Intraductal papillary neoplasms of the bile duct (IPNBs) are rare and can be difficult to diagnose, given their flat appearance and production of intraductal mucin, which limits the interpretation of cholangiography.1 IPNBs occur throughout the biliary tract and share histologic and clinical features with pancreatic intraductal papillary mucinous neoplasms. Given the risk of invasive carcinoma, surgical resection is generally warranted.2
Case presentation
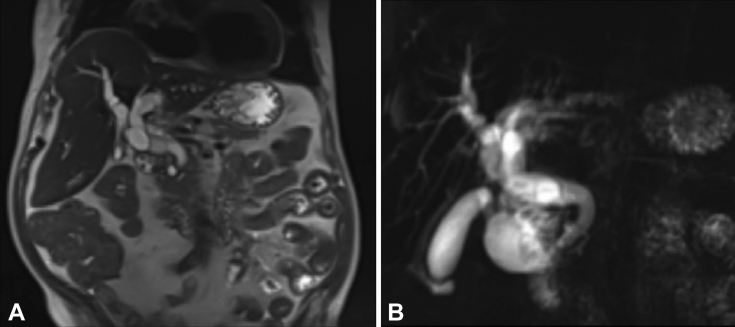
A 71-year-old man with a history of end-stage renal disease was referred for evaluation of biliary dilation noted on imaging and a history of cholangitis. Four months before our evaluation, ERCP had revealed an extensive amount of intraductal mucin. Cross-sectional imaging revealed severe intrahepatic and extrahepatic biliary ductal dilation without a definitive mass or stricture (Fig. 1). An initial ERCP at our center revealed a diffusely dilated biliary tree and a large filling defect consistent with intraductal mucin. Single-operator cholangioscopy was performed; however, visualization was extremely poor because of the extensive intraductal mucus (Fig. 2).
Figure 1.
Cross-sectional imaging demonstrating severe intrahepatic (A) and extrahepatic (B) biliary ductal dilation without focal mass or stricture.
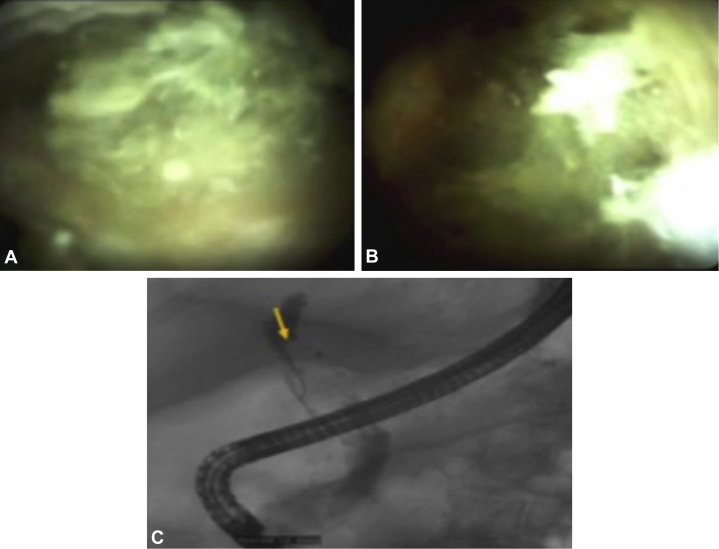
Figure 2.
A,B, Initial ERCP with use of single-operator cholangioscopy showing a significant amount of intraductal mucin, resulting in poor ductal visualization. C, Cholangiography demonstrating a filling defect consistent with intraductal mucin without focal mass or stricture.
Endoscopic technique
The patient returned to our center for further evaluation, and we elected to perform peroral cholangioscopy using a pediatric upper endoscope for further evaluation (Video 1, available online at www.VideoGIE.org). The patient received a periprocedural intravenous antibiotic agent (ciprofloxacin). Initial cholangiography demonstrated extensive biliary dilation, and balloon sweeps revealed a moderate amount of intraductal mucin. The duodenoscope was withdrawn, and the pediatric upper endoscope was advanced to the level of the major papilla.
With gentle abdominal pressure, we advanced the endoscope safely into the distal portion of the common bile duct (Fig. 3). As the endoscope was advanced proximally, an extensive amount of mucin was seen, precluding adequate visualization (Fig. 4). Then, 100 mL N-acetylcysteine was used as an intraductal mucolytic and visualization was improved, allowing safe advancement of the upper endoscope (Fig. 5).
