Significance Statement
Kidney toxicity from use of immune checkpoint inhibitors is being recognized as an increasingly frequent complication of treatment. However, existing data on immune checkpoint inhibitor–associated AKI have been limited to small, mostly single-center studies. In this multicenter study of 138 patients with immune checkpoint inhibitor–associated AKI and 276 controls, the authors characterize the clinical features of this complication and identify risk factors associated with its development, clinicopathologic features, and determinants of kidney recovery after an episode. Failure to achieve kidney recovery was associated with worse overall survival, and a minority (23%) of patients who were retreated with immune checkpoint inhibitors had a recurrence of AKI. The study provides insights into immune checkpoint inhibitor–associated AKI, although further study is needed to inform the care of affected patients.
Keywords: immune checkpoint inhibitors, tubulointerstitial nephritis, acute kidney injury
Abstract
Background
Despite increasing recognition of the importance of immune checkpoint inhibitor–associated AKI, data on this complication of immunotherapy are sparse.
Methods
We conducted a multicenter study of 138 patients with immune checkpoint inhibitor–associated AKI, defined as a ≥2-fold increase in serum creatinine or new dialysis requirement directly attributed to an immune checkpoint inhibitor. We also collected data on 276 control patients who received these drugs but did not develop AKI.
Results
Lower baseline eGFR, proton pump inhibitor use, and combination immune checkpoint inhibitor therapy were each independently associated with an increased risk of immune checkpoint inhibitor–associated AKI. Median (interquartile range) time from immune checkpoint inhibitor initiation to AKI was 14 (6–37) weeks. Most patients had subnephrotic proteinuria, and approximately half had pyuria. Extrarenal immune-related adverse events occurred in 43% of patients; 69% were concurrently receiving a potential tubulointerstitial nephritis–causing medication. Tubulointerstitial nephritis was the dominant lesion in 93% of the 60 patients biopsied. Most patients (86%) were treated with steroids. Complete, partial, or no kidney recovery occurred in 40%, 45%, and 15% of patients, respectively. Concomitant extrarenal immune-related adverse events were associated with worse renal prognosis, whereas concomitant tubulointerstitial nephritis–causing medications and treatment with steroids were each associated with improved renal prognosis. Failure to achieve kidney recovery after immune checkpoint inhibitor–associated AKI was independently associated with higher mortality. Immune checkpoint inhibitor rechallenge occurred in 22% of patients, of whom 23% developed recurrent associated AKI.
Conclusions
This multicenter study identifies insights into the risk factors, clinical features, histopathologic findings, and renal and overall outcomes in patients with immune checkpoint inhibitor–associated AKI.
Immune checkpoint inhibitors (ICPis) are a novel class of immunotherapy that have revolutionized the treatment of a number of malignancies.1,2 By targeting inhibitory receptors expressed on T lymphocytes, other immune cells, and tumor cells, these monoclonal antibodies enhance tumor-directed immune responses, and have been demonstrated to be highly effective in treating a broad spectrum of malignancies.3 However, the increased antitumor activity achieved with these agents comes at the cost of a unique spectrum of autoimmune phenomena known as immune-related adverse events (irAEs).4 The incidence of irAEs in patients receiving ICPis ranges from 60% to 85%, with the skin, gastrointestinal tract, and liver being the most common organs affected.1,5 Renal complications of ICPis, although less common, are becoming increasingly recognized as the use of these agents continues to expand.6
The estimated incidence of immune checkpoint inhibitor–associated AKI (ICPi-AKI) ranges from 1.4% to 4.9%.7 Initial reports described tubulointerstitial nephritis (TIN) as the most common renal lesion caused by ICPis,7,8 although other immune-mediated pathologies have also been reported, including various glomerulonephritides.9
Despite increasing recognition of the importance of ICPi-AKI, our current understanding of ICPi-AKI is limited to case reports and small case series, the largest of which included 16 patients.9 We therefore conducted a multicenter, retrospective study comprising 138 patients with ICPi-AKI to determine the independent risk factors for development of ICPi-AKI, the clinical and pathologic features associated with ICPi-AKI, the key factors associated with kidney recovery after an episode of ICPi-AKI, the risk of recurrent AKI with ICPi rechallenge, and the effect of ICPi-AKI on overall survival.
Methods
Overview
We performed a multicenter, retrospective cohort study to assess the clinical features and outcomes of ICPi-AKI. We contacted nephrologists and oncologists at 26 major academic cancer centers across the United States and Canada to identify cases of ICPi-AKI. All protocols were approved by the Massachusetts General Hospital institutional review board, and by the institutional review boards of all participating sites.
Patients with ICPi-AKI
Patients with ICPi-AKI were included if the AKI was attributed directly to the ICPi by the treating provider and the patient had at least a doubling of serum creatinine (SCr) or the requirement for RRT. In total, 18 institutions (Supplemental Table 1) contributed 138 cases that met the above criteria for ICPi-AKI.
Control Patients
To identify risk factors for development of ICPi-AKI, we also collected data from 276 patients from contemporaneous registries at Dana Farber Cancer Institute (n=107) and Massachusetts General Hospital (n=169) who received ICPis but did not develop AKI (case-to-control ratio of 1:2). All patients treated with ICPis were eligible to serve as controls except those who sustained an episode of AKI (defined as >50% increase in SCr). Random, rather than matched, selection of controls was chosen to preserve the ability to investigate all patient characteristics as potential risk factors for ICPi-AKI. The temporal distribution of ICPi initiation was similar between cases and controls (Supplemental Table 2).
Data Collection
We collected detailed clinical data on all patients using a secure, standardized, electronic case report form (REDCap). Data collected from each patient included demographics, comorbidities, use of concomitant potential TIN-causing medications, longitudinal SCr and other laboratory values, kidney biopsy data, treatment data, data on ICPi rechallenge, and data on renal and overall outcomes. Additional details on clinical data collected are in the Supplemental Appendix 1.
Definitions of AKI Severity, Kidney Recovery, and Recurrent ICPi-AKI
AKI severity was staged according to the Kidney Disease Improving Global Outcomes criteria.10 By definition, all cases were stage 2 (doubling of SCr) or stage 3 (tripling of SCr or need for RRT). We defined complete recovery of AKI as a return of SCr to <0.35 mg/dl above the baseline value, whereas we defined partial recovery as a return of SCr to >0.35 mg/dl but less than twice the baseline value, or liberation from RRT regardless of the SCr value.7,11 Recurrent ICPi-AKI was defined as a doubling of SCr or need for RRT after rechallenge with an ICPi.
