Abstract
Background
Diabetes is a public health problem worldwide, associated with increased morbidity and mortality. According to the International Diabetes Federation (IDF) 2017 data, around 425 million people worldwide suffer from diabetes. This number is expected to increase to 629 million in 2045. Various occidental studies reported the increased prevalence and lower control of diabetes among prisoners. However, there is no data on the characteristics of inmates with diabetes in sub-Saharan Africa.
Methods
A cross-sectional study among incarcerated detainees from the Yaoundé Central Prison was conducted from January to July 2017. Diabetes was defined according to the American Diabetes Association (ADA) criteria. Analyzed variables included phenotypic characteristics, lifestyle, the reason for detention, the sentence severity, and the length of detention.
Results
We recruited 437 inmates (344 men) with an average age of 37.0 (95% CI: 35.9-38.3) years. The most frequent age group was 20 to 39 years with 281 (64.7%) inmates, and the mean prison stay was 29.1 (95% CI: 25.7-32.8) months. The prevalence of diabetes in the Yaoundé Central Prison was 9.4%. The main cardiovascular risk factors were a sedentary lifestyle (91.1%), hypertension (39.6%), smoking (31.6%), and alcohol consumption (28.1%). Hypertension (p = 0.005), obesity (p = 0.005), obesity (p = 0.005), obesity (p = 0.005), obesity (p = 0.005), obesity (p = 0.005), obesity (
Conclusion
Diabetes prevalence in the Yaoundé Central Prison was high, at 9.4%, compared to that in the general population. It was associated with other classical cardiovascular risk factors and factors linked to the sentence (minor and major crimes). This trial is registered with CE00617/CRERSHC/2016.
1. Background
Many studies reported an increase in the carceral population worldwide, estimated at almost 11 million. This number is probably underestimated due to false reports or the unavailability of many of them [1]. Diabetes is a major public health problem in the world, with a global prevalence estimated at around 8.8% of the world population (425 million people), according to the IDF 2017 data [2]. This number is expected to increase to 629 million in 2045. Moreover, diabetes is associated with severe morbidity and mortality: 4 million of death in 2017 were diabetes-related and the cardiovascular complications are common [3–12]. The diabetes prevalence in the United States of America (USA) was estimated at 9.3% (30.2 million) in 2017. It is lower in Africa with 4.2% but probably underestimated because data are lacking [2].
Racial disparities in diabetes prevalence and care are well recognized, with increased prevalence among the Afro-American population and Hispanic population compared to the white population [13–16]. Diabetes remains one of the principal cardiovascular risk factors in Africa [17]. The prevalence of diabetes in Africa is the lowest (4.2%) compared to other continents, but the prevalence and the burden of this disease are rising quickly in Africa [18, 19]. Uncontrolled urbanization and major changes in lifestyle seemed to drive this burden [20, 21]. In Cameroon, diabetes prevalence was estimated at around 6% in 2018 [2, 22]. This prevalence is increasing in the general population, rising from 2.0% in 1999 to 4.7% in 2002 and 5.8% in 2018 [22–24]. There is a regional disparity between rural and urban areas, with a rural prevalence of diabetes lower than the urban one but rising with time [23–25]. Diabetes prevalence also seems to be increased in particular groups: patients with stroke (12.8%) and patients with end-stage renal disease (15.9%) [26, 27].
Glucose impairment seems to be associated with older age, lifestyle modification, inflammatory status, and the presence of other cardiovascular risk factors [24, 28, 29]. Other factors are also described: heredity, genetic predisposition, the influence of the environment, and lifestyles such as salt consumption and sedentary lifestyle. Nevertheless, the contribution of stress (professional, family, and social) is far from unanimous. It can be involved in the onset of diabetes or completely decompensate a well-controlled disease. Prison is known to be a stressful environment [30]. This condition can reveal or disturb the disease [31]. However, several studies in western countries showed similar or reduced diabetes prevalence among prisoners [32–34]. This prevalence could be higher among a particular group of prisoners, especially those over 50 years [35]. In Cameroon, previous studies reported promiscuity, increased carceral population, and high prevalence of obesity and hypertension among prisoners [36, 37]. It was therefore important for us to assess the prevalence of diabetes among prisoners and identify the associated factors.
2. Methods
2.1. Study Design and Setting
A cross-sectional study was conducted among Yaoundé Central Prison inmates from January to July 2017. This prison is located in Yaoundé, the city capital of Cameroon (sub-Saharan Africa), with a population of 2 million individuals. It is the main prison of this city. Although the prison was initially built for 800 prisoners, the carceral population has been evaluated at 4859 inmates in July 2017. The prison is organized in 206 rooms divided into 13 quarters. Living conditions in the Yaoundé Central Prison are bad: promiscuity and malnutrition rate are high among prisoners and bedding condition is poor (most of the prisoners sleep on a mattress laid on the floor). Clinical follow-up on prisoners is poor (there are only two doctors for managing all prisoners), and physical activities are rare [38].
