XH, Jin ZH. Paracrine regulation of melanogenesis. Br J Dermatol. 2018;178:632–639. doi: 10.1111/bjd.16387. [DOI] [PubMed] [Google Scholar]
- 28.Swope VB, Abdel-Malek ZA. MC1R: Front and center in the bright side of dark eumelanin and DNA repair. Int J Mol Sci. 2018;19(pii):E2667. doi: 10.3390/ijms19092667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grando SA, Pittelkow MR, Schallreuter KU. Adrenergic and cholinergic control in the biology of epidermis: Physiological and clinical significance. J Invest Dermatol. 2006;126:1948–1965. doi: 10.1038/sj.jid.5700151. [DOI] [PubMed] [Google Scholar]
- 30.Bonaventure J, Domingues MJ, Larue L. Cellular and molecular mechanisms controlling the migration of melanocytes and melanoma cells. Pigment Cell Melanoma Res. 2013;26:316–325. doi: 10.1111/pcmr.12080. [DOI] [PubMed] [Google Scholar]
- 31.Besmer P, Murphy JE, George PC, Qiu FH, Bergold PJ, Lederman L, Snyder HW, Jr, Brodeur D, Zuckerman EE, Hardy WD. A new acute transforming feline retrovirus and relationship of its oncogene v-kit with the protein kinase gene family. Nature. 1986;320:415–421. doi: 10.1038/320415a0. [DOI] [PubMed] [Google Scholar]
- 32.Yarden Y, Kuang WJ, Yang-Feng T, Coussens L, Munemitsu S, Dull TJ, Chen E, Schlessinger J, Francke U, Ullrich A. Human proto-oncogene c-kit: A new cell surface receptor tyrosine kinase for an unidentified ligand. EMBO J. 1987;6:3341–3351. doi: 10.1002/j.1460-2075.1987.tb02655.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dorsky RI, Raible DW, Moon RT. Direct regulation of nacre, a zebrafish MITF homolog required for pigment cell formation, by the Wnt pathway. Genes Dev. 2000;14:158–162. [PMC free article] [PubMed] [Google Scholar]
- 34.Flaherty KT, Hodi FS, Fisher DE. From genes to drugs: Targeted strategies for melanoma. Nat Rev Cancer. 2012;12:349–361. doi: 10.1038/nrc3218. [DOI] [PubMed] [Google Scholar]
- 35.Widlund HR, Horstmann MA, Price ER, Cui J, Lessnick SL, Wu M, He X, Fisher DE. Beta-catenin-induced melanoma growth requires the downstream target Microphthalmia-associated transcription factor. J Cell Biol. 2002;158:1079–1087. doi: 10.1083/jcb.200202049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jung E, Lee J, Huh S, Lee J, Kim YS, Kim G, Park D. Phloridzin-induced melanogenesis is mediated by the cAMP signaling pathway. Food Chem Toxicol. 2009;47:2436–2440. doi: 10.1016/j.fct.2009.06.039. [DOI] [PubMed] [Google Scholar]
- 37.Satomi H, Wang B, Fujisawa H, Otsuka F. Interferon-beta from melanoma cells suppresses the proliferations of melanoma cells in an autocrine manner. Cytokine. 2002;18:108–115. doi: 10.1006/cyto.2002.1028. [DOI] [PubMed] [Google Scholar]
- 38.Mattei S, Colombo MP, Melani C, Silvani A, Parmiani G, Herlyn M. Expression of cytokine/growth factors and their receptors in human melanoma and melanocytes. Int J Cancer. 1994;56:853–857. doi: 10.1002/ijc.2910560617. [DOI] [PubMed] [Google Scholar]
- 39.Mosmann TR, Sad S. The expanding universe of T-cell subsets: Th1, Th2 and more. Immunol Today. 1996;17:138–146. doi: 10.1016/0167-5699(96)80606-2. [DOI] [PubMed] [Google Scholar]