Statistical Analyses
We performed the statistical analyses with Stata version 14 (StataCorp., College Station, TX). Continuous and categorical data were compared using the Wilcoxon rank-sum and Fisher exact tests, respectively. Univariate and multivariable logistic regression were used to identify risk factors for incident ICPi-AKI, and, among those with ICPi-AKI, to identify factors associated with kidney recovery. We used the Kaplan–Meier method to estimate the cumulative death rate over time, and Cox proportional hazards models to identify risk factors associated with increased mortality. Selection of covariates in multivariable models was based on univariate associations and biologic relevance. We used Schoenfeld residuals and ln-ln plots to verify that the proportional hazards assumption was not violated. All comparisons are two-tailed, with P<0.05 considered significant.
Results
Baseline Characteristics and Risk Factors for ICPi-AKI
Baseline characteristics for patients with ICPi-AKI (n=138) and controls (n=276) are shown in Table 1. The distributions of age and sex were similar in cases and controls. Most patients in both groups were receiving an ICPi for either melanoma or lung cancer. Compared with controls, patients with ICPi-AKI had a lower median baseline eGFR, were more likely to be receiving a proton pump inhibitor (PPI), and were more likely to be receiving combination therapy with an anti-cytotoxic T lymphocyte–associated antigen 4 antibody and an anti-programed cell death 1 or anti-programmed death-ligand 1 antibody. Each of these risk factors remained associated with development of ICPi-AKI in multivariable models adjusted for each other along with age, sex, and prior autoimmune disease (Table 2). The magnitude of association was greatest for ICPi combination therapy (adjusted odds ratio, 3.88; 95% confidence interval, 2.21 to 6.81).
Table 1.
Baseline characteristics for ICPi-AKI
| Variable | ICPi-AKI (n=138) | Controls (n=276) | P Value |
|---|---|---|---|
| Age at ICPi initiation, yr | 67 (58–74) | 65 (56–73) | 0.36 |
| Female, n (%) | 55 (40) | 105 (38) | 0.75 |
| Race, n (%) | 0.15 | ||
| White | 116 (84) | 248 (91) | |
| Black | 10 (7) | 10 (4) | |
| Asian | 3 (2) | 5 (2) | |
| Comorbidities, n (%) | |||
| Hypertension | 77 (56) | 171 (62) | 0.24 |
| Diabetes | 23 (17) | 47 (17) | 1.00 |
| CHF | 3 (2) | 11 (4) | 0.40 |
| COPD | 6 (4) | 36 (13) | 0.005 |
| Cirrhosis | 2 (1) | 15 (5) | 0.06 |
| Baseline SCr, mg/dl | 0.91 (0.80–1.21) | 0.87 (0.70–1.06) | 0.002 |
| Baseline eGFR, ml/min | 72 (55–89) | 83 (63–99) | <0.001 |
| CKD, n (%) | 44 (32) | 56 (20) | 0.01 |
| CKD IV, n (%) | 9 (7) | 2 (1) | 0.001 |
| Autoimmune disease, n (%) | 17 (12) | 30 (11) | 0.74 |
| Malignancy, n (%) | 0.007 | ||
| Melanoma | 49 (36) | 82 (30) | |
| Lung | 36 (26) | 106 (38) | |
| Genitourinary | 23 (17) | 21 (8) | |
| Other | 30 (21) | 67 (24) | |
| PPI, n (%) | 75 (54) | 92 (33) | <0.001 |
| ICPia n (%) | |||
| Anti–CTLA-4b | 44 (32) | 48 (17) | 0.001 |
| Anti–PD-1c | 127 (92) | 250 (91) | 0.72 |
| Anti–PD-L1 | 10 (7) | 13 (4.7) | 0.36 |
| Combo anti–CTLA-4+anti–PD-1/PD-L1d | 39 (28) | 35 (13) | <0.001 |
Data are shown as median (IQR) and n (%). CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; IV, stage four; CTLA-4, cytotoxic T lymphocyte–associated antigen 4; PD-1, programmed cell death 1; PD-L1, programmed death-ligand 1; Combo, combination.
Denotes all ICPis ever received.
Ipilimumab was the ICPi agent in 98% of those who received an anti–CTLA-4 antibody.
Nivolumab or pembrolizumab was the anti–PD-1 antibody in 49% and 42% of patients.
Ipilimumab/nivolumab was the combination therapy regimen in 75% of cases and 66% of controls.
Table 2.
Risk factors for ICPi-AKI
| Baseline Variables | Odds Ratio (95% Confidence Interval) for ICPi-AKI | ||
|---|---|---|---|
| Univariate | Multivariate | Forest Plot | |
| Age (per 10 years) | 1.08 (0.92 to 1.26) | 0.91 (0.75 to 1.11) | 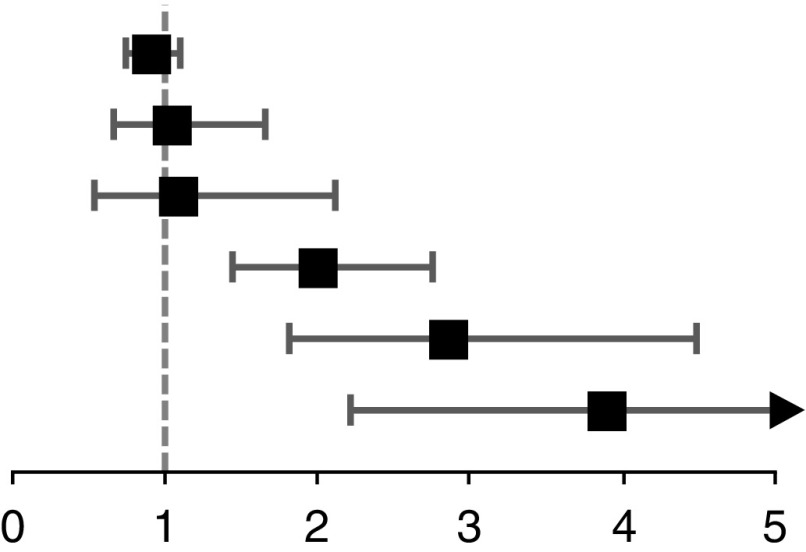 |
| Female | 1.08 (0.71 to 1.64) | 1.05 (0.67 to 1.65) | |
| Prior autoimmune disease | 1.15 (0.61 to 2.18) | 1.08 (0.55 to 2.11) | |
| eGFR, per 30 ml/min per 1.73 m2 decline | 1.67 (1.27 to 2.17) | 1.99 (1.43 to 2.76) | |
| PPI use | 2.38 (1.57 to 3.62) | 2.85 (1.81 to 4.48) | |
| Combination ICPi therapy | 2.71 (1.62 to 4.53) | 3.88 (2.21 to 6.81) | |
The full multivariable model was adjusted for the covariates listed in the table.