2.2. Variables and Measurements
All inmates were approached regardless of the in-prison stay, the sentence, or the in-prison location. Clear information was given to all inmates about the study and their participation. All consenting inmates who came at the in-prison clinic were included in the study. We excluded all subjects who did not fast, who did not sign a consent, and who were not seen at the in-prison clinic at the second passage. The second passage was useful for collecting and confirming an inmate's information. The lack of data and the not fasting situation were the most exclusion criteria.
2.2.1. Procedures
Trained medical personnel conducted the screening at the in-prison clinic. The participants underwent a face-to-face interview. All consenting participants were seen twice at a 1-month interval. Using a standardized questionnaire, data were collected on demographics, incarceration characteristics (duration, the severity of condemnation), smoking habits and alcohol consumption, diabetes and hypertension history including drug treatment and complications, and other cardiovascular risk factors.
All participants were subjected to a physical examination. It included BP and anthropometric measurements. The BP (in mmHg) was measured in each arm using a standard adult arm cuff of an aneroid manometer (OMRON) with the patient's arm supported and at least 10 min after the patient was rested in a sitting position. The measurement was repeated 2 minutes later. The average of the two measurements obtained in each arm was taken as the patient's blood pressure. Mean BP of both visits was registered. Height (in m) measurement was done to the nearest 0.01 m using a wooden platform and a height ruler, without shoes, feet together, arms by the sides, and in an erect position on the wooden platform footrest. Weight (in kg) was measured to the nearest 0.5 kg using a weight scale with the patient wearing only light clothing. Waist circumference (WC) was measured in a horizontal plane midway between the inferior margin of the ribs and the superior border of the iliac crest with the patient standing erect and breathing normally. A nonextensible measuring tape graduated in centimeters was used for the measurement. The body mass index was calculated as weight (kg)/height (m) × height (m). Fasting capillary blood sugar was measured using a OneTouch® brand glucometer. The selection process is summarized in Figure 1.
Figure 1.
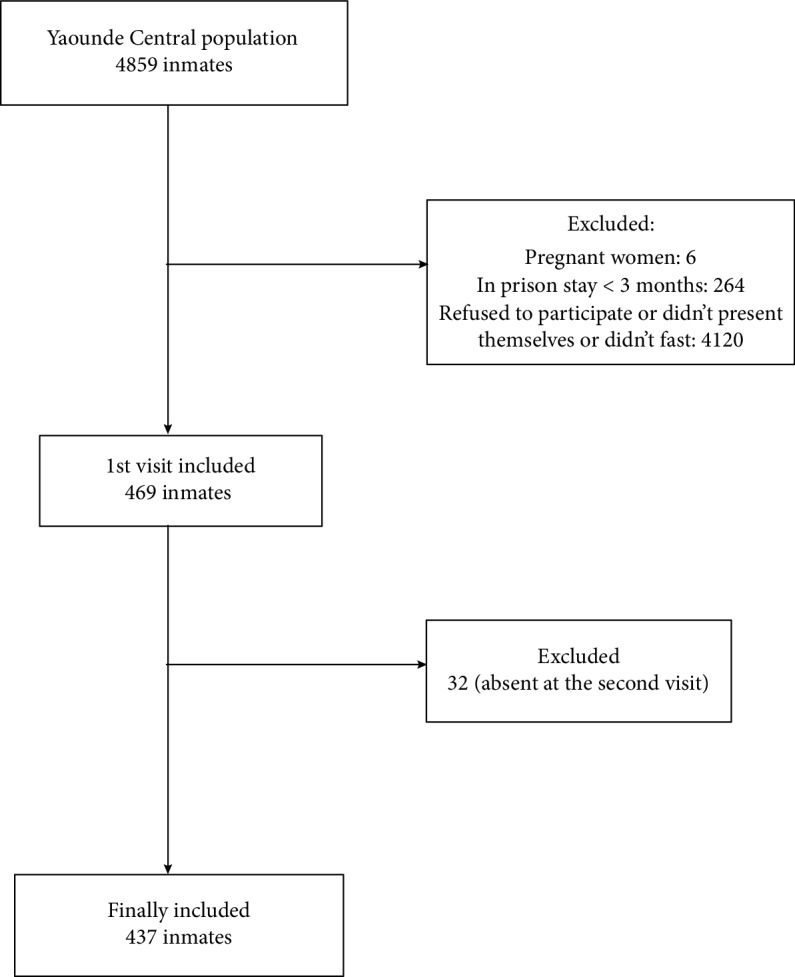
Patient flow chart.
2.3. Definitions
Patients were declared diabetic according to the following criteria defined by the American Diabetes Association: a fasting plasma glucose (FPG) level ≥ 126 mg/dL (7.0 mmol/L) on two separate occasions: a random blood glucose ≥ 200 mg/dL (11.1 mmol/L) and a two-hour plasma glucose concentration ≥ 200 mg/dL (11.1 mmol/L) after 75 g anhydrous glucose in an oral glucose tolerance test (OGTT) [39]. People with a previous diagnosis or treatment for diabetes were also considered diabetic. Systolic BP ≥ 140 mmHgand/or diastolic BP ≥ 90 mmHg defined hypertension. Obesity was defined as a BMI of ≥30 kg/m2, and overweight was defined as a BMI between 25 and 29.9. A sedentary lifestyle was defined as the absence of any physical activity (absence of at least 3 walking episodes of 45 min in a week).