- 40.O'Garra A. Cytokines induce the development of functionally heterogeneous T helper cell subsets. Immunity. 1998;8:275–283. doi: 10.1016/S1074-7613(00)80533-6. [DOI] [PubMed] [Google Scholar]
- 41.Reiner SL, Seder RA. Dealing from the evolutionary pawnshop: How lymphocytes make decisions. Immunity. 1999;11:1–10. doi: 10.1016/S1074-7613(00)80076-X. [DOI] [PubMed] [Google Scholar]
- 42.Bennicelli JL, Guerry D., VI Production of multiple cytokines by cultured human melanomas. Exp Dermatol. 1993;2:186–190. doi: 10.1111/j.1600-0625.1993.tb00031.x. [DOI] [PubMed] [Google Scholar]
- 43.Zhou J, Shang J, Song J, Ping F. Interleukin-18 augments growth ability of primary human melanocytes by PTEN inactivation through the AKT/NF-κB pathway. Int J Biochem Cell Biol. 2013;45:308–316. doi: 10.1016/j.biocel.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 44.Yun W, Li C. JNK pathway is required for TNCB-induced IL-18 expression in murine keratinocytes. Toxicol In Vitro. 2010;24:1064–1069. doi: 10.1016/j.tiv.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 45.Wittmann M, Macdonald A, Renne J. IL-18 and skin inflammation. Autoimmun Rev. 2009;9:45–48. doi: 10.1016/j.autrev.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 46.Zhou J, Ling J, Wang Y, Shang J, Ping F. Cross-talk between interferon-gamma and interleukin-18 in melanogenesis. J Photochem Photobiol B. 2016;163:133–143. doi: 10.1016/j.jphotobiol.2016.08.024. [DOI] [PubMed] [Google Scholar]
- 47.Ali S, Huber M, Kollewe C, Bischoff SC, Falk W, Martin MU. IL-1 receptor accessory protein is essential for IL-33-induced activation of T lymphocytes and mast cells. Proc Natl Acad Sci USA. 2007;104:18660–18665. doi: 10.1073/pnas.0705939104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Allakhverdi Z, Smith DE, Comeau MR, Delespesse G. Cutting edge: The ST2 ligand IL-33 potently activates and drives maturation of human mast cells. J Immunol. 2007;179:2051–2054. doi: 10.4049/jimmunol.179.4.2051. [DOI] [PubMed] [Google Scholar]
- 49.Moulin D, Donze O, Talabot-Ayer D, Mezin F, Palmer G, Gabay C. Interleukin (IL)-33 induces the release of pro-inflammatory mediators by mast cells. Cytokine. 2007;40:216–225. doi: 10.1016/j.cyto.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 50.Theoharides TC, Zhang B, Kempuraj D, Tagen M, Vasiadi M, Angelidou A, Alysandratos KD, Kalogeromitros D, Asadi S, Stavrianeas N, et al. IL-33 augments substance P-induced VEGF secretion from human mast cells and is increased in psoriatic skin. Proc Natl Acad Sci USA. 2010;107:4448–4453. doi: 10.1073/pnas.1000803107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pushparaj PN, Tay HK, H'ng SC, Pitman N, Xu D, McKenzie A, Liew FY, Melendez AJ. The cytokine interleukin-33 mediates anaphylactic shock. Proc Natl Acad Sci USA. 2009;106:9773–9778. doi: 10.1073/pnas.0901206106. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 52.Kurowska-Stolarska M, Stolarski B, Kewin P, Murphy G, Corrigan CJ, Ying S, Pitman N, Mirchandani A, Rana B, van Rooijen N, et al. IL-33 amplifies the polarization of alternatively activated macrophages that contribute to airway inflammation. J Immunol. 2009;183:6469–6477. doi: 10.4049/jimmunol.0901575. [DOI] [PubMed] [Google Scholar]