Among cases, baseline characteristics were similar in biopsied and nonbiopsied patients (Supplemental Table 3). Likewise, the same risk factors for ICPi-AKI were identified in the subset of patients who underwent renal biopsy (Supplemental Table 4).
Clinical Features of ICPi-AKI
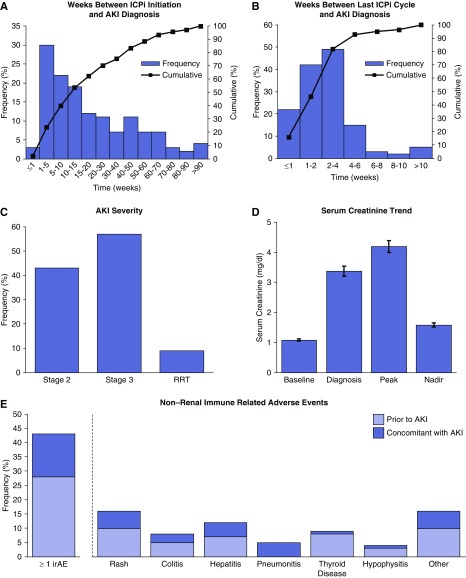
AKI developed at a median of 14 (interquartile range [IQR], 6–37) weeks after ICPi initiation (Figure 1A), and 2 (IQR, 2–3) weeks after the last ICPi dose (Figure 1B). The distribution of AKI severity was stage 2 in 43%, stage 3 in 57%, and RRT dependence in 9% of patients (Figure 1C). SCr at baseline, AKI diagnosis, peak, and nadir are shown in Figure 1D. An extrarenal irAE, most commonly rash, developed before or concomitant with AKI in 43% of cases (Figure 1E).
Figure 1.
Clinical features of ICPi-AKI. (A) The number of weeks between ICPi initiation and AKI diagnosis. (B) The number of weeks between the last ICPi cycle and AKI diagnosis. (C) The distribution of AKI severity according to the Kidney Disease Improving Global Outcomes criteria. (D) The SCr trend (mean±SEM). Baseline SCr refers to the value immediately preceding ICPi initiation; diagnosis SCr refers to the value when the patient first fulfilled criteria for ICPi-AKI (doubling of SCr or need for RRT); peak SCr refers to the highest value during the AKI episode; and nadir SCr refers to the lowest value achieved within 3 months after the AKI episode (excluding values obtained during RRT). (E) The frequency of extrarenal irAEs occurring before (>14 days before) or concomitantly (within 14 days before or after) with the AKI.
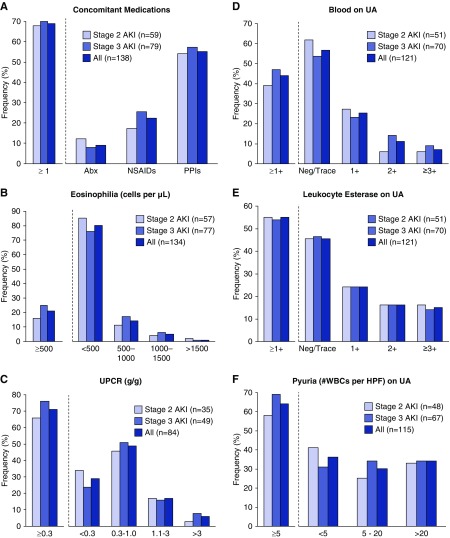
Results of the diagnostic workup performed to evaluate ICPi-AKI, stratified by AKI severity, are shown in Figure 2. Most patients (69%) were receiving a concomitant medication known to cause TIN, including antibiotics (9%), nonsteroidal anti-inflammatory drugs (NSAIDs; 22%), and PPIs (54%) (Figure 2A). A concomitant and potentially nephrotoxic chemotherapeutic agent was identified in 6% of patients; however, in each case the AKI was attributed to the ICPi (Supplemental Table 5). Most patients (79%) did not have eosinophilia (Figure 2B). The urine protein-to-creatinine ratio was ≥0.3 g/g in 71% of patients (Figure 2C). Urine dipstick was positive for leukocyte esterase and pyuria was noted on the urine sediment in approximately half of the patients (Figure 2, D and E). None of these characteristics differed significantly according to AKI severity.
Figure 2.
Clinical features of ICPi-AKI, stratified by AKI severity. (A) The frequency of concomitant potential TIN-causing medications taken within 2 weeks preceding ICPi-AKI. (B–F) The distribution of eosinophilia, proteinuria, dipstick hematuria, leukocyte esterase, and pyuria in patients with ICPi-AKI, respectively. Abx, antibiotic; HPF, high-power field; Neg, negative; UA, urinalysis; UPCR, urine protein-to-creatinine ratio; WBCs, white blood cells.
Renal biopsy was performed in 60 (43%) patients, 56 (93%) of whom had acute TIN as the dominant lesion. The remaining four patients had minimal change disease with acute tubular injury, ANCA-negative pauci-immune crescentic GN, anti–glomerular basement membrane disease, and C3 GN. Histologic features of biopsied patients with TIN are shown in Supplemental Table 6. Biopsied and nonbiopsied patients had similar clinical features of ICPi-AKI (Supplemental Figures 1 and 2).
Treatment of ICPi-AKI
ICPi therapy was held at AKI diagnosis in 134 (97%) patients, and 119 (86%) received corticosteroids. Among those who received steroids, the median time from doubling of SCr to initiation of steroids was 4 (IQR, 1–12) days. Intravenous pulse steroids were used in 36 (30%) patients. The median initial oral steroid dose in prednisone equivalent units was 60 (IQR, 60–80) mg/d. Eleven (9%) patients received additional immunosuppression beyond steroids. Additional treatment-related details are shown in Table 3 and Supplemental Tables 7 and 8.
Table 3.