Waist circumference > 94 cm in men or 80 cm in women was high. Excessive alcohol consumption was based on intake either more than 3 (2 for women) standard glasses of wine per day or more than 10 (5 for women) local beers per week. Traditional alcohol beverage was not assessed. Current smoking was defined by a consumption of at least one cigarette per day.
A monthly income of less than 86.3 $US defined low social class. Other social classes were classified into middle (by income between 86.3 and 258.9 $US) and high (by an income above this amount).
Cameroon's penal code (2016 version) classified the reason for detention into felonies or crimes (an infraction punishable with death or with loss of liberty for a maximum of more than 10 years and fine where the law so provides) and offense (an infraction punishable with loss of liberty or with fine, where the loss of liberty may be for more than 10 days but not for more than 10 years and the fine more than 43.2 $US). The crimes may be subdivided into minor (use or selling of drugs, the unauthorized use of a weapon, or robbery) and major (homicide, rape, or embezzlement of public funds) crimes [40].
Sentence severity was subdivided into short (<5 years), average (5 to less than 15 years), and severe (>15 years). In the same way, an incarceration length < 5 years, between 5 and 15 years, and more than 15 years was classified as short, average, and high, respectively.
2.4. Sample Size and Statistical Analysis
The sample size was calculated using Lorenz's formula (StatCalc of EPI Info software). Using the national prevalence of 5.8% in Cameroon, with an 80% power to detect significant associations or differences and a 5% accepted margin of error, the minimal sample size estimate was 84 participants.
Data were analyzed using the Statistical Package for the Social Sciences (SSPS Inc., Chicago, Illinois, USA) v.20.0 and EPI-INFO v.3.5 software. Quantitative data are presented as median ± confidence interval (CI), and qualitative data are presented as frequencies and percentages. Group comparisons were performed with chi-square tests and equivalents for qualitative variables and the Student t-test and analysis of variance (ANOVA) for quantitative variables. Factors associated with diabetes in univariate analysis were entered into a multivariate logistic regression. Results were considered statistically significant for p values < 0.05.
3. Results
3.1. Participants
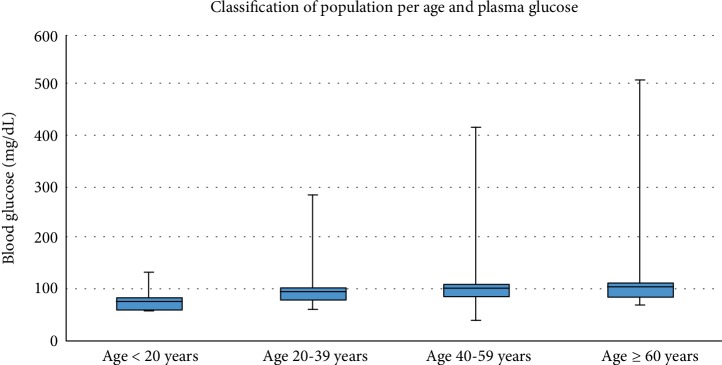
We included 437 inmates, mostly from male gender (344, 78.7%), with a median age of 37 (95% CI: 35.9–38.3) years. The most frequent age group was 20 to 39 years with 281 (64.7%) inmates (Figure 2). The median prison stay was 29.1 (95% CI: 25.7-32.8) months. Among them, 41 (9.4%) inmates were diabetic. Median blood sugar was 90 (95% CI: 0.79-1.07) mg/dL. Median blood glucose increased with age, from 0.75 for the <20 years group to 1.21 for the ≥60 years group (p < 0.001) (Figure 2).
Figure 2.
Population classification by age and mean plasma glucose.
3.2. Main Data
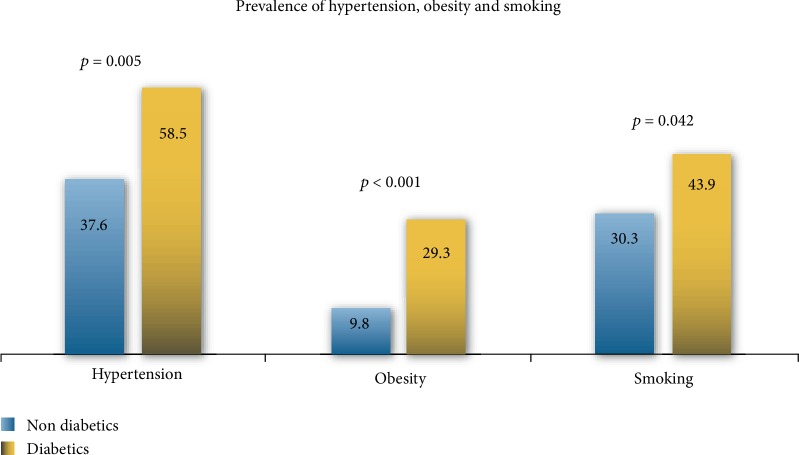
Sedentary lifestyle (91.1%), smoking (31.6%), hypertension (39.6%), and alcohol (28.1%) were the main cardiovascular risk factors among inmates. 24 (58.5%) diabetic inmates were also hypertensive. The cardiovascular risk factors are presented in Table 1. Hypertension (p = 0.005), obesity (p < 0.001), smoking (p = 0.042), and sedentary lifestyle (p = 0.039) were associated with diabetes (Figure 3).