- 53.Ohno T, Oboki K, Kajiwara N, Morii E, Aozasa K, Flavell RA, Okumura K, Saito H, Nakae S. Caspase-1, caspase-8, and calpain are dispensable for IL-33 release by macrophages. J Immunol. 2009;183:7890–7897. doi: 10.4049/jimmunol.0802449. [DOI] [PubMed] [Google Scholar]
- 54.Schmieder A, Multhoff G, Radons J. Interleukin-33 acts as a pro-inflammatory cytokine and modulates its receptor gene expression in highly metastatic human pancreatic carcinoma cells. Cytokine. 2012;60:514–521. doi: 10.1016/j.cyto.2012.06.286. [DOI] [PubMed] [Google Scholar]
- 55.Hueber AJ, Alves-Filho JC, Asquith DL, Michels C, Millar NL, Reilly JH, Graham GJ, Liew FY, Miller AM, McInnes IB. IL-33 induces skin inflammation with mast cell and neutrophil activation. Eur J Immunol. 2011;41:2229–2237. doi: 10.1002/eji.201041360. [DOI] [PubMed] [Google Scholar]
- 56.Schmitz J, Owyang A, Oldham E, Song Y, Murphy E, McClanahan TK, Zurawski G, Moshrefi M, Qin J, Li X, et al. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 2005;23:479–490. doi: 10.1016/j.immuni.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 57.Suzukawa M, Iikura M, Koketsu R, Nagase H, Tamura C, Komiya A, Nakae S, Matsushima K, Ohta K, Yamamoto K, Yamaguchi M. An IL-1 cytokine member, IL-33, induces human basophil activation via its ST2 receptor. J Immunol. 2008;181:5981–5989. doi: 10.4049/jimmunol.181.9.5981. [DOI] [PubMed] [Google Scholar]
- 58.Rank MA, Kobayashi T, Kozaki H, Bartemes KR, Squillace DL, Kita H. IL-33-activated dendritic cells induce an atypical TH2-type response. J Allergy Clin Immunol. 2009;123:1047–1054. doi: 10.1016/j.jaci.2009.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Arend WP, Palmer G, Gabay C. IL-1, IL-18, and IL-33 families of cytokines. Immunol Rev. 2008;223:20–38. doi: 10.1111/j.1600-065X.2008.00624.x. [DOI] [PubMed] [Google Scholar]
- 60.Byrne SN, Beaugie C, O'Sullivan C, Leighton S, Halliday GM. The immune-modulating cytokine and endogenous Alarmin interleukin-33 is upregulated in skin exposed to inflammatory UVB radiation. Am J Pathol. 2011;179:211–222. doi: 10.1016/j.ajpath.2011.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wu XG, Hong WS, Xu A. GM-CSF: A possible prognostic serum biomarker of vitiligo patients' considered for transplantation treatment with cultured autologous melanocytes: A pilot study. J Eur Acad Dermatol Venereol. 2016;30:1409–1411. doi: 10.1111/jdv.13256. [DOI] [PubMed] [Google Scholar]
- 62.Scott G, Leopardi S, Printup S, Malhi N, Seiberg M, Lapoint R. Proteinase-activated receptor-2 stimulates prostaglandin production in keratinocytes: Analysis of prostaglandin receptors on human melanocytes and effects of PGE2 and PGF2alpha on melanocyte dendricity. J Invest Dermatol. 2004;122:1214–1224. doi: 10.1111/j.0022-202X.2004.22516.x. [DOI] [PubMed] [Google Scholar]