Treatment of ICPi-AKI with glucocorticoids, stratified by renal recovery
| Treatment Variable | All (n=119) | Complete Recovery (n=53) | Partial or No Recovery (n=66) | P Value |
|---|---|---|---|---|
| SCr at GC initiation, mg/dl | 3.01 (2.25–4.48) | 3.34 (2.29–4.63) | 2.89 (2.24–3.81) | 0.44 |
| Required RRT at GC initiation, n (%) | 3 (3) | 1 (2) | 2 (3) | 0.99 |
| Treatment delay, da | 3 (0–8) | 3 (1–8) | 3 (0–8) | 0.70 |
| Received IV pulse GC, n (%) | 36 (30) | 19 (36) | 17 (26) | 0.32 |
| Grams of solumedrol | 1.00 (0.38–2.03) | 1.00 (0.38–1.50) | 1.0 (0.41–2.88) | 0.99 |
| Initial daily oral GC dose (mg of prednisone) | 60 (60–80) | 60 (60–80) | 60 (60–80) | 0.97 |
| Days at initial oral GC dose | 7 (5–12) | 7 (5–10) | 7 (5–13) | 0.73 |
| Days at >20 mg oral prednisone | 28 (16–47) | 26 (16–39) | 31 (17–49) | 0.52 |
| Cumulative oral GC dose in first 2 wk (mg of prednisone) | 780 (600–980) | 775 (658–955) | 780 (570–980) | 0.78 |
| Days of oral GC | 63 (32–107) | 62 (35–98) | 67 (28–119) | 0.96 |
| Received non-GC immunosuppressant, n (%)b | 11 (9) | 4 (8) | 7 (11) | 0.75 |
| Nadir SCr after treatment, mg/dlc | 1.40 (1.06–1.73) | 1.08 (0.9–1.40) | 1.6 (1.40–1.90) | <0.001 |
Data are shown as median (IQR) and n (%). GC, glucocorticoids; IV, intravenous.
Denotes time from doubling of SCr to initiation of GCs.
Non-GC immunosuppression included mycophenolate mofetil (n=7), rituximab (n=2), cyclophosphamide (n=1), and eculizumab (n=1).
Defined as the lowest value achieved within 3 months after the AKI episode (excluding values obtained during RRT).
Kidney Recovery after ICPi-AKI
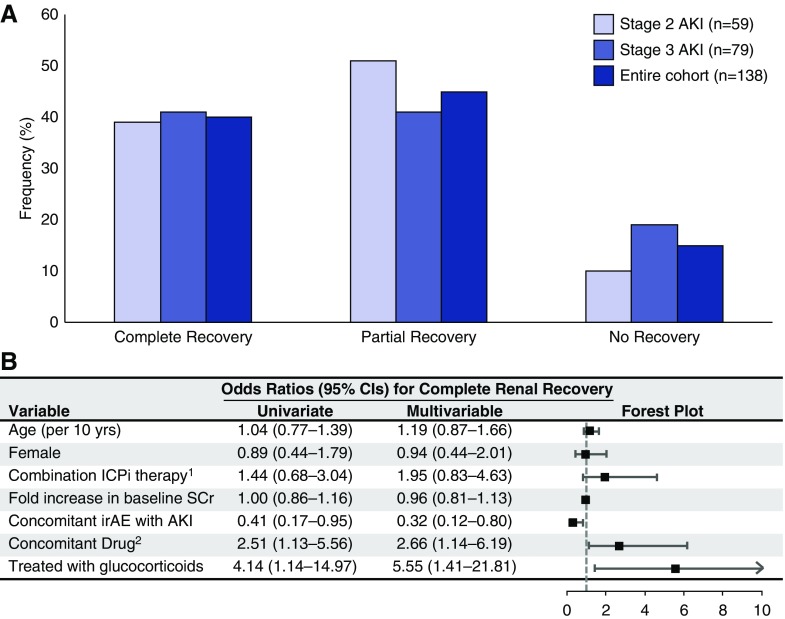
Complete, partial, and no kidney recovery after ICPi-AKI occurred in 40%, 45%, and 15% of patients, respectively, and the distribution did not differ significantly on the basis of AKI severity (Figure 3A). Similarly, there was no difference in recovery between biopsied and nonbiopsied patients (Supplemental Figure 3). Among the 13 patients who required RRT, partial (n=4) or complete (n=2) kidney recovery occurred in six (46%) patients.
Figure 3.
Renal recovery after ICPi-AKI. (A) The frequency of complete, partial, and no kidney recovery after an episode of ICPi-AKI. Complete recovery was defined as a return of SCr to <0.35 mg/dl of the baseline value, and partial recovery was defined as a return of SCr to >0.35 mg/dl but less than twice the baseline value, or liberation from RRT. (B) Univariate and multivariable adjusted odds ratios (and 95% confidence intervals) for achievement of complete kidney recovery. 1Combination ICPi therapy refers to treatment with both an anti–CTLA-4 and an anti–PD-1/PD-L1 antibody. 2Refers to concomitant use of potential TIN-causing medications, including antibiotics, NSAIDs, and PPIs within 2 weeks prior to the diagnosis of ICPi-AKI. 95% CI, confidence interval; CTLA-4, cytotoxic T lymphocyte–associated antigen 4; PD-1, programmed cell death 1; PD-L1, programmed death-ligand 1.
In a multivariable model, the presence of a concomitant extrarenal irAE was associated with a lower odds of achieving complete kidney recovery (Figure 3B). Conversely, simultaneous receipt of a TIN-causing medication and treatment with steroids were each associated with a greater odds of complete recovery. Similar results were obtained in the subgroup of patients who underwent renal biopsy, although treatment with steroids did not reach statistical significance (Supplemental Figure 4).
The more favorable outcome observed in patients taking a concomitant TIN-causing medication was driven predominantly by antibiotics and NSAIDs (Supplemental Table 9). Although treatment with steroids was associated with a greater odds of complete kidney recovery, no discernable differences in the steroid regimen were observed between patients who achieved complete recovery versus those who did not (Table 3). Finally, among patients with biopsy-confirmed TIN, no histologic feature was associated with kidney recovery, including the presence/severity of granulomatous features, tissue eosinophilia, interstitial fibrosis, or glomerulosclerosis (Supplemental Table 10).