Table 1.
Risk factors associated with diabetes among inmates in univariate analysis.
| Variables | Overall | Diabetes+, n (%) | Diabetes-, n (%) | OR (95% CI) | p value |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 341 (100) | 35 (10.3) | 306 (89.7) | 1.7 (0.7–4.2) | 0.118 |
| Female | 96 (100) | 6 (6.3) | 90 (93.7) | ||
| Age (years) | |||||
| <20 | 6 (100) | 1 (2.4) | 5 (1.3) | 1.9 (0.2–17.1) | 0.448 |
| 20-39 | 281 (100) | 23 (57.5) | 258 (65.5) | 0.7 (0.4–1.3) | 0.160 |
| 40-59 | 109 (100) | 13 (31.7) | 96 (24.2) | 1.4 (0.7–2.9) | 0.150 |
| >60 | 41 (100) | 4 (9.8) | 37 (9.3) | 1.0 (0.3–3.1) | 0.552 |
| Social class | |||||
| Low social class | 241 (100) | 22 (53.7) | 219 (55.3) | 0.9 (0.5–1.8) | 0.419 |
| Middle social class | 74 (100) | 6 (14.6) | 68 (17.2) | 0.8 (0.3–2.0) | 0.355 |
| High social class | 122 (100) | 13 (32.5) | 109 (27.7) | 1.3 (0.6–2.5) | 0.258 |
| Hypertension | 173 (100) | 24 (58.5) | 149 (37.6) | 2.3 (1.2–4.5) | 0.005 |
| Obesity | 51 (100) | 12 (29.3) | 39 (9.8) | 3.8 (1.8–8.0) | <0.001 |
| Smoking | 138 (100) | 18 (43.9) | 120 (30.3) | 1.8 (0.9–3.4) | 0.042 |
| Alcohol consumption | 123 (100) | 14 (34.1) | 109 (27.5) | 1.4 (0.7–2.7) | 0.187 |
| Sedentary lifestyle | 398 (100) | 34 (82.9) | 364 (91.9) | 0.4 (0.2–1.0) | 0.039 |
| Reason of detention | |||||
| Offense | 250 (100) | 22 (53.7) | 228 (57.6) | 0.8 (0.4–1.6) | 0.315 |
| Minor crimes | 67 (100) | 1 (2.4) | 66 (16.9) | 0.1 (0.01–0.9) | 0.003 |
| Major crimes | 120 (100) | 18 (46.2) | 102 (26.7) | 2.3 (1.2–4.6) | <0.001 |
| Length of incarceration | |||||
| Low | 387 (100) | 33 (80.5) | 354 (89.4) | 0.5 (0.2–1.2) | 0.055 |
| Average | 41 (100) | 7 (17.1) | 34 (8.6) | 2.2 (0.9–5.3) | 0.051 |
| Long | 9 (100) | 1 (2.4) | 8 (2) | 1.2 (0.1–9.4) | 0.591 |
| Sentence severity | |||||
| Short sentence | 94 (100) | 9 (22) | 85 (21.5) | 1.0 (0.5–2.2) | 0.460 |
| Average sentence | 74 (100) | 5 (12.2) | 69 (17.4) | 0.6 (0.2–1.7) | 0.206 |
| Severe sentence | 43 (100) | 7 (17.1) | 36 (9.1) | 2.0 (0.8–4.9) | 0.064 |
Figure 3.
Comparison of diabetic and nondiabetic patients according to hypertension, obesity, and smoking.
Inmates from the low social class were the most frequent, 241 (55.1%) inmates, followed by those from the high social class (122, 28.1%). Among those inmates, 226 (51.7%) of them were accused guilty, 94 (21.5%) were condemned for less than 5 years, 74 (16.9%) were condemned for 5 to 15 years, and 43 (9.8%) were condemned for more than 15 years.
Among detention variables, only major crime (p = 0.007) and minor crime (p = 0.003) were associated with diabetes. Neither social class nor sentence length nor sentence severity was associated with diabetes in univariate analysis. In multivariate analysis, only obesity was associated with diabetes among inmates (Table 2).
Table 2.
Risk factors associated with hypertension in multivariate analysis.
| Risk factor | OR (95% CI) | p value |
|---|---|---|
| Major crimes | 1.6 (0.8–3.4) | 0.181 |
| Hypertension | 1.9 (0.9–3.9) | 0.081 |
| Smoking | 1.7 (0.8–3.4) | 0.131 |
| Obesity | 3.4 (1.5–7.7) | 0.003 |
4. Discussion
This cross-sectional study is aimed at assessing the prevalence of diabetes and the associated risk factors among a group of prisoners in a sub-Saharan African setting. This study represents the first published data analysis of diabetes in a specific population of inmates in Africa.