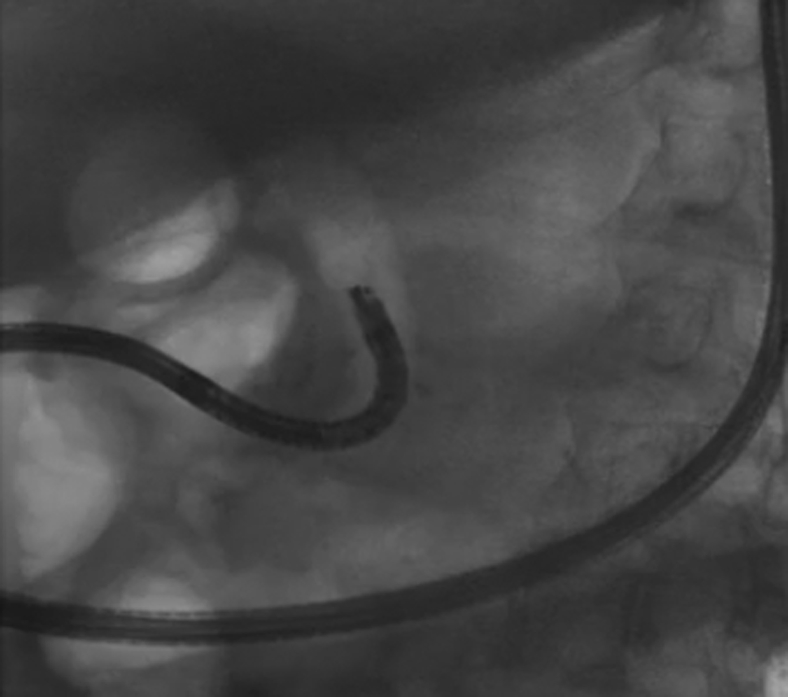
Figure 3.
Repeated ERCP, again demonstrating a significant amount of intraductal mucin; we therefore elected to perform peroral cholangioscopy.
Figure 4.
At the level of the common hepatic duct, a significant amount of intraductal mucin impaired visualization.
Figure 5.
Injection of approximately 100 mL acetylcysteine into the bile duct resulted in improved visualization, allowing for safe advancement of the endoscope.
Within the left lobe of the liver, we observed an area of grossly abnormal-appearing biliary epithelium consistent with an underlying mucinous neoplasm (Fig. 6). The lesion was evaluated under both high-definition white-light imaging and narrow-band imaging for further characterization of the overlying mucosa. Targeted biopsy specimens were obtained with the pediatric biopsy forceps. The results of pathologic examination were consistent with IPNB (Fig. 7). The patient was subsequently referred to surgery and has undergone a successful left hepatectomy.
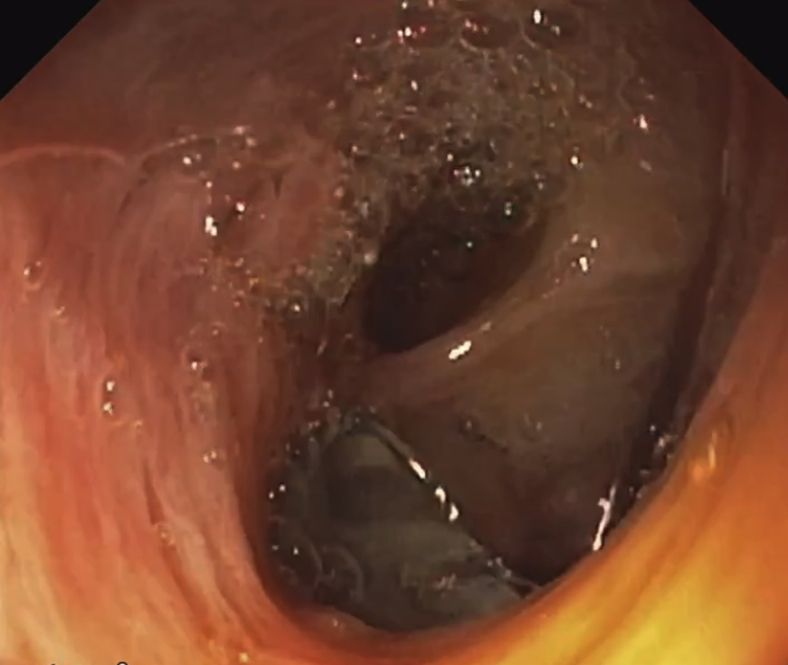
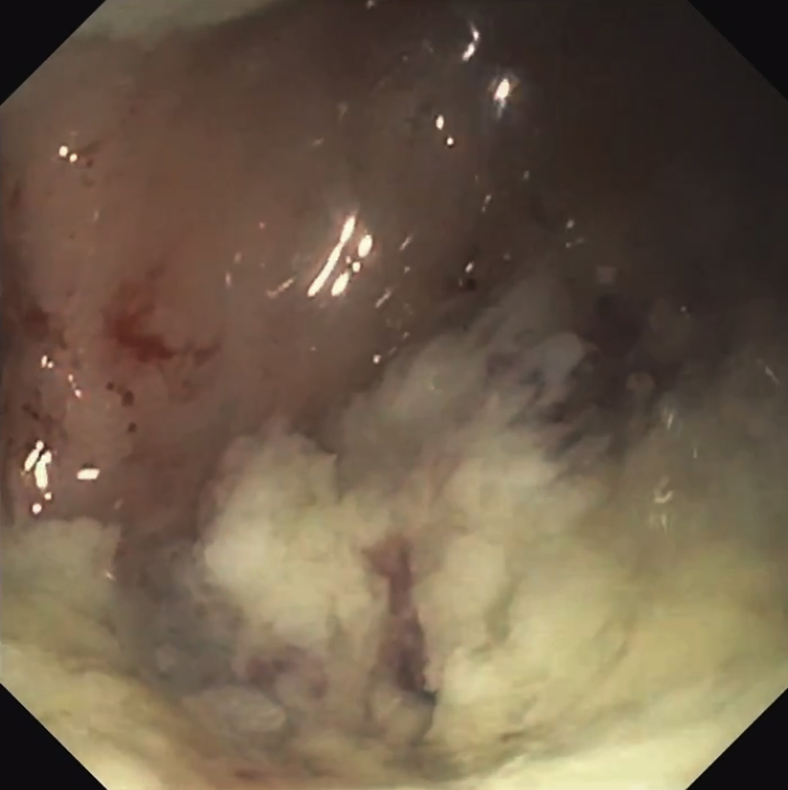
Figure 6.
Within the lobe of the left liver, an area of abnormal frondlike tissue consistent with underlying mucinous neoplasm; biopsy specimens were obtained.
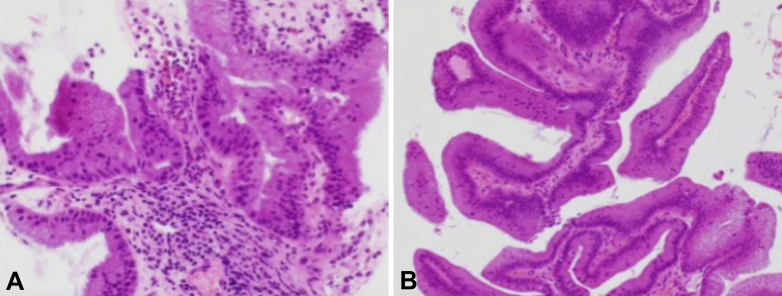
Figure 7.
Pathologic analysis demonstrating multiple fragments of ductal mucosa with prominent mucinous stromal background and focal associated epithelium with low-grade mucinous features. Findings were consistent with an underlying intraductal papillary neoplasm of the bile duct (H&E, orig. mag. × 20).