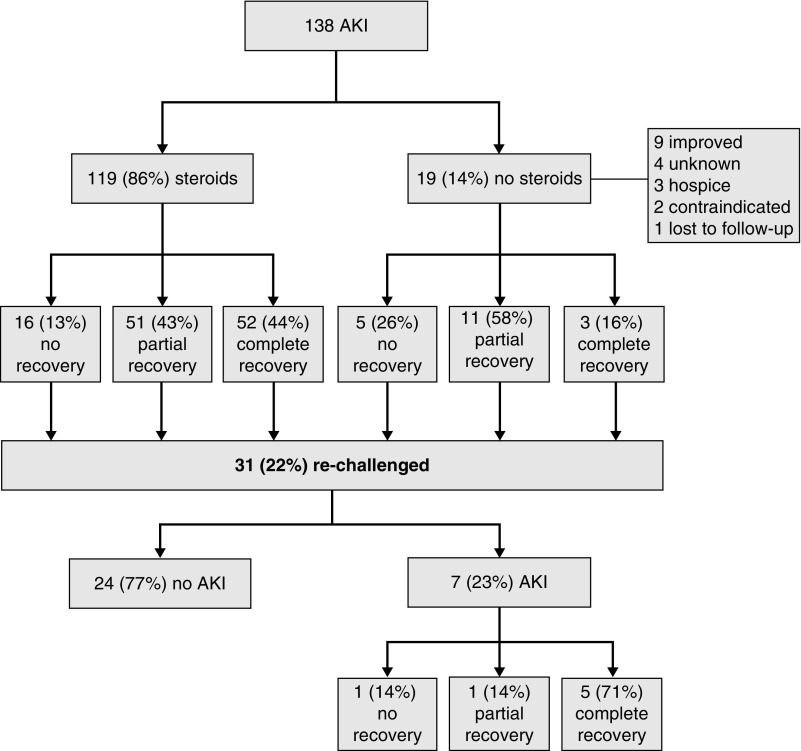
Rechallenge of Patients with ICPi-AKI
Rechallenge with an ICPi was attempted in 31 (22%) patients at a median of 1.8 (IQR, 1.2–11.0) months after the diagnosis of ICPi-AKI. Most patients (87%) were rechallenged with the same ICPi agent implicated in the initial AKI episode, and 39% of patients were receiving steroids at the time of rechallenge. Recurrent ICPi-AKI occurred in 23% of rechallenged patients (Figure 4). Patients who developed recurrent ICPi-AKI had a shorter latency period between the initial AKI episode and rechallenge (Table 4).
Figure 4.
Flow chart indicating rates of treatment with steroids, kidney recovery, rechallenge, and recurrence of ICPi-AKI.
Table 4.
Rechallenge with an ICPi after ICPi-AKI
| Variable | All Rechallenged (n=31) | Recurrent AKI (n=7) | No AKI (n=24) | P Value |
|---|---|---|---|---|
| Months from AKI to rechallenge | 1.80 (1.23–10.97) | 1.4 (0.73–1.63) | 2.05 (1.48–13.95) | 0.03 |
| Complete response, n (%) | 16 (52) | 2 (29) | 14 (58) | 0.22 |
| SCr at rechallenge, mg/dl | 1.30 (1.11–2.00) | 1.30 (1.22–1.60) | 1.39 (1.11–2.01) | 0.98 |
| On GC at rechallenge, n (%) | 12 (39) | 3 (43) | 9 (38) | 0.99 |
| Prednisone dose, mg/d | 10 (5–15) | 10 (5–10) | 10 (5–20) | 0.91 |
| Rechallenged with same ICPi, n (%) | 27 (87) | 7 (100) | 20 (83) | 0.55 |
| Months from rechallenge to AKI | NA | 1.53 (0.60–4.93) | NA | NA |
| SCr at recurrent AKI, mg/dl | NA | 2.70 (1.71–4.80) | NA | NA |
| Age at ICPi initiation, yr | 61 (57–71) | 59 (58–61) | 68 (56–71) | 0.29 |
| Female, n (%) | 8 (26) | 1 (14) | 7 (29) | 0.64 |
| Autoimmune disease, n (%) | 2 (6) | 0 (0) | 2 (8) | 0.99 |
| Extrarenal irAE, n (%) | 17 (55) | 5 (71) | 12 (50) | 0.41 |
| Stage 3 AKI, n (%) | 13 (42) | 2 (29) | 11 (46) | 0.67 |
| Biopsied, n (%) | 12 (39) | 3 (43) | 9 (38) | 0.99 |
Data are shown as median (IQR) and n (%). GC, glucocorticoids; SCr, serum creatinine; irAE, immune-related adverse event.
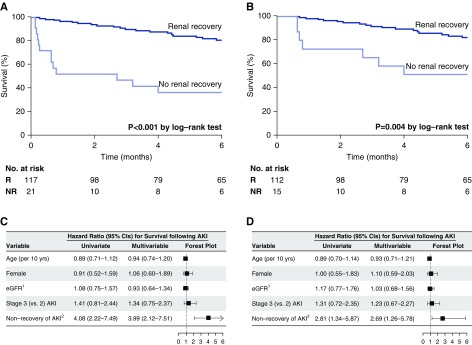
Patient Survival
Patients with no kidney recovery had a higher mortality than those with complete or partial kidney recovery (Figure 5A). Because early death after AKI precludes kidney recovery, we also performed a sensitivity analysis limited to patients who survived more than 2 weeks after ICPi-AKI, and found similar results (Figure 5B). In multivariable models, the absence of kidney recovery remained an independent predictor of increased mortality (Figure 5, C and D). Absence of kidney recovery was also independently associated with mortality in the subgroup of renal biopsied patients (Supplemental Figure 5).
Figure 5.
Kidney recovery status predicts overall survival. (A) Kaplan–Meier 6-month overall survival curves, stratified by kidney recovery status, starting at the time of development of ICPi-AKI (median duration of follow-up was 29 [IQR, 10–67] weeks). (B) Similar Kaplan–Meier survival curves but limited to patients who survived for at least 2 weeks after the development of ICPi-AKI. (C and D) Univariate and multivariable adjusted hazard ratios for 6-month mortality. 1Refers to per 30 ml/min per 1.73 m2 decline. 2The reference group is partial or complete recovery of AKI. 95% CI, 95% confidence interval; NR, no recovery; R, recovery.
Discussion
In this multicenter, retrospective cohort study of 138 patients with ICPi-AKI, the largest conducted to date, we provide several key insights into the clinical features and outcomes of ICPi-AKI. First, we identified lower baseline eGFR, PPI use, and combination therapy with anti-cytotoxic T lymphocyte–associated antigen 4 and anti-programed cell death 1/anti-programmed death-ligand 1 antibodies as independent risk factors for development of ICPi-AKI. Second, we confirm and expand on initial observations by our group7 and others8,9,12 on the clinical features of ICPi-AKI, including the variable and often prolonged delay between ICPi initiation and development of AKI, and the frequent rate of extrarenal irAEs occurring concomitantly or immediately preceding the AKI. Third, we confirm that TIN is the dominant lesion in patients with ICPi-AKI, occurring in 93% of biopsied patients. Fourth, we found that patients who have concomitant extrarenal irAEs have a lower likelihood of kidney recovery, whereas those receiving treatment with a concomitant TIN-causing medication, as well as those treated with steroids, have a higher likelihood of recovery. Fifth, we found that most patients rechallenged with an ICPi did not develop recurrence of ICPi-AKI. Finally, we found that failure to achieve kidney recovery after an episode of ICPi-AKI is associated with increased mortality.