- 63.Scott G, Jacobs S, Leopardi S, Anthony FA, Learn D, Malaviya R, Pentland A. Effects of PGF2alpha on human melanocytes and regulation of the FP receptor by ultraviolet radiation. Exp Cell Res. 2005;304:407–416. doi: 10.1016/j.yexcr.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 64.Ma HJ, Ma HY, Yang Y, Li PC, Zi SX, Jia CY, Chen R. a-Melanocyte stimulating hormone (MSH) and prostaglandin E2 (PGE2) drive melanosome transfer by promoting filopodia delivery and shedding spheroid granules: Evidences from atomic force microscopy observation. J Dermatol Sci. 2014;76:222–230. doi: 10.1016/j.jdermsci.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 65.Bach EA, Aguet M, Schreiber RD. The IFN gamma receptor: A paradigm for cytokine receptor signaling. Annu Rev Immunol. 1997;15:563–591. doi: 10.1146/annurev.immunol.15.1.563. [DOI] [PubMed] [Google Scholar]
- 66.Carnaud C, Lee D, Donnars O, Park SH, Beavis A, Koezuka Y, Bendelac A. Cutting edge: Cross-talk between cells of the innate immune system: NKT cells rapidly activate NK cells. J Immunol. 1999;163:4647–4650. [PubMed] [Google Scholar]
- 67.Frucht DM, Fukao T, Bogdan C, Schindler H, O'Shea JJ, Koyasu S. IFN-gamma production by antigen-presenting cells: Mechanisms emerge. Trends Immunol. 2001;22:556–560. doi: 10.1016/S1471-4906(01)02005-1. [DOI] [PubMed] [Google Scholar]
- 68.Flaishon L, Hershkoviz R, Lantner F, Lider O, Alon R, Levo Y, Flavell RA, Shachar I. Autocrine secretion of interferon gamma negatively regulates homing of immature B cells. J Exp Med. 2000;192:1381–1388. doi: 10.1084/jem.192.9.1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Harris JE, Harris TH, Weninger W, Wherry EJ, Hunter CA, Turka LA. A mouse model of vitiligo with focused epidermal depigmentation requires IFN-γ for autoreactive CD8+ T-cell accumulation in the skin. J Invest Dermatol. 2012;132:1869–1876. doi: 10.1038/jid.2011.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gregg RK, Nichols L, Chen Y, Lu B, Engelhard VH. Mechanisms of spatial and temporal development of autoimmune vitiligo in tyrosinase-specific TCR transgenic mice. J Immunol. 2010;184:1909–1917. doi: 10.4049/jimmunol.0902778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yang L, Wei Y, Sun Y, Shi W, Yang J, Zhu L, Li M. Interferon-gamma inhibits melanogenesis and induces apoptosis in melanocytes: A pivotal role of CD8+ cytotoxic T lymphocytes in vitiligo. Acta Derm Venereol. 2015;95:664–670. doi: 10.2340/00015555-2080. [DOI] [PubMed] [Google Scholar]
- 72.Natarajan VT, Ganju P, Singh A, Vijayan V, Kirty K, Yadav S, Puntambekar S, Bajaj S, Dani PP, Kar HK, et al. IFN-γ signaling maintains skin pigmentation homeostasis through regulation of melanosome maturation. Proc Natl Acad Sci USA. 2014;111:2301–2306. doi: 10.1073/pnas.1304988111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kristensen M, Chu CQ, Eedy DJ, Feldmann M, Brennan FM, Breathnach SM. Localization of tumour necrosis factor-alpha (TNF-alpha) and its receptors in normal and psoriatic skin: Epidermal cells express the 55-kD but not the 75-kD TNF receptor. Clin Exp Immunol. 1993;94:354–362. doi: 10.1111/j.1365-2249.1993.tb03457.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kholmanskikh O, van Baren N, Brasseur F, Ottaviani S, Vanacker J, Arts N, van der Bruggen P, Coulie P, De Plaen E. Interleukins 1alpha and 1beta secreted by some melanoma cell lines strongly reduce expression of MITF-M and melanocyte differentiation antigens. Int J Cancer. 2010;127:1625–1636. doi: 10.1002/ijc.25182. [DOI] [PubMed] [Google Scholar]