Evidence from western countries shows that noncommunicable disease (NCD) is a public health problem in prison [34, 35, 41–45]. Recent studies in Africa showed an increased prevalence of NCD among prisoners [44, 45]. Diabetes prevalence among prisoners is still poorly known in Africa. However, there is no data in Africa and particularly in Cameroon for its prevalence and risk factors.
This study should be interpreted considering some limitations. As we carried out this study in only one prison of Cameroon and an urban area, the findings could not be extrapolated to others. Another important limitation was the diagnostic mean: most of the diabetes diagnosis was made based on fasting capillary glucose, and OGTT and glycated hemoglobin were not performed. The other limitations were the population size (small compared to other studies on the topic) and the fact that the study relied on a population census that was not designed to explicitly measure the effect of exposure to incarceration (length). Our capacity to make causal inferences is limited by the cross-sectional design of the study.
Diabetes prevalence was 9.4% in the Yaoundé Central Prison. This is higher than the national prevalence of 5.8% [2, 22]. Diabetes prevalence among prisoners used to be the same or lower to the national prevalence [32, 34, 44, 46, 47]. This increased diabetes could be related to poor feeding conditions and sedentary lifestyle. It has thus been proven that improvement of diet and physical activity could improve diabetes control or metabolic syndrome among prisoners [48, 49]. However, considering the high prevalence of CVRF in this population, the inappropriate diet, and the prevalence of infectious conditions, this prevalence seems to be reliable [37]. Furthermore, Kamdem et al. reported increased overweight/obesity and impaired fasting blood glucose in teenagers, the same as Mandob who reported a prediabetes prevalence of 15.3% [50, 51]. It is therefore conceivable that such a population put in this environment could develop diabetes. Sedentary lifestyle, hypertension, smoking, and alcohol consumption were the main CVRFs in this population. This was similar to Herbert's, Munday's, Maimela's, and Sabir's findings, showing low obesity and physical activity among prisoners, while smoking and alcohol consumption are increased [35, 43–45]. As in the normal population, plasma glucose levels turn to increase with age [52].
Detention variables associated with diabetes were only the reason for detention. Major crime (p = 0.007) and minor crime (p = 0.003) and middle social class (p = 0.001) were associated with diabetes. This could be because major and minor crimes included financial crimes or fraud which in the Cameroonian setting is used to be done by people from a certain age and probably with diabetes before prison.
Preventive strategies need to be implemented regarding the high prevalence of diabetes and CVRFs among prisoners. Importance should be given on screening for diabetes, hypertension, and other CVRFs. Lifestyle modification (alcohol and smoking cessation, appropriate diet, and increased physical activity) should be in the foreground. This also means increasing the number of caregivers and making health promotion among prisoners.
5. Conclusion
Although this study is the first of its kind in Cameroon and despite its limitations, it shows a high prevalence of diabetes in the Yaoundé Central Prison. Risk factors for diabetes among prisoners included detention variables such as the sentence for a major or minor crime and classical CVRFs such as sedentary lifestyle, hypertension, smoking, and obesity. Due to the high prevalence of diabetes among this group of prisoners, there is a need to implement preventive strategies for diabetes in prison.
Acknowledgments
We thank all the staff of the infirmary of the Yaoundé Central Prison and its director.
Abbreviations
- ADA:
American Diabetes Association
- CVRF:
Cardiovascular risk factor
- IDF:
International Diabetes Federation
- NCD:
Noncommunicable diseases
- SPSS:
Statistical Package for the Social Sciences
- USA:
United States of America.
Data Availability
The excel data used to support the findings of this study are restricted by the Ministry of Justice of Cameroon in order to protect prisoners privacy. Data are available from Sylvain Raoul Simeni Njonnou after authorization of the Ministry of Justice of Cameroon for researchers who meet the criteria for access to confidential data.
Ethical Approval
This work was approved by the institutional board of the Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Cameroon; the Centre Regional Ethics Committee for Human Health Research (registration number CE00617/CRERSHC/2016); the Ministry of Justice of Cameroon, and the stage manager of the Yaoundé Central Prison. This work was carried out in accordance with the declaration of Helsinki [53]. All ethical rules involving research on disadvantaged groups such as prisoners have been respected [54]. Patients were free to attend the study without any outside constraint.
Consent
We obtained informed and signed consent form from each participant. There was no participant under 16 years in the study group.
Conflicts of Interest
The authors declare that they have no competing interest.
Authors' Contributions
ATT, SRSN, JB, AMJ, and MCEE were involved in conception and design. ATT and SRSN were involved in data collection. KNE was responsible for the administrative support. ATT, SRSN, AJM, and JB were involved in data analysis and interpretation. SRSN, ATT, AJM, JB, MCEE, and EAMSE drafted the manuscript. MJNE, OKK, STN, ANTM, MDY, and ES reviewed the manuscript. All the authors read and approved the final draft for publication.
References
- 1.Walmsley R. World Prison Population List Twelfth Edition. 2018. World prison Brief.