Our findings are consistent with and expand on prior studies of ICPi-AKI. We identified three independent risk factors for ICPi-AKI: lower baseline eGFR, combination ICPi therapy, and PPI use. CKD is a well recognized risk factor for AKI across a variety of settings.13,14 Although relatively few patients in our study had advanced CKD, these patients appeared to be at greatly increased risk of ICPi-AKI (Tables 1 and 2). It is likely that this finding was a consequence of reduced renal reserve rather than a true increased propensity to immunologic injury. Nonetheless, patients with advanced CKD receiving ICPi therapy should have renal function monitored closely. Our finding that combination ICPi therapy was associated with an increased incidence of AKI was also noted in our prior analysis of clinical trial data.7 The paradigm of increased risk of irAEs with combination therapy extends to extrarenal organs as well, including the skin, liver, and endocrine system,1,15 and likely reflects enhanced stimulation of autoreactive T cells induced by dual immune checkpoint blockade.
More interesting is the association we detected between ICPi-AKI and PPI use. PPIs are known to cause TIN, albeit rarely.16,17 However, given the high prevalence of their use, PPIs are now one of the most common causes of drug-induced TIN.18 There is likely a complex interplay between drugs known to cause TIN, like PPIs, and ICPis. ICPis alone are sufficient to induce autoimmunity (including TIN) in humans7; however, it is notable that a large proportion of previously reported patients with ICPi-AKI were also receiving drugs known to cause TIN, including NSAIDs, antibiotics, and PPIs.7,8 Similarly, we found that nearly 70% of the patients with ICPi-AKI in this study were receiving a potential TIN-causing medication, including PPI use in over 50% of the patients. These findings suggest that ICPi treatment can lead to loss of tolerance via activation or reactivation of drug-specific T cells in some patients. Thus, PPIs should be used with caution in patients receiving ICPi treatment, and should likely be discontinued in those who develop ICPi-AKI.
We found that the clinical features of ICPi-AKI largely mirror those of other causes of drug-associated TIN,18,19 with the notable exception of the variable and often prolonged latency between drug initiation and AKI. The majority of patients had subnephrotic proteinuria and pyuria at the time of ICPi-AKI. Neither finding, however, was highly sensitive for the diagnosis: proteinuria (≥0.3 g/g) and pyuria (more than a trace of leukocyte esterase on urine dipstick) were absent in 29% and 45% of cases, respectively. Finally, an extrarenal irAE occurred before or concomitantly with the AKI in 43% of cases. Thus, no clinical features reliably distinguish ICPi-AKI from other causes of AKI. These findings are of particular importance in patients with cancer, where AKI commonly occurs because of ischemic or nephrotoxic acute tubular injury/necrosis.20 Guidelines published by the American Society of Clinical Oncology discourage renal biopsy in lieu of empirical glucocorticoid treatment when ICPi-AKI is suspected.21 Given the lack of specific clinical features to distinguish ICPi-AKI from other causes of AKI, this approach runs the risk of inappropriately exposing patients with other histologic lesions to glucocorticoids. Underscoring this notion is a recent case series in which five out of ten patients with suspected ICPi-AKI were found to have acute tubular injury/necrosis on biopsy.12 An additional and likely greater risk is that ICPi therapy may be inappropriately discontinued in cases where AKI was erroneously attributed to the ICPi. The clinician must weigh the risks and benefits of renal biopsy each patient. Patients treated with ICPis are often ill with multiple comorbidities, which can make biopsy challenging and higher risk. However, given the lack of specific clinical and laboratory features, we and others22 feel that biopsy should be strongly considered when feasible, particularly when alternative causes of AKI exist.
We found that TIN was the dominant histologic lesion, occurring in 93% of biopsied patients. These findings are consistent with prior reports.7,8 Importantly, other immune-mediated lesions have also been reported, including podocytopathies and pauci-immune GN.9 In this study, we document four additional cases of ICPi-AKI due to glomerular disease. These findings further highlight the importance of obtaining a renal biopsy in patients with suspected ICPi-AKI.
Most patients with ICPi-AKI had partial (45%) or complete (40%) recovery of renal function. The presence of a concomitant irAE was associated with a worse renal prognosis. This may be the result of a greater state of immune activation in these patients that was less responsive to discontinuation of ICPi therapy and immunosuppression. It is also possible that complications from extrarenal irAEs (e.g., volume depletion from colitis, or impaired renal perfusion owing to myocarditis) led to additional tubular injury and impaired kidney recovery. Interestingly, ICPi-AKI cases that occurred in patients receiving a concomitant TIN-causing medication had a greater probability of complete kidney recovery. This may reflect T cell reactivity to the drug rather than to endogenous autoantigens, in which case cessation of the offending NSAID, antibiotic, or PPI would lead to a more rapid attenuation of immunologic activity.23
The treatment of drug-induced TIN with glucocorticoids is controversial, with data limited to conflicting observational studies.19,24 The unique proposed mechanisms of ICPi-AKI,25 in which the effects of immune stimulation persist after ICPi discontinuation, along with the experience of managing extrarenal irAEs,21 provides the rationale for glucocorticoid therapy in ICPi-AKI. In our study, treatment with glucocorticoids was independently associated with complete kidney recovery. However, we were not able to identify any specific features of the glucocorticoid regimen that were associated with greater treatment efficacy. This is not unexpected, as glucocorticoid dosing and tapering are intrinsically linked to and confounded by comorbidities, disease severity, and response to treatment. Such confounding factors have precluded the ability to define the optimal glucocorticoid regimen for drug-induced TIN in general.26
The decision to rechallenge with an ICPi after an episode of ICPi-AKI, particularly when the AKI is severe, carries enormous weight. This decision is currently rendered more difficult because of limited data on the risk of recurrent AKI. Our study provides outcomes on 31 patients with ICPi-AKI who underwent ICPi rechallenge. Despite 87% of patients receiving the same ICPi implicated in the initial AKI episode, 77% of those rechallenged did not develop recurrent AKI. We found no difference in the frequency of steroid use at rechallenge among those who developed recurrent AKI (three out of seven; 43%) versus those who did not (nine out of 24; 38%); however, because of the low event rate of recurrent AKI, these findings should be interpreted cautiously. Patients developing recurrent ICPi-AKI were rechallenged sooner after the initial ICPi-AKI episode, suggesting reinitiating of ICPis should be delayed if feasible.