- 75.Martin MU, Wesche H. Summary and comparison of the signaling mechanisms of the Toll/interleukin-1 receptor family. Biochim Biophys Acta. 2002;1592:265–280. doi: 10.1016/S0167-4889(02)00320-8. [DOI] [PubMed] [Google Scholar]
- 76.Tang A, Gilchrest B. Regulation of keratinocyte growth factor gene expression in human skin fibroblasts. J Dermatol Sci. 1996;11:41–50. doi: 10.1016/0923-1811(95)00418-1. [DOI] [PubMed] [Google Scholar]
- 77.Grewe M, Gyufko K, Budnik A, Ruzicka T, Olaizola-Horn S, Berneburg M, Krutmann J. Interleukin-1 receptors type I and type II are differentially regulated in human keratinocytes by ultraviolet B radiation. J Invest Dermatol. 1996;107:865–870. [PubMed] [Google Scholar]
- 78.Kondo S, Sauder DN, Kono T, Galley KA, McKenzie RC. Differential modulation of interleukin-1 alpha (IL-1 alpha) and interleukin-1 beta (IL-1 beta) in human epidermal keratinocytes by UVB. Exp Dermatol. 1994;3:29–39. doi: 10.1111/j.1600-0625.1994.tb00263.x. [DOI] [PubMed] [Google Scholar]
- 79.Chen N, Hu Y, Li WH, Eisinger M, Seiberg M, Lin CB. The role of keratinocyte growth factor in melanogenesis: A possible mechanism for the initiation of solar lentigines. Exp Dermatol. 2010;19:865–872. doi: 10.1111/j.1600-0625.2009.00957.x. [DOI] [PubMed] [Google Scholar]
- 80.Sims J, March C, Cosman D, Widmer MB, MacDonald HR, McMahan CJ, Grubin CE, Wignall JM, Jackson JL, Call SM, et al. cDNA expression cloning of the IL-1 receptor, a member of the immunoglobulin superfamily. Science. 1988;241:585–589. doi: 10.1126/science.2969618. [DOI] [PubMed] [Google Scholar]
- 81.Barata LT, Ying S, Meng Q, Barkans J, Rajakulasingam K, Durham SR, Kay AB. IL-4- and IL-5-positive T lymphocytes, eosinophils, and mast cells in allergen-induced late-phase cutaneous reactions in atopic subjects. J Allergy Clin Immunol. 1998;101:222–230. doi: 10.1016/S0091-6749(98)70387-2. [DOI] [PubMed] [Google Scholar]
- 82.Min B, Prout M, Hu-Li J, Zhu J, Jankovic D, Morgan ES, Urban JF, Jr, Dvorak AM, Finkelman FD, LeGros G, Paul WE. Basophils produce IL-4 and accumulate in tissues after infection with a Th2-inducing parasite. J Exp Med. 2004;200:507–517. doi: 10.1084/jem.20040590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Imran M, Laddha N, Dwivedi M, Mansuri MS, Singh J, Rani R, Gokhale RS, Sharma VK, Marfatia YS, Begum R. Interleukin-4 genetic variants correlate with its transcript and protein levels in patients with vitiligo. Br J Dermatol. 2012;167:314–323. doi: 10.1111/j.1365-2133.2012.11000.x. [DOI] [PubMed] [Google Scholar]
- 84.Salgame P, Abrams JS, Clayberger C, Goldstein H, Convit J, Modlin RL, Bloom BR. Differing lymphokine profiles of functional subsets of human CD4 and CD8 T cell clones. Science. 1991;254:279–282. doi: 10.1126/science.1681588. [DOI] [PubMed] [Google Scholar]