- 2.International diabetes Federation. IDF DIABETES ATLAS eighth edition 2017. Eighth. Brussels, Belgium: International diabetes Federation; 2017. Report No. [Google Scholar]
- 3.Danaei G., Lawes C. M., Vander Hoorn S., Murray C. J., Ezzati M. Global and regional mortality from ischaemic heart disease and stroke attributable to higher-than-optimum blood glucose concentration: comparative risk assessment. The Lancet. 2006;368(9548):1651–1659. doi: 10.1016/S0140-6736(06)69700-6. [DOI] [PubMed] [Google Scholar]
- 4.Eeg-Olofsson K., Cederholm J., Nilsson P. M., et al. Glycemic control and cardiovascular disease in 7,454 patients with type 1 diabetes: an observational study from the Swedish National Diabetes Register (NDR) Diabetes Care. 2010;33(7):1640–1646. doi: 10.2337/dc10-0398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Emerging Risk Factors Collaboration. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. The Lancet. 2010;375(9733):2215–2222. doi: 10.1016/S0140-6736(10)60484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nagy A., Adany R., Sandor J. Effect of diagnosis-time and initial treatment on the onset of type 2 diabetes mellitus complications: a population-based representative cross-sectional study in Hungary. Diabetes Research and Clinical Practice. 2011;94(3):e65–e67. doi: 10.1016/j.diabres.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Tancredi M., Rosengren A., Svensson A.-M., et al. Excess mortality among persons with type 2 diabetes. The New England Journal of Medicine. 2015;373(18):1720–1732. doi: 10.1056/NEJMoa1504347. [DOI] [PubMed] [Google Scholar]
- 8.Wright A. K., Kontopantelis E., Emsley R., et al. Life expectancy and cause-specific mortality in type 2 diabetes: a population-based cohort study quantifying relationships in ethnic subgroups. Diabetes Care. 2017;40(3):338–345. doi: 10.2337/dc16-1616. [DOI] [PubMed] [Google Scholar]
- 9.Bragg F., Li L., Smith M., et al. Associations of blood glucose and prevalent diabetes with risk of cardiovascular disease in 500 000 adult Chinese: the China Kadoorie Biobank. Diabetic Medicine. 2014;31(5):540–551. doi: 10.1111/dme.12392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zghebi S. S., Steinke D. T., Carr M. J., Rutter M. K., Emsley R. A., Ashcroft D. M. Examining trends in type 2 diabetes incidence, prevalence and mortality in the UK between 2004 and 2014. Diabetes, Obesity & Metabolism. 2017;19(11):1537–1545. doi: 10.1111/dom.12964. [DOI] [PubMed] [Google Scholar]
- 11.Huang E. S., Laiteerapong N., Liu J. Y., John P. M., Moffet H. H., Karter A. J. Rates of complications and mortality in older patients with diabetes mellitus: the diabetes and aging study. JAMA Internal Medicine. 2014;174(2):251–258. doi: 10.1001/jamainternmed.2013.12956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Z., Liu M. Life years lost associated with diabetes: an individually matched cohort study using the U.S. National Health Interview Survey data. Diabetes Research and Clinical Practice. 2016;118:69–76. doi: 10.1016/j.diabres.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 13.Heidemann D. L., Joseph N. A., Kuchipudi A., Perkins D. W., Drake S. Racial and economic disparities in diabetes in a large primary care patient population. Ethnicity & Disease. 2016;26(1):85–90. doi: 10.18865/ed.26.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferdinand K. C., Nasser S. A. Racial/ethnic disparities in prevalence and care of patients with type 2 diabetes mellitus. Current Medical Research and Opinion. 2015;31(5):913–923. doi: 10.1185/03007995.2015.1029894. [DOI] [PubMed] [Google Scholar]
- 15.Rodríguez J. E., Campbell K. M. Racial and ethnic disparities in prevalence and care of patients with type 2 diabetes. Clinical Diabetes. 2017;35(1):66–70. doi: 10.2337/cd15-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meng Y.-Y., Diamant A., Jones J., et al. Racial and ethnic disparities in diabetes care and impact of vendor-based disease management programs. Diabetes Care. 2016;39(5):743–749. doi: 10.2337/dc15-1323. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. Global status report on non-communicable diseases 2014. World Health Organization. 2014. pp. 66–77. https://www.who.int/nmh/publications/ncd-status-report-2014/en/
- 18.Mbanya J. C. N., Motala A. A., Sobngwi E., Assah F. K., Enoru S. T. Diabetes in sub-Saharan Africa. The lancet. 2010;375(9733):2254–2266. doi: 10.1016/S0140-6736(10)60550-8. [DOI] [PubMed] [Google Scholar]
- 19.Jaffiol C. The burden of diabetes in Africa : a major public health problem. Bulletin de l'Académie Nationale de Médecine. 2011;195(6):1239–1254. doi: 10.1016/S0001-4079(19)31983-1. [DOI] [PubMed] [Google Scholar]