Failure to recover from ICPi-AKI was associated with reduced survival. Although this may not be unexpected,27 it stands in contrast to the experience with irAEs in general. In patients with melanoma, neither development of an irAE requiring immunosuppression nor the need to discontinue ICPi therapy because of a severe irAE was associated with decreased survival.28,29 However, ICPi-AKI, unlike most other irAEs, can result in irreversible organ damage even after immunosuppression has led to cessation of immunologic activity. This may be partly attributable to the indolent nature of TIN and the poor sensitivity of SCr for early kidney damage, which together often allow TIN to continue unabated for extended periods before being recognized. The increased mortality associated with failure to recover from ICPi-AKI may reflect the limited cancer therapeutic options for patients with persistently impaired renal function, and stresses the importance of early recognition and treatment of this entity before irreversible kidney damage occurs.
Although our study is the largest to date and provides several key insights into ICPi-AKI, we acknowledge several limitations. We focused on patients who had at least a doubling of SCr or the need for RRT because we were interested in the most clinically relevant episodes of ICPi-AKI. However, our findings may not be generalizable to patients with more mild ICPi-AKI. Additionally, it is possible that some nonbiopsied patients had alternative causes of AKI not directly attributable to the ICPi (e.g., acute tubular necrosis), and were misadjudicated by the treating clinicians as having ICPi-AKI. It is, however, reassuring that clinical features were similar among biopsied and nonbiopsied patients. Potential TIN-causing medications were only reported if administered within 2 weeks of the AKI episode. It is therefore possible that in a small number of patients a medication discontinued more than 2 weeks before AKI could have initiated the TIN episode. Cases and controls were not selected from the same at-risk population because control patients were selected from two sites in Boston, whereas cases were selected from 18 sites from across the country. However, the two sites from which control patients were selected are each large academic cancer centers that treat highly diverse patient populations. Further, control patients initiated ICPis contemporaneously with cases and were selected at random and without any inclusion or exclusion criteria applied other than the absence of AKI. Finally, although our hypotheses were prespecified, we cannot exclude the possibility of a type 1 error because of the large number of tests performed.
In conclusion, we provide new data of interest to both clinicians and researchers, including risk factors for ICPi-AKI development, determinants of treatment response, and the recurrence rate of AKI after ICPi rechallenge. Further advancement in the care of patients with ICPi-AKI will require multicenter collaboration to collect biologically relevant samples that can be interpreted in the context of clinical outcomes. Discovery of biomarkers for ICPi-AKI could lead to early diagnosis, assist in discriminating ICPi-AKI from other causes of AKI, and help inform the risk of recurrent ICPi-AKI with rechallenge.
Disclosures
Dr. Assal reports grants from NIH/NCI Cancer Center, during the conduct of the study; personal fees from Alpha Insights, personal fees from Boston Biomedical, personal fees from Incyte Corporation, grants from Incyte Corporation, outside the submitted work. Dr. Glezerman reports other from Pfizer Inc., outside the submitted work. Dr. Gupta reports grants from NIH, during the conduct of the study. Dr. Johnson reports other from Array Biopharma, grants and other from BMS, grants and other from Incyte, other from Merck, other from Novartis, outside the submitted work. Dr. Leaf reports grants from BioPorto Diagnostics, outside the submitted work. Dr. Marrone reports other from AstraZeneca, other from Compugen, other from Takeda, outside the submitted work. Dr. Vijayan reports personal fees from Sanofi-Aventis, outside the submitted work. All other authors report no relevant disclosures.
Funding
Dr. Glezerman is supported by the National Cancer Institute (grant P30CA008748). Dr. Murakami is supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK; grant K08DK120868) and an American Society of Nephrology (ASN) Foundation for Kidney Research Carl W. Gottschalk research scholar grant. Dr. Herrmann is supported by the NIDDK (grant K08DK118120). Dr. Sise is supported by the NIDDK (grant K23DK117014). Dr. Leaf is supported by the NIDDK (grant K23DK106448), the National Heart, Lung, and Blood Institute (grant R01HL144566), and an ASN Foundation for Kidney Research Carl W. Gottschalk research scholar grant.
Supplementary Material
Acknowledgments
Concept and design: all authors. Acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: Dr. Cortazar and Dr. Leaf. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: Dr. Cortazar, Ms. Kibbelaar, and Dr. Leaf. Preparation of figures and tables: Dr. Cortazar, Ms. Kibbelaar, and Dr. Leaf. All authors approved the final version of the manuscript, and all are accountable for all aspects of the submitted work.
The authors thank Dino Mazzarelli, J.D., from Partners Healthcare Research Management, for his invaluable assistance coordinating the respective data transfer and use agreements with each institution.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
Supplemental Material
This article contains the following supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2019070676/-/DCSupplemental.
Supplemental Appendix 1. Data collected on cases.
Supplemental Table 1. List of collaborating institutions.
Supplemental Table 2. ICPi initiation by year, cases versus controls.
Supplemental Table 3. Baseline characteristics of biopsied and nonbiopsied patients with ICPi-AKI.
Supplemental Table 4. Risk factors for ICPi-AKI among biopsied patients.
Supplemental Table 5. Concomitant chemotherapeutic nephrotoxins.
Supplemental Table 6. Histologic features of biopsied patients with TIN.
Supplemental Table 7. Treatment of ICPi-AKI, stratified by biopsy status.
Supplemental Table 8. Clinical features of patients receiving immunosuppression in addition to steroids (n=11).
Supplemental Table 9. Odds ratios for complete kidney recovery according to concomitant potential TIN-causing medications.
Supplemental Table 10. Odds ratios for complete kidney recovery according to histologic features in patients with TIN.
Supplemental Figure 1. Clinical features of ICPi-AKI in biopsied patients with TIN.
Supplemental Figure 2. Clinical features of ICPi-AKI in patients with and without biopsy-proved TIN.
Supplemental Figure 3. Kidney recovery after ICPi-AKI among biopsied versus nonbiopsied patients.
Supplemental Figure 4. Factors associated with kidney recovery after ICPi-AKI among biopsied patients.
Supplemental Figure 5. Kidney recovery status predicts overall survival in biopsied-only patients.