- 85.Basak PY, Adiloglu AK, Ceyhan AM, Tas T, Akkaya VB. The role of helper and regulatory T cells in the pathogenesis of vitiligo. J Am Acad Dermatol. 2009;60:256–260. doi: 10.1016/j.jaad.2008.09.048. [DOI] [PubMed] [Google Scholar]
- 86.Nouri-Koupaee A, Mansouri P, Jahanbini H, Sanati MH, Jadali Z. Differential expression of mRNA for T-bet and GATA-3 transcription factors in peripheral blood mononuclear cells of patients with vitiligo. Clin Exp Dermatol. 2015;40:735–740. doi: 10.1111/ced.12661. [DOI] [PubMed] [Google Scholar]
- 87.Hirano T, Ishihara K, Hibi M. Roles of STAT3 in mediating the cell growth, differentiation and survival signals relayed through the IL-6 family of cytokine receptors. Oncogene. 2000;19:2548–2556. doi: 10.1038/sj.onc.1203551. [DOI] [PubMed] [Google Scholar]
- 88.Speeckaert R, Lambert J, Grine L, Van Gele M, De Schepper S, van Geel N. The many faces of interleukin-17 in inflammatory skin diseases. Br J Dermatol. 2016;175:892–901. doi: 10.1111/bjd.14703. [DOI] [PubMed] [Google Scholar]
- 89.Volpe E, Servant N, Zollinger R, Bogiatzi SI, Hupé P, Barillot E, Soumelis V. A critical function for transforming growth factor-beta, interleukin 23 and proinflammatory cytokines in driving and modulating human T(H)-17 responses. Nat Immunol. 2008;9:650–657. doi: 10.1038/ni.1613. [DOI] [PubMed] [Google Scholar]
- 90.Kang WH, Yoon KH, Lee ES, Kim J, Lee KB, Yim H, Sohn S, Im S. Melasma: Histopathological characteristics in 56 Korean patients. Br J Dermatol. 2002;146:228–237. doi: 10.1046/j.0007-0963.2001.04556.x. [DOI] [PubMed] [Google Scholar]
- 91.Nakajima M, Shinoda I, Fukuwatari Y, Hayasawa H. Arbutin increases the pigmentation of cultured human melanocytes through mechanisms other than the induction of tyrosinase activity. Pigment Cell Res. 1998;11:12–17. doi: 10.1111/j.1600-0749.1998.tb00705.x. [DOI] [PubMed] [Google Scholar]
- 92.Palumbo A, d'Ischia M, Misuraca G, Prota G. Mechanism of inhibition of melanogenesis by hydroquinone. Biochim Biophys Acta. 1991;1073:85–90. doi: 10.1016/0304-4165(91)90186-K. [DOI] [PubMed] [Google Scholar]
- 93.Smith CJ, O'Hare KB, Allen JC. Selective cytotoxicity of hydroquinone for melanocyte-derived cells is mediated by tyrosinase activity but independent of melanin content. Pigment Cell Res. 1988;1:386–389. doi: 10.1111/j.1600-0749.1988.tb00140.x. [DOI] [PubMed] [Google Scholar]
- 94.Wang X, Zhang Y. Resveratrol alleviates LPS-induced injury in human keratinocyte cell line HaCaT by up-regulation of miR-17. Biochem Biophys Res Commun. 2018;501:106–112. doi: 10.1016/j.bbrc.2018.04.184. [DOI] [PubMed] [Google Scholar]
- 95.Kim ES, Chang H, Choi H, Shin JH, Park SJ, Jo YK, Choi ES, Baek SY, Kim BG, Chang JW, et al. Autophagy induced by resveratrol suppresses a-MSH-induced melanogenesis. Exp Dermatol. 2014;23:204–206. doi: 10.1111/exd.12337. [DOI] [PubMed] [Google Scholar]
- 96.Salzes C, Abadie S, Seneschal J, Whitton M, Meurant JM, Jouary T, Ballanger F, Boralevi F, Taieb A, Taieb C, Ezzedine K. The vitiligo impact patient scale (VIPs): Development and validation of a vitiligo burden assessment tool. J Invest Dermatol. 2016;136:52–58. doi: 10.1038/JID.2015.398. [DOI] [PubMed] [Google Scholar]