- 20.Sobngwi E., Mbanya J.-C., Unwin N. C., et al. Exposure over the life course to an urban environment and its relation with obesity, diabetes, and hypertension in rural and urban Cameroon. International Journal of Epidemiology. 2004;33(4):769–776. doi: 10.1093/ije/dyh044. [DOI] [PubMed] [Google Scholar]
- 21.Fezeu L., Balkau B., Sobngwi E., et al. Waist circumference and obesity-related abnormalities in French and Cameroonian adults: the role of urbanization and ethnicity. International Journal of Obesity. 2010;34(3):446–453. doi: 10.1038/ijo.2009.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bigna J. J., Nansseu J. R., Katte J.-C., Noubiap J. J. Prevalence of prediabetes and diabetes mellitus among adults residing in Cameroon: a systematic review and meta-analysis. Diabetes Research and Clinical Practice. 2018;137:109–118. doi: 10.1016/j.diabres.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 23.Mbanya J. C., Cruickshank J. K., Forrester T., et al. Standardized comparison of glucose intolerance in west African-origin populations of rural and urban Cameroon, Jamaica, and Caribbean migrants to Britain. Diabetes Care. 1999;22(3):434–440. doi: 10.2337/diacare.22.3.434. [DOI] [PubMed] [Google Scholar]
- 24.Sobngwi E., Mbanya J. C. N., Unwin N. C., et al. Physical activity and its relationship with obesity, hypertension and diabetes in urban and rural Cameroon. International Journal of Obesity. 2002;26(7):1009–1016. doi: 10.1038/sj.ijo.0802008. [DOI] [PubMed] [Google Scholar]
- 25.Mbanya J. C. N., Ngogang J., Salah J. N., Balkau B., Minkoulou E. Prevalence of NIDDM and impaired glucose tolerance in a rural and an urban population in Cameroon. Diabetologia. 1997;40(7):824–829. doi: 10.1007/s001250050755. [DOI] [PubMed] [Google Scholar]
- 26.Lekoubou A., Clovis N., Dzudie A., Kengne A. P. Diagnosed diabetes mellitus and in-hospital stroke mortality in a major sub- Saharan African urban medical unit. Primary Care Diabetes. 2017;11(1):57–62. doi: 10.1016/j.pcd.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 27.Halle M. P., Takongue C., Kengne A. P., Kaze F. F., Ngu K. B. Epidemiological profile of patients with end stage renal disease in a referral hospital in Cameroon. BMC Nephrology. 2015;16(1):1–8. doi: 10.1186/s12882-015-0044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Awah P. K., Kengne A. P., Fezeu L. L. K., Mbanya J.-C. Perceived risk factors of cardiovascular diseases and diabetes in Cameroon. Health Education Research. 2007;23(4):612–620. doi: 10.1093/her/cym037. [DOI] [PubMed] [Google Scholar]
- 29.Nansseu J. R., Bigna J. J., Kaze A. D., Noubiap J. J. Incidence and risk factors for prediabetes and diabetes mellitus among HIV-infected adults on antiretroviral Therapy. Epidemiology. 2018;29(3):431–441. doi: 10.1097/EDE.0000000000000815. [DOI] [PubMed] [Google Scholar]
- 30.Lloyd C., Smith J., Weinger K. Stress and diabetes: a review of the links. Diabetes Spectrum: A Publication of the American Diabetes Association. 2005;18(2):121–127. doi: 10.2337/diaspect.18.2.121. [DOI] [Google Scholar]
- 31.Massoglia M., Pridemore W. A. Incarceration and health. Annual Review of Sociology. 2015;41(1):291–310. doi: 10.1146/annurev-soc-073014-112326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bai J. R., Befus M., Mukherjee D. V., Lowy F. D., Larson E. L. Prevalence and predictors of chronic health conditions of inmates newly admitted to maximum security prisons. Journal of Correctional Health Care. 2015;21(3):255–264. doi: 10.1177/1078345815587510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hannan-Jones M., Capra S. Prevalence of diet-related risk factors for chronic disease in male prisoners in a high secure prison. European Journal of Clinical Nutrition. 2016;70(2):212–216. doi: 10.1038/ejcn.2015.100. [DOI] [PubMed] [Google Scholar]
- 34.Silverman-Retana O., Servan-Mori E., Lopez-Ridaura R., Bautista-Arredondo S. Diabetes and hypertension care among male prisoners in Mexico City: exploring transition of care and the equivalence principle. International Journal of Public Health. 2016;61(6):651–659. doi: 10.1007/s00038-016-0812-1. [DOI] [PubMed] [Google Scholar]
- 35.Munday D., Leaman J., O’Moore É., Plugge E. The prevalence of non-communicable disease in older people in prison: a systematic review and meta-analysis. Age and Ageing. 2018;48(2):204–212. doi: 10.1093/ageing/afy186. [DOI] [PubMed] [Google Scholar]
- 36.Ndongmo R. Profil psychologique et facteurs de risque cardiovasculaire chez un groupe de prisonniers de Yaoundé. Yaoundé, Cameroon: Faculté de Médecine et des Sciences Biomédicales; 1992. [Google Scholar]
- 37.Tiodoung Timnou A., Boombhi J., JingiSimeni Njonnou S. R., et al. Prevalence of hypertension and associated risk factors among a group of prisoners in Yaoundé Central Prison: a cross-sectional study. Journal of Xiangya Medicine. 2019;4:22–29. doi: 10.21037/jxym.2019.05.01. [DOI] [Google Scholar]