Conclusions
IPNBss can be very obscure lesions, given their flat appearance and extensive mucus production. Peroral cholangioscopy with the use of a pediatric upper endoscope may be a useful tool, allowing for improved irrigation and subsequent visualization to obtain targeted biopsy specimens. Furthermore, acetylcysteine used as a mucolytic may be a useful adjunct when one is faced with this rare lesion.
Disclosure
Dr Mullady is a consultant for Boston Scientific and Cook Medical and the recipient of speaking fees from AbbVie. All other authors disclosed no financial relationships relevant to this publication.
Footnotes
If you would like to chat with an author of this article, you may contact Dr Bill at jasongbill@gmail.com.
Supplementary data
Use of peroral cholangioscopy to diagnose an intraductal papillary neoplasm of the bile duct.
References
- 1.Kung J., Parks R., Ireland H. Intraductal papillary neoplasm of the bile duct: the role of single-operator cholangioscopy. VideoGIE. 2018;3:55–57. doi: 10.1016/j.vgie.2017.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rocha F., Lee H., Katabi N. Intraductal papillary neoplasm of the bile duct: a biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas? Hepatology. 2012;56:1352–1360. doi: 10.1002/hep.25786. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Use of peroral cholangioscopy to diagnose an intraductal papillary neoplasm of the bile duct.