- 97.Moretti S, Spallanzani A, Amato L, Hautmann G, Gallerani I, Fabiani M, Fabbri P. New insights into the pathogenesis of vitiligo: Imbalance of epidermal cytokines at sites of lesions. Pigment Cell Res. 2002;15:87–92. doi: 10.1034/j.1600-0749.2002.1o049.x. [DOI] [PubMed] [Google Scholar]
- 98.Moretti S, Fabbri P, Baroni G, Berti S, Bani D, Berti E, Nassini R, Lotti T, Massi D. Keratinocyte dysfunction in vitiligo epidermis: Cytokine microenvironment and correlation to keratinocyte apoptosis. Histol Histopathol. 2009;24:849–857. doi: 10.14670/HH-24.849. [DOI] [PubMed] [Google Scholar]
- 99.Kim NH, Jeon S, Lee HJ, Lee AY. Impaired PI3K/Akt activation-mediated NF-kappaB inactivation under elevated TNF-alpha is more vulnerable to apoptosis in vitiliginous keratinocytes. J Invest Dermatol. 2007;127:2612–2617. doi: 10.1038/sj.jid.5700900. [DOI] [PubMed] [Google Scholar]
- 100.Barygina V, Becatti M, Lotti T, Moretti S, Taddei N, Fiorillo C. Treatment with low-dose cytokines reduces oxidative-mediated injury in perilesional keratinocytes from vitiligo skin. J Dermatol Sci. 2015;79:163–170. doi: 10.1016/j.jdermsci.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 101.Debbaneh MG, Levin E, Sanchez Rodriguez R, Leon A, Koo J, Rosenblum MD. Plaque-based sub-blistering dosimetry: Reaching PASI-75 after two treatments with 308-nm excimer laser in a generalized psoriasis patient. J Dermatolog Treat. 2015;26:45–48. doi: 10.3109/09546634.2013.879094. [DOI] [PubMed] [Google Scholar]
- 102.Grimes P, Morris R, Avaniss-Aghajani E, Soriano T, Meraz M, Metzger A. Topical tacrolimus therapy for vitiligo: Therapeutic responses and skin messenger RNA expression of proinflammatory cytokines. J Am Acad Dermatol. 2004;51:52–61. doi: 10.1016/j.jaad.2003.12.031. [DOI] [PubMed] [Google Scholar]
- 103.Sakuma S, Higashi Y, Sato N, Sasakawa T, Sengoku T, Ohkubo Y, Amaya T, Goto T. Tacrolimus suppressed the production of cytokines involved in atopic dermatitis by direct stimulation of human PBMC system. (Comparison with steroids) Int Immunopharmacol. 2001;1:1219–1226. doi: 10.1016/S1567-5769(01)00059-5. [DOI] [PubMed] [Google Scholar]
- 104.Birol A, Kisa U, Kurtipek GS, Kara F, Kocak M, Erkek E, Caglayan O. Increased tumor necrosis factor alpha (TNF-alpha) and interleukin 1 alpha (IL1-alpha) levels in the lesional skin of patients with nonsegmental vitiligo. Int J Dermatol. 2006;45:992–993. doi: 10.1111/j.1365-4632.2006.02744.x. [DOI] [PubMed] [Google Scholar]
- 105.Alghamdi K, Khurrum H. Methotrexate for the treatment of generalized vitiligo. Saudi Pharm J. 2013;21:423–424. doi: 10.1016/j.jsps.2012.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Grimes PE, Hamzavi I, Lebwohl M, Ortonne JP, Lim HW. The efficacy of afamelanotide and narrowband UV-B phototherapy for repigmentation of vitiligo. JAMA Dermatol. 2013;149:68–73. doi: 10.1001/2013.jamadermatol.386. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used during the present study are available from the corresponding author upon reasonable request.