- 38.Special Rapporteur on Prisons and Conditions of detention in Africa. Report of the Special Rapporteur on Prisons and Conditions of detention in Africa. The African Commission on Human and Peoples’ Rights; 2002. Prisons in Cameroon. [Google Scholar]
- 39.American Diabetes Association. 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes—2019. Diabetes Care. 2019;42(Supplement 1):S13–S28. doi: 10.2337/dc19-S002. [DOI] [PubMed] [Google Scholar]
- 40.Cameroon’s Penal Code. Section 21. 2016. Parliament of Cameroon. Law 2016/007; p. p. 8. [Google Scholar]
- 41.Binswanger I. A., Krueger P. M., Steiner J. F. Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. Journal of Epidemiology and Community Health. 2009;63(11):912–919. doi: 10.1136/jech.2009.090662. [DOI] [PubMed] [Google Scholar]
- 42.Silverman-Retana O., Lopez-Ridaura R., Servan-Mori E., Bautista-Arredondo S., Bertozzi S. M. Shimosawa T., editor. Cross-sectional association between length of incarceration and selected risk factors for non-communicable chronic diseases in two male prisons of Mexico City. PLoS One. 2015;10(9, article e0138063) doi: 10.1371/journal.pone.0138063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Herbert K., Plugge E., Foster C., Doll H. Prevalence of risk factors for non-communicable diseases in prison populations worldwide: a systematic review. The Lancet. 2012;379(9830):1975–1982. doi: 10.1016/S0140-6736(12)60319-5. [DOI] [PubMed] [Google Scholar]
- 44.Maimela E., Alberts M., Modjadji S. E. P., et al. The prevalence and determinants of chronic non-communicable disease risk factors amongst adults in the Dikgale Health Demographic and Surveillance System (HDSS) site, Limpopo Province of South Africa. PLoS One. 2016;11(2, article e0147926) doi: 10.1371/journal.pone.0147926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sabir A. A., Jimoh A. Non-communicable diseases among prison inmates in North-West Nigeria. Orient Journal of Medicine. 2015;27(3–4):105–108. [Google Scholar]
- 46.Nowotny K. M., Rogers R. G., Boardman J. D. Racial disparities in health conditions among prisoners compared with the general population. SSM - Population Health. 2017;3:487–496. doi: 10.1016/j.ssmph.2017.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Harzke A. J., Baillargeon J. G., Pruitt S. L., Pulvino J. S., Paar D. P., Kelley M. F. Prevalence of chronic medical conditions among inmates in the Texas prison system. Journal of Urban Health. 2010;87(3):486–503. doi: 10.1007/s11524-010-9448-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hinata M., Ono M., Midorikawa S., Nakanishi K. Metabolic improvement of male prisoners with type 2 diabetes in Fukushima Prison, Japan. Diabetes Research and Clinical Practice. 2007;77(2):327–332. doi: 10.1016/j.diabres.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 49.Firth C. L., Sazie E., Hedberg K., Drach L., Maher J. Female inmates with diabetes: results from changes in a prison food environment. Women’s Health Issues. 2015;25(6):732–738. doi: 10.1016/j.whi.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 50.Kamdem F., Lemogoum D., Jingi A. M., et al. Prevalence and determinants of abnormal glucose metabolism in urban and rural secondary schools in Cameroon: a cross-sectional study in a sub-Saharan Africa setting. Primary Care Diabetes. 2019;13(4):370–375. doi: 10.1016/j.pcd.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 51.Mandob D. E. Prevalence of prediabetes and associated risk factors among adults in Yaounde–Cameroon. World Journal of Pharmacy and Pharmaceutical Sciences. 2017;6(4):2214–2222. doi: 10.20959/wjpps20174-8872. [DOI] [Google Scholar]
- 52.Ko G. T. C., Wai H. P. S., Tang J. S. F. Effects of age on plasma glucose levels in non-diabetic Hong Kong Chinese. Croatian Medical Journal. 2006;47(5):709–713. [PMC free article] [PubMed] [Google Scholar]
- 53.Association Médicale Mondiale. Déclaration d’Helsinki de l’Association Médicale Mondiale: principes éthiques applicables aux recherches médicales sur des sujets humains. 2013, https://www.wma.net/fr/policies-post/declaration-dhelsinki-de-lamm-principes-ethiques-applicables-a-la-recherche-medicale-impliquant-des-etres-humains/
- 54.World Health Organization, Council for International Organizations of Medical Sciences. International ethical guidelines for health-related research involving humans. Geneva: CIOMS; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The excel data used to support the findings of this study are restricted by the Ministry of Justice of Cameroon in order to protect prisoners privacy. Data are available from Sylvain Raoul Simeni Njonnou after authorization of the Ministry of Justice of Cameroon for researchers who meet the criteria for access to confidential data.