References
- 1.Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Cowey CL, Lao CD, et al.: Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med 373: 23–34, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gandhi L, Rodríguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F, et al.: KEYNOTE-189 Investigators : Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med 378: 2078–2092, 2018 [DOI] [PubMed] [Google Scholar]
- 3.Wei SC, Duffy CR, Allison JP: Fundamental mechanisms of immune checkpoint blockade therapy. Cancer Discov 8: 1069–1086, 2018 [DOI] [PubMed] [Google Scholar]
- 4.Postow MA, Sidlow R, Hellmann MD: Immune-related adverse events associated with immune checkpoint blockade. N Engl J Med 378: 158–168, 2018 [DOI] [PubMed] [Google Scholar]
- 5.Haanen JBAG, Carbonnel F, Robert C, Kerr KM, Peters S, Larkin J, et al.: ESMO Guidelines Committee : Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 28[Suppl 4]: iv119–iv142, 2017 [DOI] [PubMed] [Google Scholar]
- 6.Haslam A, Prasad V: Estimation of the percentage of US patients with cancer who are eligible for and respond to checkpoint inhibitor immunotherapy drugs. JAMA Netw Open 2: e192535, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cortazar FB, Marrone KA, Troxell ML, Ralto KM, Hoenig MP, Brahmer JR, et al.: Clinicopathological features of acute kidney injury associated with immune checkpoint inhibitors. Kidney Int 90: 638–647, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shirali AC, Perazella MA, Gettinger S: Association of acute interstitial nephritis with programmed cell death 1 inhibitor therapy in lung cancer patients. Am J Kidney Dis 68: 287–291, 2016 [DOI] [PubMed] [Google Scholar]
- 9.Mamlouk O, Selamet U, Machado S, Abdelrahim M, Glass WF, Tchakarov A, et al.: Nephrotoxicity of immune checkpoint inhibitors beyond tubulointerstitial nephritis: Single-center experience. J Immunother Cancer 7: 2, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kellum JA, Lameire N, Aspelin P, Barsoum RS, Burdmann EA, Goldstein SL, et al. : Kidney disease: Improving Global Outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2: 1–138, 2012 [Google Scholar]
- 11.Dewitte A, Joannès-Boyau O, Sidobre C, Fleureau C, Bats ML, Derache P, et al.: Kinetic eGFR and novel AKI biomarkers to predict renal recovery. Clin J Am Soc Nephrol 10: 1900–1910, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Izzedine H, Mathian A, Champiat S, Picard C, Mateus C, Routier E, et al.: Renal toxicities associated with pembrolizumab. Clin Kidney J 12: 81–88, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Waikar SS, Liu KD, Chertow GM: Diagnosis, epidemiology and outcomes of acute kidney injury. Clin J Am Soc Nephrol 3: 844–861, 2008 [DOI] [PubMed] [Google Scholar]
- 14.Singh P, Rifkin DE, Blantz RC: Chronic kidney disease: An inherent risk factor for acute kidney injury? Clin J Am Soc Nephrol 5: 1690–1695, 2010 [DOI] [PubMed] [Google Scholar]
- 15.Wolchok JD, Chiarion-Sileni V, Gonzalez R, Rutkowski P, Grob JJ, Cowey CL, et al.: Overall survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med 377: 1345–1356, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brewster UC, Perazella MA: Proton pump inhibitors and the kidney: Critical review. Clin Nephrol 68: 65–72, 2007 [DOI] [PubMed] [Google Scholar]
- 17.Blank ML, Parkin L, Paul C, Herbison P: A nationwide nested case-control study indicates an increased risk of acute interstitial nephritis with proton pump inhibitor use. Kidney Int 86: 837–844, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muriithi AK, Leung N, Valeri AM, Cornell LD, Sethi S, Fidler ME, et al.: Biopsy-proven acute interstitial nephritis, 1993-2011: a case series. Am J Kidney Dis 64: 558–566, 2014 [DOI] [PubMed] [Google Scholar]
- 19.González E, Gutiérrez E, Galeano C, Chevia C, de Sequera P, Bernis C, et al.: Grupo Madrileño De Nefritis Intersticiales : Early steroid treatment improves the recovery of renal function in patients with drug-induced acute interstitial nephritis. Kidney Int 73: 940–946, 2008 [DOI] [PubMed] [Google Scholar]
- 20.Kitchlu A, McArthur E, Amir E, Booth CM, Sutradhar R, Majeed H, et al.: Acute kidney injury in patients receiving systemic treatment for cancer: A population-based cohort study [published online ahead of print November 13, 2018]. J Natl Cancer Inst doi: 10.1093/jnci/djy167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brahmer JR, Lacchetti C, Schneider BJ, Atkins MB, Brassil KJ, Caterino JM, et al.: National Comprehensive Cancer Network : Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American society of clinical oncology clinical practice guideline. J Clin Oncol 36: 1714–1768, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perazella MA, Sprangers B: AKI in patients receiving immune checkpoint inhibitors. Clin J Am Soc Nephrol 14: 1077–1079, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koda R, Watanabe H, Tsuchida M, Iino N, Suzuki K, Hasegawa G, et al.: Immune checkpoint inhibitor (nivolumab)-associated kidney injury and the importance of recognizing concomitant medications known to cause acute tubulointerstitial nephritis: A case report. BMC Nephrol 19: 48, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clarkson MR, Giblin L, O’Connell FP, O’Kelly P, Walshe JJ, Conlon P, et al.: Acute interstitial nephritis: Clinical features and response to corticosteroid therapy. Nephrol Dial Transplant 19: 2778–2783, 2004 [DOI] [PubMed] [Google Scholar]
- 25.Perazella MA, Shirali AC: Nephrotoxicity of cancer immunotherapies: Past, present and future. J Am Soc Nephrol 29: 2039–2052, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fernandez-Juarez G, Perez JV, Caravaca-Fontán F, Quintana L, Shabaka A, Rodriguez E, et al.: Spanish Group for the Study of Glomerular Diseases (GLOSEN) : Duration of treatment with corticosteroids and recovery of kidney function in acute interstitial nephritis. Clin J Am Soc Nephrol 13: 1851–1858, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pannu N, James M, Hemmelgarn B, Klarenbach S; Alberta Kidney Disease Network : Association between AKI, recovery of renal function, and long-term outcomes after hospital discharge. Clin J Am Soc Nephrol 8: 194–202, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Horvat TZ, Adel NG, Dang TO, Momtaz P, Postow MA, Callahan MK, et al.: Immune-related adverse events, need for systemic immunosuppression, and effects on survival and time to treatment failure in patients with melanoma treated with ipilimumab at memorial sloan kettering cancer center. J Clin Oncol 33: 3193–3198, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schadendorf D, Wolchok JD, Hodi FS, Chiarion-Sileni V, Gonzalez R, Rutkowski P, et al.: Efficacy and safety outcomes in patients with advanced melanoma who discontinued treatment with nivolumab and ipilimumab because of adverse events: A pooled analysis of randomized phase II and III trials. J Clin Oncol 35: 3807–3814, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.